Volume 9, Issue 2 (5-2022)
JROS 2022, 9(2): 87-92 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bagherifard A, Yahyazadeh H, Karimi Heris H. Short-term Outcomes of Semi-constrained Implants in Patients With Complex Primary Total Knee Arthroplasty. JROS 2022; 9 (2) :87-92
URL: http://jros.iums.ac.ir/article-1-2202-en.html
URL: http://jros.iums.ac.ir/article-1-2202-en.html
1- Bone and Joint Reconstruction Research Center, Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 484 kb]
(422 Downloads)
| Abstract (HTML) (1626 Views)
Full-Text: (451 Views)
1. Introduction
Total knee arthroplasty (TKA) is the choice of treatment for end-stage osteoarthritis [1]. Although most patients are satisfied with the results of TKA, almost one in five TKA patients are not satisfied for various reasons, such as unmet expectations or postoperative complications, such as instability and aseptic loosening [2]. Considering the growing number of TKA surgeries caused by the increased rate of obesity and aging in society [3], improving the outcomes of TKA and patients’ satisfaction is of critical importance.
Coronal stability is the cornerstone of a successful TKA [4], which is achieved with soft-tissue balancing and using unconstrained implants. However, in complex cases, such as patients with severe knee deformity, a more constrained implant is required to achieve adequate balance and coronal stability. Although constrained prosthesis provides better stability, it is associated with decreased survival and increased rate of complications, such as aseptic loosening [5, 6]. For this reason, a less constrained prosthesis (semi-constrained implant) was developed to reduce the detrimental impact of constrained implants on the patients’ outcomes [7]. However, the outcomes of TKA using semi-constrained implants are mainly unknown.
Objectives
This study was conducted to retrospectively evaluate the short-term outcomes and complications of primary TKA in a cohort of 23 patients with end-stage osteoarthritis who were managed with a semi-constrained implant.
2. Methods
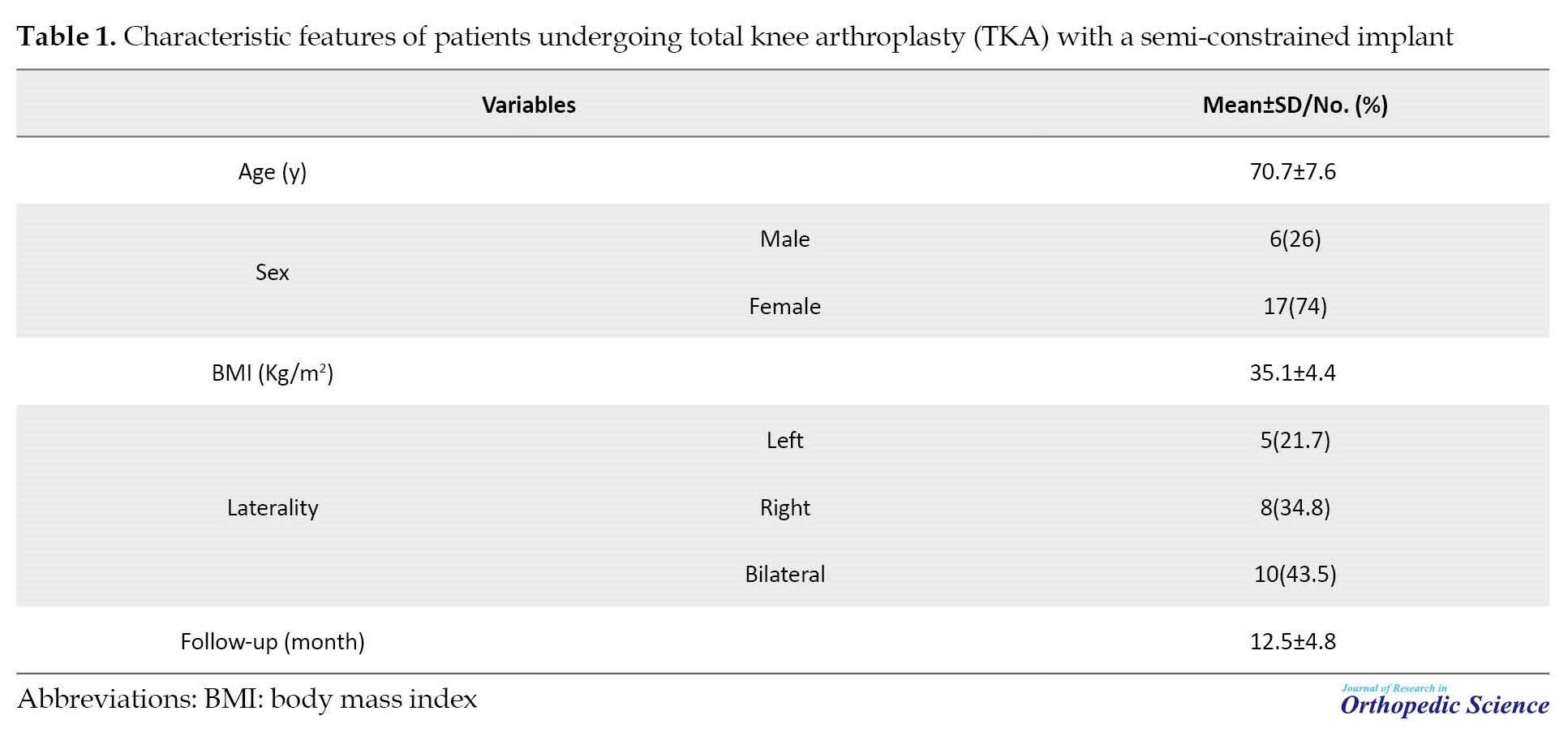
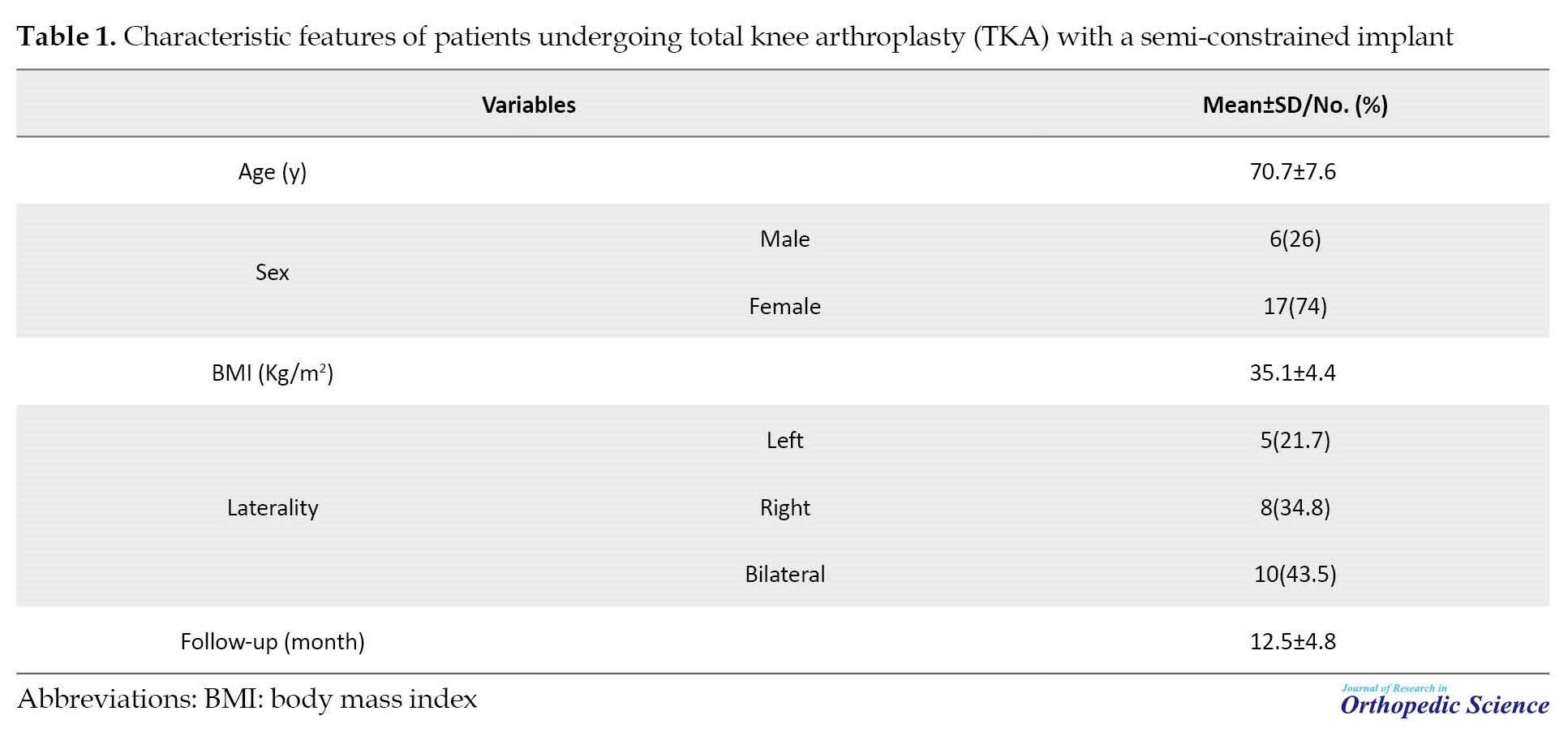
This study was approved by the Ethics Committee of Iran University of Medical Sciences under the code IR.IUMS.REC.1400.1217. Between November 2018 and August 2020, medical profiles of the patients who underwent primary TKA with the use of a Stryker Triathlon posterior stabilized TKA (Kalamazoo, MI) with a total stabilized tibial polyethylene insert were reviewed. Patients with follow-up of less than 12 months and those who were lost to the follow-up were excluded from the study. Twenty-three patients (33 knees) were included in the final analysis. The study population included 6 men (26%) and 17 women (74%). The mean age of the patients was 70.7±7.6 years (range 66-74). The mean body mass index (BMI) of the patients was 35.1±4.4 kg/m2 (range 29.5-39.2). The mean follow-up of the patients was 12.5±2.8 months (range 12-14). Table 1 presents the characteristics of the patients.
Procedure
All procedures were performed by a senior knee surgeon. Using a medial parapatellar approach, a gap-balancing technique was implemented to achieve symmetric flexion and extension gaps. Gap balancing was started with the distal femur cut and continued with the proximal tibial cut. Then, the required extension gap was calculated, and medial/lateral released by pie crusting of the medial collateral ligament or lateral collateral ligament to achieve a symmetric extension gap. After that, the flexion gap was set to achieve the same value as the extension gap. A semi-constrained TKA was indicated if the knee was not adequately balanced with these procedures or the collateral ligaments were incompetent. Patellar resurfacing was not performed for any of the patients. All implants were cemented. Postoperatively, a knee brace was used for one week. Wait-bearing was allowed as tolerated.
Outcome measures
The outcome of the patients was evaluated radiographically and clinically. In each follow-up visit, standing lateral and anteroposterior radiographs, alignment view radiographs, and Merchant view radiographs were obtained. Postoperative tibiofemoral alignment was evaluated on recent radiographs.
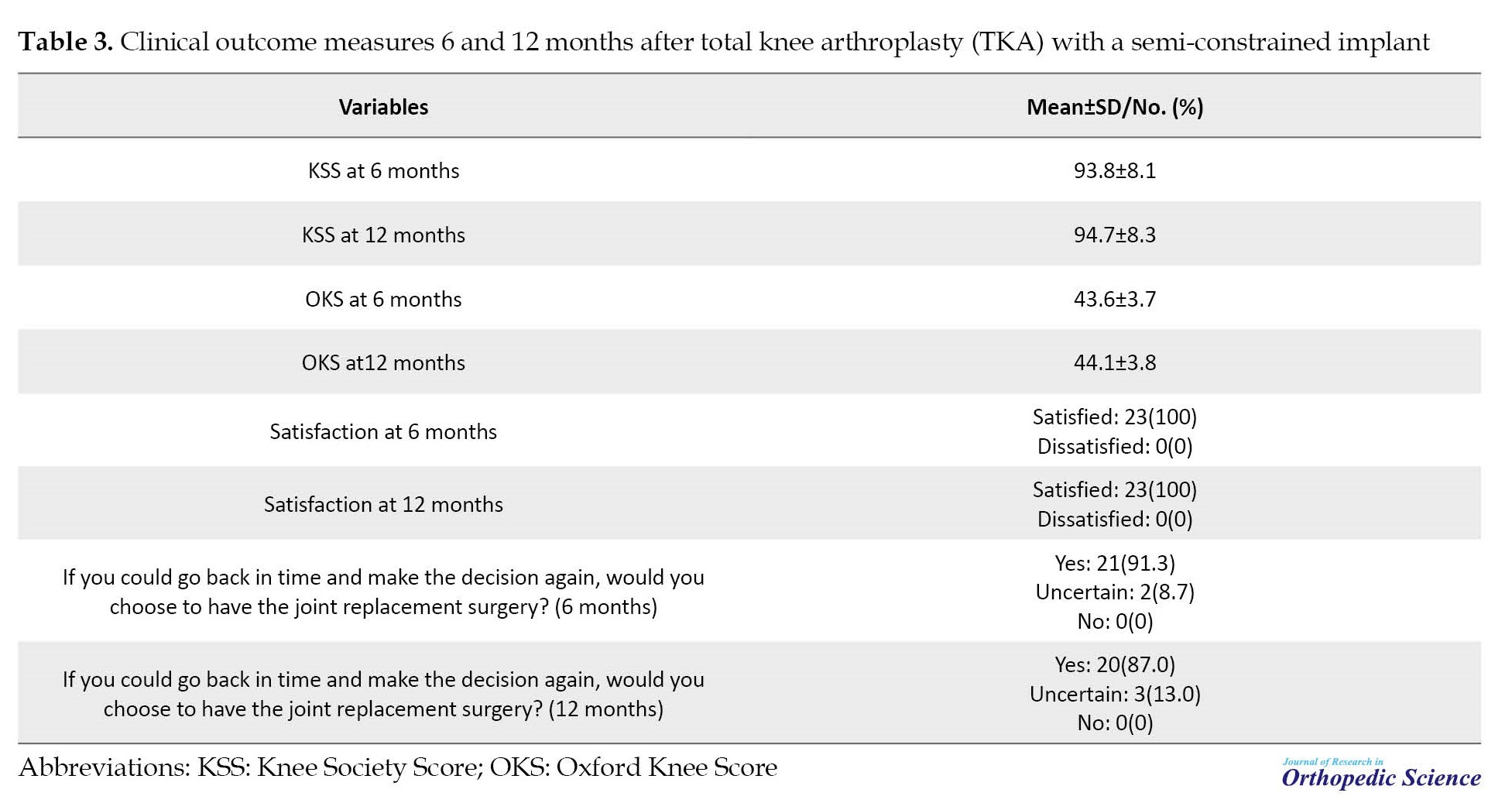
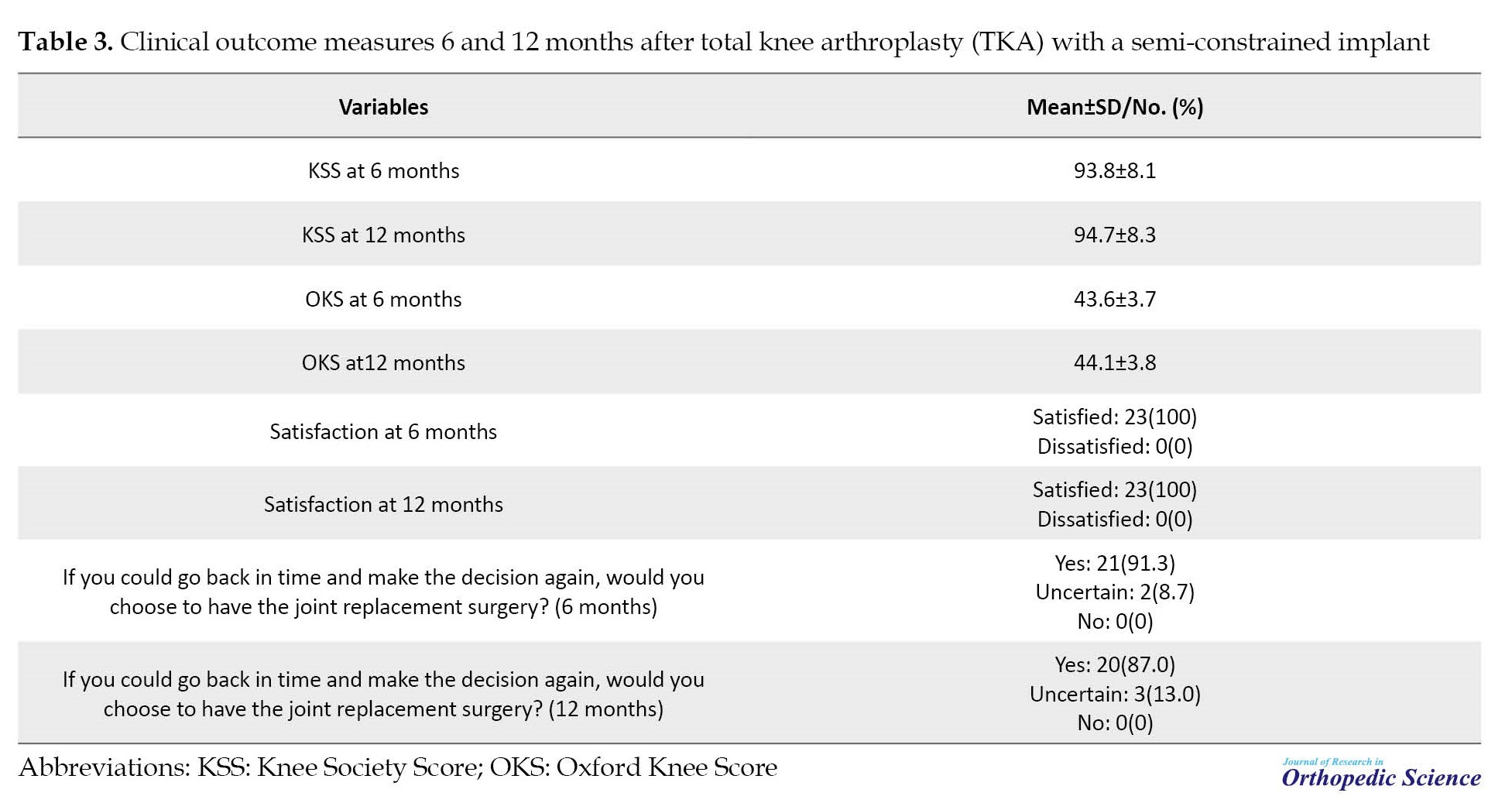
Clinical evaluation of the knee function was performed prospectively using the knee society score (KSS) and Oxford knee score (OKS). The KSS ranged from 0 to 100, with a higher score demonstrating a better function. KSS was also categorized as follows, excellent (score ≥ 90), good (score 77-90), fair (score 65-77), and poor (score <65) [8].
The OKS ranged between 0 and 48, with higher scores indicating better outcomes. The subjective satisfaction of the patients and their re-choice to undergo the same operation were evaluated with yes/no questions. Clinical evaluations were performed two times, once after six months and the other one after one year.
3. Results
Radiographic outcomes
The mean knee extension was 8.7±7.9º (range 0–20°) before the surgery and 3.1±3º (range, 0–10°) after the surgery. The mean knee flexion was 100.8±17.2º (range 65–120°) before the surgery and 119.2±14.2º (range, 90–130°) after the operation. According to the preoperative standing radiographs, a varus deformity was present in 29 (87%) knees. The mean varus angle was 14.2±5.1º (range 9-21°). The preoperative valgus deformity was present in 4 knees (13%). The mean valgus angle was 6.1±2.1° (range 5-9°). The average postoperative tibiofemoral alignment was 0.26±1.1º of valgus (ranging from 3º valgus to 2º of varus) (Table 2).

Clinical outcomes
Six months after the operation, the mean KSS of the patients was 93.8±8.1 (excellent in 19 patients and good in four patients). After 12 months, the mean KSS of the patients was 94.7±8.3 (excellent in 20 patients and good in four patients).
The mean OKS of the patients 6 and 12 months after the operation were 43.6±3.7 and 44.1±3.8, respectively. At 12 months, all the patients were satisfied with the results of TKA. Twenty patients (87%) stated that they would select the same procedure if they were to go back in time and decide again. The remaining three (13%) patients were uncertain (Table 3).
Complications
Superficial or deep infection was not seen in any of the patients. No case of aseptic loosening was recorded until the last follow-up. Also, no hardware failure or periprosthetic fracture was recorded as well. In addition, deep vein thrombosis was not detected in any of the patients.
4. Discussion
In this study, we evaluated the short-term outcomes and postoperative complications of semi-constrained TKA. After 12 months, the knee function was excellent in 20 patients (87%) and good in 3 patients (13%). None of the patients had varus or valgus deformity, according to the tibiofemoral alignment view radiographs. Aseptic loosening did not occur in any of the patients. No other postoperative complications, such as periprosthetic fracture, hardware failure, and infection were observed.
In 2011, Lachiewicz and Soileau [9] first reported the outcomes of the second-generation constrained condylar prosthesis in primary TKA in 27 knees with a mean follow-up time of 5.4 years. The most common indications for the use of the second-generation constrained condylar prosthesis were severe valgus deformity and incompetent medial collateral ligament. None of the patients required a revision TKA during the follow-up period. Aseptic loosening, prosthetic fracture, tibial fracture, and patella problems were not observed in any of the patients. A minimally displaced patella fracture was observed in two knees, which was not asymptomatic. We considered the same indications for the use of a semi-constrained prosthesis. The mean follow-up of the patients was considerably shorter in our study. Similar to the study of Lachiewicz and Soileau, we observed no serious complications following the implication of a semi-constrained prosthesis.
The results of semi-constrained TKA have been reported in a small number of previous studies. Sabatini et al. [10] reported their experience using semi-constrained prostheses in primary TKA. Twenty-eight patients who underwent second-generation semi-constrained knee arthroplasty were included in their study. All patients were >75 years of age and had a severe deformity. The mean follow-up of the patients was 31.3 months. The mean KSS improved from 30 points before the operation to 92.1 points at the last follow-up. A full-extension knee was achieved in all patients. No radiolucent lines were observed during the radiographic evaluation. No deep infections or periprosthetic fractures were observed in any of the patients. Aseptic loosening was not seen in any of the patients as well. In our study, the mean KSS of patients was 94.7 at 12 months after the operation, which was comparable to the study of Sabatini et al. Similarly, no postoperative complications, such as aseptic loosening and periprosthetic fracture were observed in our cohort.
Martin et al. [7] aimed to investigate whether differences were observed in clinical and or radiographic outcomes for those who required a semi-constrained implant with a TS tibial insert and those who did not (primary TKA design with a posterior stabilized [PS] insert). Seventy-five patients were included in each group. The average follow-up of the study was 25 months. While the TS group had significantly greater preoperative varus, the two groups were similar in terms of postoperative revision, reoperation, and other complications. Aseptic loosening occurred in one patient in the TS group and no patient in the PS group. No aseptic loosening was observed in our series. However, it should be noted that our follow-up was shorter, and the number of patients was less (12.5 months, 23 patients).
Johnson et al. [11] evaluated functional outcomes and implant survival in a series of 23 TKA patients under the age of 60 years managed with semi-constrained prostheses. At a 66-month follow-up, Western Ontario and McMaster University Osteoarthritis Index scores and KSS were 15.7 and 94.7, respectively. The patient-reported outcomes were not different between one year and the final follow-up. Aseptic loosening was not seen in any of the patients. All patients kept the implants until the last follow-up with a satisfaction rate of 85.7%. Excellent or good results were reported by 92% of the patients. Although the follow-up period of our study was significantly smaller, the patient’s functional outcome (KSS), satisfaction rate, and implant survival were similar (94.7%, 100%, and 100%). Likewise, aseptic loosening was not seen in our series.
Also, other authors have reported the outcome of the semi-constrained prosthesis for TKA [12, 13]. The majority of these studies, including ours, report the safety and effectiveness of semi-constrained prostheses in providing adequate coronal stability in patients with complex primary TKA.
5. Conclusion
Semi-constrained prosthesis provides a satisfying clinical and radiologic function for patients with complex primary TKA. They are associated with a small risk of postoperative complications, such as aseptic loosening, periprosthetic fracture, and implant failure. Therefore, the use of this prosthesis as a primary implant in patients with severe deformity or ligamentous laxity seems promising.
The present study had limitations. The main limitations of this study were its retrospective patient recruitment, the small number of patients, and the short follow-up period. Therefore, large-scale prospective studies are required to provide further support for the results presented here.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Total knee arthroplasty (TKA) is the choice of treatment for end-stage osteoarthritis [1]. Although most patients are satisfied with the results of TKA, almost one in five TKA patients are not satisfied for various reasons, such as unmet expectations or postoperative complications, such as instability and aseptic loosening [2]. Considering the growing number of TKA surgeries caused by the increased rate of obesity and aging in society [3], improving the outcomes of TKA and patients’ satisfaction is of critical importance.
Coronal stability is the cornerstone of a successful TKA [4], which is achieved with soft-tissue balancing and using unconstrained implants. However, in complex cases, such as patients with severe knee deformity, a more constrained implant is required to achieve adequate balance and coronal stability. Although constrained prosthesis provides better stability, it is associated with decreased survival and increased rate of complications, such as aseptic loosening [5, 6]. For this reason, a less constrained prosthesis (semi-constrained implant) was developed to reduce the detrimental impact of constrained implants on the patients’ outcomes [7]. However, the outcomes of TKA using semi-constrained implants are mainly unknown.
Objectives
This study was conducted to retrospectively evaluate the short-term outcomes and complications of primary TKA in a cohort of 23 patients with end-stage osteoarthritis who were managed with a semi-constrained implant.
2. Methods
This study was approved by the Ethics Committee of Iran University of Medical Sciences under the code IR.IUMS.REC.1400.1217. Between November 2018 and August 2020, medical profiles of the patients who underwent primary TKA with the use of a Stryker Triathlon posterior stabilized TKA (Kalamazoo, MI) with a total stabilized tibial polyethylene insert were reviewed. Patients with follow-up of less than 12 months and those who were lost to the follow-up were excluded from the study. Twenty-three patients (33 knees) were included in the final analysis. The study population included 6 men (26%) and 17 women (74%). The mean age of the patients was 70.7±7.6 years (range 66-74). The mean body mass index (BMI) of the patients was 35.1±4.4 kg/m2 (range 29.5-39.2). The mean follow-up of the patients was 12.5±2.8 months (range 12-14). Table 1 presents the characteristics of the patients.
Procedure
All procedures were performed by a senior knee surgeon. Using a medial parapatellar approach, a gap-balancing technique was implemented to achieve symmetric flexion and extension gaps. Gap balancing was started with the distal femur cut and continued with the proximal tibial cut. Then, the required extension gap was calculated, and medial/lateral released by pie crusting of the medial collateral ligament or lateral collateral ligament to achieve a symmetric extension gap. After that, the flexion gap was set to achieve the same value as the extension gap. A semi-constrained TKA was indicated if the knee was not adequately balanced with these procedures or the collateral ligaments were incompetent. Patellar resurfacing was not performed for any of the patients. All implants were cemented. Postoperatively, a knee brace was used for one week. Wait-bearing was allowed as tolerated.
Outcome measures
The outcome of the patients was evaluated radiographically and clinically. In each follow-up visit, standing lateral and anteroposterior radiographs, alignment view radiographs, and Merchant view radiographs were obtained. Postoperative tibiofemoral alignment was evaluated on recent radiographs.
Clinical evaluation of the knee function was performed prospectively using the knee society score (KSS) and Oxford knee score (OKS). The KSS ranged from 0 to 100, with a higher score demonstrating a better function. KSS was also categorized as follows, excellent (score ≥ 90), good (score 77-90), fair (score 65-77), and poor (score <65) [8].
The OKS ranged between 0 and 48, with higher scores indicating better outcomes. The subjective satisfaction of the patients and their re-choice to undergo the same operation were evaluated with yes/no questions. Clinical evaluations were performed two times, once after six months and the other one after one year.
3. Results
Radiographic outcomes
The mean knee extension was 8.7±7.9º (range 0–20°) before the surgery and 3.1±3º (range, 0–10°) after the surgery. The mean knee flexion was 100.8±17.2º (range 65–120°) before the surgery and 119.2±14.2º (range, 90–130°) after the operation. According to the preoperative standing radiographs, a varus deformity was present in 29 (87%) knees. The mean varus angle was 14.2±5.1º (range 9-21°). The preoperative valgus deformity was present in 4 knees (13%). The mean valgus angle was 6.1±2.1° (range 5-9°). The average postoperative tibiofemoral alignment was 0.26±1.1º of valgus (ranging from 3º valgus to 2º of varus) (Table 2).

Clinical outcomes
Six months after the operation, the mean KSS of the patients was 93.8±8.1 (excellent in 19 patients and good in four patients). After 12 months, the mean KSS of the patients was 94.7±8.3 (excellent in 20 patients and good in four patients).
The mean OKS of the patients 6 and 12 months after the operation were 43.6±3.7 and 44.1±3.8, respectively. At 12 months, all the patients were satisfied with the results of TKA. Twenty patients (87%) stated that they would select the same procedure if they were to go back in time and decide again. The remaining three (13%) patients were uncertain (Table 3).
Complications
Superficial or deep infection was not seen in any of the patients. No case of aseptic loosening was recorded until the last follow-up. Also, no hardware failure or periprosthetic fracture was recorded as well. In addition, deep vein thrombosis was not detected in any of the patients.
4. Discussion
In this study, we evaluated the short-term outcomes and postoperative complications of semi-constrained TKA. After 12 months, the knee function was excellent in 20 patients (87%) and good in 3 patients (13%). None of the patients had varus or valgus deformity, according to the tibiofemoral alignment view radiographs. Aseptic loosening did not occur in any of the patients. No other postoperative complications, such as periprosthetic fracture, hardware failure, and infection were observed.
In 2011, Lachiewicz and Soileau [9] first reported the outcomes of the second-generation constrained condylar prosthesis in primary TKA in 27 knees with a mean follow-up time of 5.4 years. The most common indications for the use of the second-generation constrained condylar prosthesis were severe valgus deformity and incompetent medial collateral ligament. None of the patients required a revision TKA during the follow-up period. Aseptic loosening, prosthetic fracture, tibial fracture, and patella problems were not observed in any of the patients. A minimally displaced patella fracture was observed in two knees, which was not asymptomatic. We considered the same indications for the use of a semi-constrained prosthesis. The mean follow-up of the patients was considerably shorter in our study. Similar to the study of Lachiewicz and Soileau, we observed no serious complications following the implication of a semi-constrained prosthesis.
The results of semi-constrained TKA have been reported in a small number of previous studies. Sabatini et al. [10] reported their experience using semi-constrained prostheses in primary TKA. Twenty-eight patients who underwent second-generation semi-constrained knee arthroplasty were included in their study. All patients were >75 years of age and had a severe deformity. The mean follow-up of the patients was 31.3 months. The mean KSS improved from 30 points before the operation to 92.1 points at the last follow-up. A full-extension knee was achieved in all patients. No radiolucent lines were observed during the radiographic evaluation. No deep infections or periprosthetic fractures were observed in any of the patients. Aseptic loosening was not seen in any of the patients as well. In our study, the mean KSS of patients was 94.7 at 12 months after the operation, which was comparable to the study of Sabatini et al. Similarly, no postoperative complications, such as aseptic loosening and periprosthetic fracture were observed in our cohort.
Martin et al. [7] aimed to investigate whether differences were observed in clinical and or radiographic outcomes for those who required a semi-constrained implant with a TS tibial insert and those who did not (primary TKA design with a posterior stabilized [PS] insert). Seventy-five patients were included in each group. The average follow-up of the study was 25 months. While the TS group had significantly greater preoperative varus, the two groups were similar in terms of postoperative revision, reoperation, and other complications. Aseptic loosening occurred in one patient in the TS group and no patient in the PS group. No aseptic loosening was observed in our series. However, it should be noted that our follow-up was shorter, and the number of patients was less (12.5 months, 23 patients).
Johnson et al. [11] evaluated functional outcomes and implant survival in a series of 23 TKA patients under the age of 60 years managed with semi-constrained prostheses. At a 66-month follow-up, Western Ontario and McMaster University Osteoarthritis Index scores and KSS were 15.7 and 94.7, respectively. The patient-reported outcomes were not different between one year and the final follow-up. Aseptic loosening was not seen in any of the patients. All patients kept the implants until the last follow-up with a satisfaction rate of 85.7%. Excellent or good results were reported by 92% of the patients. Although the follow-up period of our study was significantly smaller, the patient’s functional outcome (KSS), satisfaction rate, and implant survival were similar (94.7%, 100%, and 100%). Likewise, aseptic loosening was not seen in our series.
Also, other authors have reported the outcome of the semi-constrained prosthesis for TKA [12, 13]. The majority of these studies, including ours, report the safety and effectiveness of semi-constrained prostheses in providing adequate coronal stability in patients with complex primary TKA.
5. Conclusion
Semi-constrained prosthesis provides a satisfying clinical and radiologic function for patients with complex primary TKA. They are associated with a small risk of postoperative complications, such as aseptic loosening, periprosthetic fracture, and implant failure. Therefore, the use of this prosthesis as a primary implant in patients with severe deformity or ligamentous laxity seems promising.
The present study had limitations. The main limitations of this study were its retrospective patient recruitment, the small number of patients, and the short follow-up period. Therefore, large-scale prospective studies are required to provide further support for the results presented here.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Gao J, Xing D, Dong S, Lin J. The primary total knee arthroplasty: A global analysis. J Orthop Surg Res. 2020; 15(1):190. [DOI:10.1186/s13018-020-01707-5] [PMID] [PMCID]
- Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res. 2010; 468(1):57-63. [DOI:10.1007/s11999-009-1119-9] [PMID] [PMCID]
- Johnson CA, White CC, Kunkle BF, Eichinger JK, Friedman RJ. Effects of the Obesity Epidemic on Total Hip and Knee Arthroplasty Demographics. J Arthroplasty. 2021; 36(9):3097-100. [DOI:10.1016/j.arth.2021.04.017] [PMID]
- Cottino U, Sculco PK, Sierra RJ, Abdel MP. Instability after total knee arthroplasty. Orthop Clin North Am. 2016; 47(2):311-6. [DOI:10.1016/j.ocl.2015.09.007] [PMID]
- Cholewinski P, Putman S, Vasseur L, Migaud H, Duhamel A, Behal H, et al. Long-term outcomes of primary constrained condylar knee arthroplasty. Orthop Traumatol Surg Res. 2015; 101(4):449-54. [DOI:10.1016/j.otsr.2015.01.020] [PMID]
- Morgan H, Battista V, Leopold SS. Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg. 2005; 13(8):515-24. [DOI:10.5435/00124635-200512000-00004] [PMID]
- Martin JR, Fehring KA, Watts CD, Levy DL, Springer BD, Kim RH. Coronal alignment predicts the use of semi-constrained implants in contemporary total knee arthroplasty. Knee. 2017; 24(4):863-8. [DOI:10.1016/j.knee.2017.03.013] [PMID]
- Miralles-Muñoz FA, Gonzalez-Parreño S, Martinez-Mendez D, Gonzalez-Navarro B, Ruiz-Lozano M, Lizaur-Utrilla A, et al. A validated outcome categorization of the knee society score for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022; 30(4):1266-72. [DOI:10.1007/s00167-021-06563-2] [PMID]
- Lachiewicz PF, Soileau ES. Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty. 2011; 26(8):1228-31. [DOI:10.1016/j.arth.2011.05.010] [PMID]
- Sabatini L, Risitano S, Rissolio L, Bonani A, Atzori F, Massè A. Condylar constrained system in primary total knee replacement: Our experience and literature review. Ann Transl Med. 2017; 5(6):135. [DOI:10.21037/atm.2017.03.29] [PMID] [PMCID]
- Johnson DB Jr, Triplet JJ, Gaines DR, Gupta A, Unverferth KL. Mid-term outcomes following primary semi-constrained total knee arthroplasty in patients less than 60 years old, a retrospective review. Knee. 2019; 26(3):714-9. [DOI:10.1016/j.knee.2019.02.001] [PMID]
- Sumino T, Tomita T, Sugamoto K, Yamazaki T, Okazaki K. Semi-constrained posterior stabilized total knee arthroplasty reproduces natural deep knee bending kinematics. BMC Musculoskelet Disord. 2020; 21(1):107. [DOI:10.1186/s12891-020-3059-1] [PMID] [PMCID]
- Ye CY, Xue DT, Jiang S, He RX. Results of a second-generation constrained condylar prosthesis in complex primary and revision total knee arthroplasty: A mean 5.5-year follow-up. Chin Med J (Engl). 2016; 129(11):1334-9. [DOI:10.4103/0366-6999.182845] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Knee surgery
Received: 2022/08/2 | Accepted: 2023/06/6 | Published: 2022/05/1
Received: 2022/08/2 | Accepted: 2023/06/6 | Published: 2022/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









