Volume 9, Issue 1 (2-2022)
JROS 2022, 9(1): 41-52 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mardani-Kivi M, Kazemnejad Leili E, Sharifi F, Azari Z. Return to Sports Activity in Anterior Cruciate Ligament Reconstruction: 4-Strand Hamstring vs Quadriceps Tendon. JROS 2022; 9 (1) :41-52
URL: http://jros.iums.ac.ir/article-1-2176-en.html
URL: http://jros.iums.ac.ir/article-1-2176-en.html
1- Ghaem Clinical Research Development Unit, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Statistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Anatomical Sciences & Cell Biology, Mashhad University of medical sciences, Mashhad, Iran.
2- Department of Statistics, School of Health, Guilan University of Medical Sciences, Rasht, Iran.
3- School of Health, Guilan University of Medical Sciences, Rasht, Iran.
4- Department of Anatomical Sciences & Cell Biology, Mashhad University of medical sciences, Mashhad, Iran.
Full-Text [PDF 796 kb]
(503 Downloads)
| Abstract (HTML) (1684 Views)
Full-Text: (587 Views)
1. Introduction
An anterior cruciate ligament (ACL) tear is the most common knee injury that requires surgical intervention. It is estimated that more than 100 000 ACL reconstructions are done each year in the United States [1]. The risk of an ACL tear in athletes is 10 times higher than in the general population; female athletes are 2 to 8 times more likely to be injured compared to male athletes [2, 3].
Even though numerous studies have reported various surgical techniques for ACL reconstruction with excellent clinical outcomes, graft type selection is still controversial [4]. The use of any type of graft is accompanied by special side effects. Examining these complications and their prevalence can help physicians and patients to choose the best treatment. Meanwhile, it is argued that hamstring tendons produce successful clinical results with minimal skin incision and complications of harvesting [5], and reduce the anterior knee pain and the pain while kneeling [6]. On the other hand, studies indicate that the reduction in the flexor force of the knee is an important disadvantage of the hamstring tendon [7]. According to conducted studies on quadriceps tendon autograft, we can expect to reduce the side effects of graft donation location; however, it seems that ACL reconstruction is lately being done by the bone-quadriceps tendon [1].
Objectives
The time to return to sport is a big challenge for athletes with an ACL tear and their physicians, and surely the type of graft is the determinant in returning to sport and its quality. On the other hand, the return to sport can be affected by various factors, such as associated lesions and knee pain rate. According to the above points and the high prevalence of ACL tear in athletes and considering the results of various studies on the type of appropriate graft, there is still no consensus on this issue. The present study aims to investigate the use of two grafts and their impact on return to sport in athlete patients referred to our university hospital from 2013 to 2016.
2. Methods
Study Protocol
This is a prospective cohort study that includes athletes who had undergone arthroscopic surgery from 2013 to 2016 at the orthopedic academic center for ACL rupture. These patients were referred to our orthopedic academic center and were candidates for ACL reconstructive surgery. They were divided randomly into two groups of 4-strand hamstring tendon autograft recipients and quadriceps autograft tendon recipients on the base of quadruple blocks. Then, they were followed up 3, 6, 12, and 24 months after surgery.
Ethical considerations
All patients were surgically treated by the orthopedic surgeon, the senior author of the study. This study was approved by the University’s Ethics Committee with the ethics number IR.GUMS.REC.1396.80. The study is also registered at the Iranian Registry of Clinical Trials (IRCT) (IRCT201706107274N13). All volunteers have signed a consent form before the study and their personal information will remain confidential.
Inclusion criteria
The inclusion criteria comprised the following items:
ACL rupture defined as +3 Lachman test in physical examination confirmed by knee Magnetic Resonance Imaging (MRI) as complete rupture;
Individuals in the age range of 18 to 50;
Regular exercisers, i.e., individuals who exercise 20 min or more 3 times a week or more;
Providing consent for participation in the study.
Exclusion criteria
The exclusion criteria comprised the following items:
Any history of knee surgery;
History of ACL rupture in the opposite knee;
Any injuries in knee ligaments other than lateral and medial meniscus;
Abnormal radiography of the knee;
Any signs or symptoms in hip or ankle;
ACL injuries caused by car accidents;
Multiple ligament injuries.
Formulation of the Questionnaires
The studied variables included age, sex, body mass index (BMI), type of exercise (soccer; martial arts; wrestling; ball sports, including volleyball, basketball, handball; and other sports), acute and or chronic infections, simultaneous injury in internal and external meniscus, chondral lesion, time to return to exercise, quality of return to exercise (similar to before the injury, weaker, no reluctance to continue, stopping), range of motion (ROM), Lachman test (+3-0), knee injury and osteoarthritis outcome (KOOS) score, and the Lysholm score. Meanwhile, the international knee documentation committee (IKDC) and KT-1000 (by arthrometer) were filled by the participants and the examiner.
Of the 278 patients with ACL rupture who were referred to our academic center, 173 were eligible for this study. Among them, 89 patients were operated on using 4-strand hamstring autograft tendons and 84 were operated on using quadriceps tendons. However, 139 patients (71 patients in the hamstring group and 68 patients in the quadriceps group) provided complete information, completed the questionnaires, and had complete follow-up references.
Surgical techniques
Surgery by hamstring autograft
The routine diagnostic arthroscopy was first performed to confirm the ACL tear and find any intra-articular pathology. A 3-cm anteromedial incision was made on the tibia approximately 4 cm distal to the joint surface and 3 cm medial to the tuberosity of the tibia. The pes anserine emerged by subcutaneous dissociation. Subcutaneous dissociation was done up to the tendon insertion on the tibial crest to maintain the maximum length. Toxic tendinosus and gracilis tendons with 10-mm tendon stripper of the tendon were removed from the abdominal muscle in the proximal site. A 4-layer graft was used for the ACL reconstruction. The arthroscopic method with the anteromedial portal technique was used to rim the femoral tunnel and then the tibia tunnel was embedded. The fixation of the femoral side was done by tibial endobutton and fixation through absorbable interference Misibio screw.
Surgery by quadriceps autograft
The routine diagnostic arthroscopy was first done to confirm the ACL tear and find any intra-articular pathology. Then, a strip with a width of 10-12 mm, a thickness of 7-8 cm, and a length of 90-110 mm was harvested from the quadriceps tendon in a 90-degree knee flexion with a longitudinal cut in the distal quadriceps’ tendon until the superior patella pole in a length of 3-5 cm. In the distal site, a bone block was harvested from the patella with a length of 20-25 mm. The harvesting of the quadriceps tendon was repaired with absorbable sutures. The graft was accurately measured and a tunnel with the appropriate size was created according to the diameter of the tendon in the femur and tibia. The femur tunnel was first created in the trans portal form, and then the tibia tunnel was created by a 1-2 cm incision in the medial proximal tibia. The desired graft was then placed in both tunnels so that the bone block was placed on the tibial tunnel side. The bioabsorbable interference screw of the same size as the tunnel was used to fixate the tendon on both sides of the femur and the tibia.
Statistical analysis
After data collection, they were recorded in the SPSS software, version 21. The data were also described according to the frequency and percentage as well as the mean, Standard Deviation (SD), and median. The Chi-square and Fisher exact tests were used to compare the frequency of the qualitative variables in two types of the studied grafts. In the case of normal distribution, the independent t test was used to compare scores in two studied grafts; otherwise, the Mann-Whitney test was used. The Mann-Whitney test was used to compare ranking variables in the two groups. The significance level of the tests was considered P<0.05.
3. Results
The present study investigated 139 patients with an ACL tear who were referred to our orthopedic academic center from 2013 to 2016. A total of 71 patients were operated on using the 4-layer hamstring autograft and 68 patients with quadriceps autograft tendon. The mean age of the patients was 31.5±1.25 years, and the highest age group was less than 30 years (47.48); meanwhile, the majority of the participants were male (84.17).
The distribution of age, sex, BMI, and sports group were the same and no statistically significant difference was observed in the two groups (P>0.05). Table 1 summarizes the demographic characteristics of the patients.
.jpg)
In the studied population, 26.47 of the patients in the quadriceps group and 16.90 in the hamstring group had a grade of 1 to 4 of the chondral lesion in the internal condyle, external condyle, internal plateau, and patella (P=0.170). However, there was no statistically significant difference between the two groups in terms of internal and external meniscus tear (P = 0.997). Table 2 presents the associated problems of the studied patients.
.jpg)
One person per group had knee pain during kneeling in the final follow-up (2 years after surgery). Furthermore, 4 subjects of the quadriceps group and 2 subjects of the hamstring group complained about anterior knee pain in the last follow-up (5.8 vs 2.8). Table 3 presents the degree of pain in kneeling and the anterior knee pain in two groups in all follow-up intervals. Acute infection was seen only in one patient in the hamstring group; the effective treatment was done and the patient achieved a complete recovery. None of the patients suffered from chronic infections.
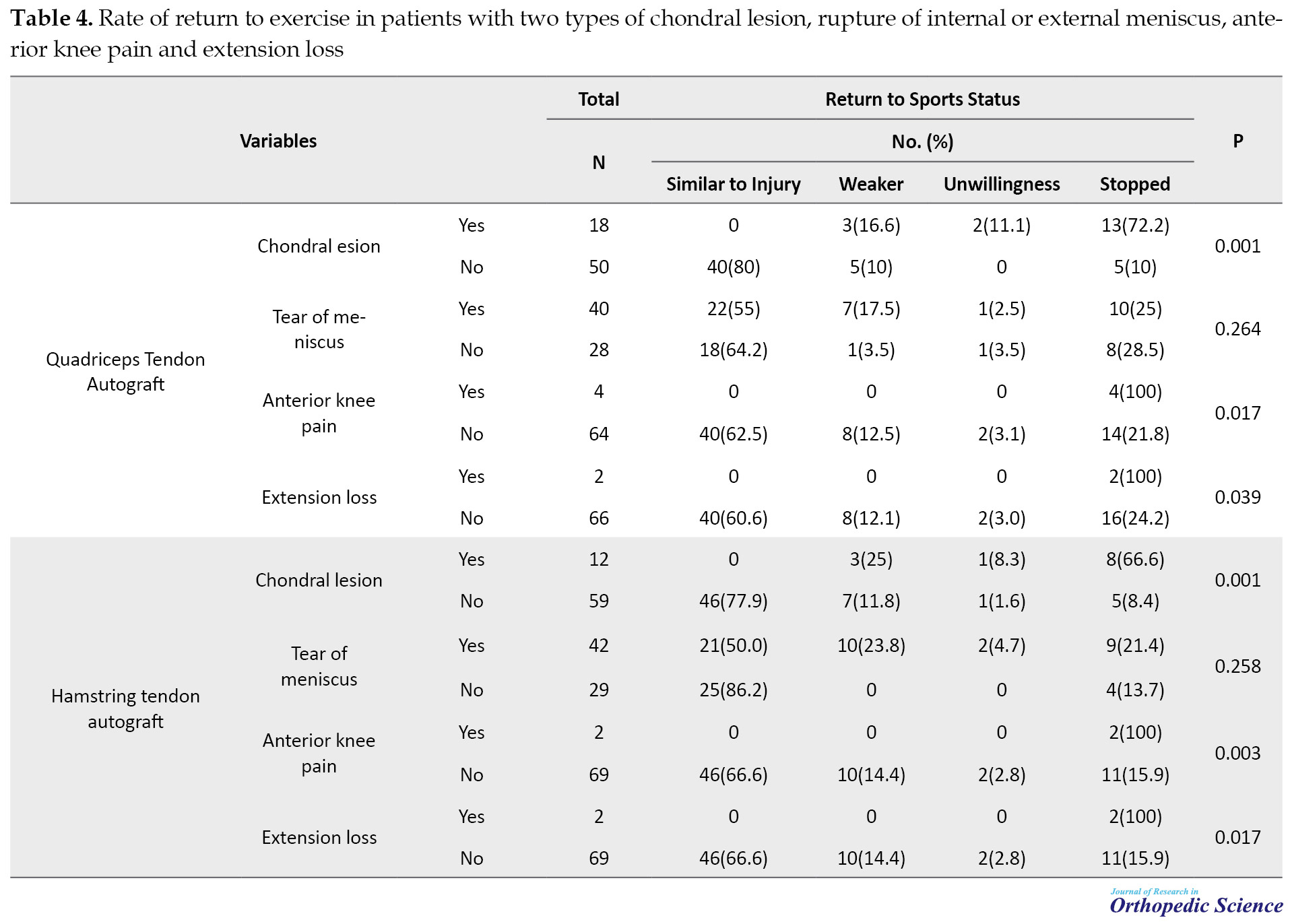
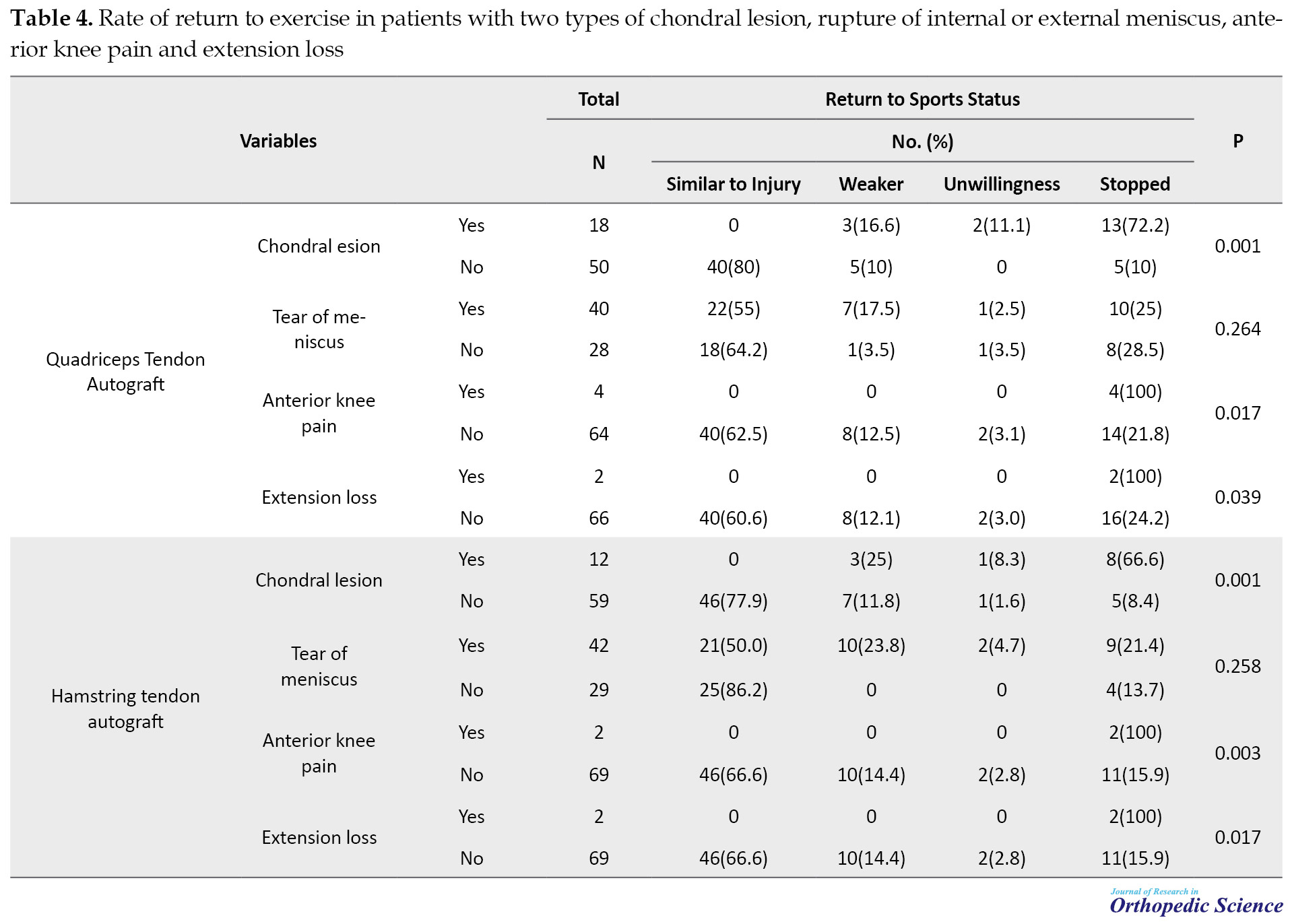
.jpg)
In the final follow-up (2 years after surgery), 2 patients of the quadriceps group and 2 patients of the hamstring group had extension loss of about 5 degrees. The flexion was complete with 135 degrees in all patients. The mean time of return to sport was 32.52±0.9 weeks in the quadriceps group and 31.36±1.44 in the hamstring group. Furthermore, 48 patients (71.64) of the quadriceps group and 56 patients (78.87) of the hamstring group returned to sports fields. Table 4 provides the rates of return to sport in patients of the two groups with the chondral lesion, internal or external meniscus tear, anterior knee pain, and extension loss.
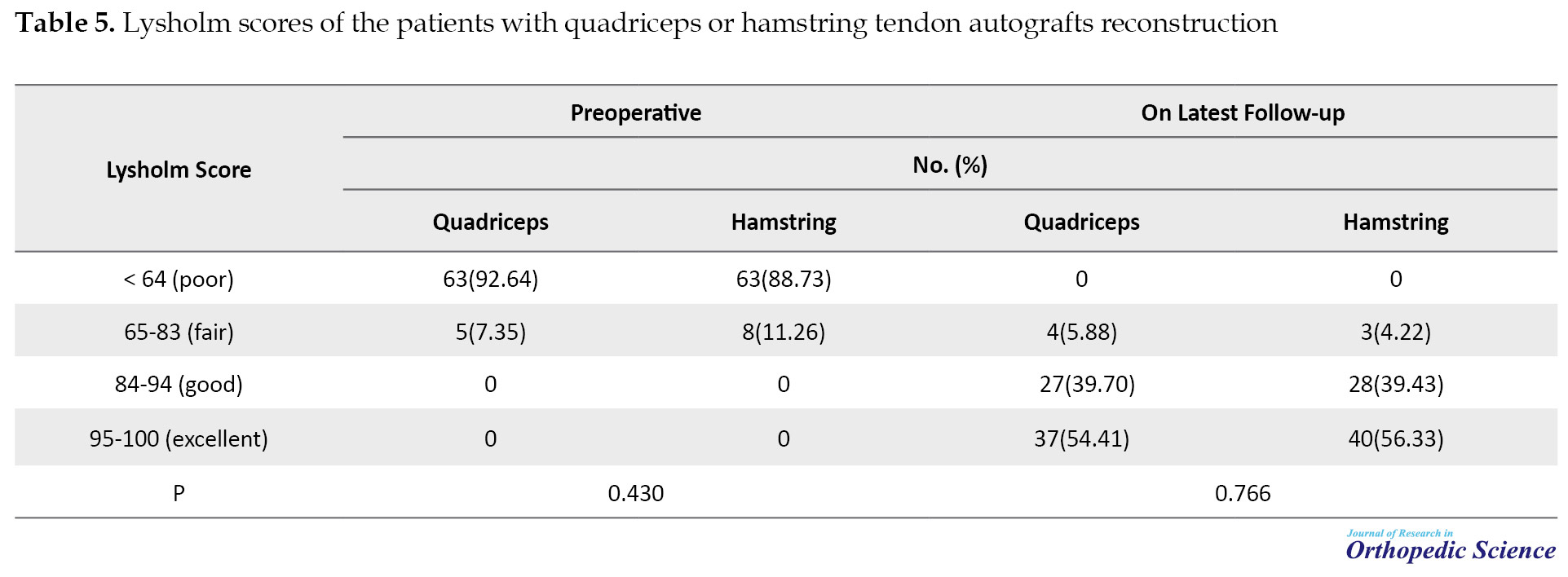
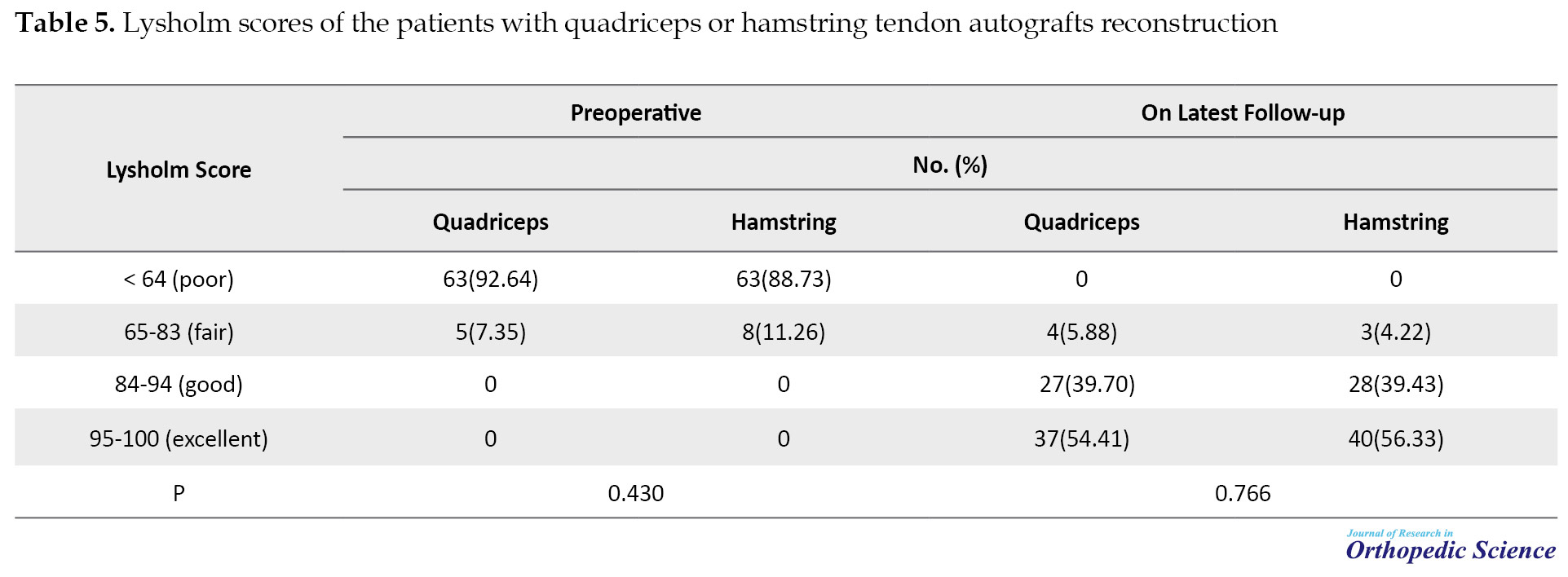
The Lysholm score had a significant improvement in both groups compared to pre-operation so 64 patients (94.11) of the quadriceps group and 68 patients (95.76) of the hamstring group had good to excellent results in the final follow-up (Table 5).
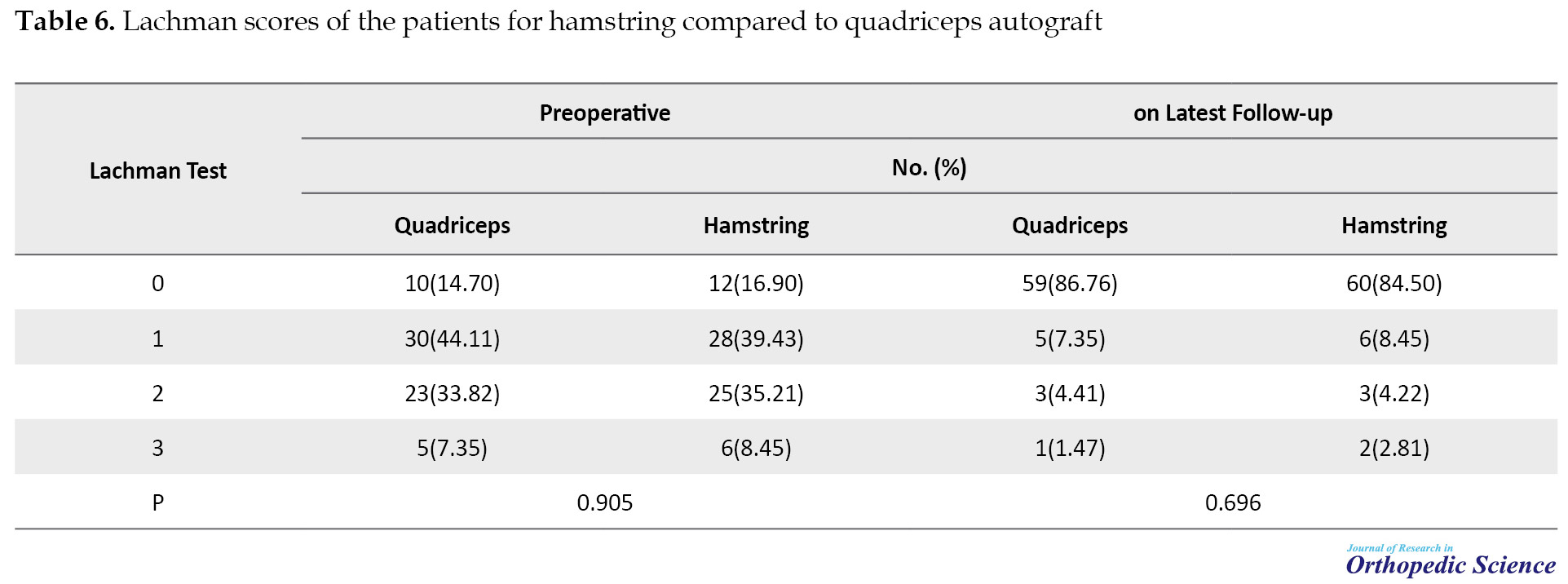
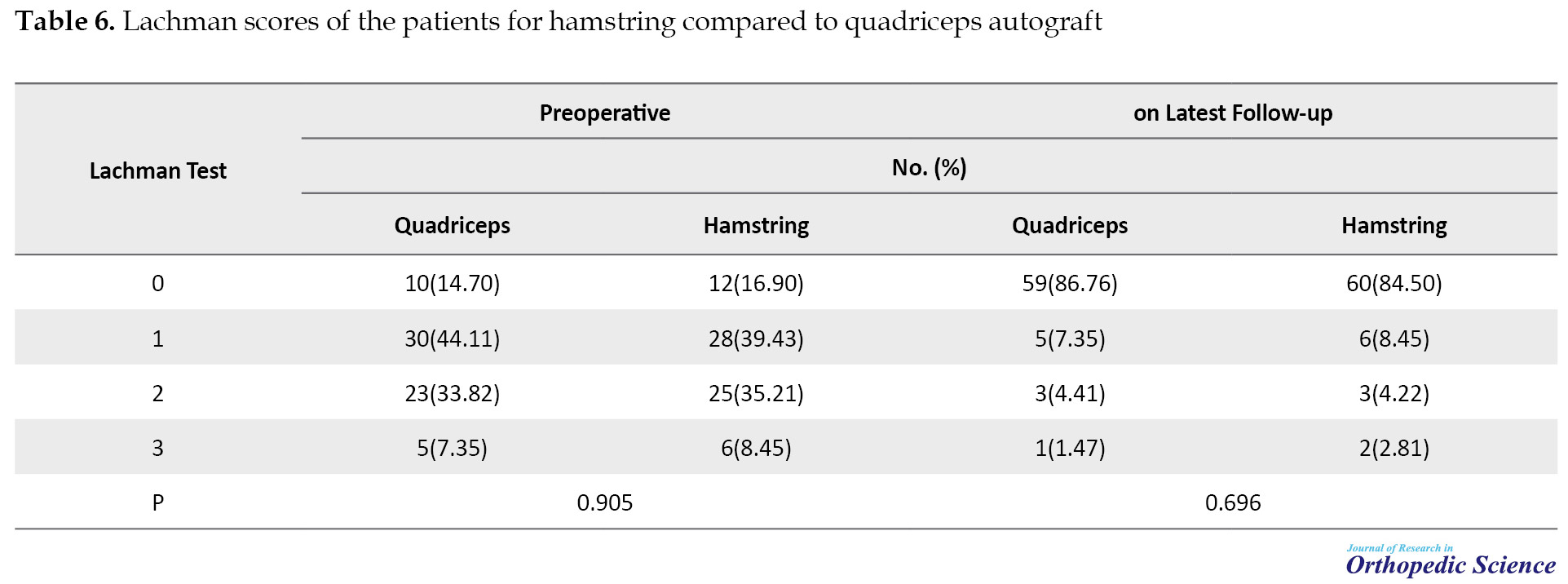
In the final follow-up, 59 patients (86.76) of the quadriceps group and 60 patients (84.50) of the hamstring group had zero Lachman test, and only 1 patient (1.47) of the quadriceps group and 2 patients (2.8) of the hamstring group had Lachman +3 (Table 6).
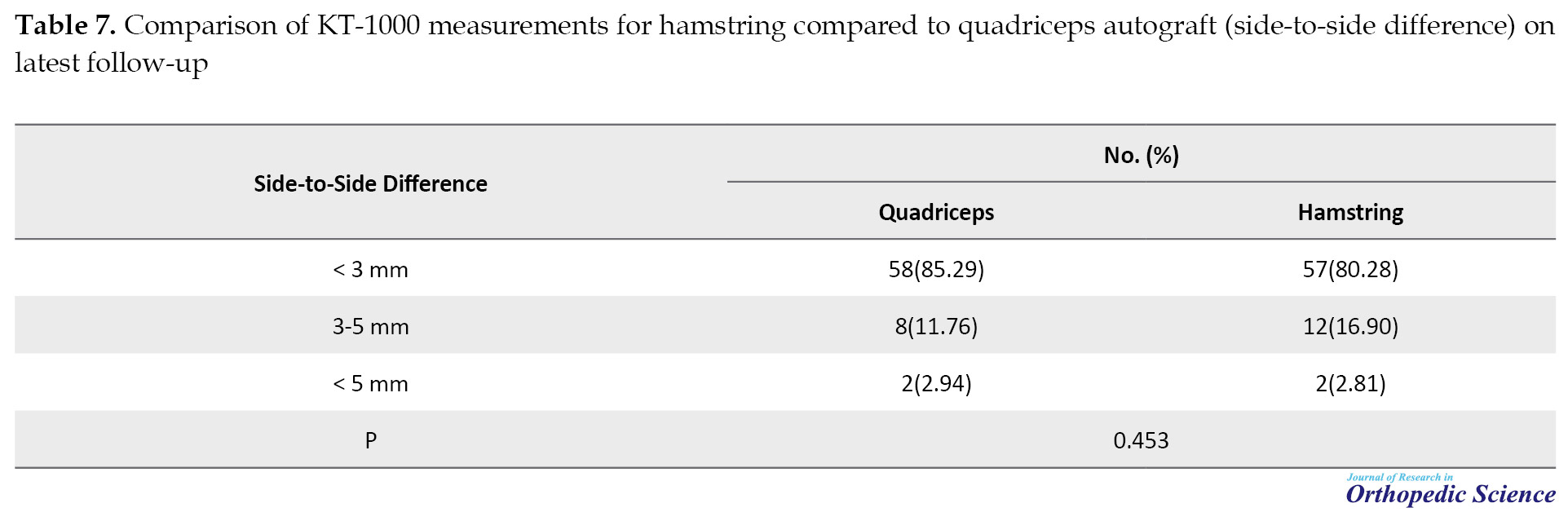
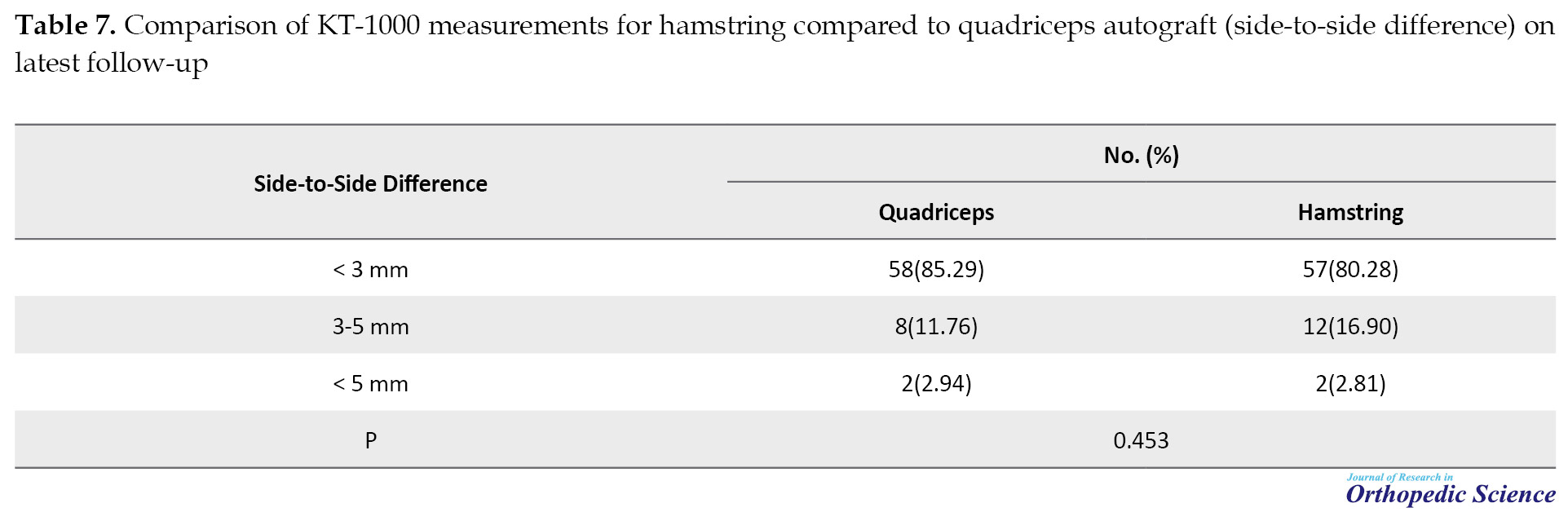
The KT-1000 tool was also used to assess knee stability. According to the results, 58 patients (85.29) of the quadriceps group and 57 patients (80.28) of the hamstring group had side-to-side differences of less than 3 mm (Table 7).
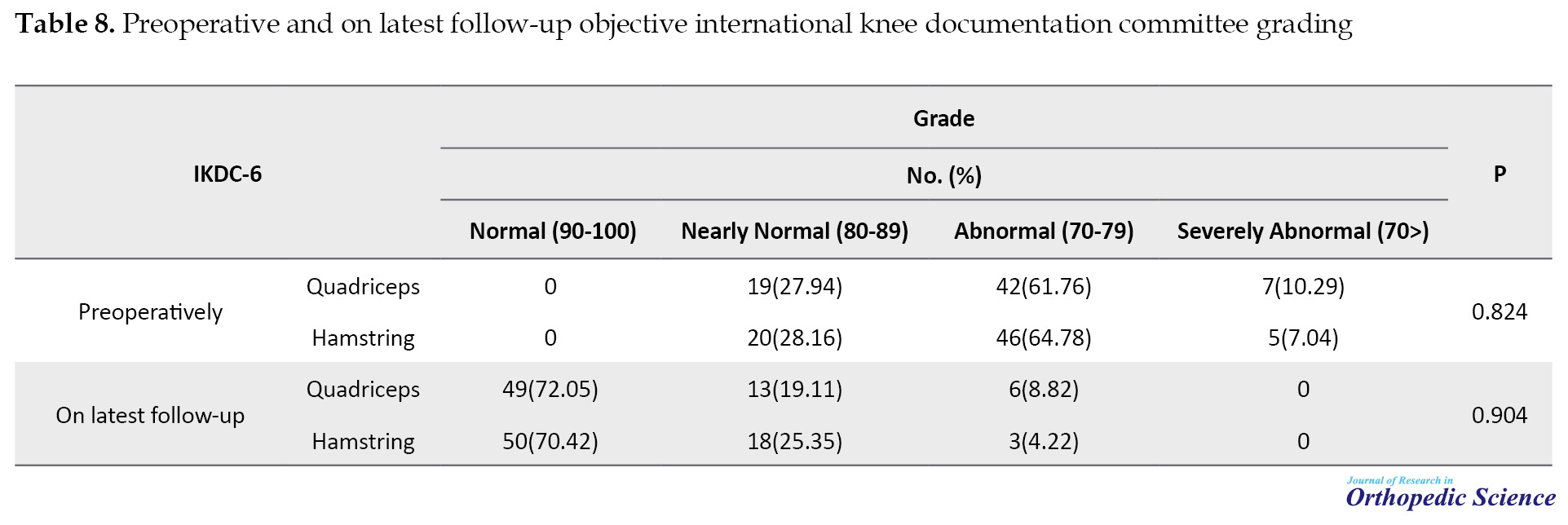
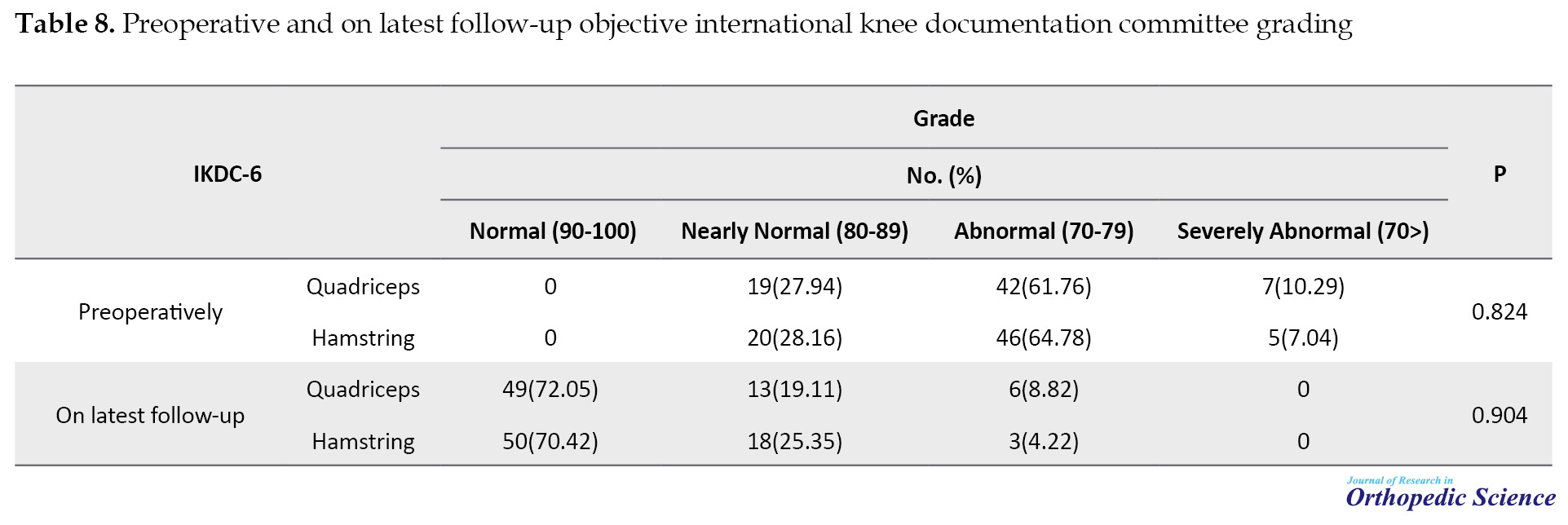
The IKDC tool was employed for all patients before surgery in the final follow-up and 49 patients (72.05) of the quadriceps group and 50 patients (70.42) of the hamstring group had normal IKDC (90-100) (Table 8).
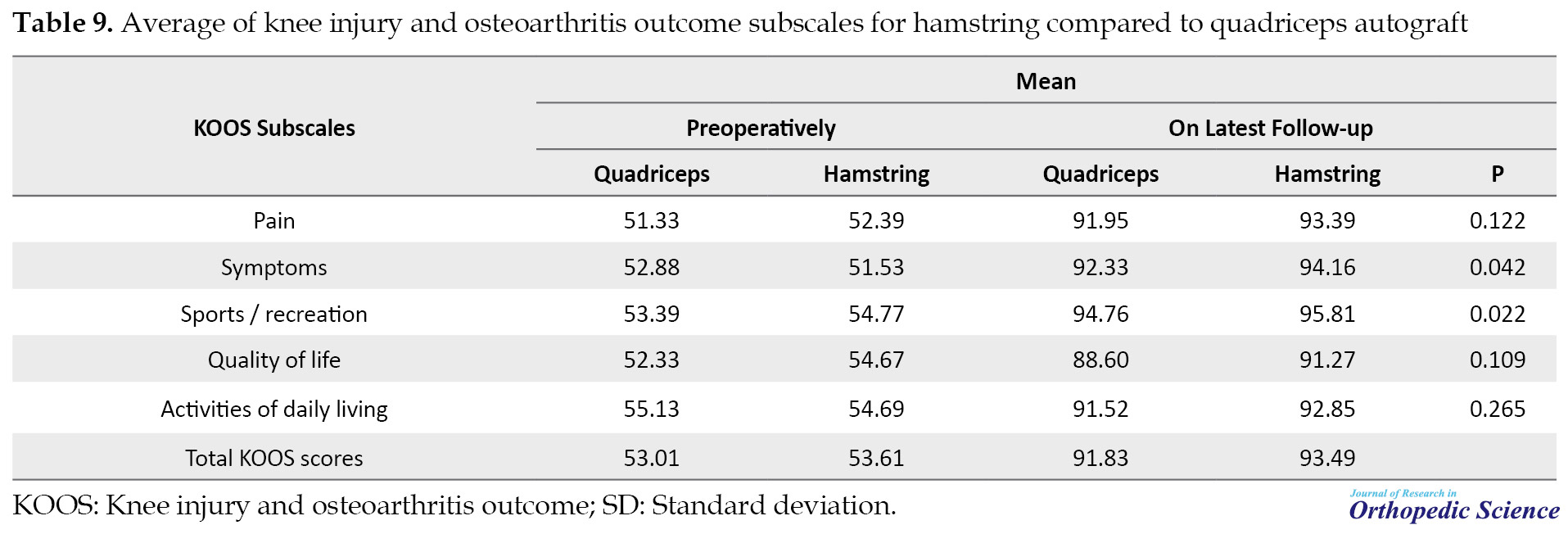
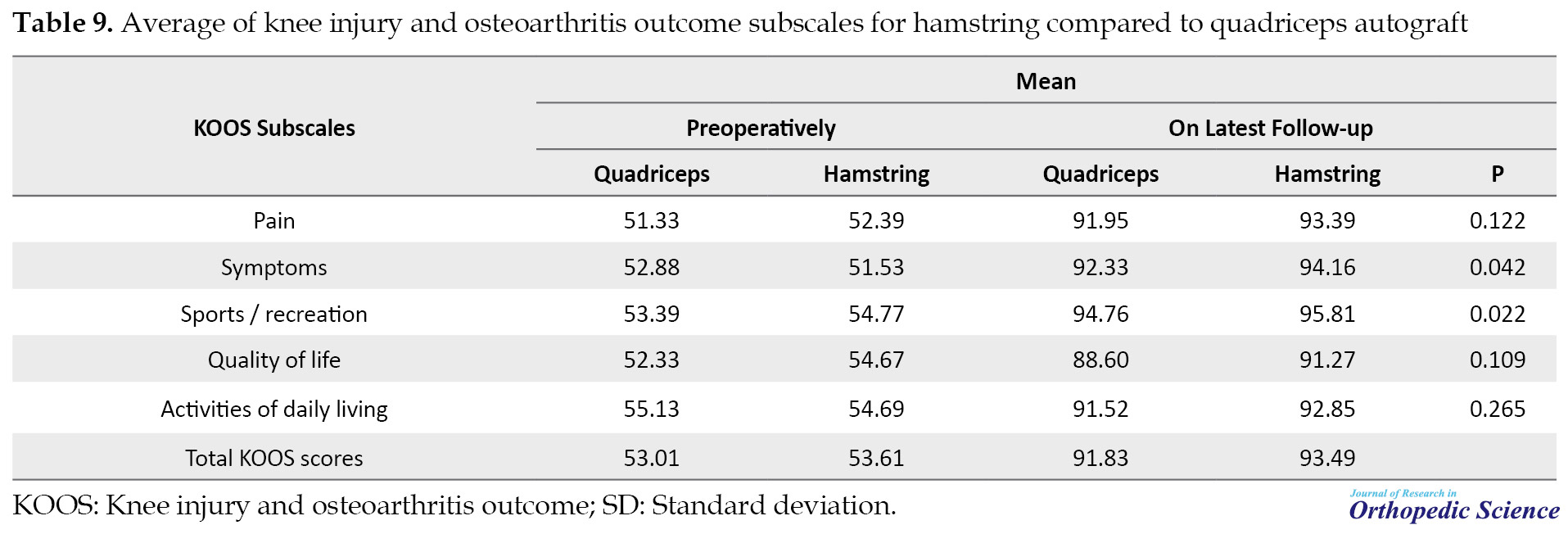
The KOOS tool, including 5 items namely pain, other symptoms, sports/ recreation, Quality of Life (QOL), and Activities of Daily Living (ADL) were studied in all patients and no significant difference was observed between the two groups in any of the subscales (Table 9).
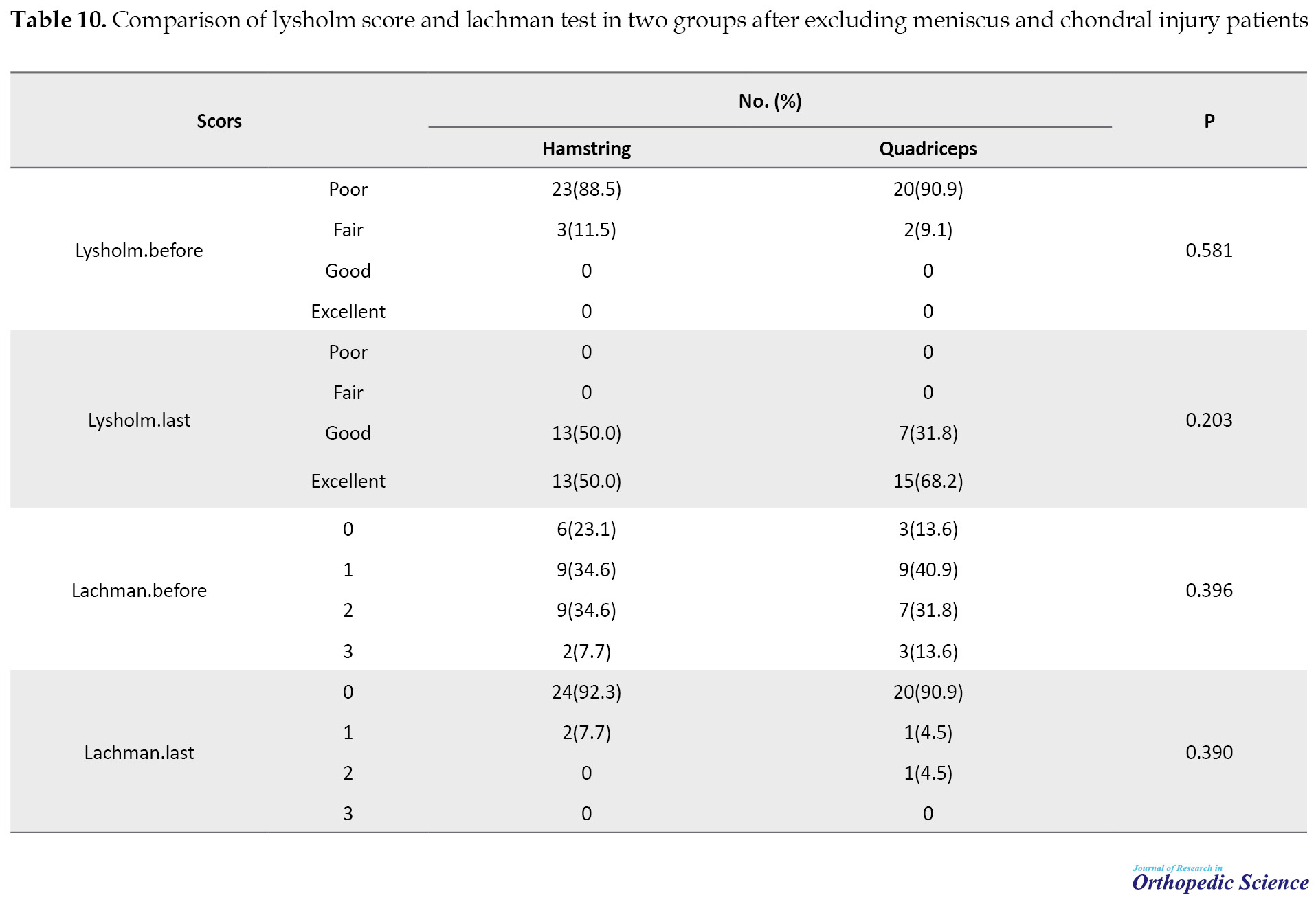
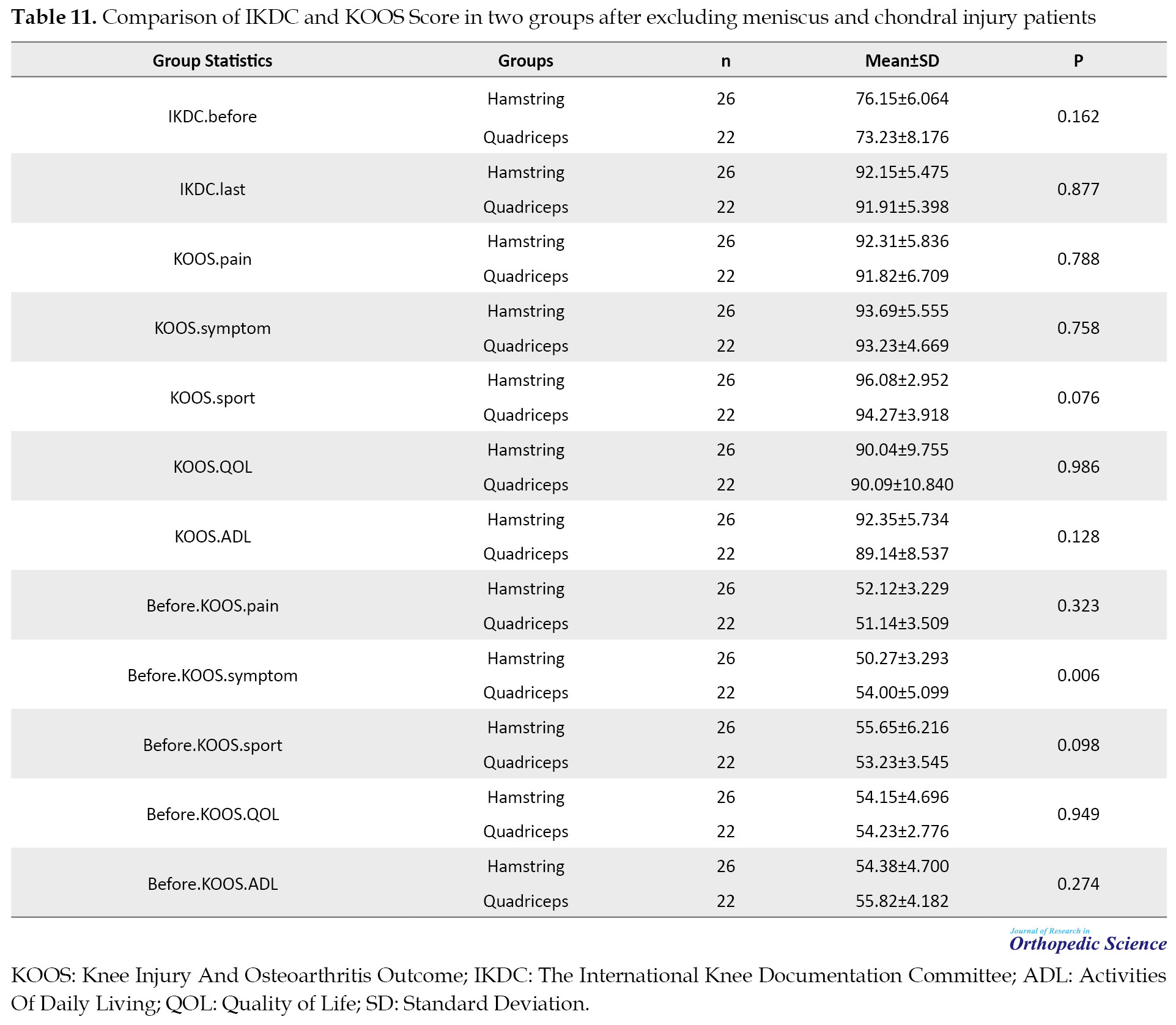
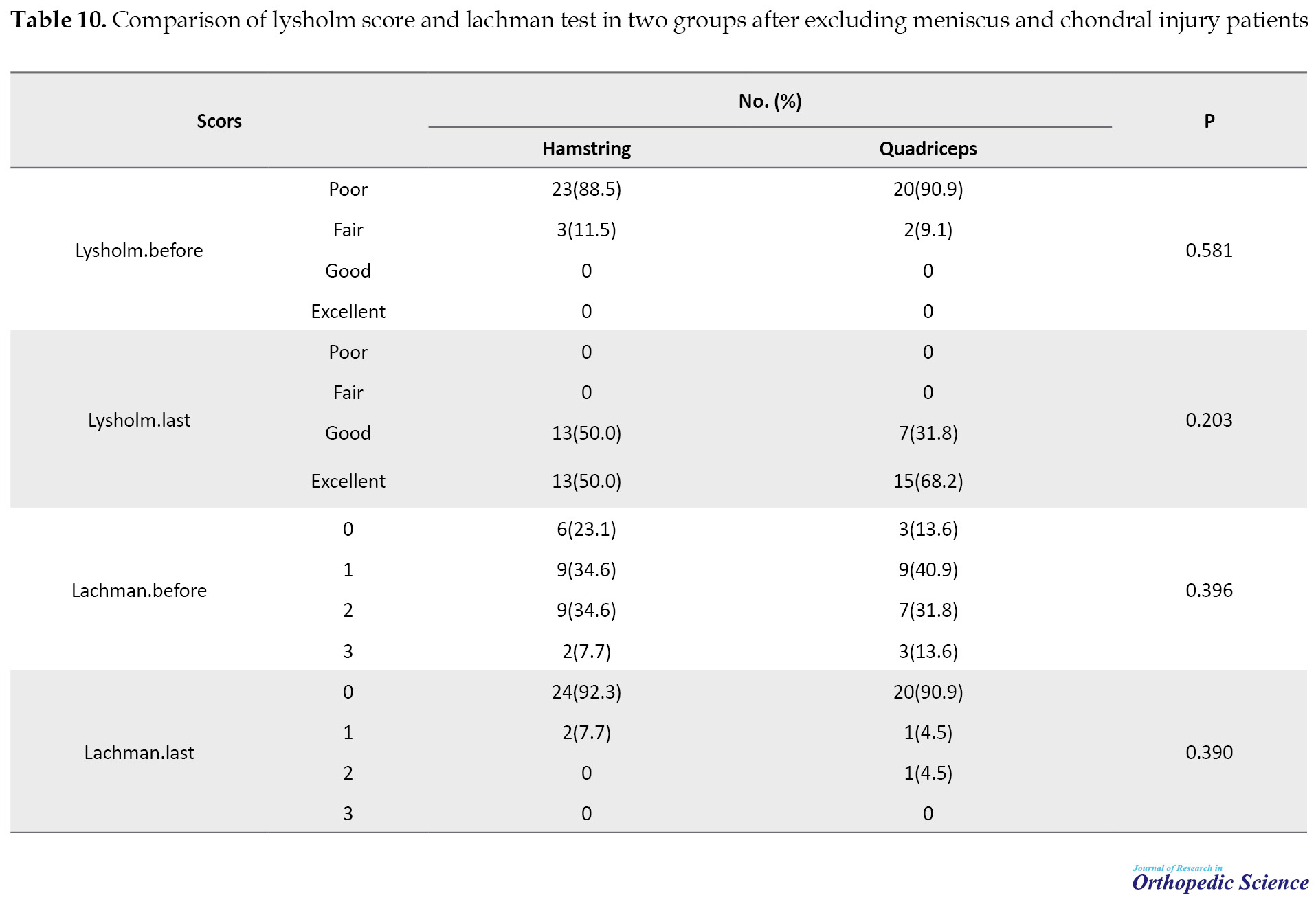
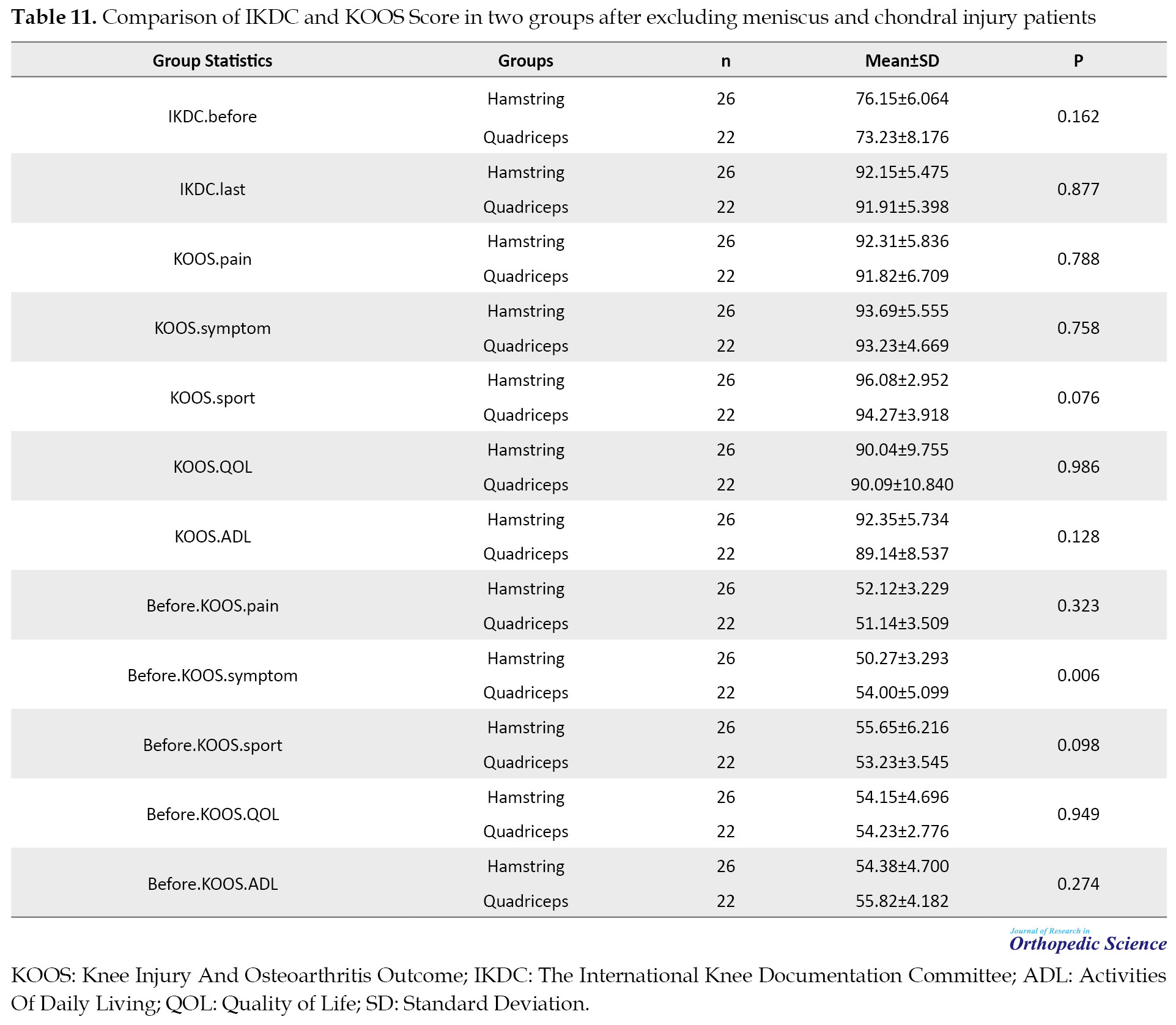
Also, the two study groups were compared after removing patients with a meniscus tear and chondral lesion and the results are shown in Table 10 and Table 11.
4. Discussion
Hamstring tendons are among the most commonly used grafts in the ACL reconstruction of the knee and they allow successful clinical outcomes with minimal skin incision, harvesting complications, and extensor mechanism dysfunction [5]. Quadriceps tendon autograft is also preferred in surgery revision or patients with multiple ligament injuries despite its less application [6]. In the present study, these two types of grafts were accurately investigated in 139 athletes with an ACL tear. In this study, there was no significant difference between the two groups in terms of age, sex, BMI, sport type, and tear of meniscus; hence, both groups matched in the above cases.
The return to sport is surely a challenging issue for athletes with ACL tear; hence, it is important to choose a graft that has the fastest time of return to sport with the same pre-injury quality. In the present study, the return to sport was more acceptable in the hamstring group compared to the quadriceps group, but it was not statistically significant (71.64 in the quadriceps group vs 78.87 in the hamstring group). In similar studies, the rate of return to sport after ACL reconstruction decreased to 67 [8] and 58 [9] by hamstring autograft, and 71 [10] by quadriceps tendon-patellar bone autograft, 65 by the patellar tendon, and hamstring graft, and 24 [11] by the full return to sport. However, a systematic survey reported that only 60 of non-elite athletes returned to a similar level of sports activities before the ACL tear [12]. In another study, more than 25 of athletes with ACL tear could not return to sport activity levels of before-ACL tear even after successful surgery and rehabilitation [13].
Meniscus tear and early onset of arthritis are the most important complications of an ACL tear. The prevalence of meniscus tear in the damaged knee was 40 in the first year, 60 in 5 years, and 80 in 10 years. The radiographic changes associated with osteoarthritis were reported in 60 to 90 of patients within 10 to 15 years after ACL tear [1, 14]. The associated injuries with an ACL tear, such as a chondral lesion certainly play important roles in returning to sports activities. Webster et al. found that patients with a chondral lesion, especially those with grades 3 and 4, had less chance to return to the same level of pre-injury sport [15]. However, it seems that problems, such as meniscus tear do not have any significant effect on the return to sport. According to a study by Anthony et al., patients with meniscus tear can have the same level of pre-injury sports by certain exercises [16]. The results of the present study also confirmed the results the above-mentioned studies. In the present research, 18 patients (26.4) of the quadriceps group and 12 patients (16.9) of the hamstring group had a chondral lesion. Furthermore, 57.8 of the quadriceps group and 59.1 of the hamstring group had an internal or external meniscus tear. However, among the patients with a meniscus tear, 72.5 of the quadriceps group and 73.8 of the hamstring group (more than 70 in both groups) returned to their sports activities. Among the patients with a chondral lesion, 16.6 in the quadriceps group and 25 in the hamstring group managed to continue their sports activities. Since the number of patients with chondral lesion did not match in both groups, the greater rate of return to sport in the hamstring group was probably associated with a lower rate of the chondral lesion in patients of this group. According to our results, the type of graft did not affect the return to sports in patients with the chondral lesion.
Knee pain is also an important factor in not returning to sports. Studies have found that the anterior knee pain and kneeling pain decrease in patients with a hamstring [6, 17], and this is perhaps another reason for the effect of more successful hamstring tendon surgery on the return to sports. In the present study, anterior knee pain in the final follow-up was observed in 4 patients of the quadriceps group and 2 patients of the hamstring group (5.88 vs 2.81). Although the anterior knee pain has a lower prevalence in quadriceps tendon graft compared to the bone-patellar tendon autograft, the anterior knee pain may have a lower prevalence in the hamstring tendon autograft compared to both quadriceps graft and bone-patellar tendon autograft. The present study found a link between anterior knee pain and non-return to sport, as none of the patients, who complained of anterior knee pain in the last follow-up, were unable to continue their sports activities. However, insufficient rehabilitation after ACL surgery is also an important reason for not returning to sports. Despite regular follow-ups of the patients, it was impossible to study the physiotherapy method after the surgery in the present study. In addition to pain, other reasons for not returning to sports include the lack of risk-taking, fear of re-injury, and inability to perform sports activities. Psychological factors affect the return to sport after ACL rupture [18]. Psychological factors and negative emotions, such as anxiety and fear can affect the patient’s return to sport as a challenging issue when they are injured and throughout the rehabilitation period [18]. Psychological readiness is a psychological factor in the field of return to sport after ACL rupture. Psychological readiness tests can be an important element in optimizing the return to sport rate [19] which was not investigated in the present study.
Extension loss is another factor in not returning to sports. According to the results of the present study, the extension loss of about 5 degrees was seen in 4 patients (2 patients of the hamstring group and 2 patients of the quadriceps group) in the last follow-up; and all 4 patients failed to return to their sports activities. Studies have found that the extension loss using the hamstring tendon largely decreased compared to the patella tendon graft. ACL reconstruction using the hamstring tendon maintained the extensor mechanism and prevents the muscle atrophy of the quadriceps [20]. In a study, the minor extension loss after the ACL reconstruction was much more common in patients with bone patellar tendon-bone autograft compared to hamstring [21]. In another study, the extension loss occurred in 52 of the bone patellar tendon bone autograft and 27 of the hamstring group [22]. Even though extension loss is an important advantage of hamstring graft, it seems that reducing the flexor force is an important disadvantage of this type of graft [7, 23]. In a study by Joon Kyu Lee et al., the knee joint stability and functional outcomes were similar in hamstring and quadriceps grafts, while the flexor muscle strength was better in bone quadriceps tendon grafts [24]. Svensson et al. also found that the use of an internal hamstring graft after arthroscopic repair of ACL could cause muscle weakness in the knee bending and delay healing the bonding site [25]. However, the flexor strength was complete in both groups and the same as before the tear in the present study. In any case, a precise and complete rehabilitation may decrease the probability of extension loss and reduced flexion in any graft, and increase the chance of returning to sports activities, as Shelborn and Tites argued that the post-operative rehabilitation program reduced the problem of short knee extension domain that was the common problem in the ACL reconstruction by bone patellar tendon bone autograft [26]. They also stated that if surgeons were not sure of the acceptance and follow-up of the post-operative physiotherapy program by the patients, they should recommend ACL reconstruction by hamstring graft. The achievement of the acceptable results in extension and excellent results in knee flexion in both groups was probably because of the successful rehabilitation in both groups in the present study.
According to our results, only one patient in the hamstring group was diagnosed with acute infection, and no disease was reported in the quadriceps group. In other studies, 2 patients [27] and 6 patients (out of 1318 patients) [17] had infections with hamstring autograft. In another study, there was no case of infection in patients by semitendinosus-gracilis and quadriceps autograft [28]. The results of the above-mentioned studies were consistent with the present study. Although the failure to observe any case of infection was not statistically significant in the quadriceps group compared to the hamstring group, it can be a positive point in using the quadriceps tendon autograft in the present study.
Based on the present study, the indices, namely KT-1000, the Lysholm, and the Luchman significantly improved in the final follow-up as indices for assessing knee stability. A total of 86.7 of the quadriceps group and 84.5 of the hamstring group had zero Luchman and KT-1000 was less than 3 mm in 85.2 of the quadriceps group and 80.2 of the hamstring group. The results indicated a relatively similar improvement in patients of both groups. Another two studies found the same stability between hamstring and quadriceps grafts of bone-quadriceps tendon via arthrometric and manual methods [29, 30]. Our results were better than some studies [31] and similar to other studies [1, 32, 33].
According to Svensson et al., although hamstring graft has no complications, such as patellofemoral pain, weakness of the quadriceps femoris muscle, and patella fracture like bone patellar tendon bone autograft, it has other side effects, such as post-operative knee instability [25]. Several meta-analyses also indicated that in the case of using hamstring grafts, the joint laxity increased, but fewer complications occurred in the graft harvesting site [34]. However, there was no significant difference between the two groups in terms of knee stability in the present study.
In the present study, the IKDC and KOOS score values indicated significant improvement in both groups as the functional knee criteria in the final follow-up. In a study by Leiter et al., IKDC was normal (90-100) in 75 of the patients with a hamstring [35]. In a study by Leys et al., the mean IKDC was 90 (normal) in the hamstring group [36]. Furthermore, Charlton et al. also reported the mean IKDC equal to 81 (nearly normal) in patients with hamstring tendon graft and bio-absorbable interference screw fixation [37]. On the other hand, in a study by Lee et al., the IKDC score had a grade of A or B (normal and nearly normal) in 94 of patients who were treated with quadriceps autograft [1]. In the present study, 72.05 of patients in the quadriceps group and 70.42 in the hamstring group had normal IKDC. However, no significant difference was observed between the IKDC score and all KOOS subscales scores in patients of both groups in the final follow-up.
Similar to the present study, Kim et al. found a significant difference in functional outcomes between bone quadriceps tendon and single-bundle hamstring tendon graft [37].
Relatively small sizes of the groups were among the limitations of the present study because we only used the information of the patients who were present in all follow-up intervals and had complete and accurate information.
However, the presence of only a surgeon to perform all surgeries and having matched participants of both groups in terms of age, sex, athletic groups, and meniscus tear made the results of the present study more valuable and comparable.
5. Conclusion
According to the results of the present study, the rate of return to sport in patients with quadriceps autografts was slightly lower than in patients with hamstring autografts in a 2-year follow-up of athletes with an ACL tear. This reduction was probably because of the higher chondral lesion in quadriceps group patients. There were no significant differences in results of the both groups. It seems that orthopedic surgeons should be responsible for selecting suitable grafts for patients with an ACL tear to make the best decisions by considering post-operative rehabilitation conditions and methods.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Guilan University’s Ethics Committee with the ethics number IR.GUMS.REC.1396.80. The study is also registered at the Iranian Registry of Clinical Trials (Code: IRCT201706107274N13). All volunteers have signed a consent form before the study and their personal information will remain confidential.
Funding
This research was supported by the research project (No. 2038), Funded by the Guilan University of Medical Sciences.
Authors' contributions
Conceptualization and supervision: Mohsen Mardani-Kivi, Zoleikha azari; Methodology: Mohsen Mardani-Kivi, Fateme Sharifi; Investigation, writing-original draft, and writing-review & editing: All authors; Data collection: Fatemeh Sharifi, Zoleikha Azari; Data analysis: Ehsan Kazemnezhad Leili; Funding acquisition and resources: Mohsen Mardani-Kivi.
Conflict of interest
The authors declared no conflict of interest.
References
An anterior cruciate ligament (ACL) tear is the most common knee injury that requires surgical intervention. It is estimated that more than 100 000 ACL reconstructions are done each year in the United States [1]. The risk of an ACL tear in athletes is 10 times higher than in the general population; female athletes are 2 to 8 times more likely to be injured compared to male athletes [2, 3].
Even though numerous studies have reported various surgical techniques for ACL reconstruction with excellent clinical outcomes, graft type selection is still controversial [4]. The use of any type of graft is accompanied by special side effects. Examining these complications and their prevalence can help physicians and patients to choose the best treatment. Meanwhile, it is argued that hamstring tendons produce successful clinical results with minimal skin incision and complications of harvesting [5], and reduce the anterior knee pain and the pain while kneeling [6]. On the other hand, studies indicate that the reduction in the flexor force of the knee is an important disadvantage of the hamstring tendon [7]. According to conducted studies on quadriceps tendon autograft, we can expect to reduce the side effects of graft donation location; however, it seems that ACL reconstruction is lately being done by the bone-quadriceps tendon [1].
Objectives
The time to return to sport is a big challenge for athletes with an ACL tear and their physicians, and surely the type of graft is the determinant in returning to sport and its quality. On the other hand, the return to sport can be affected by various factors, such as associated lesions and knee pain rate. According to the above points and the high prevalence of ACL tear in athletes and considering the results of various studies on the type of appropriate graft, there is still no consensus on this issue. The present study aims to investigate the use of two grafts and their impact on return to sport in athlete patients referred to our university hospital from 2013 to 2016.
2. Methods
Study Protocol
This is a prospective cohort study that includes athletes who had undergone arthroscopic surgery from 2013 to 2016 at the orthopedic academic center for ACL rupture. These patients were referred to our orthopedic academic center and were candidates for ACL reconstructive surgery. They were divided randomly into two groups of 4-strand hamstring tendon autograft recipients and quadriceps autograft tendon recipients on the base of quadruple blocks. Then, they were followed up 3, 6, 12, and 24 months after surgery.
Ethical considerations
All patients were surgically treated by the orthopedic surgeon, the senior author of the study. This study was approved by the University’s Ethics Committee with the ethics number IR.GUMS.REC.1396.80. The study is also registered at the Iranian Registry of Clinical Trials (IRCT) (IRCT201706107274N13). All volunteers have signed a consent form before the study and their personal information will remain confidential.
Inclusion criteria
The inclusion criteria comprised the following items:
ACL rupture defined as +3 Lachman test in physical examination confirmed by knee Magnetic Resonance Imaging (MRI) as complete rupture;
Individuals in the age range of 18 to 50;
Regular exercisers, i.e., individuals who exercise 20 min or more 3 times a week or more;
Providing consent for participation in the study.
Exclusion criteria
The exclusion criteria comprised the following items:
Any history of knee surgery;
History of ACL rupture in the opposite knee;
Any injuries in knee ligaments other than lateral and medial meniscus;
Abnormal radiography of the knee;
Any signs or symptoms in hip or ankle;
ACL injuries caused by car accidents;
Multiple ligament injuries.
Formulation of the Questionnaires
The studied variables included age, sex, body mass index (BMI), type of exercise (soccer; martial arts; wrestling; ball sports, including volleyball, basketball, handball; and other sports), acute and or chronic infections, simultaneous injury in internal and external meniscus, chondral lesion, time to return to exercise, quality of return to exercise (similar to before the injury, weaker, no reluctance to continue, stopping), range of motion (ROM), Lachman test (+3-0), knee injury and osteoarthritis outcome (KOOS) score, and the Lysholm score. Meanwhile, the international knee documentation committee (IKDC) and KT-1000 (by arthrometer) were filled by the participants and the examiner.
Of the 278 patients with ACL rupture who were referred to our academic center, 173 were eligible for this study. Among them, 89 patients were operated on using 4-strand hamstring autograft tendons and 84 were operated on using quadriceps tendons. However, 139 patients (71 patients in the hamstring group and 68 patients in the quadriceps group) provided complete information, completed the questionnaires, and had complete follow-up references.
Surgical techniques
Surgery by hamstring autograft
The routine diagnostic arthroscopy was first performed to confirm the ACL tear and find any intra-articular pathology. A 3-cm anteromedial incision was made on the tibia approximately 4 cm distal to the joint surface and 3 cm medial to the tuberosity of the tibia. The pes anserine emerged by subcutaneous dissociation. Subcutaneous dissociation was done up to the tendon insertion on the tibial crest to maintain the maximum length. Toxic tendinosus and gracilis tendons with 10-mm tendon stripper of the tendon were removed from the abdominal muscle in the proximal site. A 4-layer graft was used for the ACL reconstruction. The arthroscopic method with the anteromedial portal technique was used to rim the femoral tunnel and then the tibia tunnel was embedded. The fixation of the femoral side was done by tibial endobutton and fixation through absorbable interference Misibio screw.
Surgery by quadriceps autograft
The routine diagnostic arthroscopy was first done to confirm the ACL tear and find any intra-articular pathology. Then, a strip with a width of 10-12 mm, a thickness of 7-8 cm, and a length of 90-110 mm was harvested from the quadriceps tendon in a 90-degree knee flexion with a longitudinal cut in the distal quadriceps’ tendon until the superior patella pole in a length of 3-5 cm. In the distal site, a bone block was harvested from the patella with a length of 20-25 mm. The harvesting of the quadriceps tendon was repaired with absorbable sutures. The graft was accurately measured and a tunnel with the appropriate size was created according to the diameter of the tendon in the femur and tibia. The femur tunnel was first created in the trans portal form, and then the tibia tunnel was created by a 1-2 cm incision in the medial proximal tibia. The desired graft was then placed in both tunnels so that the bone block was placed on the tibial tunnel side. The bioabsorbable interference screw of the same size as the tunnel was used to fixate the tendon on both sides of the femur and the tibia.
Statistical analysis
After data collection, they were recorded in the SPSS software, version 21. The data were also described according to the frequency and percentage as well as the mean, Standard Deviation (SD), and median. The Chi-square and Fisher exact tests were used to compare the frequency of the qualitative variables in two types of the studied grafts. In the case of normal distribution, the independent t test was used to compare scores in two studied grafts; otherwise, the Mann-Whitney test was used. The Mann-Whitney test was used to compare ranking variables in the two groups. The significance level of the tests was considered P<0.05.
3. Results
The present study investigated 139 patients with an ACL tear who were referred to our orthopedic academic center from 2013 to 2016. A total of 71 patients were operated on using the 4-layer hamstring autograft and 68 patients with quadriceps autograft tendon. The mean age of the patients was 31.5±1.25 years, and the highest age group was less than 30 years (47.48); meanwhile, the majority of the participants were male (84.17).
The distribution of age, sex, BMI, and sports group were the same and no statistically significant difference was observed in the two groups (P>0.05). Table 1 summarizes the demographic characteristics of the patients.
.jpg)
In the studied population, 26.47 of the patients in the quadriceps group and 16.90 in the hamstring group had a grade of 1 to 4 of the chondral lesion in the internal condyle, external condyle, internal plateau, and patella (P=0.170). However, there was no statistically significant difference between the two groups in terms of internal and external meniscus tear (P = 0.997). Table 2 presents the associated problems of the studied patients.
.jpg)
One person per group had knee pain during kneeling in the final follow-up (2 years after surgery). Furthermore, 4 subjects of the quadriceps group and 2 subjects of the hamstring group complained about anterior knee pain in the last follow-up (5.8 vs 2.8). Table 3 presents the degree of pain in kneeling and the anterior knee pain in two groups in all follow-up intervals. Acute infection was seen only in one patient in the hamstring group; the effective treatment was done and the patient achieved a complete recovery. None of the patients suffered from chronic infections.
.jpg)
In the final follow-up (2 years after surgery), 2 patients of the quadriceps group and 2 patients of the hamstring group had extension loss of about 5 degrees. The flexion was complete with 135 degrees in all patients. The mean time of return to sport was 32.52±0.9 weeks in the quadriceps group and 31.36±1.44 in the hamstring group. Furthermore, 48 patients (71.64) of the quadriceps group and 56 patients (78.87) of the hamstring group returned to sports fields. Table 4 provides the rates of return to sport in patients of the two groups with the chondral lesion, internal or external meniscus tear, anterior knee pain, and extension loss.
The Lysholm score had a significant improvement in both groups compared to pre-operation so 64 patients (94.11) of the quadriceps group and 68 patients (95.76) of the hamstring group had good to excellent results in the final follow-up (Table 5).
In the final follow-up, 59 patients (86.76) of the quadriceps group and 60 patients (84.50) of the hamstring group had zero Lachman test, and only 1 patient (1.47) of the quadriceps group and 2 patients (2.8) of the hamstring group had Lachman +3 (Table 6).
The KT-1000 tool was also used to assess knee stability. According to the results, 58 patients (85.29) of the quadriceps group and 57 patients (80.28) of the hamstring group had side-to-side differences of less than 3 mm (Table 7).
The IKDC tool was employed for all patients before surgery in the final follow-up and 49 patients (72.05) of the quadriceps group and 50 patients (70.42) of the hamstring group had normal IKDC (90-100) (Table 8).
The KOOS tool, including 5 items namely pain, other symptoms, sports/ recreation, Quality of Life (QOL), and Activities of Daily Living (ADL) were studied in all patients and no significant difference was observed between the two groups in any of the subscales (Table 9).
Also, the two study groups were compared after removing patients with a meniscus tear and chondral lesion and the results are shown in Table 10 and Table 11.
4. Discussion
Hamstring tendons are among the most commonly used grafts in the ACL reconstruction of the knee and they allow successful clinical outcomes with minimal skin incision, harvesting complications, and extensor mechanism dysfunction [5]. Quadriceps tendon autograft is also preferred in surgery revision or patients with multiple ligament injuries despite its less application [6]. In the present study, these two types of grafts were accurately investigated in 139 athletes with an ACL tear. In this study, there was no significant difference between the two groups in terms of age, sex, BMI, sport type, and tear of meniscus; hence, both groups matched in the above cases.
The return to sport is surely a challenging issue for athletes with ACL tear; hence, it is important to choose a graft that has the fastest time of return to sport with the same pre-injury quality. In the present study, the return to sport was more acceptable in the hamstring group compared to the quadriceps group, but it was not statistically significant (71.64 in the quadriceps group vs 78.87 in the hamstring group). In similar studies, the rate of return to sport after ACL reconstruction decreased to 67 [8] and 58 [9] by hamstring autograft, and 71 [10] by quadriceps tendon-patellar bone autograft, 65 by the patellar tendon, and hamstring graft, and 24 [11] by the full return to sport. However, a systematic survey reported that only 60 of non-elite athletes returned to a similar level of sports activities before the ACL tear [12]. In another study, more than 25 of athletes with ACL tear could not return to sport activity levels of before-ACL tear even after successful surgery and rehabilitation [13].
Meniscus tear and early onset of arthritis are the most important complications of an ACL tear. The prevalence of meniscus tear in the damaged knee was 40 in the first year, 60 in 5 years, and 80 in 10 years. The radiographic changes associated with osteoarthritis were reported in 60 to 90 of patients within 10 to 15 years after ACL tear [1, 14]. The associated injuries with an ACL tear, such as a chondral lesion certainly play important roles in returning to sports activities. Webster et al. found that patients with a chondral lesion, especially those with grades 3 and 4, had less chance to return to the same level of pre-injury sport [15]. However, it seems that problems, such as meniscus tear do not have any significant effect on the return to sport. According to a study by Anthony et al., patients with meniscus tear can have the same level of pre-injury sports by certain exercises [16]. The results of the present study also confirmed the results the above-mentioned studies. In the present research, 18 patients (26.4) of the quadriceps group and 12 patients (16.9) of the hamstring group had a chondral lesion. Furthermore, 57.8 of the quadriceps group and 59.1 of the hamstring group had an internal or external meniscus tear. However, among the patients with a meniscus tear, 72.5 of the quadriceps group and 73.8 of the hamstring group (more than 70 in both groups) returned to their sports activities. Among the patients with a chondral lesion, 16.6 in the quadriceps group and 25 in the hamstring group managed to continue their sports activities. Since the number of patients with chondral lesion did not match in both groups, the greater rate of return to sport in the hamstring group was probably associated with a lower rate of the chondral lesion in patients of this group. According to our results, the type of graft did not affect the return to sports in patients with the chondral lesion.
Knee pain is also an important factor in not returning to sports. Studies have found that the anterior knee pain and kneeling pain decrease in patients with a hamstring [6, 17], and this is perhaps another reason for the effect of more successful hamstring tendon surgery on the return to sports. In the present study, anterior knee pain in the final follow-up was observed in 4 patients of the quadriceps group and 2 patients of the hamstring group (5.88 vs 2.81). Although the anterior knee pain has a lower prevalence in quadriceps tendon graft compared to the bone-patellar tendon autograft, the anterior knee pain may have a lower prevalence in the hamstring tendon autograft compared to both quadriceps graft and bone-patellar tendon autograft. The present study found a link between anterior knee pain and non-return to sport, as none of the patients, who complained of anterior knee pain in the last follow-up, were unable to continue their sports activities. However, insufficient rehabilitation after ACL surgery is also an important reason for not returning to sports. Despite regular follow-ups of the patients, it was impossible to study the physiotherapy method after the surgery in the present study. In addition to pain, other reasons for not returning to sports include the lack of risk-taking, fear of re-injury, and inability to perform sports activities. Psychological factors affect the return to sport after ACL rupture [18]. Psychological factors and negative emotions, such as anxiety and fear can affect the patient’s return to sport as a challenging issue when they are injured and throughout the rehabilitation period [18]. Psychological readiness is a psychological factor in the field of return to sport after ACL rupture. Psychological readiness tests can be an important element in optimizing the return to sport rate [19] which was not investigated in the present study.
Extension loss is another factor in not returning to sports. According to the results of the present study, the extension loss of about 5 degrees was seen in 4 patients (2 patients of the hamstring group and 2 patients of the quadriceps group) in the last follow-up; and all 4 patients failed to return to their sports activities. Studies have found that the extension loss using the hamstring tendon largely decreased compared to the patella tendon graft. ACL reconstruction using the hamstring tendon maintained the extensor mechanism and prevents the muscle atrophy of the quadriceps [20]. In a study, the minor extension loss after the ACL reconstruction was much more common in patients with bone patellar tendon-bone autograft compared to hamstring [21]. In another study, the extension loss occurred in 52 of the bone patellar tendon bone autograft and 27 of the hamstring group [22]. Even though extension loss is an important advantage of hamstring graft, it seems that reducing the flexor force is an important disadvantage of this type of graft [7, 23]. In a study by Joon Kyu Lee et al., the knee joint stability and functional outcomes were similar in hamstring and quadriceps grafts, while the flexor muscle strength was better in bone quadriceps tendon grafts [24]. Svensson et al. also found that the use of an internal hamstring graft after arthroscopic repair of ACL could cause muscle weakness in the knee bending and delay healing the bonding site [25]. However, the flexor strength was complete in both groups and the same as before the tear in the present study. In any case, a precise and complete rehabilitation may decrease the probability of extension loss and reduced flexion in any graft, and increase the chance of returning to sports activities, as Shelborn and Tites argued that the post-operative rehabilitation program reduced the problem of short knee extension domain that was the common problem in the ACL reconstruction by bone patellar tendon bone autograft [26]. They also stated that if surgeons were not sure of the acceptance and follow-up of the post-operative physiotherapy program by the patients, they should recommend ACL reconstruction by hamstring graft. The achievement of the acceptable results in extension and excellent results in knee flexion in both groups was probably because of the successful rehabilitation in both groups in the present study.
According to our results, only one patient in the hamstring group was diagnosed with acute infection, and no disease was reported in the quadriceps group. In other studies, 2 patients [27] and 6 patients (out of 1318 patients) [17] had infections with hamstring autograft. In another study, there was no case of infection in patients by semitendinosus-gracilis and quadriceps autograft [28]. The results of the above-mentioned studies were consistent with the present study. Although the failure to observe any case of infection was not statistically significant in the quadriceps group compared to the hamstring group, it can be a positive point in using the quadriceps tendon autograft in the present study.
Based on the present study, the indices, namely KT-1000, the Lysholm, and the Luchman significantly improved in the final follow-up as indices for assessing knee stability. A total of 86.7 of the quadriceps group and 84.5 of the hamstring group had zero Luchman and KT-1000 was less than 3 mm in 85.2 of the quadriceps group and 80.2 of the hamstring group. The results indicated a relatively similar improvement in patients of both groups. Another two studies found the same stability between hamstring and quadriceps grafts of bone-quadriceps tendon via arthrometric and manual methods [29, 30]. Our results were better than some studies [31] and similar to other studies [1, 32, 33].
According to Svensson et al., although hamstring graft has no complications, such as patellofemoral pain, weakness of the quadriceps femoris muscle, and patella fracture like bone patellar tendon bone autograft, it has other side effects, such as post-operative knee instability [25]. Several meta-analyses also indicated that in the case of using hamstring grafts, the joint laxity increased, but fewer complications occurred in the graft harvesting site [34]. However, there was no significant difference between the two groups in terms of knee stability in the present study.
In the present study, the IKDC and KOOS score values indicated significant improvement in both groups as the functional knee criteria in the final follow-up. In a study by Leiter et al., IKDC was normal (90-100) in 75 of the patients with a hamstring [35]. In a study by Leys et al., the mean IKDC was 90 (normal) in the hamstring group [36]. Furthermore, Charlton et al. also reported the mean IKDC equal to 81 (nearly normal) in patients with hamstring tendon graft and bio-absorbable interference screw fixation [37]. On the other hand, in a study by Lee et al., the IKDC score had a grade of A or B (normal and nearly normal) in 94 of patients who were treated with quadriceps autograft [1]. In the present study, 72.05 of patients in the quadriceps group and 70.42 in the hamstring group had normal IKDC. However, no significant difference was observed between the IKDC score and all KOOS subscales scores in patients of both groups in the final follow-up.
Similar to the present study, Kim et al. found a significant difference in functional outcomes between bone quadriceps tendon and single-bundle hamstring tendon graft [37].
Relatively small sizes of the groups were among the limitations of the present study because we only used the information of the patients who were present in all follow-up intervals and had complete and accurate information.
However, the presence of only a surgeon to perform all surgeries and having matched participants of both groups in terms of age, sex, athletic groups, and meniscus tear made the results of the present study more valuable and comparable.
5. Conclusion
According to the results of the present study, the rate of return to sport in patients with quadriceps autografts was slightly lower than in patients with hamstring autografts in a 2-year follow-up of athletes with an ACL tear. This reduction was probably because of the higher chondral lesion in quadriceps group patients. There were no significant differences in results of the both groups. It seems that orthopedic surgeons should be responsible for selecting suitable grafts for patients with an ACL tear to make the best decisions by considering post-operative rehabilitation conditions and methods.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Guilan University’s Ethics Committee with the ethics number IR.GUMS.REC.1396.80. The study is also registered at the Iranian Registry of Clinical Trials (Code: IRCT201706107274N13). All volunteers have signed a consent form before the study and their personal information will remain confidential.
Funding
This research was supported by the research project (No. 2038), Funded by the Guilan University of Medical Sciences.
Authors' contributions
Conceptualization and supervision: Mohsen Mardani-Kivi, Zoleikha azari; Methodology: Mohsen Mardani-Kivi, Fateme Sharifi; Investigation, writing-original draft, and writing-review & editing: All authors; Data collection: Fatemeh Sharifi, Zoleikha Azari; Data analysis: Ehsan Kazemnezhad Leili; Funding acquisition and resources: Mohsen Mardani-Kivi.
Conflict of interest
The authors declared no conflict of interest.
References
- Geib TM, Shelton WR, Phelps RA, Clark L. Anterior cruciate ligament reconstruction using quadriceps tendon autograft: Intermediate-term outcome. Arthroscopy. 2009; 25(12):1408-14. [DOI:10.1016/j.arthro.2009.06.004] [PMID]
- Chen G, Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: A meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015; 8(9):14604-14. [PMID]
- Goshima K, Kitaoka K, Nakase J, Tsuchiya H. Familial predisposition to anterior cruciate ligament injury. Asia-Pac J Sports Med Arthrosc Rehabil Technol. 2014; 1(2):62-6. [DOI:10.1016/j.asmart.2014.02.002]
- Moghtadaee M, Farahini H, Jahansouz A, Mokhtari T, Nabi R. Comparative Study of Treatment Results for Anterior Cruciate Ligament Reconstruction With Allograft and Auto Graft. J Res Orthop Sci. 2014; 1(3). [Link]
- Pinczewski L, Lyman J, Salmon L, Russell V, Roe J, Linklater J. A 10-year prospective comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft. J Sci Med Sport. 2009; 12:S59. [DOI:10.1016/j.jsams.2008.12.138]
- Sofu H, Sahin V, Gürsu S, Yıldırım T, Issın A, Ordueri M. Use of quadriceps tendon versus hamstring tendon autograft for arthroscopic anterior cruciate ligament reconstruction: A comparative analysis of clinical results. Eklem Hastalik Cerrahisi. 2013; 24(3):139-43. [DOI:10.5606/ehc.2013.31] [PMID]
- Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: A comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007; 35(3):384-94. [DOI:10.1177/0363546506294361] [PMID]
- Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K. Revision anterior cruciate ligament reconstruction with hamstring tendon autograft: 5-to 9-year follow-up. Am J Sports Med. 2006; 34(10):1604-14. [Link]
- Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am J Sports Med. 2006; 34(4):553-64. [Link]
- Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006; 14(10):1021-8. [Link]
- Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014; 48(21):1543-52. [Link]
- Padua DA, DiStefano LJ, Beutler AI, De La Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury–prevention program in elite-youth soccer athletes. J Athl Train. 2015; 50(6):589-95. [DOI:10.4085/1062-6050-50.1.10]
- Levy AS, Meier SW. Approach to cartilage injury in the anterior cruciate ligament-deficient knee. Ortho Clinic. 2003; 34(1):149-67. [Link]
- Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011; 39(3):538-43. [DOI:10.1177/0363546510384798]
- Webster KE, Feller JA, Kimp A, Devitt BMJKS, Sports Traumatology, Arthroscopy. Medial meniscal and chondral pathology at the time of revision anterior cruciate ligament reconstruction results in inferior mid-term patient-reported outcomes. Knee Surg Sports Traumatol Arthrosc. 2018; 26(4):1059-64. [DOI:10.1177/0363546510384798]
- Barcia AM, Kozlowski EJ, Tokish JM. Return to sport after meniscal repair. Clin Sports Med. 2012; 31(1):155-66. [DOI:10.1016/j.csm.2011.08.010] [PMID]
- Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR. Arthroscopic anterior cruciate ligament reconstruction: A metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003; 31(1):2-11. [DOI:10.1177/03635465030310011501] [PMID]
- Webster KE, Nagelli CV, Hewett TE, Feller JA. Factors associated with psychological readiness to return to sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2018; 46(7):1545-50. [DOI:10.1177/0363546518773757] [PMID] [PMCID]
- Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013; 41(7):1549-58. [DOI:10.1177/0363546513489284] [PMID]
- Graham SM, Parker RD. Anterior cruciate ligament reconstruction using hamstring tendon grafts. Clin Orthop Relat Res. 2002; (402):64-75. [DOI:10.1097/00003086-200209000-00007] [PMID]
- Eriksson K, Anderberg P, Hamberg P, Löfgren A, Bredenberg M, Westman I, et al. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001; 83(3):348-54. [DOI:10.1302/0301-620X.83B3.0830348]
- Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002; 30(2):214-20. [DOI:10.1177/03635465020300021201] [PMID]
- Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction: A randomized study with two-year follow-up. Am J Sports Med. 2001; 29(6):722-8. [DOI:10.1177/03635465010290060901] [PMID]
- Lee JK, Lee S, Lee MC. Outcomes of anatomic anterior cruciate ligament reconstruction: Bone-quadriceps tendon graft versus double-bundle hamstring tendon graft. Am J Sports Med. 2016; 44(9):2323-9. [DOI:10.1177/0363546516650666] [PMID]
- Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015; 22(2):100-10. [DOI:10.1016/j.knee.2014.11.014] [PMID]
- Mardani-Kivi M, Madadi F, Keyhani S, Karimi-Mobarake M, Hashemi-Motlagh K, Saheb-Ekhtiari K. Antero-medial portal vs. transtibial techniques for drilling femoral tunnel in ACL reconstruction using 4-strand hamstring tendon: A cross-sectional study with 1-year follow-up. Med Sci Monit. 2012; 18(11):CR674-9. [DOI:10.12659/MSM.883546] [PMID] [PMCID]
- Mardani-Kivi M, Karimi-Mobarakeh M, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K, Sarvi A. Hamstring tendon autograft versus fresh-frozen tibialis posterior allograft in primary arthroscopic anterior cruciate ligament reconstruction: A retrospective cohort study with three to six years follow-up. Int Orthop. 2016; 40(9):1905-11. [DOI:10.1007/s00264-016-3164-9] [PMID]
- Häner M, Bierke S, Petersen W. Anterior cruciate ligament revision surgery: ipsilateral quadriceps versus contralateral semitendinosus-gracilis autografts. Arthrosc J Arthrosc Relat Surg. 2016; 32(11):2308-17. [DOI:10.1016/j.arthro.2016.03.020]
- Gorschewsky O, Klakow A, Pütz A, Mahn H, Neumann W. Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2007; 15(11):1284-92. [DOI:10.1007/s00167-007-0371-3]
- Aronowitz ER, Ganley TJ, Goode JR, Gregg JR, Meyer JS. Anterior cruciate ligament reconstruction in adolescents with open physes. Am J Sports Med. 2000; 28(2):168-75. [Link]
- Lee S, Seong SC, Jo CH, Han HS, An JH, Lee MC. Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. JBJS. 2007; 89(suppl_3):116-26. [Link]
- Kim SJ, Jo SB, Kumar P, Oh KS. Comparison of single-and double-bundle anterior cruciate ligament reconstruction using quadriceps tendon–bone autografts. J Arthrosc Relat Surg. 2009; 25(1):70-7. [DOI:10.1016/j.arthro.2008.09.004]
- Struewer J, Ziring E, Frangen TM, Efe T, Meißner S, Buecking B, et al. Clinical outcome and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using hamstring graft: follow-up after two and ten years. Int Orthop. 2013; 37(2):271-7. [DOI:10.1007/s00264-012-1653-z]
- Leiter JR, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014; 22(5):1061-9. [DOI:10.1007/s00167-013-2466-3]
- Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012; 40(3):595-605. [DOI:10.1177/0363546511430375]
- Charlton WP, Randolph DA, Lemos S, Shields CL. Clinical outcome of anterior cruciate ligament reconstruction with quadrupled hamstring tendon graft and bioabsorbable interference screw fixation. Am J Sports Med. 2003; 31(4):518-21. [DOI:10.1177/03635465030310040701]
- Kim SJ, Lee SK, Choi CH, Kim SH, Kim SH, Jung M. Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am J Sports Med. 2014; 42(1):166-72. [DOI:10.1177/0363546513505191]
Type of Study: Research Article |
Subject:
Knee surgery
Received: 2021/10/31 | Accepted: 2022/09/8 | Published: 2022/02/1
Received: 2021/10/31 | Accepted: 2022/09/8 | Published: 2022/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |