Volume 9, Issue 2 (5-2022)
JROS 2022, 9(2): 69-78 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Norasteh A A, Zolghadr H. Functional Tests and Their Reliability for Return to Sport After Shoulder Injuries: A Review Study. JROS 2022; 9 (2) :69-78
URL: http://jros.iums.ac.ir/article-1-2201-en.html
URL: http://jros.iums.ac.ir/article-1-2201-en.html
1- Department of Physiotherapy, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Sport Injuries and Corrective Exercise, Faculty of Sport Sciences, University of Guilan, Rasht, Iran.
2- Department of Sport Injuries and Corrective Exercise, Faculty of Sport Sciences, University of Guilan, Rasht, Iran.
Full-Text [PDF 723 kb]
(406 Downloads)
| Abstract (HTML) (1841 Views)
Full-Text: (330 Views)
1. Introduction
Injured athletes seeking to return to sport (RTS) or exercise to previous levels before shoulder injury have to recapture muscle vigor, dynamic stability, and shoulder function [1]. Nevertheless, due to the dearth of evidence-based criteria to precisely evaluate the glenohumeral joint dynamic stability [2], clinical doctors utilize associated evaluations, such as function and strength to ascertain preparedness for RTS [3, 4, 5, 6, 7]. In addition, it is unlikely that any test method can demonstrate dynamic stability. Therefore, the use of objective and clinical testing etiquettes is vital to direct RTS after shoulder traumas [8]. Determining the timing of RTS after shoulder damage and the dearth of reliable and valid tests is a major problem for clinicians [9, 10]. Professional athletes who are away from sports for a long time due to shoulder injuries, it can jeopardize their career opportunities [11]. Moreover, the recurrence rate of shoulder instability after a dislocation of the shoulder can be higher than 50% with both non-surgical and surgical therapy being successful [12, 13]. In another study, the reoccurrence rate of dislocation was 40% in patients younger than 20 years, and 63% in 20 to 40 years [14, 15]. It shows that improvement in decision-making for RTS after shoulder injury is essential and a crucial step to facilitate decision-making is to create physical performance tests [16]. Wilson et al. [17] designed a practical etiquette to evaluate readiness for RTS. The etiquette used isokinetic external and internal strength, two functional evaluations, lateral rotation endurance testing, the unilateral seated shot-put test, and the closed kinetic chain upper extremity stability test (CKCUEST). This etiquette showed remarkable deficiencies in people who wanted RTS after six months of shoulder stabilization [17]. While this etiquette is vital in deciding to RTS, it has limitations that should be considered. First, this etiquette uses an isokinetic strength test, which is a time-intensive and costly test and is not commonly used in many clinical environments [18]. Even though isokinetic evaluation is the standard criteria to evaluate shoulder strength [19, 20], isometric testing through manual dynamometry is an alternative method that is more feasible to be performed by clinicians. The second one is the psychometric properties, especially the reliability and validity [21]. Physical performance tests should be uncomplicated, inexpensive, and applicable in clinics [22, 23]. In clinical trials, attention should be paid to the sport to which the athlete wants to return because many variations exist in the requests of various sports [24]. Moreover, despite most sports requiring athletes to exercise for a prolonged duration of time, contemporary physical performance tests announce secluded efforts [25-28] and do not determine toleration ability. Therefore, a one-time test may not precisely estimate the preparedness of an athlete for RTS for the required period, meaningful performance tests that inspect tolerance are needed [16]. Eventually, tests that measure only one construct have limited clinical utility. Therefore, tests that measure all the various constructs, such as strength, range of motion, power, and neuromuscular control may enhance the capability to ascertain a secure RTS (Figure 1) manifests the necessary constituents of the functional test). Therefore, it is essential to design a group of secure, valid, and reliable physical performance tests. Considering that few review studies have been conducted in this field, therefore, the main motive of this review research is to survey and announce the functional tests for RTS after shoulder injuries. Hope that the results of this research will supply guidance for the optimum method of testing in the clinic-based applications and return to the decision-making of sports.
Objectives
A comprehensive review of the functional tests and their reliability for RTS later than injuries of shoulders.
2. Methods
This is a systematic review developed according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA).
Search strategy
In the present research, a comprehensive review of the functional tests for RTS after shoulder injuries were conducted by searching the Web of Science, PEDro, Google Scholar, PubMed, ScienceDirect, SCOPUS, and CINAHL databases with the keywords using three groups of search terms, (group 1) “shoulder return to sport” or “return to play” or “return to competition” or “return to activities” or “return to participation”, and (group 2) “upper limb” or “upper body” or “upper limb” or “shoulder complex”, and (group 3) “shoulder functional tests” or “shoulder functional battery tests” or “shoulder functional assessment” or “shoulder functional evaluation”. These combinations (of three groups) were investigated in keywords, titles, and abstracts of the research published by the indexed journals in the databases that were performed from 2000 to June 2021. Also, a manual search and comprehensive review of research paper sources was conducted to find research papers that cannot be found through electronic search.
Eligibility criteria
The inclusion criteria included athletes or people who underwent rehabilitation programs, and suffered shoulder injuries, such as anterior and posterior instability, dislocations, ruptured rotator cuffs, and use of functional tests to RTS. English-language research papers, full-text studies as well as studies which were randomized control trials, cross-sectional, and cohort designs were published. The exclusion criteria included other shoulder injuries, such as fractures of the proximal arm, and research papers that were published briefly in congresses and seminars.
Study selection
The English language was used in this search. All texts were screened by researchers. Finally, using relevant keywords, 123 research papers were received from databases. At first, the titles of the research papers were examined and 11 duplicate research papers were removed. In the next step, abstracts of 112 research papers were examined, and then 79 research papers were excluded from the study due to non-compliance with the inclusion criteria. In the following, 33 research papers were studied in full text, and after that 21 research papers were removed due to non-compliance with the inclusion criteria (for example, not being in English, not using performance tests for RTS after shoulder injuries, etc.). Finally, 12 research papers were contained in the present review and their results were reported fully. Another senior researcher checked the final list of selected research papers to ensure that all research papers were consistent with the objective of the study. Figure 2 shows the study selection procedure. The population, intervention, comparison, outcomes, and study (PICOS)-type framework is based on the research inquiry stated (Table 1).

3. Results
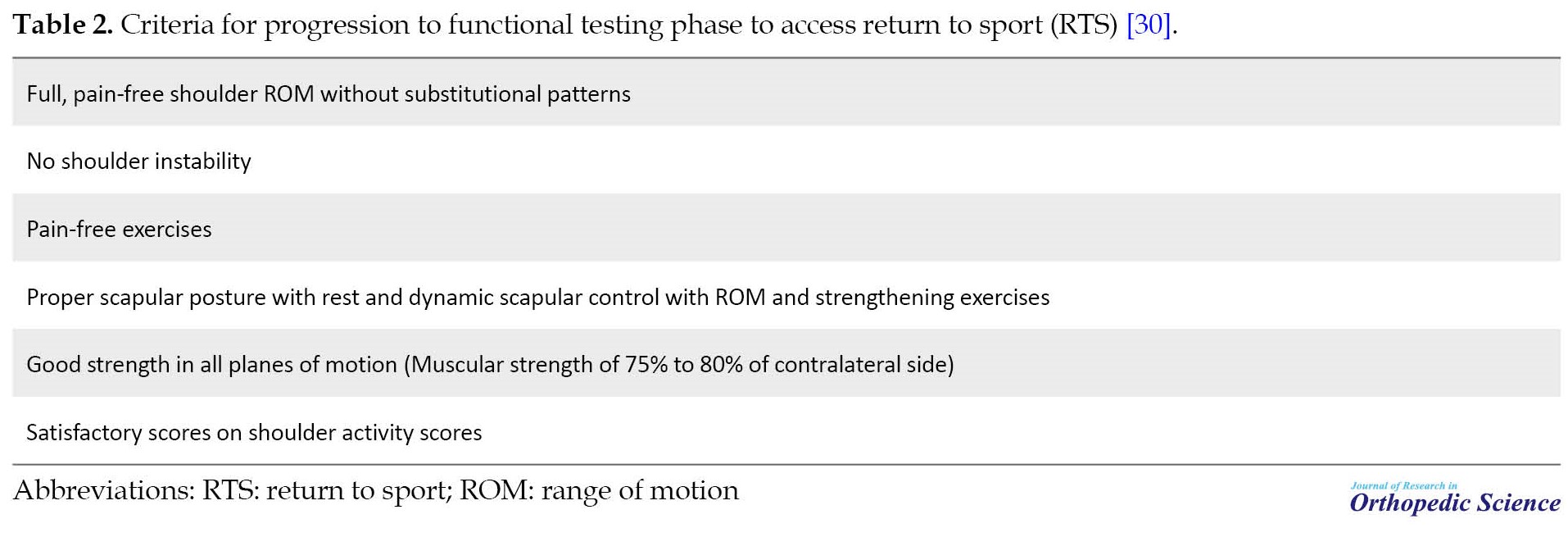
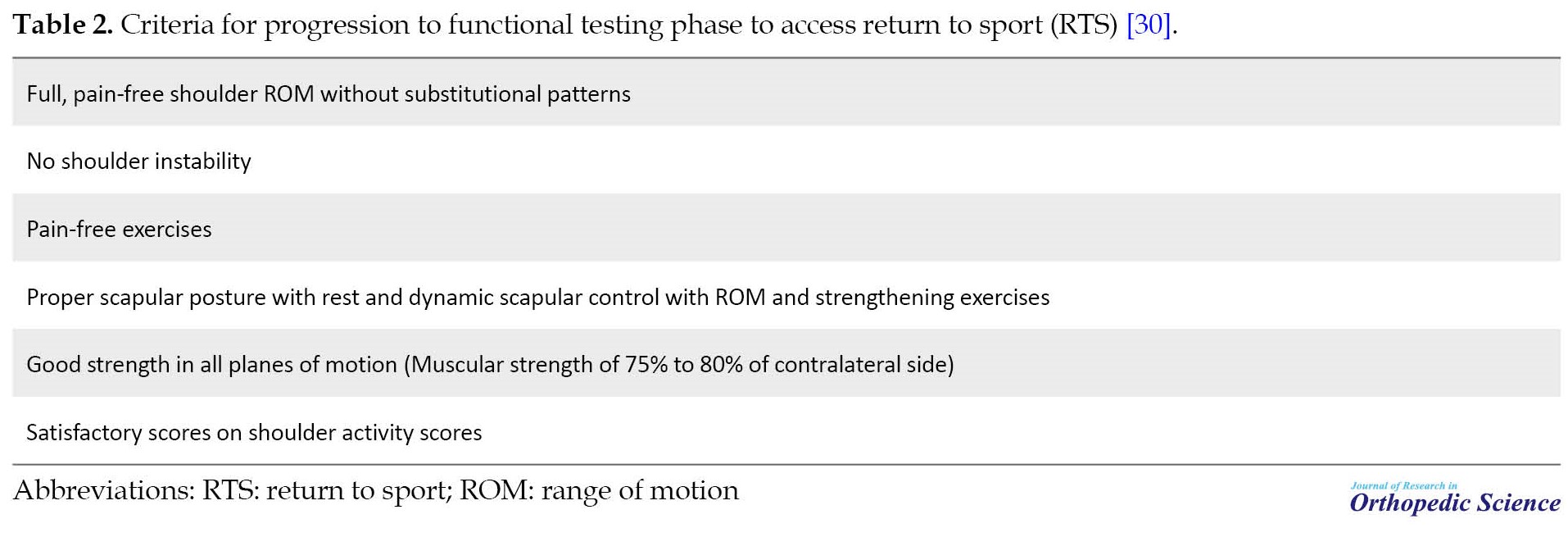
A search of Web of Science, PEDro, Google Scholar, PubMed, ScienceDirect, Scopus, and CINAHL databases found 123 research papers. After eliminating 11 identical titles, 112 abstracts were selected for review. Then the abstracts were reviewed, 79 research papers were removed and 33 research papers were selected for full-text reading. After reviewing the full-text research papers, 21 research papers were eliminated and 12 research papers were included in the study. The following are the necessary criteria to enter the stage of performing functional tests for RTS (Table 2).
The Results of Research Examining Functional Tests for Returning to Sport (RTS) After Shoulder Injuries
Popchak et al. studied the validity and reliability of RTS testing for the shoulder injury. Thirty healthy active adults with an average age of 24.0±1.6 years participated in this study. Total functional assessments (intraclass correlation coefficient [ICC]: 0.80-0.92), isometric (ICC: 0.83-0.94), and isokinetic (ICC: 0.88-0.94) had fine to very good intra-rater reliability, considering the repetition to failure testing had low to average reliability (ICC: 0.48-0.57). The results of this study also showed that the isometric, isokinetic, and functional evaluations in this testing procedure show admissible reliability and validity [8]. Pontillo et al. studied the use of an upper limb functional testing algorithm to calculate returning-to-play preparedness in collegiate soccer players. Six participants (18 to 21 years old) who experienced shoulder capsulolabral mend participated in this research. Functional tests used in this study included standing cable press, performed at 30% body weight (BW), Scaption, performed at 5% BW, Prone-y, performed at 3% BW and CKCUEST. In this study, it was shown that the upper limb functional testing algorithm assists in evaluating RTS in male collegiate athletes of soccer [31]. Wilk et al. studied the RTS criteria for injury of shoulder: A clinic-based report. In this study, Wilk presented the functional battery tests for RTS after shoulder injuries, which can be seen in Table 3.

The results of this research demonstrated many functional tests, but different tests can be used depending on the type of injury [7].
Hollstadt et al. studied the reliability of test-retest of the CKCUEST in an adjusted test place in dividing I collegiate basketball players. The results of this study showed that the CKCUEST in an adjusted test place is a reliable evaluation device and underpins preceding discoveries [32]. Decleve et al. studied the “upper limb rotation test”, a validity and reliability investigation of an up-to-date upper limb physical performance test. Results showed good reliability. A moderate correlation (r=0.553) was discovered between the CKCUEST and upper lime rotation test (ULRT) scores. A moderate correlation (r=0.556) was found between ULRT and SMBT scores [33]. Wilson et al. built up an objective and functional criterion-based shoulder testing etiquette to assess RTS preparedness in clinic-based environments. The etiquette used was external rotation endurance testing, isokinetic external and internal strength, and two functional evaluations, the CKCUEST and the unilateral seated shot put test. The use of this etiquette disclosed remarkable deficiencies in patients arranging for RTS at six months after shoulder balance. Although this etiquette is essential for RTS decisions, it has limitations that should be noted [17]. Degot et al. studied interrater reliability and consensus of a modified CKCUEST. The results showed that reasonable reliability was discovered for the muscular endurance index calculated while splitting the one-half number of touches computed throughout the final 30s of the one-min set, by the m-CKCUEST score computed above (ICC=0.86). The m-CKCUEST allows for the production of two reliable result measurements that estimate muscular endurance and upper limb stability. The aforementioned results may be utilized in the aftermath to evaluate rehabilitation level or performance [34]. Olds et al. investigated the shoulder arm RTS test reliability. Functional tests within this study were divided into two categories, which can be seen in Table 4.
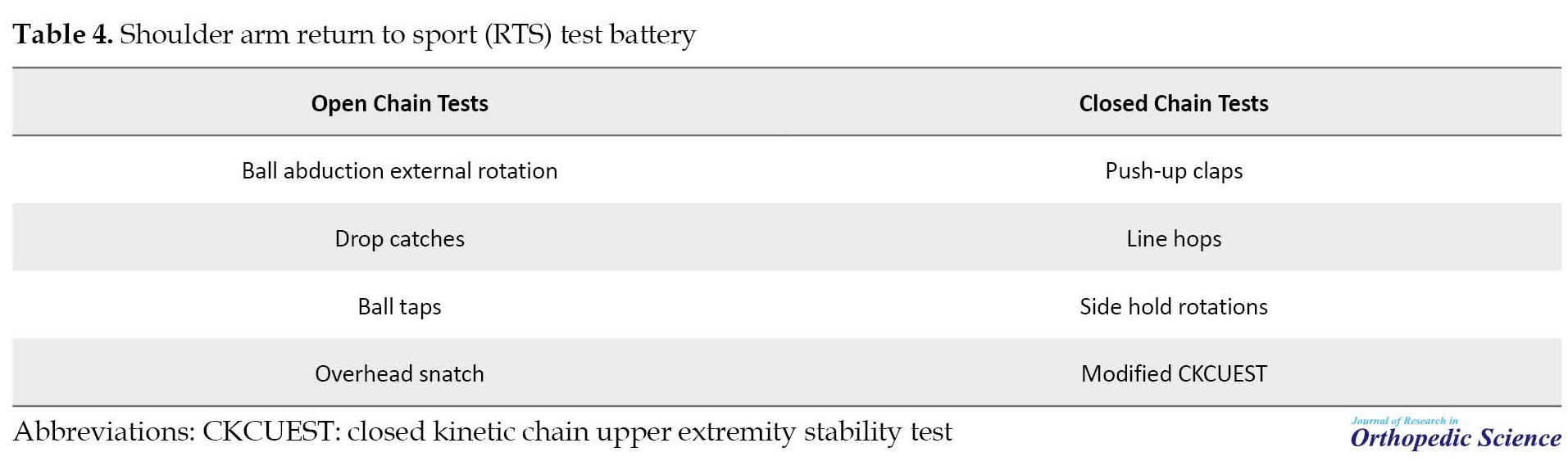
The results of this research demonstrated six of the eight tests in the shoulder arm return to sports test show fine psychometric properties to assess both closed and open-chain upper limb activities designating their preparedness for clinical utilization [16].
Borms et al. studied the upper limb functional performance test, reference values for overhead athletes’ functional tests used in present research included SMBT, CKCUEST, and upper quarter Y balance test (YBT-UQ). To sum up, this research provides normative data for the upper quarter Y balance test (YBT-UQ), CKCUEST, and seated medicine ball throw, which clinically pertinent for screening overhead athletes in terms of performance and their performance relative to others of the same age, gender, and sports [35]. Chmielewski et al. investigated standardization reflections for utilizing the one-sided seated shot-put test in rehabilitation. The results of this study showed that acquiring these data may ease the use of the one-sided seated shot-put test for RTS decision-making in upper limb rehabilitation. In limb comparison, the dominant side should perform 5% to 10% better, and performance benchmarks should be set based on gender [26]. Manske and Reiman studied functional performance testing for RTS and power. In this study, the seated shot-put throw test was executed. The results of this study showed functional performance tests can assist in deciding when an athlete can go back to unlimited activity [36]. Negrete et al. investigated minimal detectable change and normative values reliability for tests of upper limb power and function. In this study, a functional seated shot-put test for the nondominant arms and dominant, modified pull-up, and push-up tests were executed. The results of this study showed that returning to daily life activities in full or sports ought to be based on the suitable performance of the whole of the tests in succession. The present research may help in the progress of a serial testing paradigm for use through the training and rehabilitation of patients with upper limb injuries [37].
Reliability of functional tests
Table 5 presents the reliability of the performance tests.

4. Discussion
This review was conducted to assess and identify functional tests and their reliability to RTS after shoulder injuries. The results of this research showed that little research has been conducted in this field and it is a new research field. Thus, after the survey, only 12 studies presented functional tests for RTS after the trauma of the shoulders. However, two of these studies provided a pack of functional tests for RTS after the trauma of the shoulder. In the first study conducted by Olds et al., the reliability of a shoulder arm RTS group test was examined. In this study, the tests were split into two groups of open and closed-chain tests. Each group consisted of 4 tests [16]. In the second study conducted by Wilk et al., the participation criteria of the RTS after injury of the shoulder were examined. In this study, 17 functional tests for RTS after Microtrauma and Macrotrauma shoulder injuries were reported [7]. This study is both more recent and more complete than Olds et al.’s study and also provides a certain amount and numerical range for some functional tests. For example, in the CKCUEST, for an athlete to be allowed to RTS, his record in this test must be ≥25 repetitions. This study also divided shoulder injuries into two groups including Microtrauma and Macrotrauma injuries while providing specific functional tests for each group [7]. Also, the results of the study conducted by Popchak et al. demonstrated all isokinetic (ICC: 0.88-0.94), functional assessments (ICC: 0.80-0.92), and isometric (ICC: 0.83-0.94) had fine to very good intra-rater reliability, while repetition to failure testing had low to average reliability (ICC: 0.48-0.57) [8].
The topic of RTS after a shoulder injury has become vital in the rehabilitation program today because the athlete should reach the previous level of preparation for RTS. To ascertain if an athlete is prepared for RTS, various tools are used, one of the most practical and inexpensive of which is functional tests, which are recommended for several reasons, these tests are similar to the athlete’s movement patterns, these tests have the necessary capabilities to assess the athlete’s physical fitness, in addition to the global components of the movement system, these tests also pay attention to the local components of the movement system, the tests are tailored to the needs of the athlete, these tests identify the strengths and weaknesses of movement patterns, these tests are made of inexpensive tools and equipment and can be used in sports environments, and finally, these tests can gauge an athlete’s preparedness to RTS [29, 44].
However, the point is that the functional tests used in the studies evaluated some physical factors and ignored the evaluation of some factors. Most tests presented in the studies evaluated the strength, stability, and range of motion of the shoulder. These factors are indeed the main elements of an athlete’s mobility, but it can also be crucial to consider some other factors, such as muscle endurance, coordination, and reaction time [29]. Because as much as an athlete needs stability and strength in the shoulder joint, he can also need endurance and coordination of the shoulder joint muscles. To improve the movement pattern and RTS, it is essential to pay attention to all the elements of physical fitness of the upper limbs, especially the shoulder joint. Considering that most of the research conducted in the field of RTS after shoulder injury was conducted from 2018 to 2021. It indicates that a new field of study is ahead and, in the future, it can be expected that new studies will address the issues mentioned and cover the weaknesses of previous studies and more functional tests to the functional battery RTS tests after adding shoulder injuries, the result of which can be the athlete RTS and competition environment as fully as possible.
5. Conclusion
Functional tests can assist in ascertaining when athletes can RTS or exercise without restrictions. However, more research is needed to quantify the tests. In addition, it is essential to convert quantities to standard norms for reference in other studies because little information exists about functional tests to return to activity after an injury of the shoulder. One of the limitations of the present study was that only studies published in English were reviewed, and more extensive research was needed. Therefore, according to the results of the current research, it can be noted that functional tests can be an effective tool to assess RTS after shoulder injuries, but due to the limitations and shortcomings in this area, it is required to conduct further research, such as normalizing functional tests for RTS and providing a functional battery test for RTS after shoulder injuries. Therefore, caution should be taken and a general rule should not be drawn for all shoulder injuries.
Ethical Considerations
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Injured athletes seeking to return to sport (RTS) or exercise to previous levels before shoulder injury have to recapture muscle vigor, dynamic stability, and shoulder function [1]. Nevertheless, due to the dearth of evidence-based criteria to precisely evaluate the glenohumeral joint dynamic stability [2], clinical doctors utilize associated evaluations, such as function and strength to ascertain preparedness for RTS [3, 4, 5, 6, 7]. In addition, it is unlikely that any test method can demonstrate dynamic stability. Therefore, the use of objective and clinical testing etiquettes is vital to direct RTS after shoulder traumas [8]. Determining the timing of RTS after shoulder damage and the dearth of reliable and valid tests is a major problem for clinicians [9, 10]. Professional athletes who are away from sports for a long time due to shoulder injuries, it can jeopardize their career opportunities [11]. Moreover, the recurrence rate of shoulder instability after a dislocation of the shoulder can be higher than 50% with both non-surgical and surgical therapy being successful [12, 13]. In another study, the reoccurrence rate of dislocation was 40% in patients younger than 20 years, and 63% in 20 to 40 years [14, 15]. It shows that improvement in decision-making for RTS after shoulder injury is essential and a crucial step to facilitate decision-making is to create physical performance tests [16]. Wilson et al. [17] designed a practical etiquette to evaluate readiness for RTS. The etiquette used isokinetic external and internal strength, two functional evaluations, lateral rotation endurance testing, the unilateral seated shot-put test, and the closed kinetic chain upper extremity stability test (CKCUEST). This etiquette showed remarkable deficiencies in people who wanted RTS after six months of shoulder stabilization [17]. While this etiquette is vital in deciding to RTS, it has limitations that should be considered. First, this etiquette uses an isokinetic strength test, which is a time-intensive and costly test and is not commonly used in many clinical environments [18]. Even though isokinetic evaluation is the standard criteria to evaluate shoulder strength [19, 20], isometric testing through manual dynamometry is an alternative method that is more feasible to be performed by clinicians. The second one is the psychometric properties, especially the reliability and validity [21]. Physical performance tests should be uncomplicated, inexpensive, and applicable in clinics [22, 23]. In clinical trials, attention should be paid to the sport to which the athlete wants to return because many variations exist in the requests of various sports [24]. Moreover, despite most sports requiring athletes to exercise for a prolonged duration of time, contemporary physical performance tests announce secluded efforts [25-28] and do not determine toleration ability. Therefore, a one-time test may not precisely estimate the preparedness of an athlete for RTS for the required period, meaningful performance tests that inspect tolerance are needed [16]. Eventually, tests that measure only one construct have limited clinical utility. Therefore, tests that measure all the various constructs, such as strength, range of motion, power, and neuromuscular control may enhance the capability to ascertain a secure RTS (Figure 1) manifests the necessary constituents of the functional test). Therefore, it is essential to design a group of secure, valid, and reliable physical performance tests. Considering that few review studies have been conducted in this field, therefore, the main motive of this review research is to survey and announce the functional tests for RTS after shoulder injuries. Hope that the results of this research will supply guidance for the optimum method of testing in the clinic-based applications and return to the decision-making of sports.
Objectives
A comprehensive review of the functional tests and their reliability for RTS later than injuries of shoulders.
2. Methods
This is a systematic review developed according to the preferred reporting items for systematic reviews and meta-analysis (PRISMA).
Search strategy
In the present research, a comprehensive review of the functional tests for RTS after shoulder injuries were conducted by searching the Web of Science, PEDro, Google Scholar, PubMed, ScienceDirect, SCOPUS, and CINAHL databases with the keywords using three groups of search terms, (group 1) “shoulder return to sport” or “return to play” or “return to competition” or “return to activities” or “return to participation”, and (group 2) “upper limb” or “upper body” or “upper limb” or “shoulder complex”, and (group 3) “shoulder functional tests” or “shoulder functional battery tests” or “shoulder functional assessment” or “shoulder functional evaluation”. These combinations (of three groups) were investigated in keywords, titles, and abstracts of the research published by the indexed journals in the databases that were performed from 2000 to June 2021. Also, a manual search and comprehensive review of research paper sources was conducted to find research papers that cannot be found through electronic search.
Eligibility criteria
The inclusion criteria included athletes or people who underwent rehabilitation programs, and suffered shoulder injuries, such as anterior and posterior instability, dislocations, ruptured rotator cuffs, and use of functional tests to RTS. English-language research papers, full-text studies as well as studies which were randomized control trials, cross-sectional, and cohort designs were published. The exclusion criteria included other shoulder injuries, such as fractures of the proximal arm, and research papers that were published briefly in congresses and seminars.
Study selection
The English language was used in this search. All texts were screened by researchers. Finally, using relevant keywords, 123 research papers were received from databases. At first, the titles of the research papers were examined and 11 duplicate research papers were removed. In the next step, abstracts of 112 research papers were examined, and then 79 research papers were excluded from the study due to non-compliance with the inclusion criteria. In the following, 33 research papers were studied in full text, and after that 21 research papers were removed due to non-compliance with the inclusion criteria (for example, not being in English, not using performance tests for RTS after shoulder injuries, etc.). Finally, 12 research papers were contained in the present review and their results were reported fully. Another senior researcher checked the final list of selected research papers to ensure that all research papers were consistent with the objective of the study. Figure 2 shows the study selection procedure. The population, intervention, comparison, outcomes, and study (PICOS)-type framework is based on the research inquiry stated (Table 1).

3. Results
A search of Web of Science, PEDro, Google Scholar, PubMed, ScienceDirect, Scopus, and CINAHL databases found 123 research papers. After eliminating 11 identical titles, 112 abstracts were selected for review. Then the abstracts were reviewed, 79 research papers were removed and 33 research papers were selected for full-text reading. After reviewing the full-text research papers, 21 research papers were eliminated and 12 research papers were included in the study. The following are the necessary criteria to enter the stage of performing functional tests for RTS (Table 2).
The Results of Research Examining Functional Tests for Returning to Sport (RTS) After Shoulder Injuries
Popchak et al. studied the validity and reliability of RTS testing for the shoulder injury. Thirty healthy active adults with an average age of 24.0±1.6 years participated in this study. Total functional assessments (intraclass correlation coefficient [ICC]: 0.80-0.92), isometric (ICC: 0.83-0.94), and isokinetic (ICC: 0.88-0.94) had fine to very good intra-rater reliability, considering the repetition to failure testing had low to average reliability (ICC: 0.48-0.57). The results of this study also showed that the isometric, isokinetic, and functional evaluations in this testing procedure show admissible reliability and validity [8]. Pontillo et al. studied the use of an upper limb functional testing algorithm to calculate returning-to-play preparedness in collegiate soccer players. Six participants (18 to 21 years old) who experienced shoulder capsulolabral mend participated in this research. Functional tests used in this study included standing cable press, performed at 30% body weight (BW), Scaption, performed at 5% BW, Prone-y, performed at 3% BW and CKCUEST. In this study, it was shown that the upper limb functional testing algorithm assists in evaluating RTS in male collegiate athletes of soccer [31]. Wilk et al. studied the RTS criteria for injury of shoulder: A clinic-based report. In this study, Wilk presented the functional battery tests for RTS after shoulder injuries, which can be seen in Table 3.

The results of this research demonstrated many functional tests, but different tests can be used depending on the type of injury [7].
Hollstadt et al. studied the reliability of test-retest of the CKCUEST in an adjusted test place in dividing I collegiate basketball players. The results of this study showed that the CKCUEST in an adjusted test place is a reliable evaluation device and underpins preceding discoveries [32]. Decleve et al. studied the “upper limb rotation test”, a validity and reliability investigation of an up-to-date upper limb physical performance test. Results showed good reliability. A moderate correlation (r=0.553) was discovered between the CKCUEST and upper lime rotation test (ULRT) scores. A moderate correlation (r=0.556) was found between ULRT and SMBT scores [33]. Wilson et al. built up an objective and functional criterion-based shoulder testing etiquette to assess RTS preparedness in clinic-based environments. The etiquette used was external rotation endurance testing, isokinetic external and internal strength, and two functional evaluations, the CKCUEST and the unilateral seated shot put test. The use of this etiquette disclosed remarkable deficiencies in patients arranging for RTS at six months after shoulder balance. Although this etiquette is essential for RTS decisions, it has limitations that should be noted [17]. Degot et al. studied interrater reliability and consensus of a modified CKCUEST. The results showed that reasonable reliability was discovered for the muscular endurance index calculated while splitting the one-half number of touches computed throughout the final 30s of the one-min set, by the m-CKCUEST score computed above (ICC=0.86). The m-CKCUEST allows for the production of two reliable result measurements that estimate muscular endurance and upper limb stability. The aforementioned results may be utilized in the aftermath to evaluate rehabilitation level or performance [34]. Olds et al. investigated the shoulder arm RTS test reliability. Functional tests within this study were divided into two categories, which can be seen in Table 4.
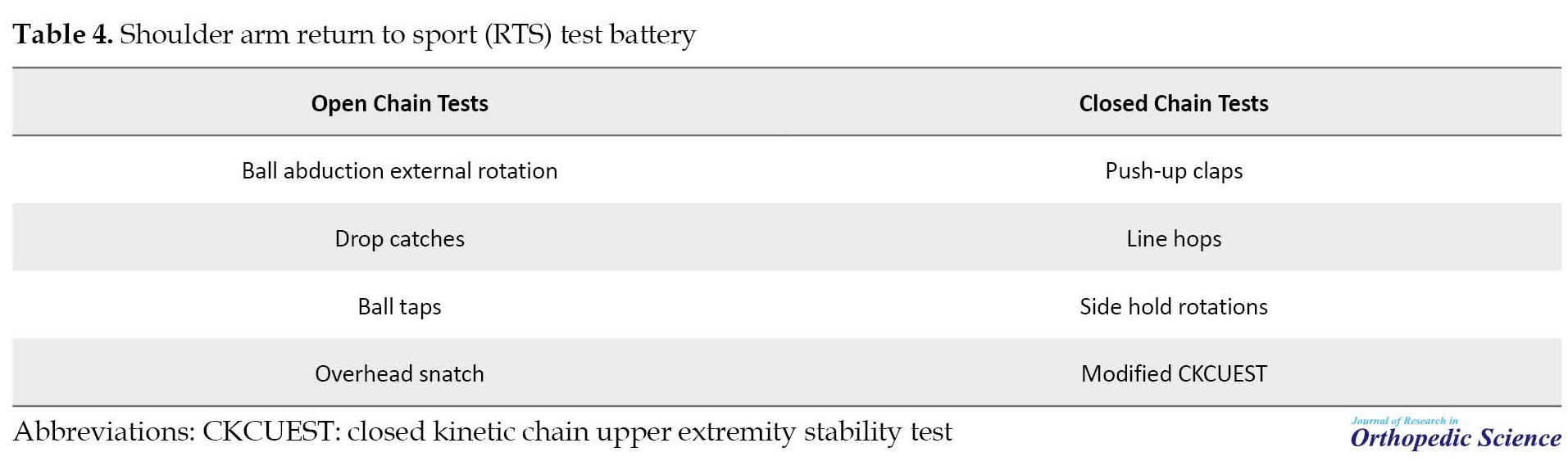
The results of this research demonstrated six of the eight tests in the shoulder arm return to sports test show fine psychometric properties to assess both closed and open-chain upper limb activities designating their preparedness for clinical utilization [16].
Borms et al. studied the upper limb functional performance test, reference values for overhead athletes’ functional tests used in present research included SMBT, CKCUEST, and upper quarter Y balance test (YBT-UQ). To sum up, this research provides normative data for the upper quarter Y balance test (YBT-UQ), CKCUEST, and seated medicine ball throw, which clinically pertinent for screening overhead athletes in terms of performance and their performance relative to others of the same age, gender, and sports [35]. Chmielewski et al. investigated standardization reflections for utilizing the one-sided seated shot-put test in rehabilitation. The results of this study showed that acquiring these data may ease the use of the one-sided seated shot-put test for RTS decision-making in upper limb rehabilitation. In limb comparison, the dominant side should perform 5% to 10% better, and performance benchmarks should be set based on gender [26]. Manske and Reiman studied functional performance testing for RTS and power. In this study, the seated shot-put throw test was executed. The results of this study showed functional performance tests can assist in deciding when an athlete can go back to unlimited activity [36]. Negrete et al. investigated minimal detectable change and normative values reliability for tests of upper limb power and function. In this study, a functional seated shot-put test for the nondominant arms and dominant, modified pull-up, and push-up tests were executed. The results of this study showed that returning to daily life activities in full or sports ought to be based on the suitable performance of the whole of the tests in succession. The present research may help in the progress of a serial testing paradigm for use through the training and rehabilitation of patients with upper limb injuries [37].
Reliability of functional tests
Table 5 presents the reliability of the performance tests.

4. Discussion
This review was conducted to assess and identify functional tests and their reliability to RTS after shoulder injuries. The results of this research showed that little research has been conducted in this field and it is a new research field. Thus, after the survey, only 12 studies presented functional tests for RTS after the trauma of the shoulders. However, two of these studies provided a pack of functional tests for RTS after the trauma of the shoulder. In the first study conducted by Olds et al., the reliability of a shoulder arm RTS group test was examined. In this study, the tests were split into two groups of open and closed-chain tests. Each group consisted of 4 tests [16]. In the second study conducted by Wilk et al., the participation criteria of the RTS after injury of the shoulder were examined. In this study, 17 functional tests for RTS after Microtrauma and Macrotrauma shoulder injuries were reported [7]. This study is both more recent and more complete than Olds et al.’s study and also provides a certain amount and numerical range for some functional tests. For example, in the CKCUEST, for an athlete to be allowed to RTS, his record in this test must be ≥25 repetitions. This study also divided shoulder injuries into two groups including Microtrauma and Macrotrauma injuries while providing specific functional tests for each group [7]. Also, the results of the study conducted by Popchak et al. demonstrated all isokinetic (ICC: 0.88-0.94), functional assessments (ICC: 0.80-0.92), and isometric (ICC: 0.83-0.94) had fine to very good intra-rater reliability, while repetition to failure testing had low to average reliability (ICC: 0.48-0.57) [8].
The topic of RTS after a shoulder injury has become vital in the rehabilitation program today because the athlete should reach the previous level of preparation for RTS. To ascertain if an athlete is prepared for RTS, various tools are used, one of the most practical and inexpensive of which is functional tests, which are recommended for several reasons, these tests are similar to the athlete’s movement patterns, these tests have the necessary capabilities to assess the athlete’s physical fitness, in addition to the global components of the movement system, these tests also pay attention to the local components of the movement system, the tests are tailored to the needs of the athlete, these tests identify the strengths and weaknesses of movement patterns, these tests are made of inexpensive tools and equipment and can be used in sports environments, and finally, these tests can gauge an athlete’s preparedness to RTS [29, 44].
However, the point is that the functional tests used in the studies evaluated some physical factors and ignored the evaluation of some factors. Most tests presented in the studies evaluated the strength, stability, and range of motion of the shoulder. These factors are indeed the main elements of an athlete’s mobility, but it can also be crucial to consider some other factors, such as muscle endurance, coordination, and reaction time [29]. Because as much as an athlete needs stability and strength in the shoulder joint, he can also need endurance and coordination of the shoulder joint muscles. To improve the movement pattern and RTS, it is essential to pay attention to all the elements of physical fitness of the upper limbs, especially the shoulder joint. Considering that most of the research conducted in the field of RTS after shoulder injury was conducted from 2018 to 2021. It indicates that a new field of study is ahead and, in the future, it can be expected that new studies will address the issues mentioned and cover the weaknesses of previous studies and more functional tests to the functional battery RTS tests after adding shoulder injuries, the result of which can be the athlete RTS and competition environment as fully as possible.
5. Conclusion
Functional tests can assist in ascertaining when athletes can RTS or exercise without restrictions. However, more research is needed to quantify the tests. In addition, it is essential to convert quantities to standard norms for reference in other studies because little information exists about functional tests to return to activity after an injury of the shoulder. One of the limitations of the present study was that only studies published in English were reviewed, and more extensive research was needed. Therefore, according to the results of the current research, it can be noted that functional tests can be an effective tool to assess RTS after shoulder injuries, but due to the limitations and shortcomings in this area, it is required to conduct further research, such as normalizing functional tests for RTS and providing a functional battery test for RTS after shoulder injuries. Therefore, caution should be taken and a general rule should not be drawn for all shoulder injuries.
Ethical Considerations
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Popchak A, Patterson-Lynch B, Christain H, Irrgang JJ. Rehabilitation and return to sports after anterior shoulder stabilization. Ann Jt. 2017; 2(10):62. [DOI:10.21037/aoj.2017.10.06]
- Magarey ME, Jones MA. Dynamic evaluation and early management of altered motor control around the shoulder complex. Man Ther. 2003; 8(4):195-206. [DOI:10.1016/S1356-689X(03)00094-8] [PMID]
- Alentorn-Geli E, Álvarez-Díaz P, Doblas J, Steinbacher G, Seijas R, Ares O, et al. Return to sports after arthroscopic capsulolabral repair using knotless suture anchors for anterior shoulder instability in soccer players: Minimum 5-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2016; 24(2):440-6. [DOI:10.1007/s00167-015-3895-y] [PMID]
- Garofalo R, Mocci A, Moretti B, Callari E, Di Giacomo G, Theumann N, et al. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy. 2005; 21(11):1283-9. [DOI:10.1016/j.arthro.2005.08.033] [PMID]
- Hart D, Funk L. Serious shoulder injuries in professional soccer: Return to participation after surgery. Knee Surg Sports Traumatol Arthrosc. 2015; 23(7):2123-9. [DOI:10.1007/s00167-013-2796-1] [PMID]
- Ozturk BY, Maak TG, Fabricant P, Altchek DW, Williams RJ, Warren RF, et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy: Arthroscopy. 2013; 29(12):1922-31. [DOI:10.1016/j.arthro.2013.09.008] [PMID]
- Wilk KE, Bagwell MS, Davies GJ, Arrigo CA. Return to sport participation criteria following shoulder injury: A clinical commentary. Int J Sports Phys Ther. 2020; 15(4):624-42. [DOI:10.26603/ijspt20200624] [PMID] [PMCID]
- Popchak A, Poploski K, Patterson-Lynch B, Nigolian J, Lin A. Reliability and validity of a return to sports testing battery for the shoulder. Phys Ther Sport. 2021; 48:1-11. [DOI:10.1016/j.ptsp.2020.12.003] [PMID]
- Cools AM, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyskinesis: From the office worker to the elite overhead athlete. Br J Sports Med. 2014; 48(8):692-7. [DOI:10.1136/bjsports-2013-092148] [PMID]
- Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return-to-play in sport: A decision-based model. Clin J Sport Med. 2010; 20(5):379-85. [DOI:10.1097/JSM.0b013e3181f3c0fe] [PMID]
- Headey J, Brooks JH, Kemp SP. The epidemiology of shoulder injuries in English professional rugby :union:. Am J Sports Med. 2007; 35(9):1537-43. [DOI:10.1177/0363546507300691] [PMID]
- Torrance E, Clarke CJ, Monga P, Funk L, Walton MJ. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. 2018; 46(12):2969-74. [DOI:10.1177/0363546518794673] [PMID]
- Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989; 5(3):213-7.[DOI:10.1016/0749-8063(89)90174-6] [PMID]
- Akbari Aghdam H, Dehghani M, Karimi P. Evaluation of recurrence rate and risk factors affecting recurrence of recurrent shoulder dislocation in Kashani Hospital in 2017-2018. J Res Orthop Sci. 2021; 8(2):77-82. [DOI:10.32598/JROSJ.8.2.750.1]
- Mardani-Kivi M, Shirangi A, Mardani-Kivi A, Haghparast Ghadim-Limudahi Z, Izadi A. Shoulder disorders: The challenging issue among orthopedic surgeons. J Res Orthop Sci. 2021. 8(2):83-94. [DOI:10.32598/JROSJ.8.2.769.1]
- Olds M, Coulter C, Marant D, Uhl T. Reliability of a shoulder arm return to sport test battery. Phys Ther Sport. 2019; 39:16-22. [DOI:10.1016/j.ptsp.2019.06.001] [PMID]
- Wilson KW, Popchak A, Li RT, Kane G, Lin A. Return to sport testing at 6 months after arthroscopic shoulder stabilization reveals residual strength and functional deficits. J Shoulder Elbow Surg. 2020; 29(7S):S107-14. [DOI:10.1016/j.jse.2020.04.035] [PMID]
- Holt KL, Raper DP, Boettcher CE, Waddington GS, Drew MK. Hand-held dynamometry strength measures for internal and external rotation demonstrate superior reliability, lower minimal detectable change and higher correlation to isokinetic dynamometry than externally-fixed dynamometry of the shoulder. Phys Ther Sport. 2016; 21:75-81. [DOI:10.1016/j.ptsp.2016.07.001] [PMID]
- Borms D, Maenhout A, Cools AM. Upper quadrant field tests and isokinetic upper limb strength in overhead athletes. J Athl Train. 2016; 51(10):789-96. [DOI:10.4085/1062-6050-51.12.06] [PMID] [PMCID]
- Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: A systematic review. PM&R. 2011; 3(5):472-9. [DOI:10.1016/j.pmrj.2010.10.025] [PMID]
- Popchak AJ, Lynch AD, Irrgang JJ. Framework for selecting clinical outcomes for clinical trials, In: Musahl V, editor. Basic methods handbook for clinical orthopaedic research. Berlin: Springer; 2019. [DOI:10.1007/978-3-662-58254-1_15]
- Ardern CL, Bizzini M, Bahr R. It is time for consensus on return to play after injury: Five key questions. Br J Sports Med. 2016; 50(9):506-8. [DOI:10.1136/bjsports-2015-095475] [PMID]
- Goldbeck TG, Davies GJ. Test-Retest reliability of the closed kinetic chain upper extremity stability test: A clinical field test. J Sport Rehabil. 2000; 9(1):35-45. [DOI:10.1123/jsr.9.1.35]
- Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: Collision athletes versus noncollision athletes. Arthroscopy. 2006; 22(9):947-53. [DOI:10.1016/j.arthro.2006.05.015] [PMID]
- Ashworth B, Hogben P, Singh N, Tulloch L, Cohen DD. The Athletic Shoulder (ASH) test: Reliability of a novel upper body isometric strength test in elite rugby players. BMJ Open Sport Exerc Med. 2018; 4(1):e000365. [DOI:10.1136/bmjsem-2018-000365] [PMID] [PMCID]
- Chmielewski TL, Martin C, Lentz TA, Tillman SM, Moser MW, Farmer KW, et al. Normalization considerations for using the unilateral seated shot put test in rehabilitation. J Orthop Sports Phys Ther. 2014; 44(7):518-24. [DOI:10.2519/jospt.2014.5004] [PMID]
- Gorman PP, Butler RJ, Plisky PJ, Kiesel KB. Upper Quarter Y Balance Test: Reliability and performance comparison between genders in active adults. J Strength Cond Res. 2012; 26(11):3043-8. [DOI:10.1519/JSC.0b013e3182472fdb] [PMID]
- Harris C, Wattles AP, DeBeliso M, Sevene-Adams PG, Berning JM, Adams KJ. The seated medicine ball throw as a test of upper body power in older adults. J Strength Cond Res. 2011; 25(8):2344-8. [DOI:10.1519/JSC.0b013e3181ecd27b] [PMID]
- Reiman, MP, Manske RC. Functional testing in human performance. Champaign: Human Kinetics; 2009. [DOI:10.5040/9781492596882]
- Jonathan F. Owens B. Shoulder instability in the athlete: Management and surgical techniques for optimized return to play. New Jersey:SLACK Incorporated; 2020. [Link]
- Pontillo M, Sennett BJ, Bellm E. Use of an upper extremity functional testing algorithm to determine return to play readiness in Collegiate football players: A case series. Int J Sports Phys Ther. 2020; 15(6):1141-50. [DOI:10.26603/ijspt20201141] [PMID] [PMCID]
- Hollstadt K, Boland M, Mulligan I. Test-retest reliability of the Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST) in a modified test position in division I collegiate basketball players. Int J Sports Phys Ther. 2020; 15(2):203-9. [DOI:10.26603/ijspt20200203] [PMID] [PMCID]
- Decleve P, Attar T, Benameur T, Gaspar V, Van Cant J, Cools AM. The “upper limb rotation test”: Reliability and validity study of a new upper extremity physical performance test. Phys Ther Sport. 2020; 42:118-23. [DOI:10.1016/j.ptsp.2020.01.009] [PMID]
- Degot M, Blache Y, Vigne G, Juré D, Borel F, Neyton L, et al. Intrarater reliability and agreement of a modified closed kinetic chain upper extremity stability test. Phys Ther Sport. 2019; 38:44-8. [DOI:10.1016/j.ptsp.2019.04.017] [PMID]
- Borms D, Cools A. Upper-extremity functional performance tests: Reference values for overhead athletes. Int J Sports Med. 2018; 39(6):433-41. [DOI:10.1055/a-0573-1388] [PMID]
- Manske R, Reiman M. Functional performance testing for power and return to sports. Sports Health. 2013; 5(3):244-50. [DOI:10.1177/1941738113479925] [PMID] [PMCID]
- Negrete RJ, Hanney WJ, Kolber MJ, Davies GJ, Ansley MK, McBride AB, et al. Reliability, minimal detectable change, and normative values for tests of upper extremity function and power. J Strength Cond Res. 2010; 24(12):3318-25. [DOI:10.1519/JSC.0b013e3181e7259c] [PMID]
- Burnstein BD, Steele RJ, Shrier I. Reliability of fitness tests using methods and time periods common in sport and occupational management. J Athl Train. 2011; 46(5):505-13. [DOI:10.4085/1062-6050-46.5.505] [PMID] [PMCID]
- Davies GJ, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation of the shoulder complex. J Orthop Sports Phys Ther. 1993; 18(2):449-58. [DOI:10.2519/jospt.1993.18.2.449] [PMID]
- Seo DI, Kim E, Fahs CA, Rossow L, Young K, Ferguson SL, et al. Reliability of the one-repetition maximum test based on muscle group and gender. J Sports Sci Med. 2012; 11(2): 221-5. [PMID]
- Westrick RB, Miller JM, Carow SD, Gerber JP. Exploration of the y-balance test for assessment of upper quarter closed kinetic chain performance.Int J Sports Phys Ther. 2012; 7(2):139-47. [PMID]
- Falsone SA, Gross MT, Guskiewicz KM, Schneider RA. One-arm hop test: Reliability and effects of arm dominance. J Orthop Sports Phys Ther. 2002; 32(3):98-103. [DOI:10.2519/jospt.2002.32.3.98] [PMID]
- Collins DR, Hodges PB. A chomprehensive guide to sports skills test and measurement. Maryland: Scarecrow Press; 2001. [Link]
- Liebenson C. Functional training handbook. Pennsylvania: Wolters Kluwer Health; 2014. [Link]
Type of Study: Review Paper |
Subject:
Shoulder / Elbow
Received: 2022/07/28 | Accepted: 2022/12/24 | Published: 2022/05/1
Received: 2022/07/28 | Accepted: 2022/12/24 | Published: 2022/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |