Volume 9, Issue 1 (2-2022)
JROS 2022, 9(1): 65-68 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Torkaman A, Azizi A, Kazemi J, Mousapour A. Post COVID-19 Anterior Cruciate Ligament (ACL) Tear in Twin Sisters After Re-starting Professional Futsal Exercises: A Case Report. JROS 2022; 9 (1) :65-68
URL: http://jros.iums.ac.ir/article-1-2199-en.html
URL: http://jros.iums.ac.ir/article-1-2199-en.html
1- Bone and Joint Reconstruction Research Center, Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1316 kb]
(350 Downloads)
| Abstract (HTML) (1323 Views)
Full-Text: (457 Views)
1. Introduction
Although coronavirus disease 2019 (COVID-19) is mainly a respiratory illness, its symptoms are not limited to the respiratory system. It is well acknowledged that COVID-19 infection is associated with multiple organ involvement and a variety of symptoms, including neuromuscular problems [1]. Some of these symptoms are long-lasting and may prolong up to 3 months after the disease onset [2]. Persistent fatigue and musculoskeletal weakness are among the most common long-term symptoms of COVID-19 [3].
An Anterior Cruciate Ligament (ACL) tear is one of the most frequent and debilitating sport-related injuries, particularly in young and active female athletes. The higher prevalence of ACL tear in females is attributable to a variety of factors, such as anatomical and hormonal differences [4]. In the context of such susceptibility, poor neuromuscular control during the COVID-19 recovery period may also increase the risk of an ACL tear in the female population [5].
In this report, we present an ACL tear in futsal player identical twin sisters after restarting the exercises almost 2 months after the COVID-19 infection.
2. Case Presentation
A 28-year-old athletic girl who was a professional futsal player with 15 years of experience was referred to our center with a left knee injury. In the history-taking session, the patient reported a 15-day quarantine period because of the COVID-19 infection, which started on August 30, 2021, and ended on September 14, 2021. The patient had a sense of muscle weakness during the COVID-19 recovery period. The patient’s father died of COVID-19 on September 16, 2021. She restarted her futsal exercise on October 15, 2021. The injury occurred on November 1, 2021, during a sudden twisting movement in the air. The patient was single and in her luteal phase of the menstrual cycle. She had a normal 28- to 30-day menstrual cycle, and was not using oral contraceptive pills. The patient had no familial history of an ACL tear. The body mass index (BMI) of the patient was 21.95 kg/m2.
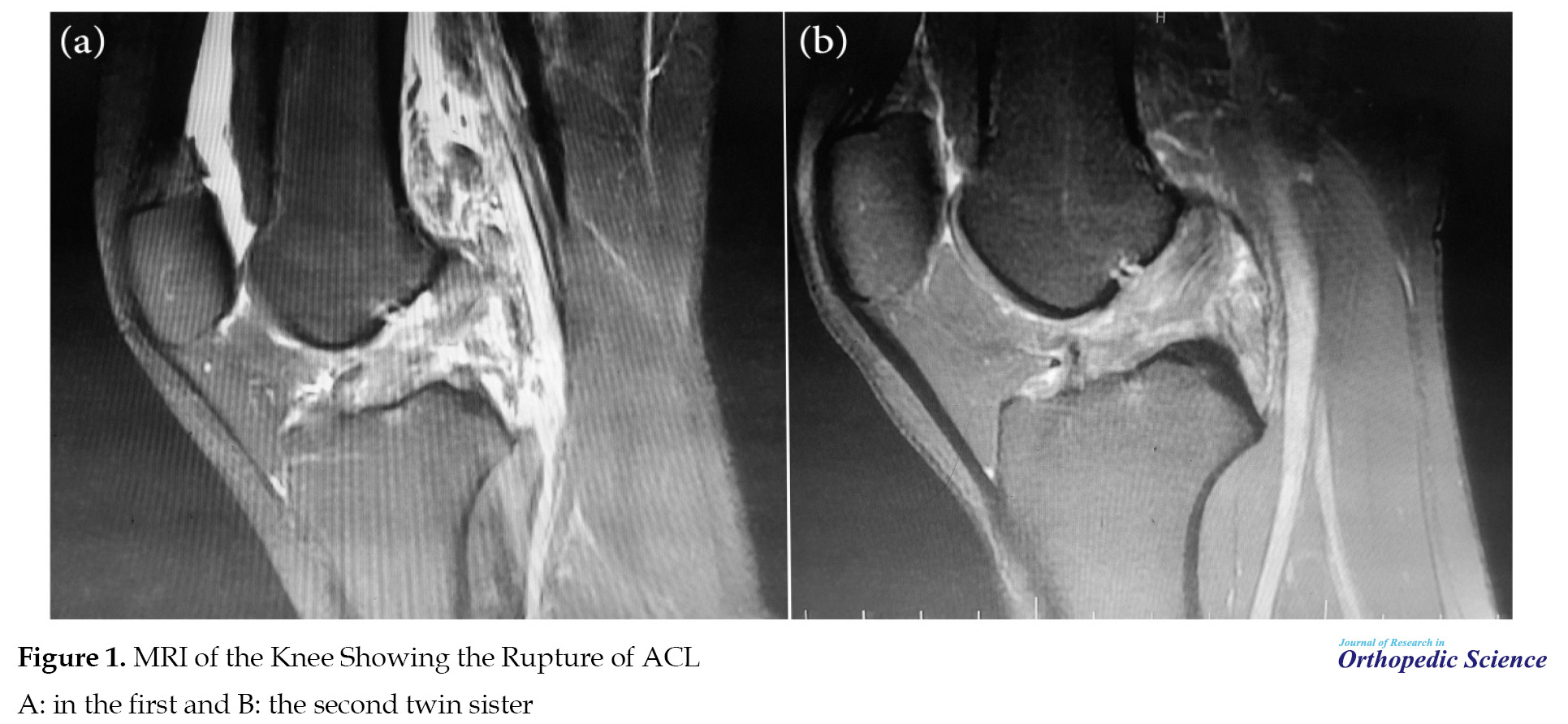
In the physical examination, the patient had a marked reduction in the knee range of motion (ROM) (120º), while the knee ROM was full before the injury. In addition, the patient had a positive anterior drawer test, a positive pivot shift test (+3), and a positive Lachman test (+3) performed by an orthopedic surgeon with a knee subspecialty. In the imaging evaluation, the intercondylar notch width index was 0.323 in the involved leg and 0.26 in the non-involved leg. The tibial slope was 7.8º. The involved knee had obvious genu recurvatum, while the valgus stress test was negative in the contralateral knee. Meanwhile, the Beighton score was 3. According to the physical symptoms along with the magnetic resonance imaging (MRI) findings (Figure 1a), a complete ACL tear was diagnosed and the patient underwent ACL reconstruction surgery with hamstring autograft.
After 11 days, the twin sister of the patient, who was also a professional futsal player, was referred with the same symptoms in the left leg (non-dominant leg), and an ACL tear was detected in the knee MRI (Figure 1b).
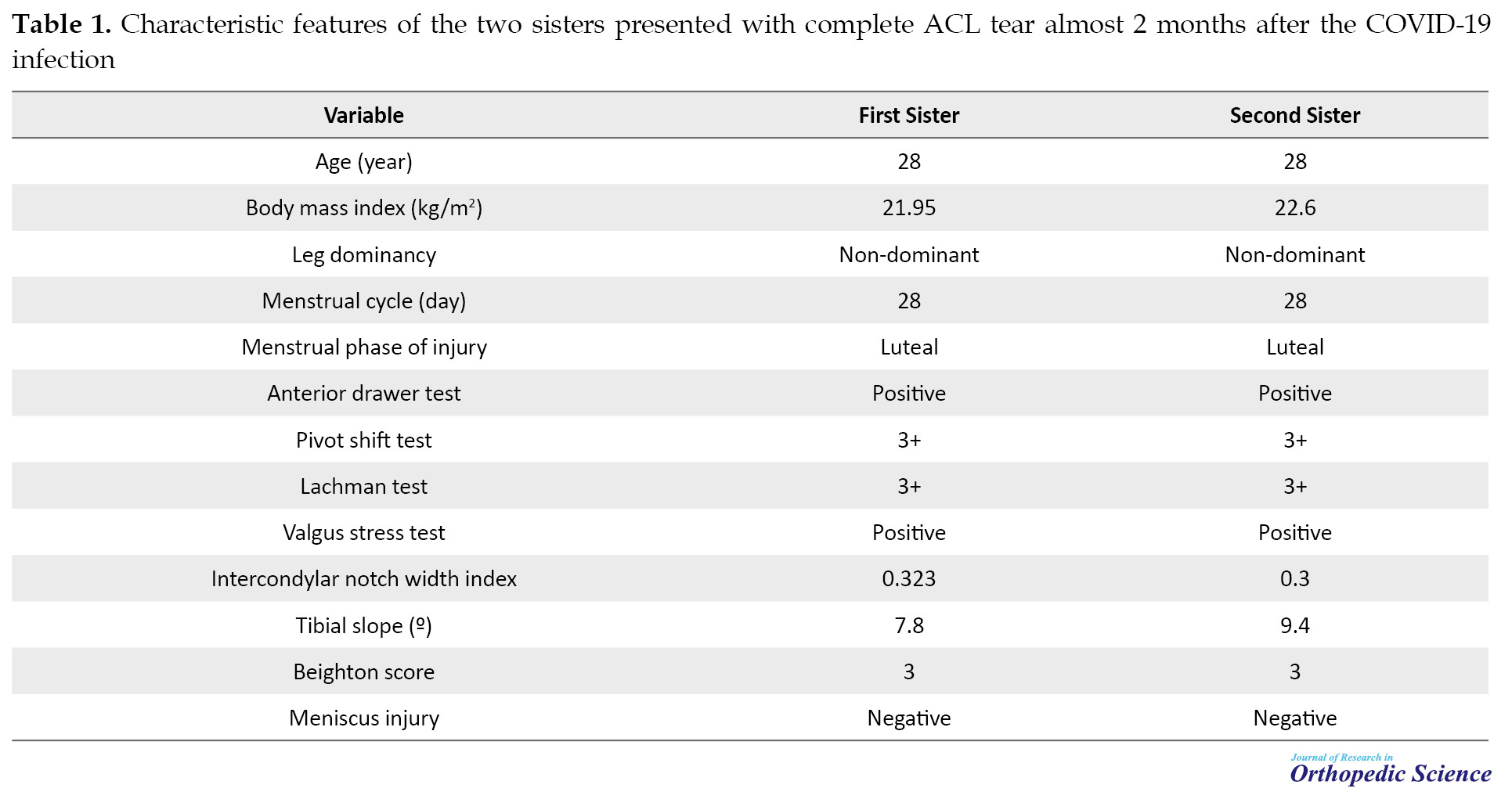
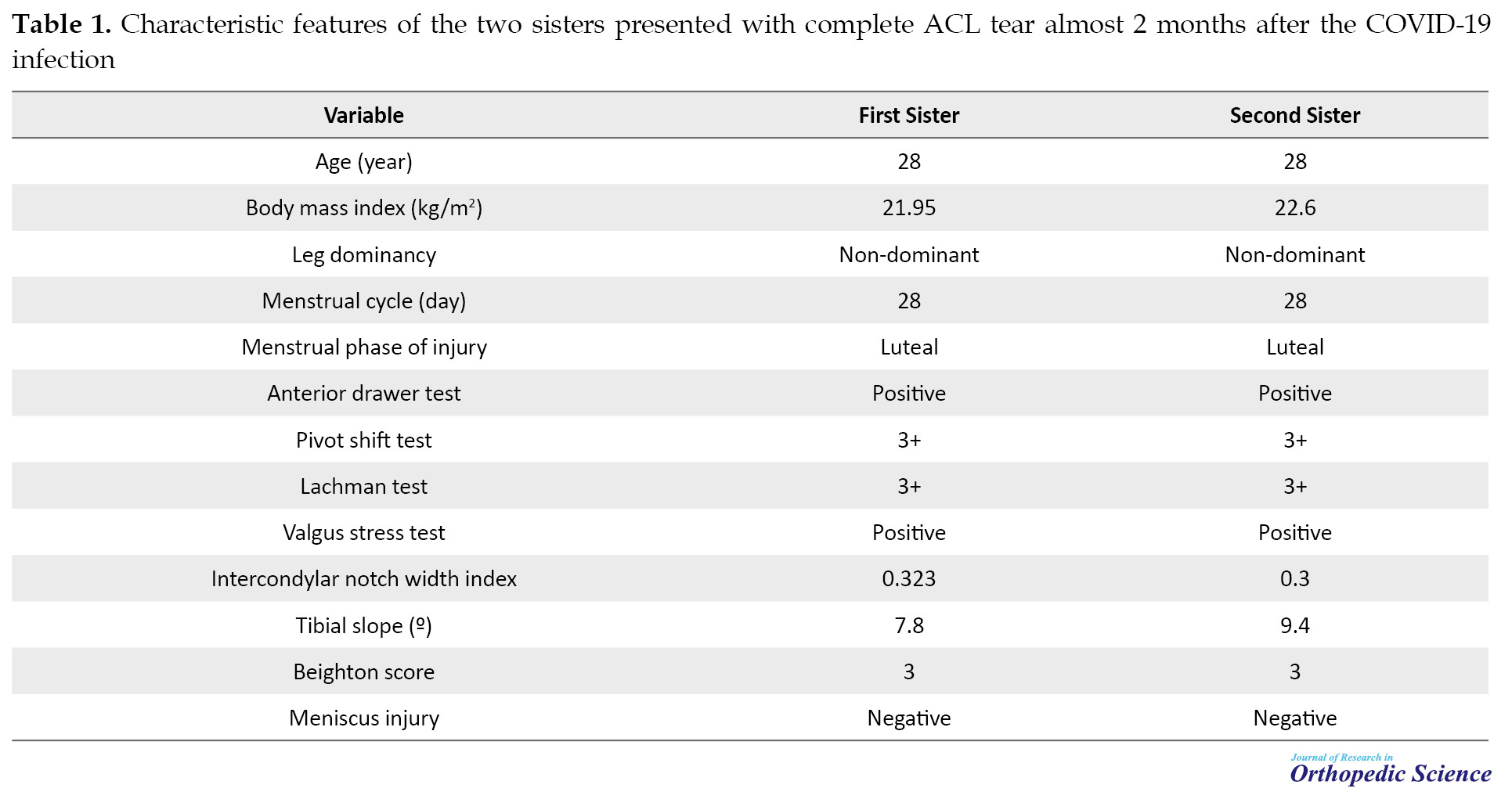
The characteristic features of the twin sister were completely similar to her sister in terms of BMI, menstrual status, history of COVID-19 infection, and so on. The physical and radiographic characteristics, including the anterior drawer test, pivot shift test, the Lachman test, intercondylar notch width index, tibial slope, and the Beighton score were similar, as well (Table 1).
Akin to her sister, the patient underwent ACL reconstruction surgery with hamstring autograft.
Nearly 3 months of follow-up of the patients was event-free. The patients were receiving a rehabilitation program, and no complication was recorded during the follow-up period. The patients provided written consent to use their medical data for publication.
3. Discussion
In this study, we reported a complete ACL tear in athlete twin sisters, 10 days apart, almost 2 months after the COVID-19 infection. The patients had no familial history of an ACL tear. Their menstrual cycle was normal and both ruptures occurred in the luteal phase of menstruation. The tibial slope and the intercondylar notch width index were in the normal range. However, the patients had obvious ligamentous laxity based on the Beighton criteria. Also, the patients reported a sense of severe muscle weakness (3/5) during the COVID-19 recovery period that almost regained (5/5) in the last follow-up, as the patients were athletes and had good cooperation in the postoperative rehabilitation.
The association of lower extremity muscle strength weakness with ACL tear has been reported in several studies. The study of Myer et al. observed a combination of decreased hamstring strength but not quadriceps strength in female athletes compared to males [6]. The study by Augustsson and Ageberg revealed that the odds of sustaining an ACL injury were 7 times higher in females with weak lower extremity muscle strength compared to males [7]. The study of Weinhandl et al. revealed a 36% increased ACL loading after fatigue-induced hamstring strength reduction [8].
Muscle weakness after COVID-19 has also been reported frequently [9, 10, 11]. Sire et al. investigated the neuromuscular impairment of knee stabilizer muscles after the COVID-19 infection. They evaluated thigh muscle activation, body composition, and physical performance after the COVID-19 infection in a series of 12 female volleyball players of the same team. Pre-activation time of thigh muscles was assessed before and after the COVID-19 infection using Bioelectrical Impedance Analysis (BIA) and jump tests. They found a significant delay in the activation time of rectus femoris, vastus medialis, biceps femoris, and medial hamstring. In addition, a significant reduction was observed in the body composition at BIA. They concluded that the neuromotor balance of the knee stabilizer muscle is impaired after the COVID-19 infection in female athletes, and this metabolic sequela should be considered to prevent musculoskeletal injuries, such as an ACL tear in high-risk patients. They also suggested designing specific neuromuscular rehabilitation protocols for this group of patients [5]. In the present report, both patients reported musculoskeletal weakness in the COVID-19 recovery period and afterward. In addition, they had obvious ligamentous laxity in the clinical examination and according to the Beighton criteria. Therefore, the ACL tear in our patients could be attributed to persistent COVID-19 neuromuscular impairment.
Jafari-Nodoushan et al. investigated the prevalence of musculoskeletal disorders among faculty members of Yazd University before and after the COVID-19 pandemic. According to their report, after the spread of COVID-19, musculoskeletal disorders significantly increased in most organs. The majority of the musculoskeletal disorders during the COVID-19 outbreak were in the back, neck, and knees. The frequency of knee injuries for the 3 different campus members increased from 42%, 31%, and 37% to 54%, 44%, and 49%, respectively. Considering the lower participation of the population during the COVID-19 period, a reduced rate of musculoskeletal injuries could be expected. However, the rate of musculoskeletal injuries increased during this period, and this increase could be attributed to the detrimental effect of COVID-19 infection on the musculoskeletal system [12]. The present report also confirms the higher rate of ACL injury after the COVID-19 infection. Therefore, it is necessary to raise awareness regarding the long-term complications of COVID-19 to reduce its catastrophic consequence, particularly in female athletes.
Altogether, the results of the present study suggest an association between COVID-19 muscle weakness and increased risk of ACL injury in female athletes, even months after the infection. Therefore, prophylactic rehabilitating programs are recommended before re-participation in professional athletic activities after the COVID-19 infection.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Although coronavirus disease 2019 (COVID-19) is mainly a respiratory illness, its symptoms are not limited to the respiratory system. It is well acknowledged that COVID-19 infection is associated with multiple organ involvement and a variety of symptoms, including neuromuscular problems [1]. Some of these symptoms are long-lasting and may prolong up to 3 months after the disease onset [2]. Persistent fatigue and musculoskeletal weakness are among the most common long-term symptoms of COVID-19 [3].
An Anterior Cruciate Ligament (ACL) tear is one of the most frequent and debilitating sport-related injuries, particularly in young and active female athletes. The higher prevalence of ACL tear in females is attributable to a variety of factors, such as anatomical and hormonal differences [4]. In the context of such susceptibility, poor neuromuscular control during the COVID-19 recovery period may also increase the risk of an ACL tear in the female population [5].
In this report, we present an ACL tear in futsal player identical twin sisters after restarting the exercises almost 2 months after the COVID-19 infection.
2. Case Presentation
A 28-year-old athletic girl who was a professional futsal player with 15 years of experience was referred to our center with a left knee injury. In the history-taking session, the patient reported a 15-day quarantine period because of the COVID-19 infection, which started on August 30, 2021, and ended on September 14, 2021. The patient had a sense of muscle weakness during the COVID-19 recovery period. The patient’s father died of COVID-19 on September 16, 2021. She restarted her futsal exercise on October 15, 2021. The injury occurred on November 1, 2021, during a sudden twisting movement in the air. The patient was single and in her luteal phase of the menstrual cycle. She had a normal 28- to 30-day menstrual cycle, and was not using oral contraceptive pills. The patient had no familial history of an ACL tear. The body mass index (BMI) of the patient was 21.95 kg/m2.
In the physical examination, the patient had a marked reduction in the knee range of motion (ROM) (120º), while the knee ROM was full before the injury. In addition, the patient had a positive anterior drawer test, a positive pivot shift test (+3), and a positive Lachman test (+3) performed by an orthopedic surgeon with a knee subspecialty. In the imaging evaluation, the intercondylar notch width index was 0.323 in the involved leg and 0.26 in the non-involved leg. The tibial slope was 7.8º. The involved knee had obvious genu recurvatum, while the valgus stress test was negative in the contralateral knee. Meanwhile, the Beighton score was 3. According to the physical symptoms along with the magnetic resonance imaging (MRI) findings (Figure 1a), a complete ACL tear was diagnosed and the patient underwent ACL reconstruction surgery with hamstring autograft.
After 11 days, the twin sister of the patient, who was also a professional futsal player, was referred with the same symptoms in the left leg (non-dominant leg), and an ACL tear was detected in the knee MRI (Figure 1b).
The characteristic features of the twin sister were completely similar to her sister in terms of BMI, menstrual status, history of COVID-19 infection, and so on. The physical and radiographic characteristics, including the anterior drawer test, pivot shift test, the Lachman test, intercondylar notch width index, tibial slope, and the Beighton score were similar, as well (Table 1).
Akin to her sister, the patient underwent ACL reconstruction surgery with hamstring autograft.
Nearly 3 months of follow-up of the patients was event-free. The patients were receiving a rehabilitation program, and no complication was recorded during the follow-up period. The patients provided written consent to use their medical data for publication.
3. Discussion
In this study, we reported a complete ACL tear in athlete twin sisters, 10 days apart, almost 2 months after the COVID-19 infection. The patients had no familial history of an ACL tear. Their menstrual cycle was normal and both ruptures occurred in the luteal phase of menstruation. The tibial slope and the intercondylar notch width index were in the normal range. However, the patients had obvious ligamentous laxity based on the Beighton criteria. Also, the patients reported a sense of severe muscle weakness (3/5) during the COVID-19 recovery period that almost regained (5/5) in the last follow-up, as the patients were athletes and had good cooperation in the postoperative rehabilitation.
The association of lower extremity muscle strength weakness with ACL tear has been reported in several studies. The study of Myer et al. observed a combination of decreased hamstring strength but not quadriceps strength in female athletes compared to males [6]. The study by Augustsson and Ageberg revealed that the odds of sustaining an ACL injury were 7 times higher in females with weak lower extremity muscle strength compared to males [7]. The study of Weinhandl et al. revealed a 36% increased ACL loading after fatigue-induced hamstring strength reduction [8].
Muscle weakness after COVID-19 has also been reported frequently [9, 10, 11]. Sire et al. investigated the neuromuscular impairment of knee stabilizer muscles after the COVID-19 infection. They evaluated thigh muscle activation, body composition, and physical performance after the COVID-19 infection in a series of 12 female volleyball players of the same team. Pre-activation time of thigh muscles was assessed before and after the COVID-19 infection using Bioelectrical Impedance Analysis (BIA) and jump tests. They found a significant delay in the activation time of rectus femoris, vastus medialis, biceps femoris, and medial hamstring. In addition, a significant reduction was observed in the body composition at BIA. They concluded that the neuromotor balance of the knee stabilizer muscle is impaired after the COVID-19 infection in female athletes, and this metabolic sequela should be considered to prevent musculoskeletal injuries, such as an ACL tear in high-risk patients. They also suggested designing specific neuromuscular rehabilitation protocols for this group of patients [5]. In the present report, both patients reported musculoskeletal weakness in the COVID-19 recovery period and afterward. In addition, they had obvious ligamentous laxity in the clinical examination and according to the Beighton criteria. Therefore, the ACL tear in our patients could be attributed to persistent COVID-19 neuromuscular impairment.
Jafari-Nodoushan et al. investigated the prevalence of musculoskeletal disorders among faculty members of Yazd University before and after the COVID-19 pandemic. According to their report, after the spread of COVID-19, musculoskeletal disorders significantly increased in most organs. The majority of the musculoskeletal disorders during the COVID-19 outbreak were in the back, neck, and knees. The frequency of knee injuries for the 3 different campus members increased from 42%, 31%, and 37% to 54%, 44%, and 49%, respectively. Considering the lower participation of the population during the COVID-19 period, a reduced rate of musculoskeletal injuries could be expected. However, the rate of musculoskeletal injuries increased during this period, and this increase could be attributed to the detrimental effect of COVID-19 infection on the musculoskeletal system [12]. The present report also confirms the higher rate of ACL injury after the COVID-19 infection. Therefore, it is necessary to raise awareness regarding the long-term complications of COVID-19 to reduce its catastrophic consequence, particularly in female athletes.
Altogether, the results of the present study suggest an association between COVID-19 muscle weakness and increased risk of ACL injury in female athletes, even months after the infection. Therefore, prophylactic rehabilitating programs are recommended before re-participation in professional athletic activities after the COVID-19 infection.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Thakur V, Ratho RK, Kumar P, Bhatia SK, Bora I, Mohi GK, et al. Multi-organ involvement in COVID-19: Beyond pulmonary manifestations. J Clin Med. 2021; 10(3):446. [DOI:10.3390/jcm10030446] [PMID] [PMCID]
- Understanding the long-term health effects of COVID-19. EClinicalMedicine. 2020; 26:100586. [DOI:10.1016/j.eclinm.2020.100586] [PMID] [PMCID]
- Yang C, Zhao H, Tebbutt SJ. Long-term effects on survivors with COVID-19. Lancet. 2021; 398(10314):1872. [DOI:10.1016/S0140-6736(21)02323-0]
- Moeller JL, Lamb MM. Anterior cruciate ligament injuries in female athletes: Why are women more susceptible? Phys Sportsmed. 1997; 25(4):31-48. [DOI:10.3810/psm.1997.04.1272] [PMID]
- de Sire A, Demeco A, Marotta N, Spanò R, Curci C, Farì G, et al. Neuromuscular impairment of knee stabilizer muscles in a COVID-19 cluster of female volleyball players: Which role for rehabilitation in the post-COVID-19 return-to-play? Appl Sci. 2022; 12(2):557. [DOI:10.3390/app12020557]
- Myer GD, Ford KR, Barber Foss KD, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009; 19(1):3-8. [DOI:10.1097/JSM.0b013e318190bddb] [PMID]
- Ryman Augustsson S, Ageberg E. Weaker lower extremity muscle strength predicts traumatic knee injury in youth female but not male athletes. BMJ Open Sport Exerc Med. 2017; 3(1):e000222. [DOI:10.1136/bmjsem-2017-000222] [PMID] [PMCID]
- Weinhandl JT, Earl-Boehm JE, Ebersole KT, Huddleston WE, Armstrong BS, O’Connor KM. Reduced hamstring strength increases anterior cruciate ligament loading during anticipated sidestep cutting. Clin Biomech. 2014; 29(7):752-9. [DOI:10.1016/j.clinbiomech.2014.05.013] [PMID]
- Medrinal C, Prieur G, Bonnevie T, Gravier F-E, Mayard D, Desmalles E, et al. Muscle weakness, functional capacities and recovery for COVID-19 ICU survivors. BMC Anesthesiol. 2021; 21(1):64. [DOI:10.1186/s12871-021-01274-0] [PMID] [PMCID]
- Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet. 2021; 397(10270):220-32. [DOI:10.1016/S0140-6736(20)32656-8]
- Mohammadpour M, Yazdi H, Bagherifard A, Jabalameli M, Moghtadaei M, Torkaman A, et al. Evaluation of early complications, outcome, and mortality in Coronavirus Disease 2019 (COVID-19) infection in patients who underwent orthopedic surgery. BMC Musculoskele Disord. 2022; 23(1):64. [DOI:10.1186/s12891-022-05010-8] [PMID] [PMCID]
- Jafari-Nodoushan A, Bagheri G, Mosavi Nodoushan f. [Effect of COVID-19 virus on prevalence of musculoskeletal disorders of faculty members of Yazd University (Persian)]. Iran J Ergon. 2020; 8(3):1-12. [DOI:10.30699/jergon.8.3.1]
Type of Study: Case Report |
Subject:
Knee surgery
Received: 2022/06/15 | Accepted: 2022/08/30 | Published: 2022/02/1
Received: 2022/06/15 | Accepted: 2022/08/30 | Published: 2022/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |