Volume 7, Issue 1 (2-2020)
JROS 2020, 7(1): 13-22 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bagherifard A, Gharanizadeh K, Salehpour M, Jafarpour H, Mahmoudi M. Comparing Prophylactic Effect of Rivaroxaban and Enoxaparin on Thromboembolism After Total Hip or Knee Arthroplasty. JROS 2020; 7 (1) :13-22
URL: http://jros.iums.ac.ir/article-1-2060-en.html
URL: http://jros.iums.ac.ir/article-1-2060-en.html
Abolfazl Bagherifard1 

 , Kaveh Gharanizadeh1
, Kaveh Gharanizadeh1 

 , Mostafa Salehpour1
, Mostafa Salehpour1 

 , Hamed Jafarpour2
, Hamed Jafarpour2 

 , Mani Mahmoudi1
, Mani Mahmoudi1 




 , Kaveh Gharanizadeh1
, Kaveh Gharanizadeh1 

 , Mostafa Salehpour1
, Mostafa Salehpour1 

 , Hamed Jafarpour2
, Hamed Jafarpour2 

 , Mani Mahmoudi1
, Mani Mahmoudi1 


1- Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
2- Student Research Committee, Faculty of Medicine, Mazandaran University of Medical Sciences, Sari, Iran.
Keywords: Arthroplasty, Knee joint replacement, Hip arthroplasty, Thromboprophylactic, Rivaroxaban, Enoxaparin
Full-Text [PDF 632 kb]
(917 Downloads)
Full-Text: (803 Views)
1. Introduction
Vascular thromboembolism is one of the essential factors in reducing the quality of life after arthroplasty. Intravenous thromboembolism occurs in about two-thirds of patients, especially in the first three weeks after the operation, and becomes symptomatic in 2%-4% of cases. Besides, one-third of thromboembolism patients are vulnerable to problems such as post-thromboembolism syndrome. Therefore, reducing the incidence of thromboembolism after arthroplasty is one of the priorities for optimizing these operations [1, 2]. Anticoagulant prophylaxis is one of the most common thromboembolism risk reduction methods. However, various drugs are used in this prophylaxis.
Unfractionated heparin is one of the oldest thromboprophylactic drugs. It binds to anti-thrombin III to prevent thrombin activation and thereby preventing blood clotting. From time immemorial, heparin has been widely used to reduce vascular thromboembolism following surgery [3]. However, its use has been minimized due to its unpleasant method of use (subcutaneous injection 2-3 times a day). Low molecular weight heparin is the next generation of thromboprophylactic drugs derived from decomposed heparin. Enoxaparin is one of the low molecular weight heparins [3].
Other thromboprophylactic agents include warfarin, which acts as a vitamin K inhibitor, thereby preventing blood coagulation. Warfarin is one of the first oral thromboprophylactic drugs. However, its use has been minimized due to the risk of bleeding, potential drug reactions, and the need for continued monitoring [3]. Aspirin is another thromboprophylactic drug that acts primarily through platelet inhibition. Aspirin is one of the favored thromboprophylactic drugs and is still widely used in many conditions. However, aspirin use is mainly limited to patients with low risk of vascular thromboembolism. Factor Xa inhibitors are the newest generation of thromboprophylactic drugs. Rivaroxaban is one of these medications that is taken orally and does not require continuous monitoring [4].
In the past, the use of injectable anticoagulants such as enoxaparin was much more common. Now, these anticoagulants are used less because of the need for continuous monitoring and their unpleasant administration route (injection). Oral anticoagulants, such as aspirin and rivaroxaban, are more popular nowadays. They do not need constant supervision and will cost less for the patient and the health system because the patient can use them without needing to visit health centers for injections [4].
Although different protocols have been proposed for the use of thromboprophylactic drugs, there is still no consensus over a standard protocol, and even some centers have developed their protocols. Anticoagulant prophylaxis is prescribed to minimize vascular thromboembolism and bleeding complications. In this study, the efficacy and safety of enoxaparin injectable drug are compared with oral medications, aspirin, and rivaroxaban regarding vascular thromboembolism and their side effects after knee and hip replacement surgery. We are going to determine which of them is best suited for broader use.
2. Methods
This study is a double-blind, randomized controlled trial conducted in patients undergoing total hip or knee arthroplasty at Shafa Yahyaian Hospital from 2016 to 2018 to compare the effect of rivaroxaban and enoxaparin on thromboembolism prophylaxis.
Study patients:
Patients undergoing knee or hip arthroplasty who were 18 years or older were enrolled in the study. The patients who were pregnant, lactating, have active bleeding, liver disease, severe renal failure (creatinine clearance less than 30 mL/min) were excluded from the study.
Study design and drugs
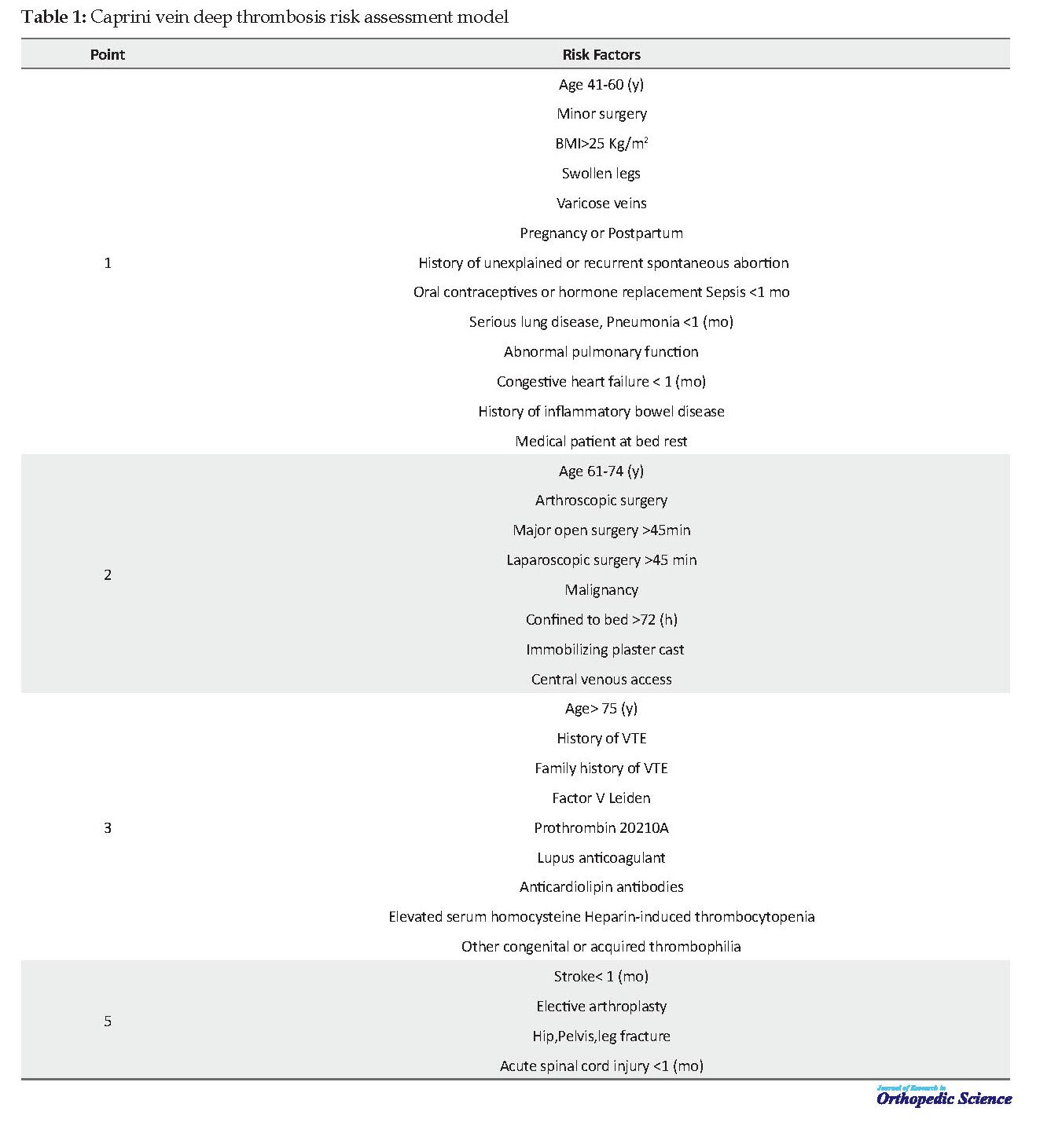
Patients were divided into low-risk and moderate- to high-risk groups according to Caprini score. Thus, if the Caprini score of the patients was 1-2, they were classified as low-risk patients, Caprini score of 3-4, as moderate, and Caprini score of 5 and above as high risk (Table 1). The low-risk patients were treated with aspirin, and moderate- to high-risk patients were randomly assigned to one of the enoxaparin and rivaroxaban groups.
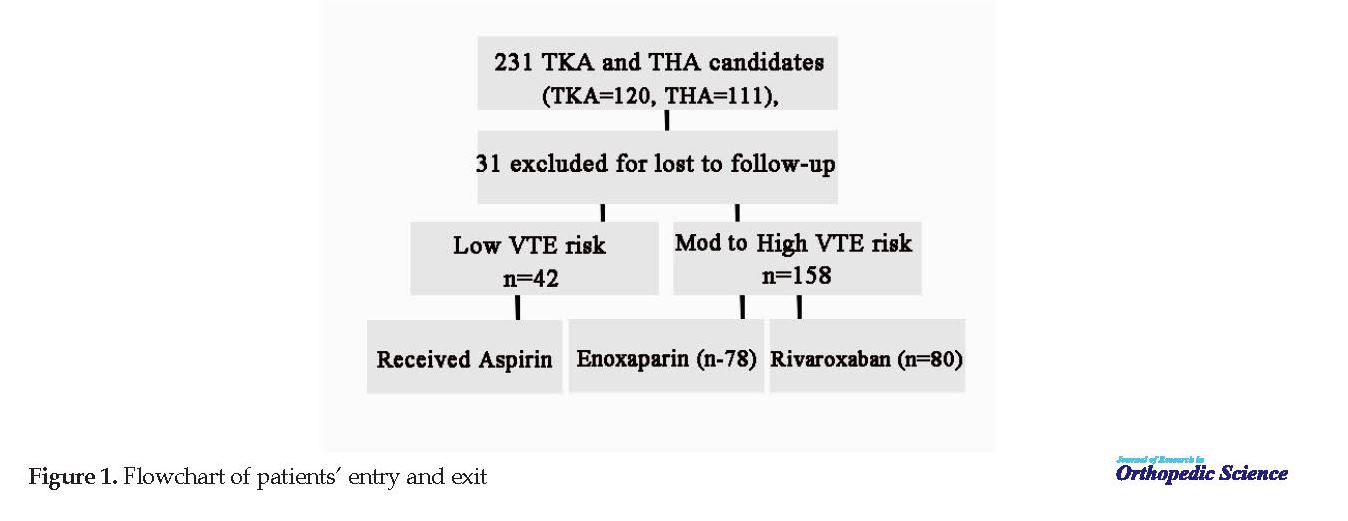
The aspirin group received oral aspirin at a dose of 325 mg once daily for 28 days. The enoxaparin group received enoxaparin with a dose of 40 mg subcutaneously for 14 days and then aspirin with a dose of 325 mg for another 14 days. The rivaroxaban group received rivaroxaban with a dose of 10 mg orally for 12 days (mean 10-14) and then aspirin with a dose of 325 mg daily for 14 days. The first dose of the drug was received on the evening of operation day. All patients received rivaroxaban from the Axabin brand (Arena Hayat Danesh Company, Iran), and in the enoxaparin group, all patients were treated with the Rolexan brand (Ronak Daru, Iran) (Figure 1).
Complete Blood Count (CBC) and renal tests, including BUN (Blood Urea Nitrogen) and Cr (Creatinine), were performed for all patients before the surgery. Also, these tests were performed daily for up to 3 days after surgery and at discharge. Patients were followed up after the operation and until hospitalization, and then they were visited in 2, 6, and 24 weeks after discharge. Clinical examination for symptoms of DVT (deep vein thrombosis) including swelling (the increase in size compared with the opposite organ) and extreme pain in lower organs (especially in patio dorsiflexion) and inferior limbs and clinical symptoms of PTE (pulmonary thromboembolism), such as shortness of breath, increased heart rate, and lowered blood pressure were checked at these visits.
In case of any suspicious or obvious symptom, the patient would undergo intravenous Doppler ultrasound or diffusion perfusion scan after consultation with a cardiologist. These clinical symptoms are also instructed at the time of discharge so that patients visit the emergency room if any of the symptoms occurred. Any gastrointestinal or systemic complaints, including skin problems that began after the start of the treatment, were also examined.
Severe hemorrhage (hemoglobin reduction of more than 2 g/dL or requiring blood transfusion) was assessed after the first dose of medication until patient discharge with daily hemoglobin testing. Frequency of other side effects such as wound complications (ecchymosis, hematoma, and wound infection) and gastrointestinal or skin problems were recorded and compared by daily examination during the hospital stay and then in the future visits to the clinic for up to 6 months in each group. Follow up visits were performed at weeks 6, 12, and 24.
Data analysis method
Statistical analysis was done in SPSS 24. The central tendency and dispersion indices, including mean and standard deviation, were used to present the descriptive data. In the case of the normal distribution, the Independent t test, and in the case of abnormal distribution, the Mann-Whitney U test was used to compare quantitative criteria between two groups of patients. The Chi-square test was used to compare the qualitative criteria between the two groups. P values less than 0.05 were considered significant in all tests.
Operation procedure
Unless there was a contraindication, all operations were performed under general or spinal anesthesia. A standard protocol was used in all operations. All total knee joint replacement operations were performed under tourniquet control and through an anterior medial cut using the middle parapatellar or subvastus approach. Pelvic joint replacement was also performed with either anterior or anterolateral or lateral approach.
3. Results
A total of 231 patients undergoing knee replacement or hip replacement operations were included in the study. Thirty-one patients were excluded due to missing the follow-up visits. In the remaining 200 patients, 42 low-risk and 158 moderate- to high-risk patients were identified, according to Caprini risk assessment model. They were divided into three groups: aspirin (42 patients), enoxaparin (78 patients), and rivaroxaban (80 patients). The study population consisted of 105 cases of total knee arthroplasty and 95 cases of total hip arthroplasty (Figure 1).
Vascular thromboembolism is one of the essential factors in reducing the quality of life after arthroplasty. Intravenous thromboembolism occurs in about two-thirds of patients, especially in the first three weeks after the operation, and becomes symptomatic in 2%-4% of cases. Besides, one-third of thromboembolism patients are vulnerable to problems such as post-thromboembolism syndrome. Therefore, reducing the incidence of thromboembolism after arthroplasty is one of the priorities for optimizing these operations [1, 2]. Anticoagulant prophylaxis is one of the most common thromboembolism risk reduction methods. However, various drugs are used in this prophylaxis.
Unfractionated heparin is one of the oldest thromboprophylactic drugs. It binds to anti-thrombin III to prevent thrombin activation and thereby preventing blood clotting. From time immemorial, heparin has been widely used to reduce vascular thromboembolism following surgery [3]. However, its use has been minimized due to its unpleasant method of use (subcutaneous injection 2-3 times a day). Low molecular weight heparin is the next generation of thromboprophylactic drugs derived from decomposed heparin. Enoxaparin is one of the low molecular weight heparins [3].
Other thromboprophylactic agents include warfarin, which acts as a vitamin K inhibitor, thereby preventing blood coagulation. Warfarin is one of the first oral thromboprophylactic drugs. However, its use has been minimized due to the risk of bleeding, potential drug reactions, and the need for continued monitoring [3]. Aspirin is another thromboprophylactic drug that acts primarily through platelet inhibition. Aspirin is one of the favored thromboprophylactic drugs and is still widely used in many conditions. However, aspirin use is mainly limited to patients with low risk of vascular thromboembolism. Factor Xa inhibitors are the newest generation of thromboprophylactic drugs. Rivaroxaban is one of these medications that is taken orally and does not require continuous monitoring [4].
In the past, the use of injectable anticoagulants such as enoxaparin was much more common. Now, these anticoagulants are used less because of the need for continuous monitoring and their unpleasant administration route (injection). Oral anticoagulants, such as aspirin and rivaroxaban, are more popular nowadays. They do not need constant supervision and will cost less for the patient and the health system because the patient can use them without needing to visit health centers for injections [4].
Although different protocols have been proposed for the use of thromboprophylactic drugs, there is still no consensus over a standard protocol, and even some centers have developed their protocols. Anticoagulant prophylaxis is prescribed to minimize vascular thromboembolism and bleeding complications. In this study, the efficacy and safety of enoxaparin injectable drug are compared with oral medications, aspirin, and rivaroxaban regarding vascular thromboembolism and their side effects after knee and hip replacement surgery. We are going to determine which of them is best suited for broader use.
2. Methods
This study is a double-blind, randomized controlled trial conducted in patients undergoing total hip or knee arthroplasty at Shafa Yahyaian Hospital from 2016 to 2018 to compare the effect of rivaroxaban and enoxaparin on thromboembolism prophylaxis.
Study patients:
Patients undergoing knee or hip arthroplasty who were 18 years or older were enrolled in the study. The patients who were pregnant, lactating, have active bleeding, liver disease, severe renal failure (creatinine clearance less than 30 mL/min) were excluded from the study.
Study design and drugs
Patients were divided into low-risk and moderate- to high-risk groups according to Caprini score. Thus, if the Caprini score of the patients was 1-2, they were classified as low-risk patients, Caprini score of 3-4, as moderate, and Caprini score of 5 and above as high risk (Table 1). The low-risk patients were treated with aspirin, and moderate- to high-risk patients were randomly assigned to one of the enoxaparin and rivaroxaban groups.
The aspirin group received oral aspirin at a dose of 325 mg once daily for 28 days. The enoxaparin group received enoxaparin with a dose of 40 mg subcutaneously for 14 days and then aspirin with a dose of 325 mg for another 14 days. The rivaroxaban group received rivaroxaban with a dose of 10 mg orally for 12 days (mean 10-14) and then aspirin with a dose of 325 mg daily for 14 days. The first dose of the drug was received on the evening of operation day. All patients received rivaroxaban from the Axabin brand (Arena Hayat Danesh Company, Iran), and in the enoxaparin group, all patients were treated with the Rolexan brand (Ronak Daru, Iran) (Figure 1).
Complete Blood Count (CBC) and renal tests, including BUN (Blood Urea Nitrogen) and Cr (Creatinine), were performed for all patients before the surgery. Also, these tests were performed daily for up to 3 days after surgery and at discharge. Patients were followed up after the operation and until hospitalization, and then they were visited in 2, 6, and 24 weeks after discharge. Clinical examination for symptoms of DVT (deep vein thrombosis) including swelling (the increase in size compared with the opposite organ) and extreme pain in lower organs (especially in patio dorsiflexion) and inferior limbs and clinical symptoms of PTE (pulmonary thromboembolism), such as shortness of breath, increased heart rate, and lowered blood pressure were checked at these visits.
In case of any suspicious or obvious symptom, the patient would undergo intravenous Doppler ultrasound or diffusion perfusion scan after consultation with a cardiologist. These clinical symptoms are also instructed at the time of discharge so that patients visit the emergency room if any of the symptoms occurred. Any gastrointestinal or systemic complaints, including skin problems that began after the start of the treatment, were also examined.
Severe hemorrhage (hemoglobin reduction of more than 2 g/dL or requiring blood transfusion) was assessed after the first dose of medication until patient discharge with daily hemoglobin testing. Frequency of other side effects such as wound complications (ecchymosis, hematoma, and wound infection) and gastrointestinal or skin problems were recorded and compared by daily examination during the hospital stay and then in the future visits to the clinic for up to 6 months in each group. Follow up visits were performed at weeks 6, 12, and 24.
Data analysis method
Statistical analysis was done in SPSS 24. The central tendency and dispersion indices, including mean and standard deviation, were used to present the descriptive data. In the case of the normal distribution, the Independent t test, and in the case of abnormal distribution, the Mann-Whitney U test was used to compare quantitative criteria between two groups of patients. The Chi-square test was used to compare the qualitative criteria between the two groups. P values less than 0.05 were considered significant in all tests.
Operation procedure
Unless there was a contraindication, all operations were performed under general or spinal anesthesia. A standard protocol was used in all operations. All total knee joint replacement operations were performed under tourniquet control and through an anterior medial cut using the middle parapatellar or subvastus approach. Pelvic joint replacement was also performed with either anterior or anterolateral or lateral approach.
3. Results
A total of 231 patients undergoing knee replacement or hip replacement operations were included in the study. Thirty-one patients were excluded due to missing the follow-up visits. In the remaining 200 patients, 42 low-risk and 158 moderate- to high-risk patients were identified, according to Caprini risk assessment model. They were divided into three groups: aspirin (42 patients), enoxaparin (78 patients), and rivaroxaban (80 patients). The study population consisted of 105 cases of total knee arthroplasty and 95 cases of total hip arthroplasty (Figure 1).
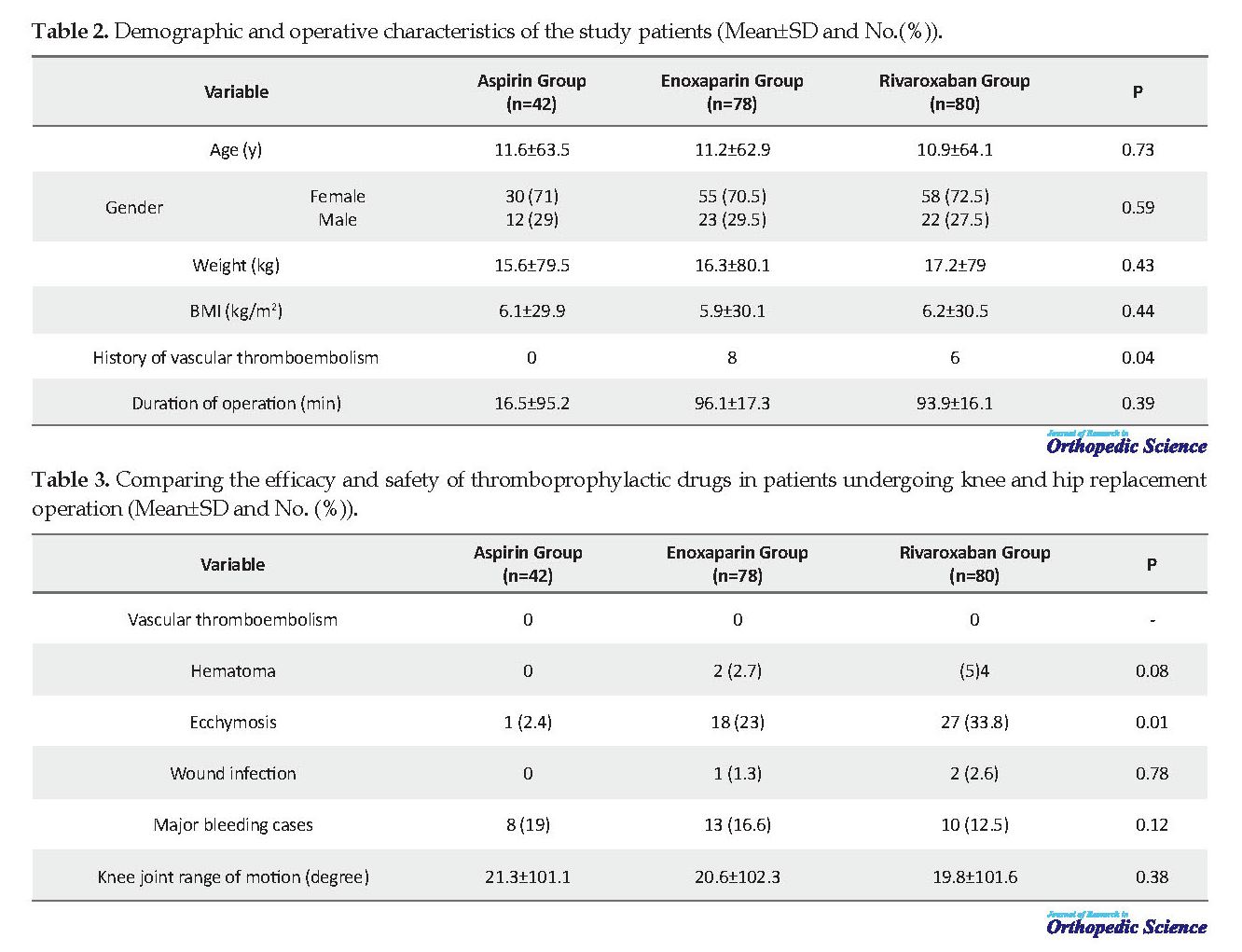
The Mean±SD age of patients in the three groups of aspirin, enoxaparin, rivaroxaban were 63.5±11.6, 62.9±11.2 and 64.1±10.9 years, respectively. In the aspirin group, 29% and 71% were men and women, in the enoxaparin group, 29.5% and 70.5%, and in the rivaroxaban group, 27.5% and 72.5%, respectively. The Mean±SD weight of the patients in the aspirin, enoxaparin, rivaroxaban groups were 79.5±15.6, 80.1±16.3, and 79±17.2 kg, respectively. Eight patients in the enoxaparin group and 6 in the rivaroxaban group had a history of thromboembolism. The Mean±SD of the model of operation in the three groups was 95.2±16.5, 96.1±17.3 and 93.9±16.1, respectively. There was no significant difference in demographic and surgical characteristics of the study groups (P>0.05). But the history of vascular thromboembolism was significantly higher in the enoxaparin and the rivaroxaban group than in the aspirin group (P=0.04) (Table 2).
In 19 cases, patients underwent Doppler ultrasound because of swelling and suspicion of vascular thromboembolism, but the vascular thromboembolism was dismissed in all cases. Therefore, no case of vascular thromboembolism was observed in any of the study groups. The highest number of ecchymosis was seen in the rivaroxaban group with 27 patients and then in the enoxaparin and aspirin groups with 18 and 1 patient(s), respectively (P=0.01). Two patients in the enoxaparin and 4 in the rivaroxaban group developed a hematoma. Overall, three cases had wound infection, two in the rivaroxaban group, one in the enoxaparin group and none in the aspirin group. Major bleeding cases were 19%, 16.6%, and 12.5%, respectively. There was no significant difference in the number of cases of vascular thromboembolism, major bleeding, hematoma, and wound infection (P>0.05).
The efficacy of the two drugs rivaroxaban and enoxaparin was compared separately. There were no significant differences between the efficacy and safety of rivaroxaban and enoxaparin. However, the number of ecchymosis cases in the rivaroxaban group was significantly higher than that in the enoxaparin group (P=0.06). However, this difference was not statistically significant. To further investigate the efficacy and safety of each drug for knee and hip joint operation, they were evaluated separately.
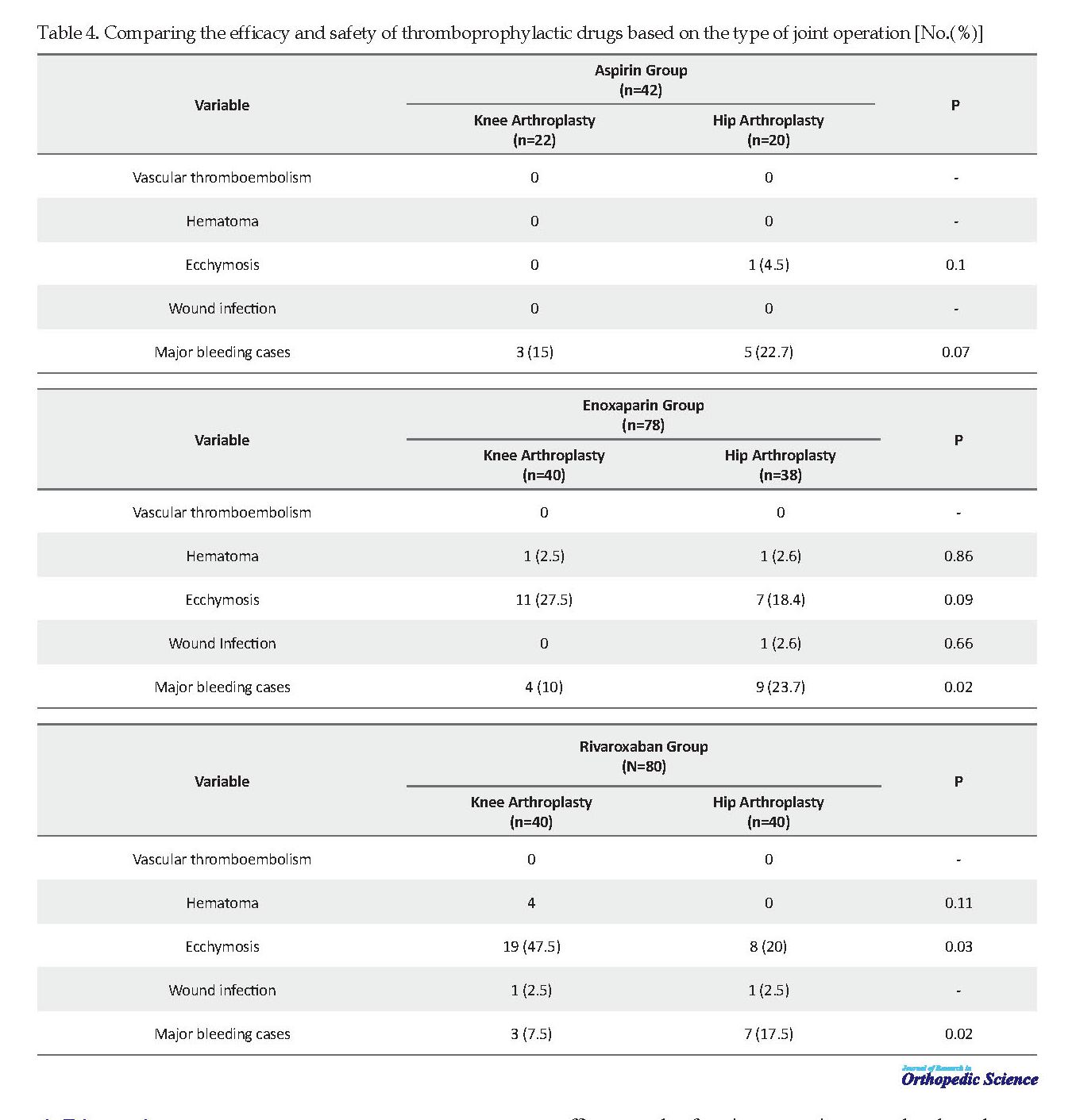
There was no significant difference between the safety and efficacy of aspirin in the two groups of knee replacement operation (P>0.05). In the enoxaparin-treated group, there was no significant difference in the number of ecchymosis cases between the knee and hip replacement groups (P=0.09). However, the number of major bleeding cases was significantly higher in the hip replacement group (P=0.02). There was no significant difference between the patients in the hip and knee joint replacement group in terms of safety and efficacy. In the rivaroxaban recipient group, the number of ecchymosis cases was significantly higher in the knee replacement group (P=0.03). The number of major bleedings was considerably higher in the hip group compared to the knee group (P=0.02). There was no significant difference between the patients in the hip and knee group in terms of safety and efficacy (Table 3 & 4).
4. Discussion
A total of 200 patients were studied in three groups of aspirin (42 patients), enoxaparin (78 patients), and rivaroxaban (80 patients). The study population consisted of 105 cases of total knee arthroplasty and 95 cases of total hip arthroplasty. No cases of vascular thromboembolism were observed in any patient in our study. The number of ecchymosis cases in the aspirin group was significantly lower than that in the enoxaparin and rivaroxaban groups. No significant differences were observed in the aspirin group compared with the other two groups. Accordingly, our study also showed that aspirin has high efficacy and safety in preventing vascular thromboembolism following arthroplasty in patients with low risk of vascular thromboembolism.
No differences in bleeding cases indicate that the safety of rivaroxaban and enoxaparin is similar in the prevention of vascular thromboembolism following arthroplasty. Therefore rivaroxaban may be a suitable alternative to enoxaparin. However, aspirin use is not recommended for patients with a high risk of vascular thromboembolism, such as patients with a history of vascular thromboembolism, so the use of more potent thromboprophylactic drugs such as enoxaparin and rivaroxaban is indicated. Although the use of oral thromboprophylactic drugs such as rivaroxaban is preferable to thromboprophylactic injectable medicines such as enoxaparin.
There is insufficient evidence on the efficacy and safety of these drugs. Despite numerous studies in this field, there is still no agreement on the thromboprophylactic drug used for patients with a high risk of thromboembolism. In this study, we evaluated the efficacy and safety of enoxaparin and rivaroxaban in thromboprophylaxis following arthroplasty.
The efficacy and safety of both enoxaparin and rivaroxaban in the prevention of vascular thromboembolism following arthroplasty have also been examined in other studies. In one of the most comprehensive studies, Eriksson et al. researched the efficacy and safety of both enoxaparin and rivaroxaban in patients undergoing hip replacement operation in a double-blind, randomized clinical trial. Patients in the rivaroxaban group received 10 mg of rivaroxaban daily per oral, which was the first dose received after the operation. Patients in the enoxaparin group received 40 mg of enoxaparin daily subcutaneously, the first dose being administered the evening before operation.
The rivaroxaban group received a placebo injection, and the enoxaparin group received a placebo tablet. Vascular thromboembolism was used to evaluate the efficacy and major bleeding to assess the safety. Vascular thromboembolism occurred in 4 of 1686 patients receiving rivaroxaban, and in 33 of 1678 patients receiving enoxaparin. Accordingly, the use of rivaroxaban reduces the risk of vascular thromboembolism after hip replacement by 1.7%. Major bleeding occurred in 6 of the 2209 patients receiving rivaroxaban and in 2 of the 2224 patients receiving enoxaparin. But the difference was not significant. Untreated hemorrhage (including hematoma, ecchymosis, etc.) occurred in 1.5% of patients in the rivaroxaban group and 1.7% in the enoxaparin group. This difference was not statistically significant. They concluded that the safety of both enoxaparin and rivaroxaban in thromboprophylaxis was similar in hip replacement. Still, the efficacy of rivaroxaban was significantly higher, and therefore its use is more justified in these patients [5].
In another study, Lassen et al. examined the efficacy and safety of the enoxaparin and rivaroxaban drugs in knee arthroplasty for thromboprophylaxis in a double-blind, randomized clinical trial. Patients received either oral rivaroxaban with a dose of 10 mg daily (starting 6-8 hours postoperatively) or enoxaparin with a dose of 40 mg daily (beginning 12 hours preoperatively). Nine out of 908 patients received rivaroxaban, and 24 out of 928 patients received vascular thromboembolic enoxaparin. Accordingly, the use of rivaroxaban was associated with a 1.6% reduction in the risk of vascular thromboembolism following knee replacement.
Major bleeding occurred in 0.6% of patients in the rivaroxaban group and 0.5% in the enoxaparin group. Untreated hemorrhage (including hematoma, ecchymosis, etc.) occurred in 3.3% of the rivaroxaban group and 2.7% of the enoxaparin group. This difference was not statistically significant. They concluded that rivaroxaban was more effective than enoxaparin after knee arthroplasty in vascular prophylaxis, whereas the safety of the two drugs (major and unintentional bleeding cases) was similar [6].
Although most studies have not shown a significant difference in the side effects of rivaroxaban and heparins with low molecular weight, the factors that directly inhibit Xa are potentially associated with a higher risk of bleeding than heparins with low molecular weight [3]. Besides, the results of some other studies showed that the risk of bleeding after enoxaparin was higher than that of rivaroxaban [7, 8]. In Li et al. study, 15.7% in the rivaroxaban group and 3.6% in the enoxaparin group showed a statistically significant difference [9]. In Ricket et al. study, patients undergoing hip or knee arthroplasty with thromboembolism prophylaxis were evaluated, with 6.8% bleeding in the rivaroxaban group and 2.2% in the enoxaparin group that was a statistically significant difference [8].
In Ageno et al. study, 5142 patients were studied, with 1.4% in the rivaroxaban group and 2.3% in the enoxaparin group having thromboembolism, which showed a statistically significant difference. Also, 0.8% in the rivaroxaban group and 1.2% in the enoxaparin group experienced bleeding, which was not significantly different [10]. Also, some studies reported different efficacy for rivaroxaban compared with enoxaparin. In Kwong et al. review study, it was found that the effect of rivaroxaban was higher in patients undergoing hip and knee replacement operation compared with enoxaparin in the prophylaxis of thromboembolism [11].
In Kakkar et al. study, the use of rivaroxaban for 35 days was compared with enoxaparin for 10-14 days after hip replacement operation. According to the results of this study, rivaroxaban was significantly more effective in reducing vascular thromboembolism than enoxaparin. Besides, there was no significant difference in bleeding symptoms between the two study groups [12]. In Levitan et al. study, 442 patients underwent hip or knee arthroplasty with thromboembolism prophylaxis. They found that the efficacy of rivaroxaban was higher than that of enoxaparin, and its side effects were lower [13]. In a meta-analysis done by Cao et al., the efficacy of rivaroxaban was found to be higher than that of enoxaparin with lower thromboembolism and mortality. Still, their side effects were similar [12].
Turpie et al., in phase III clinical trial, compared the efficacy and safety of enoxaparin and rivaroxaban in the prevention of vascular thromboembolism following knee replacement operation. Patients received either oral rivaroxaban with a dose of 10 mg daily (starting 6-8 hours postoperatively) or enoxaparin with a dose of 30 mg daily (starting 12-24 hours preoperatively). Complications related to efficacy, including deep thrombosis, non-fatal pulmonary embolism, and death occurred in 67 (6.7%) of 965 patients receiving rivaroxaban and 97 (10.1%) of 959 patients receiving enoxaparin. Accordingly, the use of rivaroxaban was associated with a 3.2% reduction in the risk of side effects. Major bleeding occurred in 0.7% of patients receiving rivaroxaban and 0.3% of patients receiving enoxaparin. This difference was not statistically significant. Based on these results, rivaroxaban is more effective than enoxaparin and, therefore, preferable to enoxaparin [14].
Zou et al. investigated the safety and efficacy of aspirin, rivaroxaban, and enoxaparin in 324 patients with knee osteoarthritis. Twelve hours after the operation, the first group received rivaroxaban with a dose of 10 mg, the second group received IU aXa 4000 enoxaparin, and the third group received aspirin with a dose of 100 mg. The drugs were taken daily (all groups for 14 days). The incidence of DVT in the rivaroxaban group was significantly lower than the other two groups (P=0.017). However, the number of ecchymosis cases was also considerably higher in the rivaroxaban group than in the aspirin group (P=0.039). More ecchymosis was seen following rivaroxaban use compared with the enoxaparin in Xie et al. study [15].
Although most studies indicate the superiority of rivaroxaban over enoxaparin [9, 16, 17], no difference was seen regarding the efficacy of rivaroxaban and enoxaparin in our study. In this regard, no cases of vascular thromboembolism occurred in any of the enoxaparin and rivaroxaban groups in our study. This disagreement may be due to the low number of patients in our study compared to other studies. While our study was performed on 158 patients, most other studies have involved far more patients (thousands of patients). Besides, in most other studies, Doppler or venography ultrasound has been performed to diagnose vascular thromboembolism in all patients. However, in the present study, Doppler ultrasound was performed only for patients with clinical suspicion of vascular thromboembolism [17].
In most previous studies, no significant differences were observed between the safety of rivaroxaban and enoxaparin [17]. According to the results of this study, there was no significant difference between the enoxaparin and rivaroxaban groups. However, the number of ecchymosis cases was significantly higher in the rivaroxaban group (although this difference was not significant).
Another point to note is the significant number of ecchymosis in the enoxaparin and rivaroxaban groups compared to the aspirin group. According to our study, ecchymosis around the wound can be one of the common side effects of enoxaparin and rivaroxaban. One hypothesis is that ecchymosis or hematoma around the wound may restrict the range of motion of the patient’s knee and ultimately lead to knee stiffness [18]. If this hypothesis is true, the possibility of ecchymosis or hematoma around the wound should also be considered in the choice of thromboprophylactic drug. In our study, there was no significant difference among the three groups of aspirin, enoxaparin, and rivaroxaban in the knee range of motion. Therefore, higher ecchymosis following enoxaparin or rivaroxaban administration will not result in the restriction of knee range of motion and, consequently, knee stiffness.
Gastrointestinal complications are also one of the issues after using rivaroxaban and enoxaparin. In Lassen et al. study, gastrointestinal complications were seen in 12% of rivaroxaban patients and 13% of enoxaparin patients [17]. In Turpie et al. study, a case of fatal gastrointestinal bleeding was observed in one of the patients in the rivaroxaban group. No cases of gastrointestinal complications were seen in any of the patients in our study group [18]. Skin complications have also been reported as one of the rare events following the use of rivaroxaban and enoxaparin. In the ROCKET-AF study, toxic skin eruption was observed in 0.03% of patients. Besides, cutaneous vasculitis and exfoliative rash were also seen in 0.01% of patients [19]. Hypersensitivity to enoxaparin has also been reported in some cases [20, 21]. However, no skin complications were seen in any of the study groups.
5. Conclusion
According to the results of the present study, despite the higher number of ecchymosis following rivaroxaban use, its use is still recommended instead of enoxaparin, because rivaroxaban is an oral drug and its use decreases hospital stay duration and does not involve ongoing surveillance. It will also reduce the economic burden on the individual and the health care system.
Study recommendations
The efficacy and safety of rivaroxaban and enoxaparin are comparable. However, the number of ecchymosis around the wound appears to be more following rivaroxaban administration. Al in all, rivaroxaban is orally administered and will be less costly to the patient and health system and does not require continuous monitoring, so its use as a thromboprophylactic drug following hip and knee arthroplasty operation is preferred. It is recommended that this drug be used as a drug of choice for the prevention of vascular thromboembolism after hip and knee arthroplasty.
Study limitations
The low number of patients compared to other studies may affect the statistical analysis power of the study. Therefore, future studies with more patients are needed to confirm the results of this study. The results are likely to be underestimated, given that the Shafa Yahyaian Healing Center specializes in only one field. Patients with lower risk factors underwent surgery at the center. Thus, conducting similar studies in multidisciplinary centers can support the results of this study. Since all patients did not undergo a similar surgical approach, the number of bleeding cases may be affected by the surgical procedure. Therefore, similar studies on the populations who have undergone a similar surgical approach may also be considered to support the results of this study.
Ethical Considerations
Compliance with ethical guidelines
The study began after the approval of Iran University of Medical Sciences and the Ethics Committee on Biomedical Research (Code: IR.IUMS.FMD.REC.1395.347) and RCT (Code: IRCT20191121031003N1). Also, written consent was obtained from all patients to use the information in their case files.
Funding
All the costs of the study, including Doppler ultrasound and heart scan tests, as needed, as well as the provision of rivaroxaban medication, were paid from the project funding, and no additional costs were imposed on the patient.
Authors' contributions
Conceptualization: Abolfazl Bagherifard, Kaveh Gharanizadeh; Methodology: Abolfazl Bagherifard , Kaveh Gharanizadeh, Mostafa Salehpour; Investigation: Mostafa Salehpour, Hamed Jafarpour; Writing – original draft: Mostafa Salehpour, Mani Mahmoudi; Writing – review & editing: Mani Mahmoudi; Resources: Mani Mahmoudi, Hamed Jafarpour; Supervision: Abolfazl Bagherifard, Kaveh Gharanizadeh.
Conflict of interest
The authors declared no conflict of interests.
References
White RH, Henderson MC. Risk factors for venous thromboembolism after total hip and knee replacement surgery. Curr Opin Pulm Med. 2002; 8(5):365-71. [DOI:10.1097/00063198-200209000-00004] [PMID]
Schindler O, Dalziel R. Post-thrombotic syndrome after total hip or knee arthroplasty: Incidence in patients with asymptomatic deep venous thrombosis. J Orthop Surg (Hong Kong). 2005; 13(2):113-9. [DOI:10.1177/230949900501300202] [PMID]
Budhiparama NC, Abdel MP, Ifran NN, Parratte S. Venous thromboembolism (VTE) prophylaxis for hip and knee arthroplasty: Changing trends. Curr Rev Musculoskelet Med. 2014; 7(2):108-16. [DOI:10.1007/s12178-014-9207-1] [PMID] [PMCID]
Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. The Lancet. 2007; 370(9597):1508-19. [DOI:10.1016/S0140-6736(07)60457-7]
Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008; 358(26):2765-75. [DOI:10.1056/NEJMoa0800374] [PMID]
Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008; 358(26):2776-86. [DOI:10.1056/NEJMoa076016] [PMID]
Huisman MV, Quinlan DJ, Dahl OE, Schulman S. Enoxaparin versus dabigatran or rivaroxaban for thromboprophylaxis after hip or knee arthroplasty: Results of separate pooled analyses of phase III multicenter randomized trials. Circ Cardiovasc Qual Outcomes. 2010; 3(6):652-60. [DOI:10.1161/CIRCOUTCOMES.110.957712] [PMID]
Ricket AL, Stewart DW, Wood RC, Cornett L, Odle B, Cluck D, et al. Comparison of postoperative bleeding in total hip and knee arthroplasty patients receiving rivaroxaban or enoxaparin. Ann Pharmacother. 2016; 50(4):270-5. [DOI:10.1177/1060028015626435] [PMID]
Li J, Jing J, Zhou Y, Yao Y, Zhan J. [Comparison of rivaroxaban and enoxaparin on blood loss after total knee arthroplasty (Persian)]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014; 28(1):26-9.
Ageno W, Mantovani LG, Haas S, Kreutz R, Monje D, Schneider J, et al. Safety and effectiveness of oral rivaroxaban versus standard anticoagulation for the treatment of symptomatic deep-vein thrombosis (XALIA): An international, prospective, non-interventional study. Lancet Haematol. 2016; 3(1):e12-21. [DOI:10.1016/S2352-3026(15)00257-4]
Kwong LM. Comparative safety and efficacy of antithrombotics in the management of venous thromboembolism after knee or hip replacement surgery: Focus on rivaroxaban. Clin Pharmacol. 2013; 5:143-8. [DOI:10.2147/CPAA.S26647] [PMID] [PMCID]
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: A double-blind, randomised controlled trial. Lancet. 2008; 372(9632):31-9. [DOI:10.1016/S0140-6736(08)60880-6]
Levitan B, Yuan Z, Turpie AG, Friedman RJ, Homering M, Berlin JA, et al. Benefit-risk assessment of rivaroxaban versus enoxaparin for the prevention of venous thromboembolism after total hip or knee arthroplasty. Vasc Health Risk Manag. 2014; 10:157-67. [DOI:10.2147/VHRM.S54714] [PMID] [PMCID]
Turpie AG, Lassen MR, Eriksson BI, Gent M, Berkowitz SD, Misselwitz F, et al. Rivaroxaban for the prevention of venous thromboembolism after hip or knee arthroplasty. Thromb Haemost. 2011; 106(03):444-53. [DOI:10.1160/TH10-09-0601] [PMID]
Zou Y, Tian S, Wang Y, Sun K. Administering aspirin, rivaroxaban and low-molecular-weight heparin to prevent deep venous thrombosis after total knee arthroplasty. Blood Coagul Fibrinolysis. 2014; 25(7):660-4. [DOI:10.1097/MBC.0000000000000121] [PMID]
Turpie AG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): A randomised trial. Lancet. 2009; 373(9676):1673-80. [DOI:10.1016/S0140-6736(09)60734-0]
Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P, et al. Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): A randomized double-blind trial. Lancet. 2010; 375(9717):807-15. [DOI:10.1016/S0140-6736(09)62125-5]
Kahlenberg CA, Richardson SS, Schairer WW, Sculco PK. Type of anticoagulant used after total knee arthroplasty affects the rate of knee manipulation for postoperative stiffness. J Bone Joint Surg Am. 2018; 100(16):1366-72. [DOI:10.2106/JBJS.17.01110] [PMID]
Hofmeier KS. Hypersensitivity reactions to modern antiplatelet and anticoagulant drugs. Allergo J Int. 2015; 24(2):58-66. [DOI:10.1007/s40629-015-0048-2] [PMID] [PMCID]
Antony AM. Hypersensitivity skin reaction to enoxapari. Aust Prescr. 2011; 34:152. [DOI:10.18773/austprescr.2011.077]
Ronceray S, Dinulescu M, Le Gall F, Polard E, Alain Dupuy A, Adamskia H. Enoxaparin-induced DRESS syndrome. Case Rep Dermatol. 2012; 4(3):233-7. [DOI:10.1159/000345096] [PMID] [PMCID]
4. Discussion
A total of 200 patients were studied in three groups of aspirin (42 patients), enoxaparin (78 patients), and rivaroxaban (80 patients). The study population consisted of 105 cases of total knee arthroplasty and 95 cases of total hip arthroplasty. No cases of vascular thromboembolism were observed in any patient in our study. The number of ecchymosis cases in the aspirin group was significantly lower than that in the enoxaparin and rivaroxaban groups. No significant differences were observed in the aspirin group compared with the other two groups. Accordingly, our study also showed that aspirin has high efficacy and safety in preventing vascular thromboembolism following arthroplasty in patients with low risk of vascular thromboembolism.
No differences in bleeding cases indicate that the safety of rivaroxaban and enoxaparin is similar in the prevention of vascular thromboembolism following arthroplasty. Therefore rivaroxaban may be a suitable alternative to enoxaparin. However, aspirin use is not recommended for patients with a high risk of vascular thromboembolism, such as patients with a history of vascular thromboembolism, so the use of more potent thromboprophylactic drugs such as enoxaparin and rivaroxaban is indicated. Although the use of oral thromboprophylactic drugs such as rivaroxaban is preferable to thromboprophylactic injectable medicines such as enoxaparin.
There is insufficient evidence on the efficacy and safety of these drugs. Despite numerous studies in this field, there is still no agreement on the thromboprophylactic drug used for patients with a high risk of thromboembolism. In this study, we evaluated the efficacy and safety of enoxaparin and rivaroxaban in thromboprophylaxis following arthroplasty.
The efficacy and safety of both enoxaparin and rivaroxaban in the prevention of vascular thromboembolism following arthroplasty have also been examined in other studies. In one of the most comprehensive studies, Eriksson et al. researched the efficacy and safety of both enoxaparin and rivaroxaban in patients undergoing hip replacement operation in a double-blind, randomized clinical trial. Patients in the rivaroxaban group received 10 mg of rivaroxaban daily per oral, which was the first dose received after the operation. Patients in the enoxaparin group received 40 mg of enoxaparin daily subcutaneously, the first dose being administered the evening before operation.
The rivaroxaban group received a placebo injection, and the enoxaparin group received a placebo tablet. Vascular thromboembolism was used to evaluate the efficacy and major bleeding to assess the safety. Vascular thromboembolism occurred in 4 of 1686 patients receiving rivaroxaban, and in 33 of 1678 patients receiving enoxaparin. Accordingly, the use of rivaroxaban reduces the risk of vascular thromboembolism after hip replacement by 1.7%. Major bleeding occurred in 6 of the 2209 patients receiving rivaroxaban and in 2 of the 2224 patients receiving enoxaparin. But the difference was not significant. Untreated hemorrhage (including hematoma, ecchymosis, etc.) occurred in 1.5% of patients in the rivaroxaban group and 1.7% in the enoxaparin group. This difference was not statistically significant. They concluded that the safety of both enoxaparin and rivaroxaban in thromboprophylaxis was similar in hip replacement. Still, the efficacy of rivaroxaban was significantly higher, and therefore its use is more justified in these patients [5].
In another study, Lassen et al. examined the efficacy and safety of the enoxaparin and rivaroxaban drugs in knee arthroplasty for thromboprophylaxis in a double-blind, randomized clinical trial. Patients received either oral rivaroxaban with a dose of 10 mg daily (starting 6-8 hours postoperatively) or enoxaparin with a dose of 40 mg daily (beginning 12 hours preoperatively). Nine out of 908 patients received rivaroxaban, and 24 out of 928 patients received vascular thromboembolic enoxaparin. Accordingly, the use of rivaroxaban was associated with a 1.6% reduction in the risk of vascular thromboembolism following knee replacement.
Major bleeding occurred in 0.6% of patients in the rivaroxaban group and 0.5% in the enoxaparin group. Untreated hemorrhage (including hematoma, ecchymosis, etc.) occurred in 3.3% of the rivaroxaban group and 2.7% of the enoxaparin group. This difference was not statistically significant. They concluded that rivaroxaban was more effective than enoxaparin after knee arthroplasty in vascular prophylaxis, whereas the safety of the two drugs (major and unintentional bleeding cases) was similar [6].
Although most studies have not shown a significant difference in the side effects of rivaroxaban and heparins with low molecular weight, the factors that directly inhibit Xa are potentially associated with a higher risk of bleeding than heparins with low molecular weight [3]. Besides, the results of some other studies showed that the risk of bleeding after enoxaparin was higher than that of rivaroxaban [7, 8]. In Li et al. study, 15.7% in the rivaroxaban group and 3.6% in the enoxaparin group showed a statistically significant difference [9]. In Ricket et al. study, patients undergoing hip or knee arthroplasty with thromboembolism prophylaxis were evaluated, with 6.8% bleeding in the rivaroxaban group and 2.2% in the enoxaparin group that was a statistically significant difference [8].
In Ageno et al. study, 5142 patients were studied, with 1.4% in the rivaroxaban group and 2.3% in the enoxaparin group having thromboembolism, which showed a statistically significant difference. Also, 0.8% in the rivaroxaban group and 1.2% in the enoxaparin group experienced bleeding, which was not significantly different [10]. Also, some studies reported different efficacy for rivaroxaban compared with enoxaparin. In Kwong et al. review study, it was found that the effect of rivaroxaban was higher in patients undergoing hip and knee replacement operation compared with enoxaparin in the prophylaxis of thromboembolism [11].
In Kakkar et al. study, the use of rivaroxaban for 35 days was compared with enoxaparin for 10-14 days after hip replacement operation. According to the results of this study, rivaroxaban was significantly more effective in reducing vascular thromboembolism than enoxaparin. Besides, there was no significant difference in bleeding symptoms between the two study groups [12]. In Levitan et al. study, 442 patients underwent hip or knee arthroplasty with thromboembolism prophylaxis. They found that the efficacy of rivaroxaban was higher than that of enoxaparin, and its side effects were lower [13]. In a meta-analysis done by Cao et al., the efficacy of rivaroxaban was found to be higher than that of enoxaparin with lower thromboembolism and mortality. Still, their side effects were similar [12].
Turpie et al., in phase III clinical trial, compared the efficacy and safety of enoxaparin and rivaroxaban in the prevention of vascular thromboembolism following knee replacement operation. Patients received either oral rivaroxaban with a dose of 10 mg daily (starting 6-8 hours postoperatively) or enoxaparin with a dose of 30 mg daily (starting 12-24 hours preoperatively). Complications related to efficacy, including deep thrombosis, non-fatal pulmonary embolism, and death occurred in 67 (6.7%) of 965 patients receiving rivaroxaban and 97 (10.1%) of 959 patients receiving enoxaparin. Accordingly, the use of rivaroxaban was associated with a 3.2% reduction in the risk of side effects. Major bleeding occurred in 0.7% of patients receiving rivaroxaban and 0.3% of patients receiving enoxaparin. This difference was not statistically significant. Based on these results, rivaroxaban is more effective than enoxaparin and, therefore, preferable to enoxaparin [14].
Zou et al. investigated the safety and efficacy of aspirin, rivaroxaban, and enoxaparin in 324 patients with knee osteoarthritis. Twelve hours after the operation, the first group received rivaroxaban with a dose of 10 mg, the second group received IU aXa 4000 enoxaparin, and the third group received aspirin with a dose of 100 mg. The drugs were taken daily (all groups for 14 days). The incidence of DVT in the rivaroxaban group was significantly lower than the other two groups (P=0.017). However, the number of ecchymosis cases was also considerably higher in the rivaroxaban group than in the aspirin group (P=0.039). More ecchymosis was seen following rivaroxaban use compared with the enoxaparin in Xie et al. study [15].
Although most studies indicate the superiority of rivaroxaban over enoxaparin [9, 16, 17], no difference was seen regarding the efficacy of rivaroxaban and enoxaparin in our study. In this regard, no cases of vascular thromboembolism occurred in any of the enoxaparin and rivaroxaban groups in our study. This disagreement may be due to the low number of patients in our study compared to other studies. While our study was performed on 158 patients, most other studies have involved far more patients (thousands of patients). Besides, in most other studies, Doppler or venography ultrasound has been performed to diagnose vascular thromboembolism in all patients. However, in the present study, Doppler ultrasound was performed only for patients with clinical suspicion of vascular thromboembolism [17].
In most previous studies, no significant differences were observed between the safety of rivaroxaban and enoxaparin [17]. According to the results of this study, there was no significant difference between the enoxaparin and rivaroxaban groups. However, the number of ecchymosis cases was significantly higher in the rivaroxaban group (although this difference was not significant).
Another point to note is the significant number of ecchymosis in the enoxaparin and rivaroxaban groups compared to the aspirin group. According to our study, ecchymosis around the wound can be one of the common side effects of enoxaparin and rivaroxaban. One hypothesis is that ecchymosis or hematoma around the wound may restrict the range of motion of the patient’s knee and ultimately lead to knee stiffness [18]. If this hypothesis is true, the possibility of ecchymosis or hematoma around the wound should also be considered in the choice of thromboprophylactic drug. In our study, there was no significant difference among the three groups of aspirin, enoxaparin, and rivaroxaban in the knee range of motion. Therefore, higher ecchymosis following enoxaparin or rivaroxaban administration will not result in the restriction of knee range of motion and, consequently, knee stiffness.
Gastrointestinal complications are also one of the issues after using rivaroxaban and enoxaparin. In Lassen et al. study, gastrointestinal complications were seen in 12% of rivaroxaban patients and 13% of enoxaparin patients [17]. In Turpie et al. study, a case of fatal gastrointestinal bleeding was observed in one of the patients in the rivaroxaban group. No cases of gastrointestinal complications were seen in any of the patients in our study group [18]. Skin complications have also been reported as one of the rare events following the use of rivaroxaban and enoxaparin. In the ROCKET-AF study, toxic skin eruption was observed in 0.03% of patients. Besides, cutaneous vasculitis and exfoliative rash were also seen in 0.01% of patients [19]. Hypersensitivity to enoxaparin has also been reported in some cases [20, 21]. However, no skin complications were seen in any of the study groups.
5. Conclusion
According to the results of the present study, despite the higher number of ecchymosis following rivaroxaban use, its use is still recommended instead of enoxaparin, because rivaroxaban is an oral drug and its use decreases hospital stay duration and does not involve ongoing surveillance. It will also reduce the economic burden on the individual and the health care system.
Study recommendations
The efficacy and safety of rivaroxaban and enoxaparin are comparable. However, the number of ecchymosis around the wound appears to be more following rivaroxaban administration. Al in all, rivaroxaban is orally administered and will be less costly to the patient and health system and does not require continuous monitoring, so its use as a thromboprophylactic drug following hip and knee arthroplasty operation is preferred. It is recommended that this drug be used as a drug of choice for the prevention of vascular thromboembolism after hip and knee arthroplasty.
Study limitations
The low number of patients compared to other studies may affect the statistical analysis power of the study. Therefore, future studies with more patients are needed to confirm the results of this study. The results are likely to be underestimated, given that the Shafa Yahyaian Healing Center specializes in only one field. Patients with lower risk factors underwent surgery at the center. Thus, conducting similar studies in multidisciplinary centers can support the results of this study. Since all patients did not undergo a similar surgical approach, the number of bleeding cases may be affected by the surgical procedure. Therefore, similar studies on the populations who have undergone a similar surgical approach may also be considered to support the results of this study.
Ethical Considerations
Compliance with ethical guidelines
The study began after the approval of Iran University of Medical Sciences and the Ethics Committee on Biomedical Research (Code: IR.IUMS.FMD.REC.1395.347) and RCT (Code: IRCT20191121031003N1). Also, written consent was obtained from all patients to use the information in their case files.
Funding
All the costs of the study, including Doppler ultrasound and heart scan tests, as needed, as well as the provision of rivaroxaban medication, were paid from the project funding, and no additional costs were imposed on the patient.
Authors' contributions
Conceptualization: Abolfazl Bagherifard, Kaveh Gharanizadeh; Methodology: Abolfazl Bagherifard , Kaveh Gharanizadeh, Mostafa Salehpour; Investigation: Mostafa Salehpour, Hamed Jafarpour; Writing – original draft: Mostafa Salehpour, Mani Mahmoudi; Writing – review & editing: Mani Mahmoudi; Resources: Mani Mahmoudi, Hamed Jafarpour; Supervision: Abolfazl Bagherifard, Kaveh Gharanizadeh.
Conflict of interest
The authors declared no conflict of interests.
References
White RH, Henderson MC. Risk factors for venous thromboembolism after total hip and knee replacement surgery. Curr Opin Pulm Med. 2002; 8(5):365-71. [DOI:10.1097/00063198-200209000-00004] [PMID]
Schindler O, Dalziel R. Post-thrombotic syndrome after total hip or knee arthroplasty: Incidence in patients with asymptomatic deep venous thrombosis. J Orthop Surg (Hong Kong). 2005; 13(2):113-9. [DOI:10.1177/230949900501300202] [PMID]
Budhiparama NC, Abdel MP, Ifran NN, Parratte S. Venous thromboembolism (VTE) prophylaxis for hip and knee arthroplasty: Changing trends. Curr Rev Musculoskelet Med. 2014; 7(2):108-16. [DOI:10.1007/s12178-014-9207-1] [PMID] [PMCID]
Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. The Lancet. 2007; 370(9597):1508-19. [DOI:10.1016/S0140-6736(07)60457-7]
Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008; 358(26):2765-75. [DOI:10.1056/NEJMoa0800374] [PMID]
Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008; 358(26):2776-86. [DOI:10.1056/NEJMoa076016] [PMID]
Huisman MV, Quinlan DJ, Dahl OE, Schulman S. Enoxaparin versus dabigatran or rivaroxaban for thromboprophylaxis after hip or knee arthroplasty: Results of separate pooled analyses of phase III multicenter randomized trials. Circ Cardiovasc Qual Outcomes. 2010; 3(6):652-60. [DOI:10.1161/CIRCOUTCOMES.110.957712] [PMID]
Ricket AL, Stewart DW, Wood RC, Cornett L, Odle B, Cluck D, et al. Comparison of postoperative bleeding in total hip and knee arthroplasty patients receiving rivaroxaban or enoxaparin. Ann Pharmacother. 2016; 50(4):270-5. [DOI:10.1177/1060028015626435] [PMID]
Li J, Jing J, Zhou Y, Yao Y, Zhan J. [Comparison of rivaroxaban and enoxaparin on blood loss after total knee arthroplasty (Persian)]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014; 28(1):26-9.
Ageno W, Mantovani LG, Haas S, Kreutz R, Monje D, Schneider J, et al. Safety and effectiveness of oral rivaroxaban versus standard anticoagulation for the treatment of symptomatic deep-vein thrombosis (XALIA): An international, prospective, non-interventional study. Lancet Haematol. 2016; 3(1):e12-21. [DOI:10.1016/S2352-3026(15)00257-4]
Kwong LM. Comparative safety and efficacy of antithrombotics in the management of venous thromboembolism after knee or hip replacement surgery: Focus on rivaroxaban. Clin Pharmacol. 2013; 5:143-8. [DOI:10.2147/CPAA.S26647] [PMID] [PMCID]
Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: A double-blind, randomised controlled trial. Lancet. 2008; 372(9632):31-9. [DOI:10.1016/S0140-6736(08)60880-6]
Levitan B, Yuan Z, Turpie AG, Friedman RJ, Homering M, Berlin JA, et al. Benefit-risk assessment of rivaroxaban versus enoxaparin for the prevention of venous thromboembolism after total hip or knee arthroplasty. Vasc Health Risk Manag. 2014; 10:157-67. [DOI:10.2147/VHRM.S54714] [PMID] [PMCID]
Turpie AG, Lassen MR, Eriksson BI, Gent M, Berkowitz SD, Misselwitz F, et al. Rivaroxaban for the prevention of venous thromboembolism after hip or knee arthroplasty. Thromb Haemost. 2011; 106(03):444-53. [DOI:10.1160/TH10-09-0601] [PMID]
Zou Y, Tian S, Wang Y, Sun K. Administering aspirin, rivaroxaban and low-molecular-weight heparin to prevent deep venous thrombosis after total knee arthroplasty. Blood Coagul Fibrinolysis. 2014; 25(7):660-4. [DOI:10.1097/MBC.0000000000000121] [PMID]
Turpie AG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): A randomised trial. Lancet. 2009; 373(9676):1673-80. [DOI:10.1016/S0140-6736(09)60734-0]
Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P, et al. Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): A randomized double-blind trial. Lancet. 2010; 375(9717):807-15. [DOI:10.1016/S0140-6736(09)62125-5]
Kahlenberg CA, Richardson SS, Schairer WW, Sculco PK. Type of anticoagulant used after total knee arthroplasty affects the rate of knee manipulation for postoperative stiffness. J Bone Joint Surg Am. 2018; 100(16):1366-72. [DOI:10.2106/JBJS.17.01110] [PMID]
Hofmeier KS. Hypersensitivity reactions to modern antiplatelet and anticoagulant drugs. Allergo J Int. 2015; 24(2):58-66. [DOI:10.1007/s40629-015-0048-2] [PMID] [PMCID]
Antony AM. Hypersensitivity skin reaction to enoxapari. Aust Prescr. 2011; 34:152. [DOI:10.18773/austprescr.2011.077]
Ronceray S, Dinulescu M, Le Gall F, Polard E, Alain Dupuy A, Adamskia H. Enoxaparin-induced DRESS syndrome. Case Rep Dermatol. 2012; 4(3):233-7. [DOI:10.1159/000345096] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Knee surgery
Received: 2019/09/15 | Accepted: 2020/01/5 | Published: 2020/02/1
Received: 2019/09/15 | Accepted: 2020/01/5 | Published: 2020/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |