Volume 6, Issue 4 (11-2019)
JROS 2019, 6(4): 13-18 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shariatzadeh H, Najd Mazhar F, Sadony H, Bagheri N. The Role of Lunate Morphology in the Severity of Kienböck Disease: A Retrospective Study. JROS 2019; 6 (4) :13-18
URL: http://jros.iums.ac.ir/article-1-2080-en.html
URL: http://jros.iums.ac.ir/article-1-2080-en.html
1- Department of Orthopedic Surgery, Bone and Joint Reconstruction Research Center, Faculty of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 820 kb]
(774 Downloads)
| Abstract (HTML) (1601 Views)
Full-Text: (942 Views)
1. Introduction
Kienböck disease, also known as avascular necrosis of lunate, is a condition in which the lunate loses its blood supply resulting in the necrosis of the lunate bone. Kienböck disease is associated with pain, swelling, and increased risk of fracture, and in late stages with carpal osteoarthritis [1]. It is an almost rare disease with a prevalence of less than 5 in 10,000 people [2].
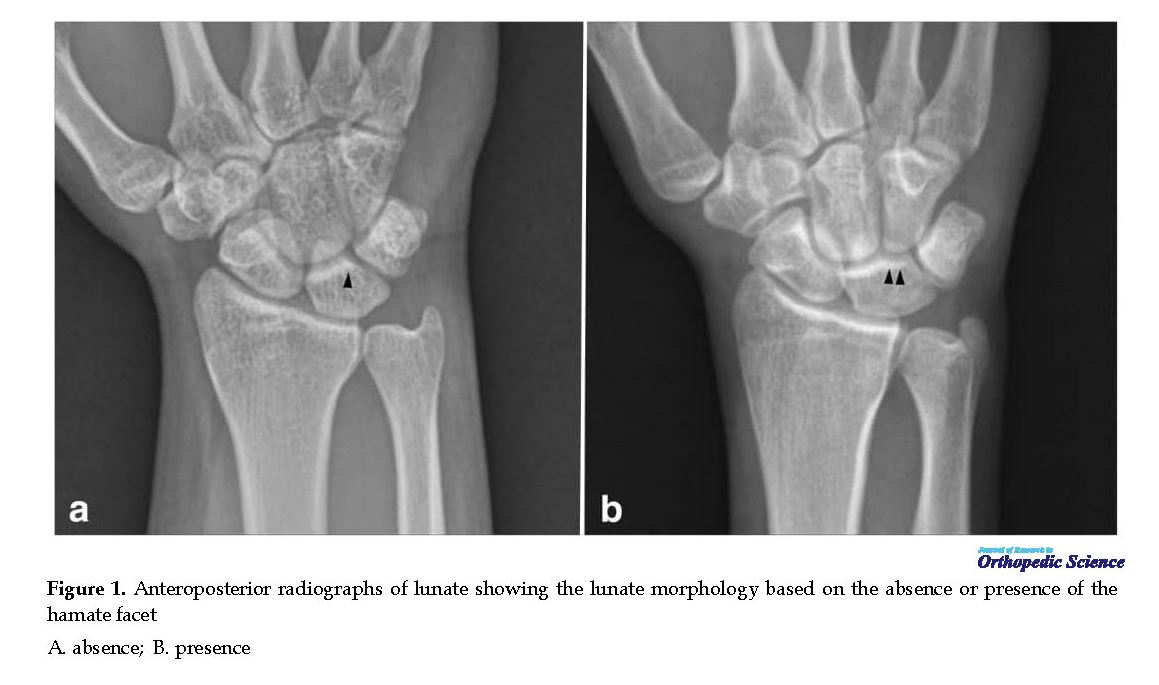
Despite the identification of the disease entity over 100 years ago, the etiopathogenesis of Kienböck disease is still uncertain. Even so, it has been associated with a variety of predisposing factors including single trauma, repetitive microtrauma, damage to the lunate blood supply, corticosteroid use, negative ulnar variance, decreased radial inclination, and lunate morphology [3-5]. Viegas et al. classified the lunate morphology based on the absence (type I) or presence (type II) of hamate facet at least 2 mm. They attributed the type II lunate with a higher risk of degenerative change at the proximal pole of the hamate [6]. Later, the lunate morphology was associated with greater scaphoid translation in type I and greater scaphoid flexion with radial deviation in type II [7, 8].
Recently, a connection was suggested to be present between the lunate morphology and severity of Kienböck disease so that type II lunates appeared to be protective against the disease progression [9]. This association may have therapeutic implications for the treatment of Kienböck disease. However, further evidence is required to more comprehensively understand the extent of such connection.In this study, we aimed to find if the lunate classification (absence or presence of hamate fact) associates with the severity of Kienböck disease and if yes, in what direction this association plays its role.
2. Methods
This retrospective study was approved by the review board of our institute, and informed consent was obtained from the patients to use their medical data for publication. Between 2014 and 2018, patients who were referred to our center with a diagnosis of stage IIIA or stage IIIB of Kienböck disease were evaluated for eligibility criteria. Only patients with the radiologic confirmation of Kienböck disease were included. The exclusion criteria were a concomitant wrist ligamentous injury, history of inflammatory disease, and history of operation on the involved wrist.
Kienböck disease, also known as avascular necrosis of lunate, is a condition in which the lunate loses its blood supply resulting in the necrosis of the lunate bone. Kienböck disease is associated with pain, swelling, and increased risk of fracture, and in late stages with carpal osteoarthritis [1]. It is an almost rare disease with a prevalence of less than 5 in 10,000 people [2].
Despite the identification of the disease entity over 100 years ago, the etiopathogenesis of Kienböck disease is still uncertain. Even so, it has been associated with a variety of predisposing factors including single trauma, repetitive microtrauma, damage to the lunate blood supply, corticosteroid use, negative ulnar variance, decreased radial inclination, and lunate morphology [3-5]. Viegas et al. classified the lunate morphology based on the absence (type I) or presence (type II) of hamate facet at least 2 mm. They attributed the type II lunate with a higher risk of degenerative change at the proximal pole of the hamate [6]. Later, the lunate morphology was associated with greater scaphoid translation in type I and greater scaphoid flexion with radial deviation in type II [7, 8].
Recently, a connection was suggested to be present between the lunate morphology and severity of Kienböck disease so that type II lunates appeared to be protective against the disease progression [9]. This association may have therapeutic implications for the treatment of Kienböck disease. However, further evidence is required to more comprehensively understand the extent of such connection.In this study, we aimed to find if the lunate classification (absence or presence of hamate fact) associates with the severity of Kienböck disease and if yes, in what direction this association plays its role.
2. Methods
This retrospective study was approved by the review board of our institute, and informed consent was obtained from the patients to use their medical data for publication. Between 2014 and 2018, patients who were referred to our center with a diagnosis of stage IIIA or stage IIIB of Kienböck disease were evaluated for eligibility criteria. Only patients with the radiologic confirmation of Kienböck disease were included. The exclusion criteria were a concomitant wrist ligamentous injury, history of inflammatory disease, and history of operation on the involved wrist.
Demographic and clinical characteristics of the patients were extracted from their medical records. A standardized lateral radiograph was used for carpal measurement so that radius-to-long finger metacarpal angle was fewer than 20º from the neutral position, and an appropriate scaphopisocapitate alignment was obtained. Modified Litchman classification system was used for staging the Kienböck disease. Accordingly, patients with a normal carpal alignment and height were considered as stage IIIA, while patients with fixed scaphoid rotation, decreased carpal height, and proximal migration of capitate was classified as stage IIIB [10].
Lunate morphology was investigated on plain radiograph and computed tomography scan or magnetic resonance imaging and was classified into type I (absence of hamate facet) and type II (presence of hamate facet) (Figure 1) [6]. Two fellowship-trained hand surgeons reviewed the radiographs for the typing of Kienböck disease as well as lunate morphology. In case the report of two observers did not match, a third observer was involved in reaching a consensus.
Lunate morphology was investigated on plain radiograph and computed tomography scan or magnetic resonance imaging and was classified into type I (absence of hamate facet) and type II (presence of hamate facet) (Figure 1) [6]. Two fellowship-trained hand surgeons reviewed the radiographs for the typing of Kienböck disease as well as lunate morphology. In case the report of two observers did not match, a third observer was involved in reaching a consensus.
Statistical analysis
SPSS V. 16 was used for the statistical evaluation of data. Descriptive statistics were provided as mean±SD or number and percentage. Comparison of the mean values between the quantitative variables was done using an independent t-test or its nonparametric equivalent (Mann-Whitney U test). Qualitative variables were compared using a chi-square test or Fisher exact test whenever the low expected cell counts were observed. All statistical tests were two-sided, and a p-value of fewer than 0.05 was considered as statistically significant.
3. Results
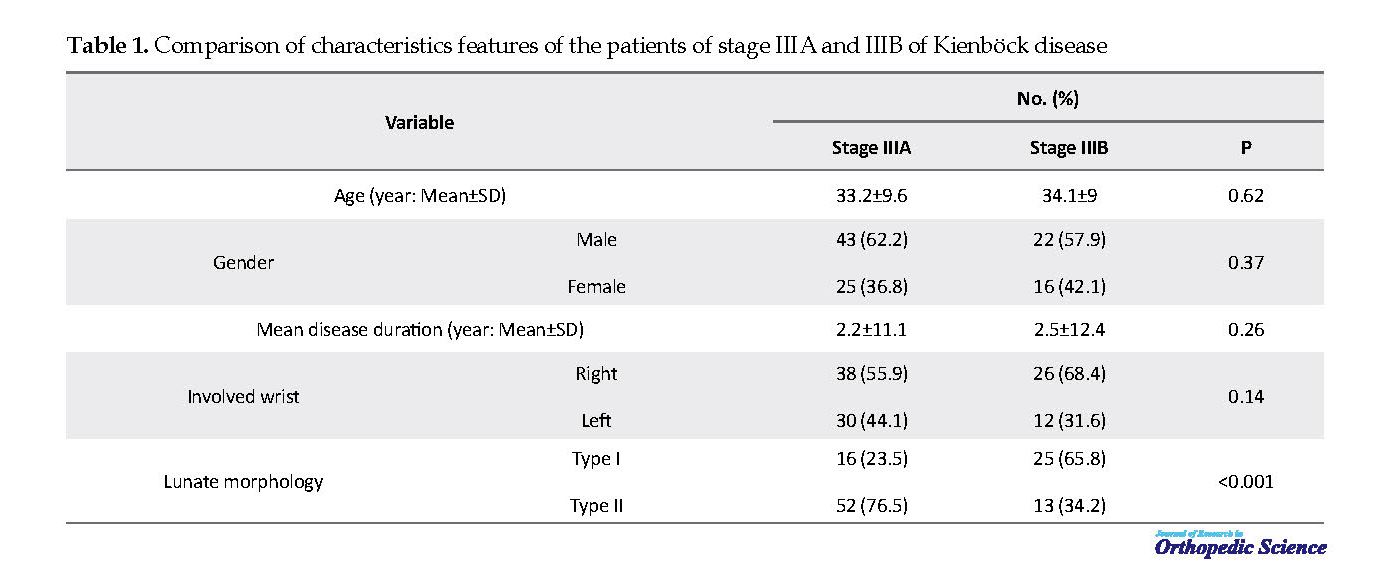
A total of 106 patients with a confirmed diagnosis of Kienböck disease were included in the analysis. The mean±SD age of the patients was 33.5±9.2 years, ranging from 12 to 63 years. Study population included 65 males (61.3%) and 41 females (38.7%). The disease was on the right side in 64 (60.4%) patients and the left side in 42 (39.6%) patients. Hamate facet was present in 65 (61.3%) patients and absent 41 (38.7%) patients. Stage IIIA and IIIB of Kienböck disease were identified in 68 (64.2%) and 38 (35.8%), respectively. Characteristics features of the patients of stage IIIA and IIIB are demonstrated in Table 1.
No significant difference was observed between the characteristic features of the patients of stage IIIA and IIIB (Table 1). A significant association was found between lunate morphology and stage of disease so that the number of patients with lunate type I was significantly more in stage IIIB of Kienböck disease (p<0.001) (Table 1). Lunate morphology was not associated with the gender of the patient (p=0.56). The stage of disease was not associated with the demographic characteristics of the patients such as age, gender (p=0.39 and p=0.58, respectively).
4. Discussion
The primary goal of treatment in Kienböck’s disease is to revascularize the lunate to prevent disease progression. Although many forms of surgical treatments have been described, there is no strong evidence to support any particular treatment over the others [11]. In this dilemma, identification of the disease risk factor could be regarded as a valuable choice to prevent disease progression and reduce the disease health and financial burden.
In this study, we aimed to evaluate how lunate morphology associate with the disease progression in Kienböck’s disease. We included a series of 106 patients with Kienböck’s disease of stage IIIA (68 patients) and stage IIIB (38 patients). The statistical analysis of data revealed a strong association between the stage of Kienböck’s disease and lunate morphology so that the number of patients with lunate type I (abcense of hamate facet) was significantly more in the stage IIIB. In another word, the results of the present study reveal that type II of lunate could be regarded as a protective factor against the progression of the Kienböck’s disease.
Viegas et al. reviewed the incidence of hamate facet and any associated pathologic conditions in 165 cadaveric wrists. Based on their results, type I and II of lunate were seen in 34.5% and 65.5% of patients, respectively [12]. A range of 27%-73% for the type II lunate has been reported in the subsequent investigations [13-15]. Kato et al. in patients with radiographic findings consistent with Kienböck disease noticed a prevalence of type II lunate in 26% of the unaffected wrist [16]. Rhee et al. reported a 29% prevalence of a type II lunate in the involved wrist of patients with Kienböck disease [9]. The prevalence of type II lunate was 61.3% in patients the present series.
Rhee et al. aimed to determine the role of lunate morphology on the radiographic characteristics of Kienböck disease in a retrospective study of 106 patients. At the presentation, patients with type I of lunate had significantly more advanced disease so that 41.3% of patients with type I lunate were categorized as stage IIIB or greater, versus 29% of patients with type II lunate. Coronal fracture of the lunate was also more prevalent in type I lunate. They concluded that lunate morphology affects the severity of Kienböck disease, and type II of the lunate seem to be protective against the progression of the disease [9]. Similar to the study of Rhee et al. the results of the present study revealed that patients with type II of the lunate at initial presentation might experience less severe disease so that lunate type II was identified in 76.5% of the patients who were categorized as stage IIIA and 34.2% of patients who were detected with type IIIB of Kienböck disease.
Based on the provided evidence, a type II lunate could also result in a better outcome in early stages of disease (II-IIIA), as classically, stage II-IIIA of Kienböck disease are managed with unloading or joint leveling procedure. However, in higher stages (IIIB or IV), which carpal malalignment or degenerative change is present, wrist arthrodesis is the main choice of treatment [17].
The present study was not without limitation. The main limitation of this study was the retrospective nature of the study. For this limitation, we were not able to follow patients and monitor disease progression. Thus, further steps to more comprehensively evaluate the role of lunate morphology in the progression of Kienböck disease would be to perform a prospective study. A longitudinal study also provides an opportunity to evaluate the effect of the lunate morphology on the outcome of treatment.
5. Conclusion
Lunate type I was more frequent in patients initially presented with stage IIIB of Kienböck disease, whereas lunate type II was more prevalent in patients who were initially presented with stage IIIA. These results suggest that lunate morphology is associated with the severity of Kienböck disease and could be used to prevent disease progression and optimize the outcome of treatment. However, longitudinal studies are required to confirm the results of present investigation.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article and all data used with patients permission.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Sampling and methodology: Hooman Shariatzadeh; Data analysis: Farid Najd Mazhar; Writing the manuscript: Hanon Sadony; Paper writing, editing: Nima Bagheri.
Conflict of interest
The authors declared no conflict of interest.
References
Stahl S, Stahl AS, Meisner C, Rahmanian-Schwarz A, Schaller HE, Lotter O. A systematic review of the etiopathogenesis of Kienböck’s disease and a critical appraisal of its recognition as an occupational disease related to hand-arm vibration. BMC Musculoskelet Disord. 2012; 13:225. [DOI:10.1186/1471-2474-13-225] [PMID] [PMCID]
Official Journal of the European. Decision No 1295/1999/EC of the European Parliament and of the council of 29 April 1999 adopting a programme of Community action on rare diseases within the framework for action in the field of public health (1999 to 2003). New York: Official Journal of the European; 1999.
Bain GI, MacLean SBM, Yeo CJ, Perilli E, Lichtman DM. The etiology and pathogenesis of kienböck disease. J wrist Surg. 2016; 5(4):248-54. [DOI:10.1055/s-0036-1583755] [PMID] [PMCID]
Jafari D, Shariatzadeh H, Ajvadi A. Kienböck’s disease; the length of capitate and third metacarpal bones. Shafa Ortho J. 2016; 3(3):e5659. [DOI:10.17795/soj-5659]
Jafari D, Shariatzadeh H, Hosseini B. [The effect of proximal lunate morphology “Zapico Classification” on Kienböck’s disease (Persian)]. Shafa Ortho J. 2017; 4(3):1-9. [DOI:10.5812/soj.12303]
Viegas SF, Wagner K, Patterson R, Peterson P. Medial (hamate) facet of the lunate. J Hand Surg. 1990; 15(4):564-71. [DOI:10.1016/S0363-5023(09)90016-8]
Nakamura K, Patterson RM, Moritomo H, Viegas SF. Type I versus type II lunates: Ligament anatomy and presence of arthrosis. J Hand Surg. 2001; 26(3):428-36. [DOI:10.1053/jhsu.2001.24140] [PMID]
Galley I, Bain GI, McLean JM. Influence of lunate type on scaphoid kinematics. J Hand Surg. 2007; 32(6):842-7. [DOI:10.1016/j.jhsa.2007.03.012] [PMID]
Rhee PC, Jones DB, Moran SL, Shin AY. The effect of lunate morphology in Kienböck disease. J Hand Surg. 2015; 40(4):738-44. [DOI:10.1016/j.jhsa.2014.12.024] [PMID]
Allan CH, Joshi A, Lichtman DM. Kienböck’s disease: Diagnosis and treatment. J American Acad Ortho Surg. 2001; 9(2):128-36. [DOI:10.5435/00124635-200103000-00006] [PMID]
Schuind F, Eslami S, Ledoux P. Kienbock’s disease. J Bone Joint Surg Br. 2008; 90(2):133-9. [DOI:10.1302/0301-620X.90B2.20112] [PMID]
Kim YS, Lee HM. The scaphocapitate fracture syndrome. Eur J Orthopedic Surgeon Traumatol. 2013; 23(s2):207-12.[DOI:10.1016/S0363-5023(09)90016-8]
Viegas SF, Patterson RM, Hokanson JA, Davis J. Wrist anatomy: Incidence, distribution, and correlation of anatomic variations, tears, and arthrosis. J Hand Surg. 1993; 18(3):463-75. [DOI:10.1016/0363-5023(93)90094-J]
Dharap A, Al-Hashimi H, Kassab S, Abu-Hijleh M. The hamate facet of the lunate: A radiographic study in an Arab population from Bahrain. Surg Radiolog Anatom. 2006; 28(2):185-8. [DOI:10.1007/s00276-005-0061-0] [PMID]
Dyankova S. Anthropometric characteristics of wrists joint surfaces depending on lunate types. Surg Radiolog Anatom. 2007; 29(7):551-9. [DOI:10.1007/s00276-007-0236-y] [PMID]
Kato H, Nakamura R. Lunate morphology of Kienböck’s disease on x-ray study. Hand Surg. 1999; 4(01):75-9. [DOI:10.1142/S0218810499000137]
Goldfarb CA, Hsu J, Gelberman RH, Boyer MI. The Lichtman classification for Kienböck’s disease: An assessment of reliability. J Hand Surger. 2003; 28(1):74-80. [DOI:10.1053/jhsu.2003.50035] [PMID]
SPSS V. 16 was used for the statistical evaluation of data. Descriptive statistics were provided as mean±SD or number and percentage. Comparison of the mean values between the quantitative variables was done using an independent t-test or its nonparametric equivalent (Mann-Whitney U test). Qualitative variables were compared using a chi-square test or Fisher exact test whenever the low expected cell counts were observed. All statistical tests were two-sided, and a p-value of fewer than 0.05 was considered as statistically significant.
3. Results
A total of 106 patients with a confirmed diagnosis of Kienböck disease were included in the analysis. The mean±SD age of the patients was 33.5±9.2 years, ranging from 12 to 63 years. Study population included 65 males (61.3%) and 41 females (38.7%). The disease was on the right side in 64 (60.4%) patients and the left side in 42 (39.6%) patients. Hamate facet was present in 65 (61.3%) patients and absent 41 (38.7%) patients. Stage IIIA and IIIB of Kienböck disease were identified in 68 (64.2%) and 38 (35.8%), respectively. Characteristics features of the patients of stage IIIA and IIIB are demonstrated in Table 1.
No significant difference was observed between the characteristic features of the patients of stage IIIA and IIIB (Table 1). A significant association was found between lunate morphology and stage of disease so that the number of patients with lunate type I was significantly more in stage IIIB of Kienböck disease (p<0.001) (Table 1). Lunate morphology was not associated with the gender of the patient (p=0.56). The stage of disease was not associated with the demographic characteristics of the patients such as age, gender (p=0.39 and p=0.58, respectively).
4. Discussion
The primary goal of treatment in Kienböck’s disease is to revascularize the lunate to prevent disease progression. Although many forms of surgical treatments have been described, there is no strong evidence to support any particular treatment over the others [11]. In this dilemma, identification of the disease risk factor could be regarded as a valuable choice to prevent disease progression and reduce the disease health and financial burden.
In this study, we aimed to evaluate how lunate morphology associate with the disease progression in Kienböck’s disease. We included a series of 106 patients with Kienböck’s disease of stage IIIA (68 patients) and stage IIIB (38 patients). The statistical analysis of data revealed a strong association between the stage of Kienböck’s disease and lunate morphology so that the number of patients with lunate type I (abcense of hamate facet) was significantly more in the stage IIIB. In another word, the results of the present study reveal that type II of lunate could be regarded as a protective factor against the progression of the Kienböck’s disease.
Viegas et al. reviewed the incidence of hamate facet and any associated pathologic conditions in 165 cadaveric wrists. Based on their results, type I and II of lunate were seen in 34.5% and 65.5% of patients, respectively [12]. A range of 27%-73% for the type II lunate has been reported in the subsequent investigations [13-15]. Kato et al. in patients with radiographic findings consistent with Kienböck disease noticed a prevalence of type II lunate in 26% of the unaffected wrist [16]. Rhee et al. reported a 29% prevalence of a type II lunate in the involved wrist of patients with Kienböck disease [9]. The prevalence of type II lunate was 61.3% in patients the present series.
Rhee et al. aimed to determine the role of lunate morphology on the radiographic characteristics of Kienböck disease in a retrospective study of 106 patients. At the presentation, patients with type I of lunate had significantly more advanced disease so that 41.3% of patients with type I lunate were categorized as stage IIIB or greater, versus 29% of patients with type II lunate. Coronal fracture of the lunate was also more prevalent in type I lunate. They concluded that lunate morphology affects the severity of Kienböck disease, and type II of the lunate seem to be protective against the progression of the disease [9]. Similar to the study of Rhee et al. the results of the present study revealed that patients with type II of the lunate at initial presentation might experience less severe disease so that lunate type II was identified in 76.5% of the patients who were categorized as stage IIIA and 34.2% of patients who were detected with type IIIB of Kienböck disease.
Based on the provided evidence, a type II lunate could also result in a better outcome in early stages of disease (II-IIIA), as classically, stage II-IIIA of Kienböck disease are managed with unloading or joint leveling procedure. However, in higher stages (IIIB or IV), which carpal malalignment or degenerative change is present, wrist arthrodesis is the main choice of treatment [17].
The present study was not without limitation. The main limitation of this study was the retrospective nature of the study. For this limitation, we were not able to follow patients and monitor disease progression. Thus, further steps to more comprehensively evaluate the role of lunate morphology in the progression of Kienböck disease would be to perform a prospective study. A longitudinal study also provides an opportunity to evaluate the effect of the lunate morphology on the outcome of treatment.
5. Conclusion
Lunate type I was more frequent in patients initially presented with stage IIIB of Kienböck disease, whereas lunate type II was more prevalent in patients who were initially presented with stage IIIA. These results suggest that lunate morphology is associated with the severity of Kienböck disease and could be used to prevent disease progression and optimize the outcome of treatment. However, longitudinal studies are required to confirm the results of present investigation.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article and all data used with patients permission.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Sampling and methodology: Hooman Shariatzadeh; Data analysis: Farid Najd Mazhar; Writing the manuscript: Hanon Sadony; Paper writing, editing: Nima Bagheri.
Conflict of interest
The authors declared no conflict of interest.
References
Stahl S, Stahl AS, Meisner C, Rahmanian-Schwarz A, Schaller HE, Lotter O. A systematic review of the etiopathogenesis of Kienböck’s disease and a critical appraisal of its recognition as an occupational disease related to hand-arm vibration. BMC Musculoskelet Disord. 2012; 13:225. [DOI:10.1186/1471-2474-13-225] [PMID] [PMCID]
Official Journal of the European. Decision No 1295/1999/EC of the European Parliament and of the council of 29 April 1999 adopting a programme of Community action on rare diseases within the framework for action in the field of public health (1999 to 2003). New York: Official Journal of the European; 1999.
Bain GI, MacLean SBM, Yeo CJ, Perilli E, Lichtman DM. The etiology and pathogenesis of kienböck disease. J wrist Surg. 2016; 5(4):248-54. [DOI:10.1055/s-0036-1583755] [PMID] [PMCID]
Jafari D, Shariatzadeh H, Ajvadi A. Kienböck’s disease; the length of capitate and third metacarpal bones. Shafa Ortho J. 2016; 3(3):e5659. [DOI:10.17795/soj-5659]
Jafari D, Shariatzadeh H, Hosseini B. [The effect of proximal lunate morphology “Zapico Classification” on Kienböck’s disease (Persian)]. Shafa Ortho J. 2017; 4(3):1-9. [DOI:10.5812/soj.12303]
Viegas SF, Wagner K, Patterson R, Peterson P. Medial (hamate) facet of the lunate. J Hand Surg. 1990; 15(4):564-71. [DOI:10.1016/S0363-5023(09)90016-8]
Nakamura K, Patterson RM, Moritomo H, Viegas SF. Type I versus type II lunates: Ligament anatomy and presence of arthrosis. J Hand Surg. 2001; 26(3):428-36. [DOI:10.1053/jhsu.2001.24140] [PMID]
Galley I, Bain GI, McLean JM. Influence of lunate type on scaphoid kinematics. J Hand Surg. 2007; 32(6):842-7. [DOI:10.1016/j.jhsa.2007.03.012] [PMID]
Rhee PC, Jones DB, Moran SL, Shin AY. The effect of lunate morphology in Kienböck disease. J Hand Surg. 2015; 40(4):738-44. [DOI:10.1016/j.jhsa.2014.12.024] [PMID]
Allan CH, Joshi A, Lichtman DM. Kienböck’s disease: Diagnosis and treatment. J American Acad Ortho Surg. 2001; 9(2):128-36. [DOI:10.5435/00124635-200103000-00006] [PMID]
Schuind F, Eslami S, Ledoux P. Kienbock’s disease. J Bone Joint Surg Br. 2008; 90(2):133-9. [DOI:10.1302/0301-620X.90B2.20112] [PMID]
Kim YS, Lee HM. The scaphocapitate fracture syndrome. Eur J Orthopedic Surgeon Traumatol. 2013; 23(s2):207-12.[DOI:10.1016/S0363-5023(09)90016-8]
Viegas SF, Patterson RM, Hokanson JA, Davis J. Wrist anatomy: Incidence, distribution, and correlation of anatomic variations, tears, and arthrosis. J Hand Surg. 1993; 18(3):463-75. [DOI:10.1016/0363-5023(93)90094-J]
Dharap A, Al-Hashimi H, Kassab S, Abu-Hijleh M. The hamate facet of the lunate: A radiographic study in an Arab population from Bahrain. Surg Radiolog Anatom. 2006; 28(2):185-8. [DOI:10.1007/s00276-005-0061-0] [PMID]
Dyankova S. Anthropometric characteristics of wrists joint surfaces depending on lunate types. Surg Radiolog Anatom. 2007; 29(7):551-9. [DOI:10.1007/s00276-007-0236-y] [PMID]
Kato H, Nakamura R. Lunate morphology of Kienböck’s disease on x-ray study. Hand Surg. 1999; 4(01):75-9. [DOI:10.1142/S0218810499000137]
Goldfarb CA, Hsu J, Gelberman RH, Boyer MI. The Lichtman classification for Kienböck’s disease: An assessment of reliability. J Hand Surger. 2003; 28(1):74-80. [DOI:10.1053/jhsu.2003.50035] [PMID]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2019/11/8 | Accepted: 2019/11/9 | Published: 2019/12/25
Received: 2019/11/8 | Accepted: 2019/11/9 | Published: 2019/12/25
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |