BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jros.iums.ac.ir/article-1-2110-en.html


 , Hossein Farahini1
, Hossein Farahini1 
 , Mikaiel Hajializade1
, Mikaiel Hajializade1 

 , Shadi Abdollahi Kordkandi1
, Shadi Abdollahi Kordkandi1 
 , Reza Amiri1
, Reza Amiri1 
 , Mani Mahmoudi1
, Mani Mahmoudi1 

 , Seyed Mani Mahdavi1
, Seyed Mani Mahdavi1 
 , Mehdi Moghtadaei1
, Mehdi Moghtadaei1 


1. Introduction
Femoral head fractures are rare injuries caused by high-energy trauma applied to the hip or lower extremity, such as car accidents [1]. These injuries are frequently associated with a hip dislocation so that nearly 6%-16% of posterior hip dislocations are getting complicated with femoral head fracture [2-4].
Since femoral head fractures are intra-articular injuries, their management always presents distinctive complexities for surgeons. Delayed reduction of the dislocated hip increases the prevalence of osteonecrosis. Therefore, the reduction of associated hip dislocations is an emergency [2]. Moreover, removal of the loose body of joint, anatomic reduction of large displaced fracture fragments, and restoration of congruity and stability of hip joint are necessary to achieve a favorable long-term outcome [5].Treatment options range from a simple closed reduction to resection of the femoral head, open reduction and fixation, arthrodesis, or primary arthroplasty. Even after the timely management of the injury, reported outcomes continue to be relatively poor with high rates of post-traumatic arthritis, avascular necrosis [6], and Heterotopic Ossification (HO).
For several reasons, there is no consensus over the optimal treatment of femoral head fractures. Considering the rare incidence of this injury, even the largest series have included a few patients. Fracture characteristics such as fracture location, size, and displacement have all been used as a rationale for injury management and could be regarded as a source of heterogeneity. fractures that need an operation, the surgical approach, choosing between fragment fixation or excision, and the very fixation technique are matters of debate. Besides, multiple classification systems have been proposed, and a uniform classification system has not been used by different authors [7, 8]. Because of these inconsistencies, issues such as overall prognosis, long-term outcome, rate of fixation failure, Avascular Necrosis (AVN), HO, post-traumatic arthritis, and conversion to total hip arthroplastyare still poorly understood.
The main question that should be answered is what treatment strategy results in better function and less complicated outcomes. We hypothesized that reporting the results of a series of patients with femoral head fractures managed according to a predesigned therapeutic algorithm would shed some light on the management of femoral head fracture. In this study, we report the initial management, outcomes, and complications of femoral head fracture in a consecutive series of patients treated at a single health center with the same therapeutic guideline.
2. Methods
This study was approved by the Review Board of our institute under the code of IR.IUMS.REC.1398.618 and patients provided written consent for using their medical data for publication. In a retrospective review of a prospectively collected orthopedic database, patients with femoral head fractures [9] who were treated in our University Hospital between 2009 and 2018 were evaluated for eligibility criteria. The inclusion criteria were an acute traumatic fracture of the femoral head, an available plain Anteroposterior (AP) radiograph of the affected hip and a follow-up period of more than six months. Patients with a pathologic fracture, previous hip surgery, history of severe underlying disease like Alzheimer’, etc. that cause recurrent falling down were excluded even the patient who were treated with new drugs and have no history of falling down during recent years [10]. Also patients' with incomplete documentation were excluded.
The demographic data, fracture characteristics, operative detail, clinical, and radiographic outcomes were extracted from the patients' medical records. The demographic data of the patients included age, gender, Body Mass Index (BMI), mechanism of injury, and follow-up period. Fracture characteristics included the type of fracture according to the Pipkin classification system [11]. Accordingly, Pipkin type (I) was defined as a femoral head fracture distal to the fovea (Figure 1).

Pipkin type II was defined as a femoral head fracture proximal to the fovea (Figure 2).

Pipkin type III was defined as a femoral head fracture associated with femoral neck fracture (Figure 3).

Pipkin type IV w::as char::acterized as a femoral head fracture associated with acetabulum fracture (Figure 4).
.png)
Operative details included the surgical approach, the hardware used, and intraoperative blood loss.
The clinical outcome was evaluated with the Harris Hip Score (HHS) with the maximum possible score of 100 so that a higher score indicates a better outcome. The HHS score is categorized as follows: poor (a score of <70), fair (a score of 70–80), good (a score of 80–90), and excellent (a score of 90–100) [12]. The radiologic outcome included the evaluation of AVN, heterotopic ossification, fracture :union:, and arthritis. Any postoperative complication such as infection, arterial injury, sciatic nerve dysfunction, dislocation, and conversion to total hip arthroplasty was also extracted.
Fracture :union: was defined clinically as a lack of pain with full weight-bearing and radiographically as fracture consolidation. The presence of radiographic sclerosis and flattening of the femoral head, conjunct with persistent/worsening hip pain, was used for the identification of AVN. HO was investigated on the AP pelvic radiograph and classified using the Brooker system [13].
Surgical approach
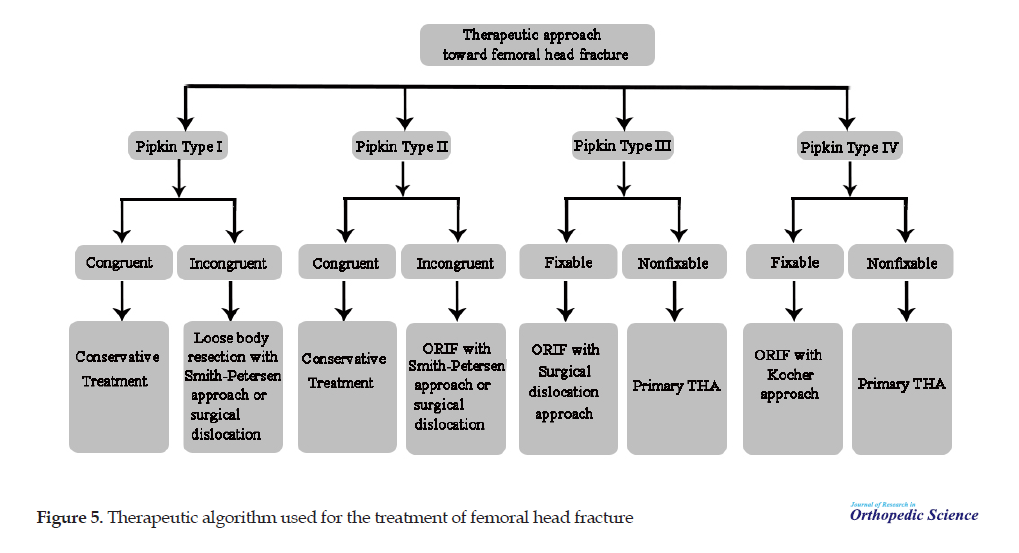
After ruling out a concomitant femoral neck fracture, an immediate reduction of a dislocated hip is performed in the emergency room. If closed reduction was not successful, the patient was urgently sent to the operating room for an open reduction. Plain radiographs and CT scan were obtained following a reduction in all patients [14]. For patients with Pipkin type I and II, a congruent joint conservative treatment is implicated. Total hip arthroplasty was used for patients with Pipkin type III or IV that was not fixable. Otherwise, the fracture was fixed via one of the following approaches: Smith-Peterson, Kocher-Langenbeck, or surgical dislocation approach. Our therapeutic approach is demonstrated in Figure 5.
Herbert or biodegradable screws were used for fixation purposes. Loose body resection was done whenever indicated. All the surgeries were done by one senior hip surgeon.
Postoperative protocol
All patients were partial weight-bearing the day after surgery and the patient with concomitant pelvic ring fracture was wheelchair band.
Demographic characteristics
A total of 41 patients with femoral head fractures were identified as eligible for the study. The study population included 34 (82.9%) males and 7 (17.1%) females with the Mean±SD age of 35.8±14.1 years (range 18-65 y). The Mean±SD follow-up of the patients was 32.6±11.3 months (range 6-48 mo). Pipkin type classification of the patients’ fractures was as follows: Pipkin type I in 19 (46.3%), II in 6 (14.6%), III in 4 (9.8%), and IV in 12 (29.3%) patients. Two patients (4.9%) patients were treated conservatively, while the remaining 39 patients (95.1%) patients were treated surgically. In 13 patients (31.7%) patients, the femoral head fracture was associated with hip dislocation. Seven patients (17.7%) patients were presented with sciatic nerve injury. Twenty-five patients were presented with one or more associated injuries including knee ligament injury (n=11, 26.8%), pelvic ring fracture (n=8, 19.5%), femoral shaft fracture (n=8, 19.5%), soft-tissue injury (n=6, 14.6%), and spine injury (n=1, 2.4%). The detailed characteristics of the patients are presented in Table 1.

Statistical analysis
Statistical analyses were done in SPSSV. 16. Descriptive variables were presented as Mean±SD for numerical variables and number and percentage for categorical variables. A comparison of mean values between the two groups was made using the independent t-test or its nonparametric counterpart (Mann-Whitney U test). A P value of <0.05 was considered significant. A comparison of mean values between more than two groups was made using the analysis of variance (ANOVA) test or its nonparametric counterpart (The Kruskal-Wallis H test). A Chi-squared test was used for the comparison of categorical variables. The Pearson's or Spearman's correlation coefficient test was used for the evaluation of potential correlations. A P value of less than 0.05 was considered significant.
3. Results
Of 41 cases of femoral head fracture, 34 cases (82.9%) had uncomplicated outcomes. The remaining 8 patients (17.1%) patients had one or more complications. Four out of 7 fractures (57.1%) that were treated with THA ended up with a complicated outcomes because of infection and loosening. Six out of 7 patients (85.7%) who had complicated outcome were presented with associated injuries (Table 2).

AVN was the most common complication of patients in the current study, which was observed in 5 patients (12.2%). The other complications included HO (n=2, 4.9%), infection (n=2, 4.9%), and prosthesis dislocation (n=1, 2.4%). No case of fixation failure and non:union: was seen in the present series. Despite the new way for the treatment of non:union: and bone healing, it is very difficult to treat; non:union: always was a major concern for orthopedic surgeons [15]. The characteristic feature of patients who sustained a postoperative complication is presented in Table 2.
The Mean±SD HHS score was 85.1±109 (range 49-96). According to the HHS score, poor, fair, good, and excellent results were seen in 4 (9.8%), 6 (14.6%), 13 (31.7%), and 17 (41.5%) patients, respectively. Two patients (50%) with poor results had Pipkin type III, and the other two had Pipkin type IV. The distribution of HHS status, according to the Pipkin type, is presented in Table 3.

The Mean±SD HHS score was 75.3±14.7 in patients with a complicated outcome and 89.4±4.5 in patients with an uncomplicated outcome. This difference was statistically significant (P=0.007). The Mean±SD HHS score was 87.8±7.2 in Pipkin type I, 89.8±6.1 in Pipkin type II, 75.3±17.6 in Pipkin type III, and 81.5±13.2 in Pipkin type IV. This difference was not statistically significant (P=0.071).
The Mean±SD HHS score was 91±5.6 in the conservative treatment group. The Mean±SD HHS score was 85.9±9.3 in the surgical fixation group with Kocher approach, 85.1±15.1 in the surgical fixation with surgical dislocation approach, and 87.1±5.8 in the surgical fixation with Smith-Peterson approach (P=0.25). The Mean±SD HHS score was 75.8±12.6 in the THA group, which was significantly lower than that in the other groups (P=0.022). The Mean±SD HHS score was 82.1±11.4 in patients in whom Herbert screw was used, 89±7.7 in patients in whom biodegradable screw was used. Accordingly, in case of using Herbert screw the HHS score was significantly lower (P=0.041). No significant correlation was found between the HHS scores and demographic characteristics of patients, such as age, gender, and BMI.
The Mean±SD surgical bleeding was 170.8±96 mL (range 75-550). The Mean±SD surgical bleeding was 170±107.9 in fractures with the complicated outcomes and 171.7±61 in fractures with the uncomplicated outcome (P=0.97). The Mean±SD surgical bleeding was 143.1±75.6 in Pipkin type I, 124.2±39 cc in Pipkin type II, 175±35.3 cc in Pipkin type III, and 238±121.7 cc in Pipkin type IV. Accordingly, surgical bleeding was significantly more in Pipkin type IV (P=0.034). The mean surgical bleeding was not significantly different between different types of approaches (P=0.949).
The number of associated injuries was significantly more in patients with a complicated outcome in comparison with patients with uncomplicated outcomes (85.7% vs. 47.5%, P=0.049). The mean patients' age and BMI were not significantly different between patients with complicated and uncomplicated outcomes (P=0.272, P=0.222, respectively). The mechanism of injury was not associated with a complicated outcome, as well (P=0.542).
4. Discussion
There is no concrete information about many aspects of femoral head fracture, including optimal management, outcomes, and complications [16-20]. As a general rule, Open Reduction and Internal Fixation (ORIF) is the treatment of choice for most patients with femoral head fracture. Whenever there is a very small fragment located in the region below the fovea, loose body resection should be indicated. Total hip arthroplasty is preferable in elderly patients and those who experience comminuted femoral head fracture [16]. Besides this general guideline, there is no detailed consensus for the treatment of femoral head fracture, such as the approach of fixation [16].
This heterogeneity could be regarded as one of the main reasons causing the results of different studies incomparable. For this reason, we aimed to provide a treatment algorithm for the treatment of femoral head fracture (Figure 5). In this study, we reported the outcomes of our therapeutic algorithm in a consecutive series of patients with femoral head fracture. Based on our results, femoral head fracture treatment resulted in good to excellent outcomes in 73.2% of cases. Patients with complications will probably have poor outcomes. Complicated outcomes are more frequent in patients with associated injuries and those who are treated with THA. The mean HHS score was significantly lower in THA patients, as well. AVN was the most frequent complication which was observed in 12.2% of patients, respectively.
Yu et al. evaluated the clinical results of femoral head fracture-dislocation in 19 patients who were treated according to the Pipkin classification. Their general treatment guideline included conservative treatment for congruent fractures of Pipkin type I and II and THA for unfixable fractures of Pipkin type III and IV. Otherwise, fixation was performed via either Smith-Peterson or Kocher approach. They did not use the surgical dislocation approach. Functional results were assessed by HHS criteria. Based on their results, excellent and good results were observed in 73.7%. Poor and fair results were more frequent in Pipkin type III and IV. They concluded that although Pipkin classification helped judge the prognosis, many other other factors such as age may affect the clinical outcomes [21].
The HHS status of our series was comparable to the study of Yu et al. Similar to the study of Yu et al., the poor result was more frequent in Pipkin type IV. However, the correlation of Pipkin type with HHS was not significant in the present series, which confirms the role of other factors on the outcomes of treatment, such as the presence of associated injuries. Yet, in contrast to the station of Yu et al., the outcomes of treatment were not associated with the age of the patient in our study. This inconsistency could be explained by the age difference of the patients in two studies. The mean age of the patients was 35.8 years in the present series and 40.2 years in the study of Yu et al.
Tonetti et al. evaluated the outcome of femoral head fracture in a cohort of 110 patients. The posterior, anterior, medial, or double anteromedial approach was recorded in patients who underwent surgery (78 patients). Surgical treatment comprised of osteosynthesis 46 cases, removal of fragments in 40 cases, and Total Hip Replacement (THR) in five cases as a primary treatment. The mean visual analog scale was higher in the THR group at the end of follow-up [22]. Similar to the study of Tonetti et al., the complicated outcome was more frequent in the THR group of the present study. The clinical outcome was poor in this group, as well.
Scolaro et al. evaluated the incidence, method of treatment, and outcomes of femoral head fractures in 164 fractures in 163 consecutive patients. Their treatment was ORIF in 78 patients, fragment excision in 37 patients, and non-operative in 28 patients. Fracture fixation was performed through the Smith-Peterson approach in the majority of cases. Fragment excision was performed via the Kocher approach. All Pipkin type III fractures of this series had a failure of fixation. AVN was developed is six patients. HO developed in 28 patients (40.6%) of this series [18]. No fixation failure was seen recorded in the present study. The rate of HO was considerably lower in our series compared to the study of Sclaro et al.
The outcomes of femoral head fracture have also been evaluated in several other investigations. Giannoudis et al. conducted a systematic review of the literature to investigate the management, complications, and clinical results of femoral head fracture. Twenty-nine eligible articles, reporting the outcome of 453 femoral head fractures in 450 patients, met the inclusion criteria for this study. According to this study, fractured fragment excision seems to give better results in Pipkin type I compared to ORIF, while for Pipkin type II, anatomic reduction and stable fixation were recommended. The rate of wound infection was 3.2% in this review. Sciatic nerve palsy complicated 3.95% of fractures. Major late complications included AVN (11.9%), arthritis (20%), and HO (16.8%) [8]. The rate of infection in the present study was comparable to the study of Giannoudis et al. AVN was the most common late complication of femoral head fracture in the current series.
The results of the present study reveal that an inferior outcome could be expected in patients who undergo THA for the treatment of the femoral head fracture. Also patients with associated injuries are at a higher risk of a complicated outcome. Even so, the outcome of femoral head fracture is good to excellent in the majority of patients.
This study was not without limitations. The main limitation of this study was the small number of patients in some subgroups, which might have affected the power of statistical analysis. The retrospective design of the study could be regarded as its other limitation.
The therapeutic algorithm used in the present study led to the good to excellent results in the majority of patients who sustained a femoral head fracture. However, according to our results, patients with associated injuries and those who undergo THA might experience a complicated outcome as well as inferior clinical results. Also, late complications of this fracture, such as AVN, should be discussed with patients to address their expectations. After all, further standardization of the therapeutic strategy is required to make the results of different studies comparable.
We can sum up the main points of this study as below: 1. A femoral head fracture has a variable outcome; 2. The best approach for femoral head fracture is unknown; 3.Surgeon skill has a major role in the outcome of the femoral head fracture.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Review Board of Iran University of Medical Sciences (Code: IR.IUMS.REC.1398.618) and patients provided written consent for using their medical data for publication.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Operation: Ali Yeganeh, Mikaiel Hajializade, Mani Mahmudi; Visualization, assisted surgeon: Reza Amiri, Mikaiel Hajializade; Writing the original draft, data curation, methodology: Mikaiel Hajializade. Shadi Abdollahi Kordkandi, Seyed Mani Mahdavi.
Conflict of interest
The authors declared no conflict of interest.
References
1.Ross JR, Gardner MJ. Femoral head fractures. Curr Rev Musculoskelet Med. 2012; 5(3):199-205. [DOI:10.1007/s12178-012-9129-8] [PMID] [PMCID]
2.Hougaard K, Thomsen PB. Traumatic posterior fracture-dislocation of the hip with fracture of the femoral head or neck, or both. J Bone Joint Surg Am. 1988; 70(2):233-9. [DOI:10.2106/00004623-198870020-00011] [PMID]
3.Sahin V, Karakas ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma. 2003;54(3):520-9. [DOI:10.1097/01.TA.0000020394.32496.52] [PMID]
4.Pisoudeh K, Gharanizadeh k, Sarshar MR, Mahmoudi M. Surgical treatment outcome in young adults with femoral neck fractures. J Res Orthop Sci. 2020; 7(1):23-8. [DOI:10.32598/JROS.7.1.23]
5.Asghar FA, Karunakar MA. Femoral head fractures: Diagnosis, management, and complications. Orthop Clin North Am. 2004; 35(4):463-72. [DOI:10.1016/j.ocl.2004.05.004] [PMID]
6.Abolghasemian M, Ramezan Shirazi M, Gharanizadeh K, Yeganeh A, Safir O, Gross AE, et al. Actors associated with the course of femoral head osteonecrosis; A retrospective study. J Res Orthop Sci. 2015; 2(2).
7.Guimaraes RP, Saeki de Souza G, da Silva Reginaldo S, Ono NK, Honda EK, Polesello GC, et al. Study of the treatment of femoral head fractures. Rev Bras Ortop. 2015; 45(4):355-61. [DOI:10.1016/S2255-4971(15)30381-5]
8.Giannoudis P, Kontakis G, Christoforakis Z, Akula M, Tosounidis T, Koutras C. Management, complications and clinical results of femoral head fractures. Injury. 2009; 40(12):1245-51. [DOI:10.1016/j.injury.2009.10.024] [PMID]
9.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007; 21(Suppl. 10):S1-133. [DOI:10.1097/00005131-200711101-00001] [PMID]
10.Berahmand F, Anoush G, Hosseini MJ, Anoush M. Grape seed oil as a natural therapy in male rats with alzheimer’s diseases. Adv Pharm Bull. 2020; 10(3):430-6. [DOI:10.34172/apb.2020.052] [PMID] [PMCID]
11.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am. 1957; 39-A(5):1027-42. [DOI:10.2106/00004623-195739050-00004]
12.Banaszkiewicz PA. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty: An end-result study using a new method of result evaluation. In: Banaszkiewicz PA, Kader DF, editors. Classic Papers in Orthopaedics. Basel: Springer; 2014. [DOI:10.1007/978-1-4471-5451-8_3]
13.Brooker AF, Bowerman JW, Robinson RA, Riley Jr LH. Ectopic ossification following total hip replacement: Incidence and a method of classification. Jbjs. 1973; 55(8):1629-32. [DOI:10.2106/00004623-197355080-00006]
14.Tazeabadi SA, Noroozi SG, Salehzadeh M, Bahardoust M, Farahini H, Hajializade M, et al. Evaluation of judet view radiographs accuracy in classification of acetabular fractures compared with three-dimensional computerized tomographic scan: A retrospective study. BMC Musculoskelet Disord. 2020; 21(1):405. [DOI:10.1186/s12891-020-03441-9] [PMID] [PMCID]
15.Hajializade M, Moghtadaei M, Mirzaei A, Abdollahi Kordkandi S, Babaheidarian P, Pazoki-Toroudi H, et al. Significant effect of simvastatin and/or ezetimibe-loaded nanofibers on the healing of femoral defect: An experimental study. Mater Sci Eng C Mater Biol Appl. 2020; 111:110861. [DOI: 10.1016/j.msec.2020.110861] [PMID]
16.Giordano V, Giordano M, Glória RC, de Souza FS, di Tullio P, Lages MM, et al. General principles for treatment of femoral head fractures. J Clin Orthop Trauma. 2019; 10(1):155-60. [DOI:10.1016/j.jcot.2017.07.013] [PMID] [PMCID]
17.Hayat Z, Varacallo M. Surgical management of femoral neck fractures. StatPearls [Internet]: StatPearls Publishing. 2019 [Updated 2020 Jun 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538236/
18.Scolaro JA, Marecek G, Firoozabadi R, Krieg JC, Lee M. Management and radiographic outcomes of femoral head fractures. J Orthop Traumatol. 2017; 18(3):235-41. [DOI:10.1007/s10195-017-0445-z] [PMID] [PMCID]
19.Bahardoust M, Hajializade M, Amiri R, Mousazadeh F, Pisoudeh K. Evaluation of health-related quality of life after total hip arthroplasty: A case-control study in the Iranian population. BMC Musculoskelet Disord. 2019; 20(1):46. [DOI:10.1186/s12891-019-2428-0] [PMID] [PMCID]
20.Pisoude K, Elahifar O, Sohrabi MB, Khajemozafari J. Comparison of proximal femur locking compression plate and intramedullary nailing in the treatment of sub-trochanteric fractures. J Res Orthop Sci. 2019; 6(2):0-0. [DOI:10.5812/soj.91166]
21.Yu X, Pang QJ, Chen XJ. Clinical results of femoral head fracture-dislocation treated according to the Pipkin classification. Pak J Med Sci. 2017; 33(3):650-3. [DOI:10.12669/pjms.333.12633] [PMID] [PMCID]
22.Tonetti J, Ruatti S, Lafontan V, Loubignac F, Chiron P, Sari-Ali H, et al. Is femoral head fracture-dislocation management improvable: A retrospective study in 110 cases. Orthop Traumatol: Surg Res. 2010; 96(6):623-31. [DOI:10.1016/j.otsr.2010.03.020] [PMID]
Received: 2020/03/25 | Accepted: 2020/06/13 | Published: 2020/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






