Volume 9, Issue 2 (5-2022)
J. Res. Orthop. Sci. 2022, 9(2): 93-98 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Maleki A, Qoreishy M, Kazemi S M, Yahya G. Pediatric Tibial Shaft Fractures Remodeling After Casting. J. Res. Orthop. Sci. 2022; 9 (2) :93-98
URL: http://jros.iums.ac.ir/article-1-2204-en.html
URL: http://jros.iums.ac.ir/article-1-2204-en.html
1- Akhtar Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 599 kb]
(147 Downloads)
| Abstract (HTML) (691 Views)
Full-Text: (130 Views)
1. Introduction
Tibial shaft fracture is the most common long bone fracture in children, accounting for about 15% of all pediatric fractures. The usual age of onset is between 2 and 8 years old, and it is more common in boys [1, 2]. In 70% of the cases, these fractures are isolated and caused by a low-energy rotational deformity force [3]. Various treatment options exist for tibial shaft fracture, ranging from closed reduction and casting to open reduction and internal fixation. In older children, flexible intramedullary fixation is frequently used [4, 5] despite some severe consequences, including, compartment syndrome [6, 7], mal:union:, non:union:, and nail migration [8, 9]. The main advantage of casting is that, it is a non-invasive procedure, and because no internal device is being used, no wound exists and hence no chance of infection. Also, this procedure is cost economical. Disadvantages include a long period of immobilization that can last up to 12 weeks, during which it should be clinically and radiologically monitored [10]. Due to its thick periosteum and strong circulation, the vast majority of tibial fractures in children have an intense propensity to :union:. As a result of bone development, closed tibial shaft fractures in youngsters heal quickly [11]. Therefore, casting is an efficient treatment option for tibial shaft fractures [12]. Natural stressors, such as body weight, muscle function, reaction forces, and joint and inherent factors, such as the periosteum promote bone reconstruction in children [13]. Younger age and proximity of the fracture to the growth plate are factors connected to the high capacity of spontaneous repair of the fractured bone. In theory, the ideal remodeling conditions are flexion and varus, while recurvatum is the worst position [14, 15]. According to the points described above, this study was conducted to investigate the rate of remodeling in tibial shaft fractures casting, over six months.
2. Methods
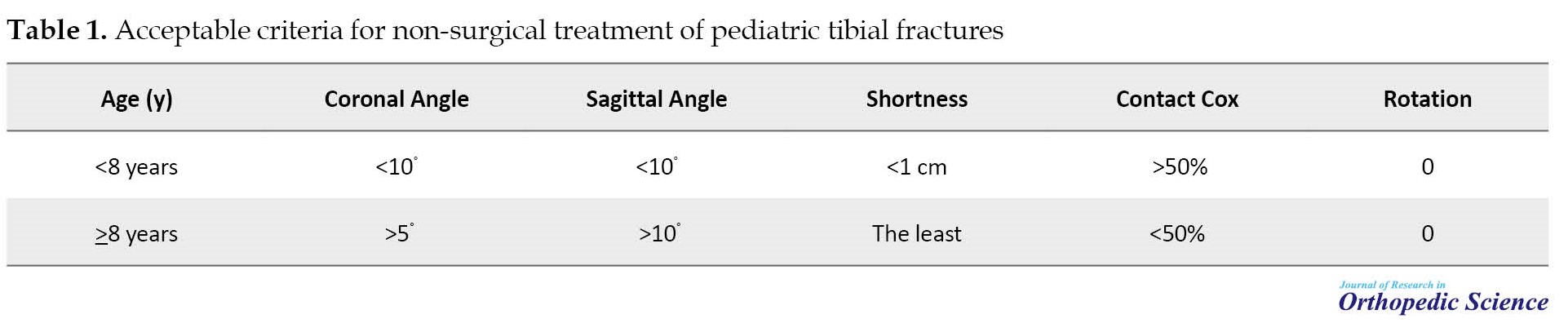
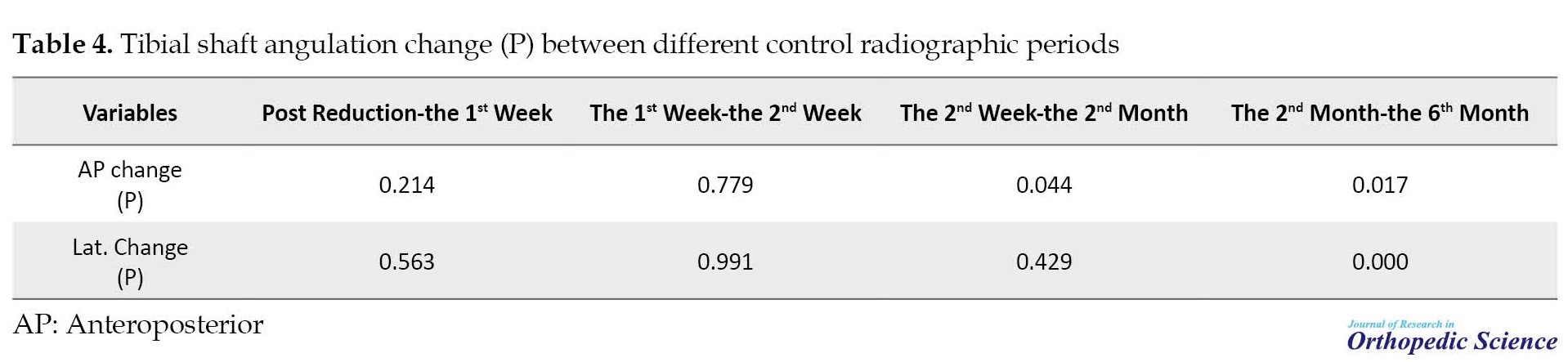
The Ethics Committee of Shahid Beheshti University of Medical Sciences approved this retrospective investigation. Between March 2017 and March 2018, our pediatric trauma center treated 74 children younger than 14 years old with tibial shaft fractures. Informed consent was obtained from all patients’ parents about the course of treatment, which allows the children to remain immobile for 3 months, and also the possible complications The exclusion criteria included open fracture, age over 14 years and obese children who have casting difficulties and are at risk for compartment syndrome [8], severe swelling with a high probability of compartment syndrome, segmental fracture, multiple-trauma patients, floating knee, fracture pattern that cannot be controlled with plaster, such as Varus greater than 10° with intact fibula [16], and irregular follow-up. Finally, 35 children were enrolled according to our criteria. After entering the emergency room, a physical examination was performed in terms of soft tissue health, nerve damage, and compartment syndrome. Routine radiographs of the tibia, including the anteroposterior (AP) and lateral views, as well as neighboring joints, such as the knee and ankle, were taken for all patients. Table 1 presents acceptable criteria for non-surgical therapy [10].
All patients were treated in the operating room under general anesthesia, with the knee bent between 20° and 40° and the ankle in 20° of plantar flexion to inhibit walking, relax the gastrocnemius muscle, and provide rotational stability [17]. Patient information, such as age and gender, was taken from the electronic data set Patients were placed in long-leg casts for 4-6 weeks before being transitioned to brief walking casts, if all parameters were completed and no evidence of :union: was found. The remodeling rate of the fracture site in the coronal and sagittal planes was examined using control radiographs taken in the first, second, and sixth months following the initial casting.
Patient data were expressed based on percentage and frequency. The chi-square test was used for qualitative variables and t-test and analysis of variance (ANOVA) were used for quantitative variables. Statistical software SPSS software, version 16.0 (SPSS Inc., Chicago, IL) was used, which has a statistically significant P<0.05.
3. Results
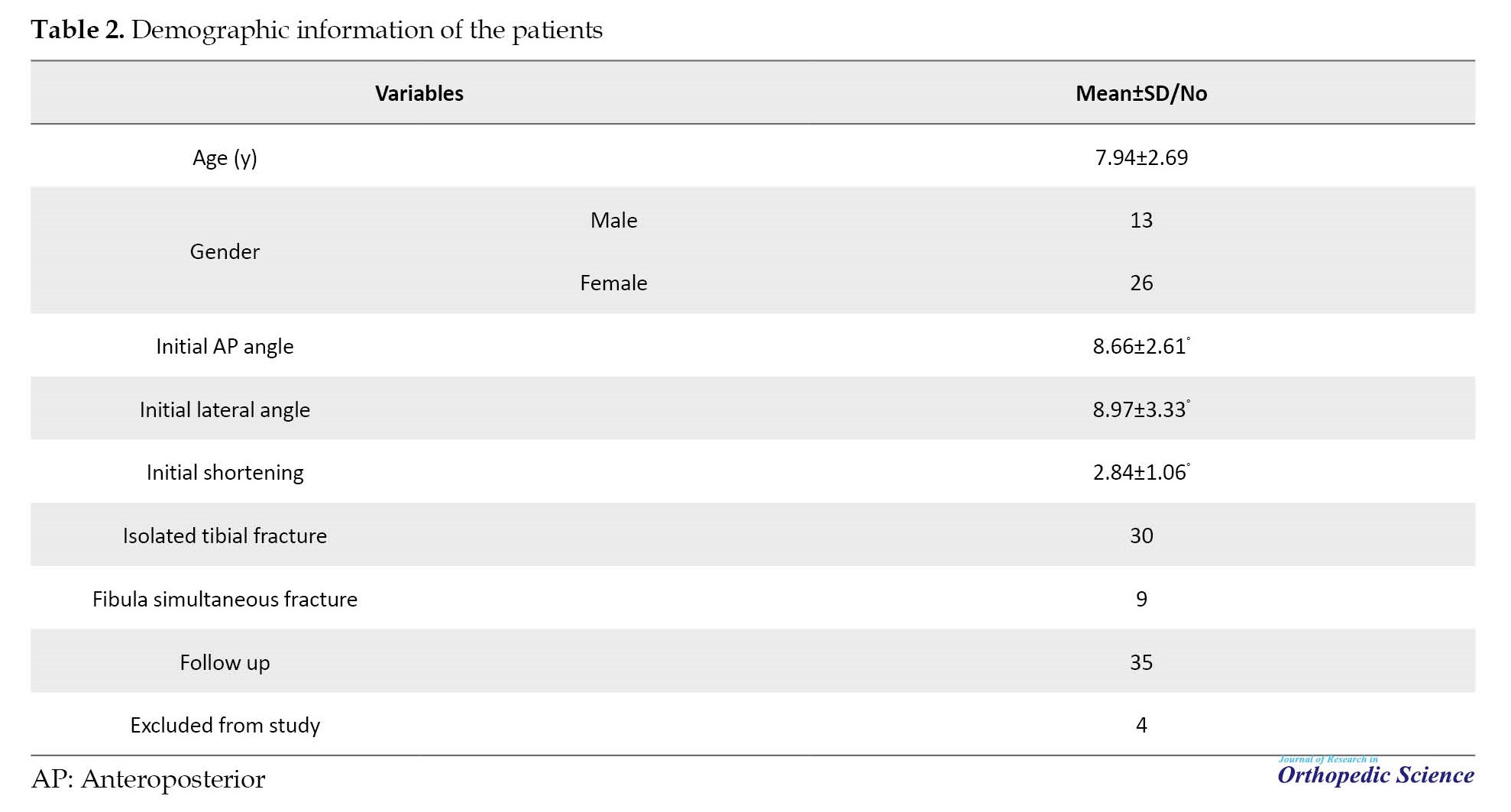
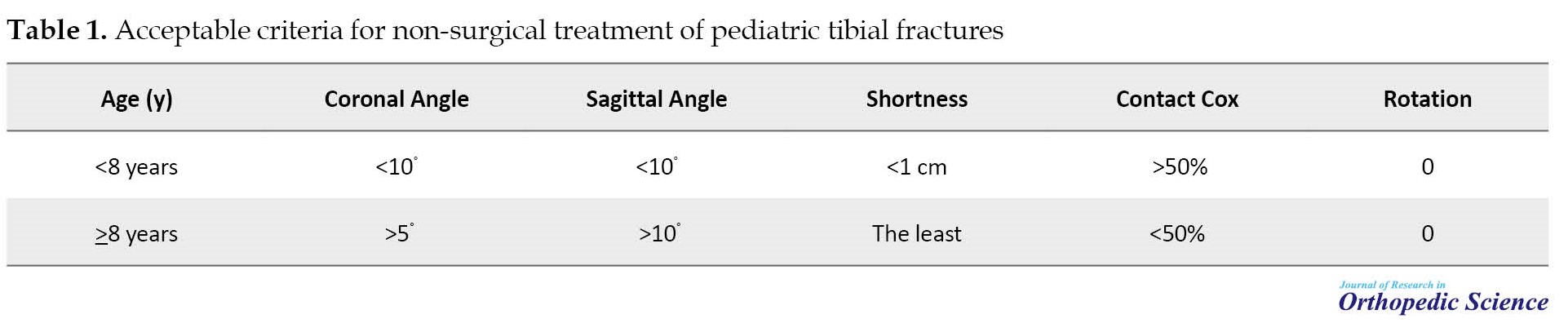
A total of 74 individuals with tibial fractures were admitted, of which 39 patients (52%) were treated with a long leg cast. The average age of these patients was 7.94±2.69 years, with a range of 2-14 years. In terms of gender distribution, 13 women and 26 men were included. Nine of 39 cases (23.1%). Initial radiographic results had 8.97±3.33° and 8.66±2.61° angulation on AP and lateral view and 2.84±1.06 mm shortening. After casting, angulation was decreased to 3.83±2.01° and 4.27±1.68° on AP and lateral, respectively. Four cases (one boy and three girls) were eliminated from the study because their tibial angular deformity was more than 10° control x-rays which was not acceptable, therefore they underwent a secondary closed reduction procedure and titanium elastic nail fixation, after one week. Thirty-five patients had acceptable eligibility and all of their fractures healed at the end of the sixth week (Table 2).
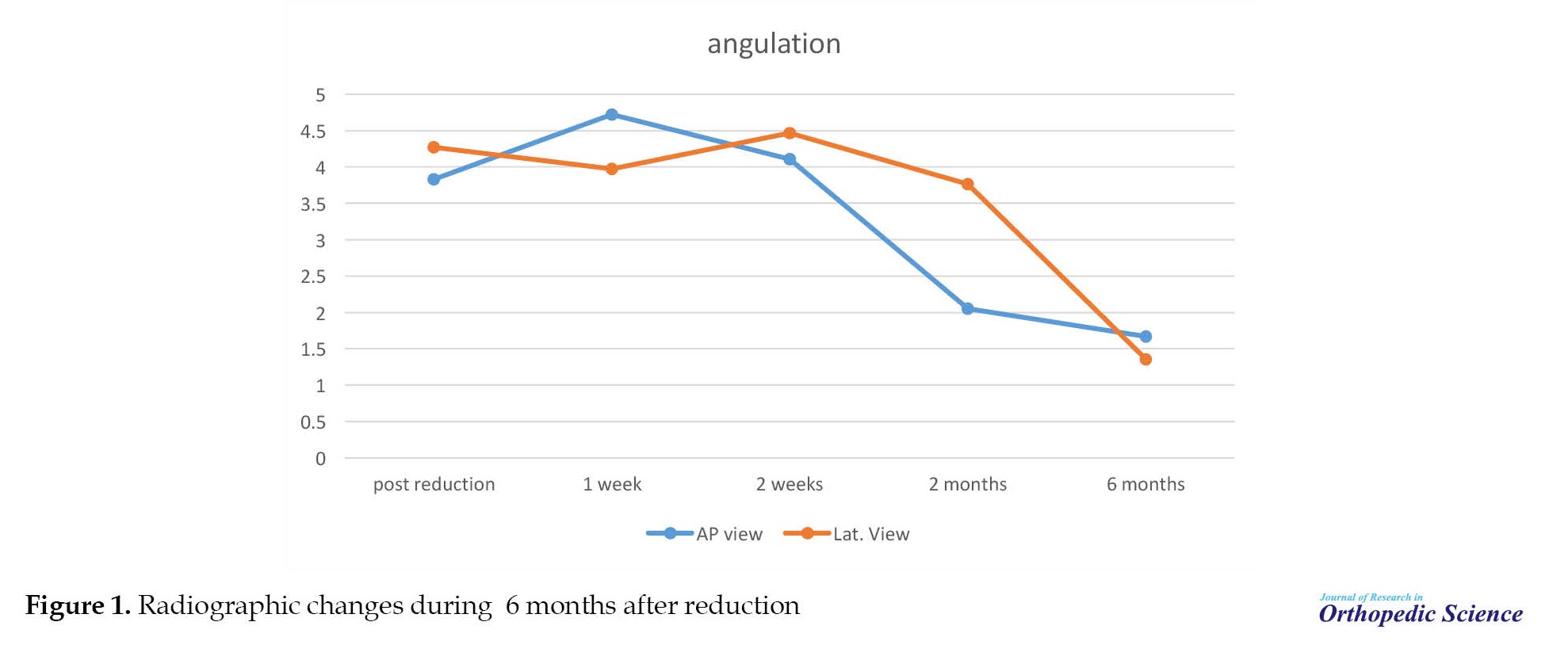
Radiographic changes in 6 months follow-up (Figure 1, Table 3) showed that tibial angulation increased in the first two weeks after reduction.
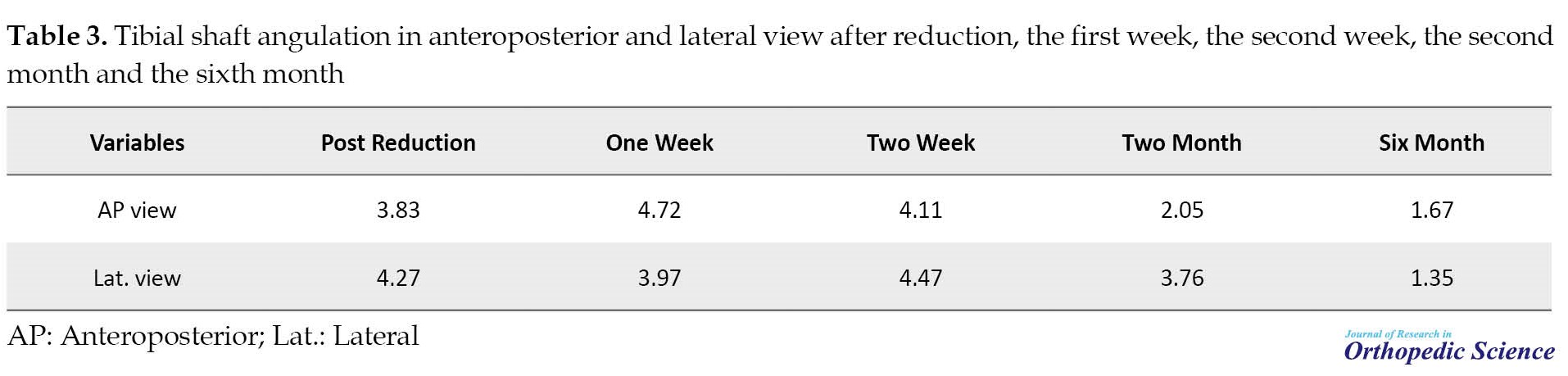
However, after the first two weeks, tibial angulation gradually decreased in the control radiographic, these changes showed that tibial bone remodeling was started after the fracture’s displacement occurring in the first 2 weeks after reduction. Also, it showed that the fracture alignment on AP view at the end of the second month was significantly changed compared to the radiographic results of the second week (P=0.044) (Table 4) but no significant correlation is observed with the initial x-ray in lateral view (P=0.429).
During the six-month follow-up period, the results demonstrated that remodeling in AP and lateral radiography is nearly complete and tibial angulation was decreased to 1.67±0.87° and 1.35±0.56°, respectively (P=0.017) (Figure 1).
4. Discussion
Although tibial shaft fracture is the most common long bone fracture in children, due to the existence of a thick periosteum and rich blood arteries that supply the bone and soft tissue, children’s bones exhibit a unique fracture pattern. Children have a greater ability to regenerate bone than adults; therefore, anatomical reduction is less necessary in young patients. This means that youngsters can smooth out and correct residual deformities [18]. The required degree of correction is determined by the child’s age, the position of the bone injury, its distance from the growth plate, and the presence of a bone injury in the adjacent joint [14, 15].
On the other hand, obtaining the best reduction in the early stages of treatment promotes the regeneration process. According to the tibial anatomy, overgrowth of the tibial bone is caused by stimulation of the proximal growth plate. Deformity of the tibial metaphyseal bone develops as a result of excessive development of the fibula during the tibial fracture [19]. According to the results, the remodeling process was satisfactory and statistically significant throughout the six-month follow-up. Related investigations also supported our results. According to Sarmiento’s [20] study on adult tibial shaft fractures treated by casting, 11% of patients had angulation in the coronal plane greater than 7°, 5% had angulation in the sagittal plane greater than 10°, and 1.4%had limb shortening greater than 2 cm. In addition according to a study conducted by Ho et al. [21] on 75 adolescents with tibial shaft fracture treated with long-leg casts, 4% of patients failed conservative treatment and needed surgery. According to the study of Gordon and O'Donnell [22] on the treatment of tibial fractures, non-surgical treatments (casting by Sarmiento technique) are an effective treatment for individuals without compartment syndrome, open wounds, or fractures of the shaft of the femur. In 2018, Stenroos et al. [23] discovered that treating patients with tibial shaft fracture, by long-leg casting (143 (47.3%) of 296) was the safest choice possible, and had the fewest complications. Goodwin 4 found that surgical therapy resulted in 10% of patients with a deformity of more than 10°, and Sankar 7 found that 12% of the malalignments were higher than 10° Swaan et al. [24] found that in 86 children (girls aged 1 to 8 years and boys aged 1 to 10 years) treated for tibial shaft fracture, some residual angular deformity spontaneously corrected. According to several studies, around 50% of the angular deformity is corrected in girls aged 9 to 12 years, and boys aged 11 to 12 years. Hansen et al. [25] observed that out of the 102 tibia fractures, 25 patients experienced mal:union: ranging from 4° to 19°. This ranged from 3° to 19° in pursuit of this feature. Steinert et al. [26] demonstrated that 26 of 28 infants had varus or valgus deformity in the coronal plane after the :union:, indicating a considerable residual deformity. Our study detected that angular deformity may increase one week after primary reduction, but the angular deformities were gradually corrected over 6 months.
Limitations and challenges
1. The number of study samples is limited.
2. Gender may affect remodeling; therefore, further research on gender segregation is advised.
3. In the current study, tibial fractures were not classified (transverse, spiral, short oblique, long oblique, comminuted) and the relationship between the type of fractures and results were not assessed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (Code:IR.SBMU.RETECH.REC.1399.1265).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design: Arash Maleki and Seyyed Morteza Kazemi; Manuscript preparation: Arash Maleki and Mohammad Qoreishy; Performing measurement: Ghulam Yahya; Statistical analysis: Arash Maleki.
Conflict of interest
The authors declared no conflict of interest.
References
Tibial shaft fracture is the most common long bone fracture in children, accounting for about 15% of all pediatric fractures. The usual age of onset is between 2 and 8 years old, and it is more common in boys [1, 2]. In 70% of the cases, these fractures are isolated and caused by a low-energy rotational deformity force [3]. Various treatment options exist for tibial shaft fracture, ranging from closed reduction and casting to open reduction and internal fixation. In older children, flexible intramedullary fixation is frequently used [4, 5] despite some severe consequences, including, compartment syndrome [6, 7], mal:union:, non:union:, and nail migration [8, 9]. The main advantage of casting is that, it is a non-invasive procedure, and because no internal device is being used, no wound exists and hence no chance of infection. Also, this procedure is cost economical. Disadvantages include a long period of immobilization that can last up to 12 weeks, during which it should be clinically and radiologically monitored [10]. Due to its thick periosteum and strong circulation, the vast majority of tibial fractures in children have an intense propensity to :union:. As a result of bone development, closed tibial shaft fractures in youngsters heal quickly [11]. Therefore, casting is an efficient treatment option for tibial shaft fractures [12]. Natural stressors, such as body weight, muscle function, reaction forces, and joint and inherent factors, such as the periosteum promote bone reconstruction in children [13]. Younger age and proximity of the fracture to the growth plate are factors connected to the high capacity of spontaneous repair of the fractured bone. In theory, the ideal remodeling conditions are flexion and varus, while recurvatum is the worst position [14, 15]. According to the points described above, this study was conducted to investigate the rate of remodeling in tibial shaft fractures casting, over six months.
2. Methods
The Ethics Committee of Shahid Beheshti University of Medical Sciences approved this retrospective investigation. Between March 2017 and March 2018, our pediatric trauma center treated 74 children younger than 14 years old with tibial shaft fractures. Informed consent was obtained from all patients’ parents about the course of treatment, which allows the children to remain immobile for 3 months, and also the possible complications The exclusion criteria included open fracture, age over 14 years and obese children who have casting difficulties and are at risk for compartment syndrome [8], severe swelling with a high probability of compartment syndrome, segmental fracture, multiple-trauma patients, floating knee, fracture pattern that cannot be controlled with plaster, such as Varus greater than 10° with intact fibula [16], and irregular follow-up. Finally, 35 children were enrolled according to our criteria. After entering the emergency room, a physical examination was performed in terms of soft tissue health, nerve damage, and compartment syndrome. Routine radiographs of the tibia, including the anteroposterior (AP) and lateral views, as well as neighboring joints, such as the knee and ankle, were taken for all patients. Table 1 presents acceptable criteria for non-surgical therapy [10].
All patients were treated in the operating room under general anesthesia, with the knee bent between 20° and 40° and the ankle in 20° of plantar flexion to inhibit walking, relax the gastrocnemius muscle, and provide rotational stability [17]. Patient information, such as age and gender, was taken from the electronic data set Patients were placed in long-leg casts for 4-6 weeks before being transitioned to brief walking casts, if all parameters were completed and no evidence of :union: was found. The remodeling rate of the fracture site in the coronal and sagittal planes was examined using control radiographs taken in the first, second, and sixth months following the initial casting.
Patient data were expressed based on percentage and frequency. The chi-square test was used for qualitative variables and t-test and analysis of variance (ANOVA) were used for quantitative variables. Statistical software SPSS software, version 16.0 (SPSS Inc., Chicago, IL) was used, which has a statistically significant P<0.05.
3. Results
A total of 74 individuals with tibial fractures were admitted, of which 39 patients (52%) were treated with a long leg cast. The average age of these patients was 7.94±2.69 years, with a range of 2-14 years. In terms of gender distribution, 13 women and 26 men were included. Nine of 39 cases (23.1%). Initial radiographic results had 8.97±3.33° and 8.66±2.61° angulation on AP and lateral view and 2.84±1.06 mm shortening. After casting, angulation was decreased to 3.83±2.01° and 4.27±1.68° on AP and lateral, respectively. Four cases (one boy and three girls) were eliminated from the study because their tibial angular deformity was more than 10° control x-rays which was not acceptable, therefore they underwent a secondary closed reduction procedure and titanium elastic nail fixation, after one week. Thirty-five patients had acceptable eligibility and all of their fractures healed at the end of the sixth week (Table 2).
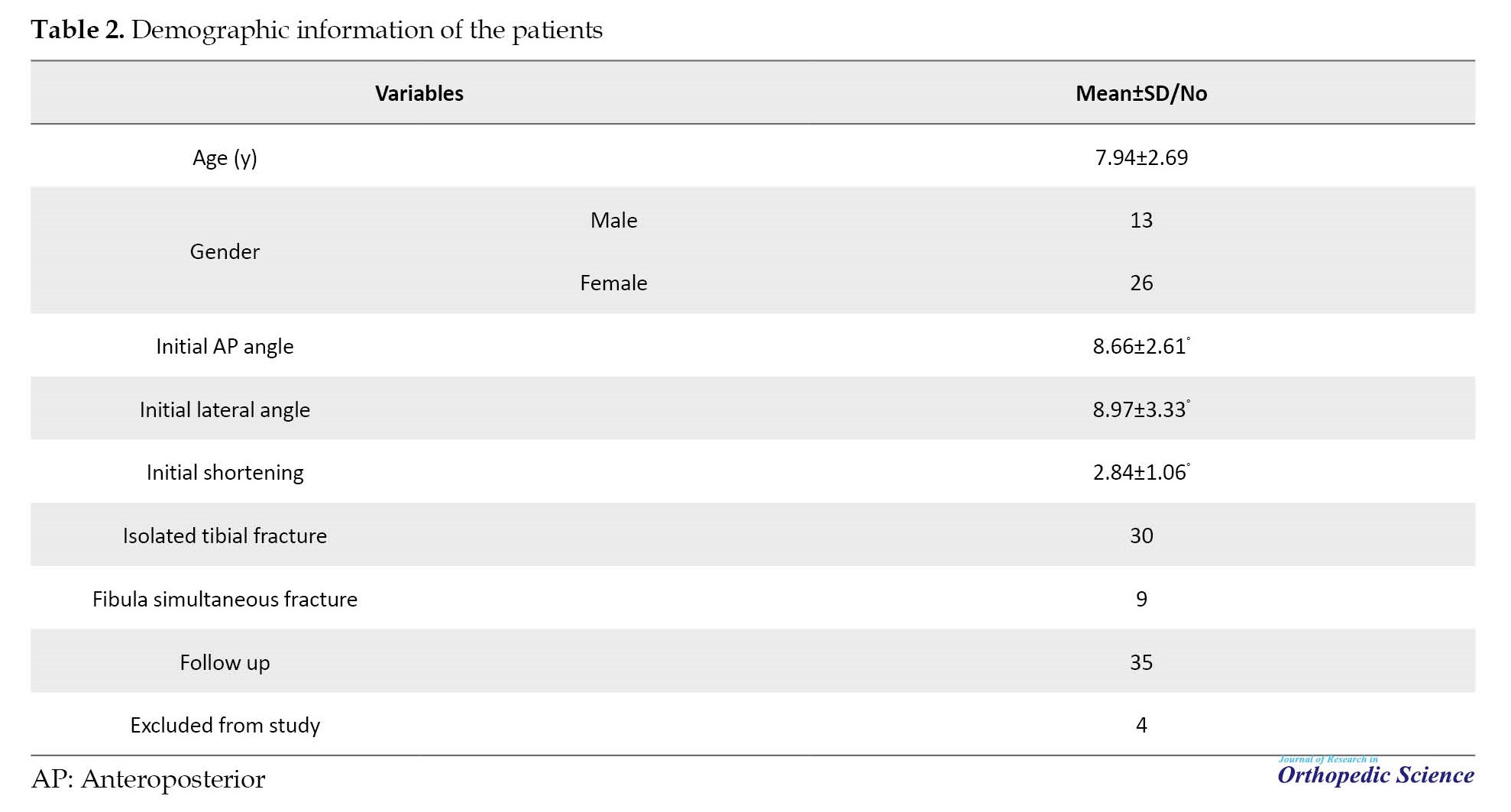
Radiographic changes in 6 months follow-up (Figure 1, Table 3) showed that tibial angulation increased in the first two weeks after reduction.
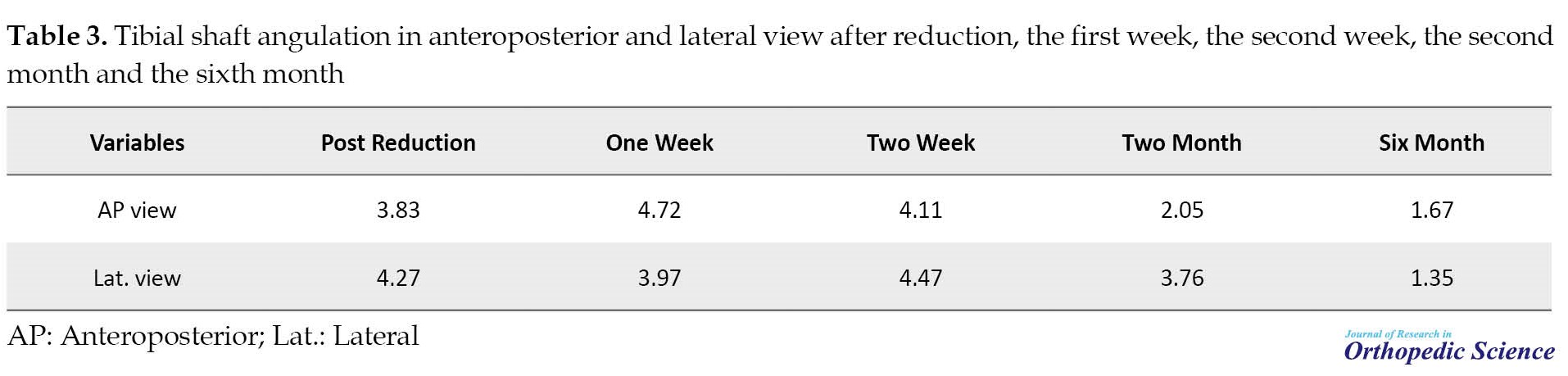
However, after the first two weeks, tibial angulation gradually decreased in the control radiographic, these changes showed that tibial bone remodeling was started after the fracture’s displacement occurring in the first 2 weeks after reduction. Also, it showed that the fracture alignment on AP view at the end of the second month was significantly changed compared to the radiographic results of the second week (P=0.044) (Table 4) but no significant correlation is observed with the initial x-ray in lateral view (P=0.429).
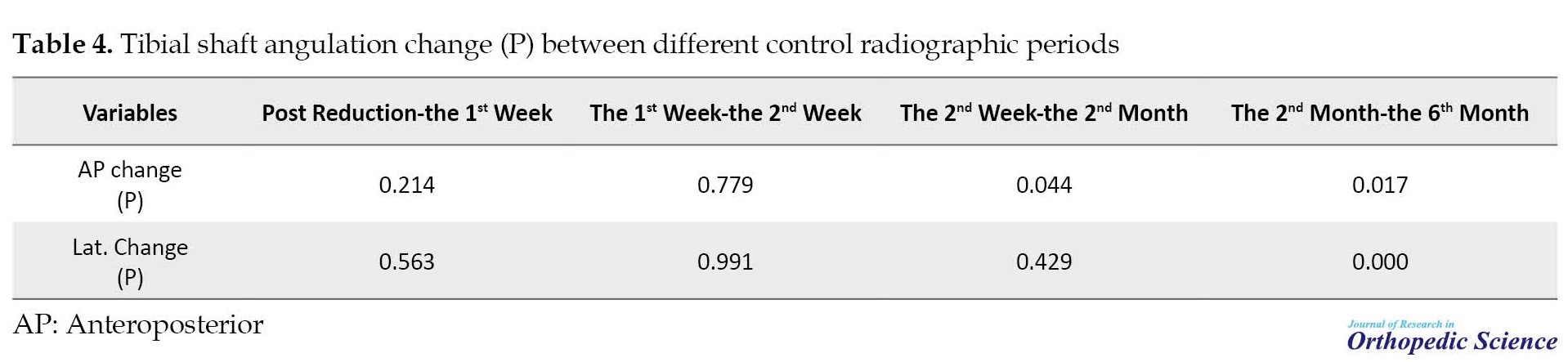
During the six-month follow-up period, the results demonstrated that remodeling in AP and lateral radiography is nearly complete and tibial angulation was decreased to 1.67±0.87° and 1.35±0.56°, respectively (P=0.017) (Figure 1).
4. Discussion
Although tibial shaft fracture is the most common long bone fracture in children, due to the existence of a thick periosteum and rich blood arteries that supply the bone and soft tissue, children’s bones exhibit a unique fracture pattern. Children have a greater ability to regenerate bone than adults; therefore, anatomical reduction is less necessary in young patients. This means that youngsters can smooth out and correct residual deformities [18]. The required degree of correction is determined by the child’s age, the position of the bone injury, its distance from the growth plate, and the presence of a bone injury in the adjacent joint [14, 15].
On the other hand, obtaining the best reduction in the early stages of treatment promotes the regeneration process. According to the tibial anatomy, overgrowth of the tibial bone is caused by stimulation of the proximal growth plate. Deformity of the tibial metaphyseal bone develops as a result of excessive development of the fibula during the tibial fracture [19]. According to the results, the remodeling process was satisfactory and statistically significant throughout the six-month follow-up. Related investigations also supported our results. According to Sarmiento’s [20] study on adult tibial shaft fractures treated by casting, 11% of patients had angulation in the coronal plane greater than 7°, 5% had angulation in the sagittal plane greater than 10°, and 1.4%had limb shortening greater than 2 cm. In addition according to a study conducted by Ho et al. [21] on 75 adolescents with tibial shaft fracture treated with long-leg casts, 4% of patients failed conservative treatment and needed surgery. According to the study of Gordon and O'Donnell [22] on the treatment of tibial fractures, non-surgical treatments (casting by Sarmiento technique) are an effective treatment for individuals without compartment syndrome, open wounds, or fractures of the shaft of the femur. In 2018, Stenroos et al. [23] discovered that treating patients with tibial shaft fracture, by long-leg casting (143 (47.3%) of 296) was the safest choice possible, and had the fewest complications. Goodwin 4 found that surgical therapy resulted in 10% of patients with a deformity of more than 10°, and Sankar 7 found that 12% of the malalignments were higher than 10° Swaan et al. [24] found that in 86 children (girls aged 1 to 8 years and boys aged 1 to 10 years) treated for tibial shaft fracture, some residual angular deformity spontaneously corrected. According to several studies, around 50% of the angular deformity is corrected in girls aged 9 to 12 years, and boys aged 11 to 12 years. Hansen et al. [25] observed that out of the 102 tibia fractures, 25 patients experienced mal:union: ranging from 4° to 19°. This ranged from 3° to 19° in pursuit of this feature. Steinert et al. [26] demonstrated that 26 of 28 infants had varus or valgus deformity in the coronal plane after the :union:, indicating a considerable residual deformity. Our study detected that angular deformity may increase one week after primary reduction, but the angular deformities were gradually corrected over 6 months.
Limitations and challenges
1. The number of study samples is limited.
2. Gender may affect remodeling; therefore, further research on gender segregation is advised.
3. In the current study, tibial fractures were not classified (transverse, spiral, short oblique, long oblique, comminuted) and the relationship between the type of fractures and results were not assessed.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (Code:IR.SBMU.RETECH.REC.1399.1265).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Study design: Arash Maleki and Seyyed Morteza Kazemi; Manuscript preparation: Arash Maleki and Mohammad Qoreishy; Performing measurement: Ghulam Yahya; Statistical analysis: Arash Maleki.
Conflict of interest
The authors declared no conflict of interest.
References
- Lieber J, Schmittenbecher P. Developments in the treatment of pediatric long bone shaft fractures. Eur J Pediatr Surg. 2013; 23(6):427-33. [DOI:10.1055/s-0033-1360460] [PMID]
- Mann DC, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0-16 years.J Pediatr Orthop. 1990; 10(6):713-6.[DOI:10.1097/01241398-199011000-00002] [PMID]
- Mooney J, Hennrikus W. Fractures of the shaft of the tibia and fibula. In: Flynn JM, Skaggs DL, Waters PM, editors. Rockwood and Wilkins fractures in children. Philadelphia: Wolters Kluwer Health; 2014.
- Goodwin RC, Gaynor T, Mahar A, Oka R, Lalonde FD. Intramedullary flexible nail fixation of unstable pediatric tibial diaphyseal fractures. J Pediatr Orthop. 2005; 25(5):570-6. [DOI:10.1097/01.mph.0000165135.38120.ce] [PMID]
- Griffet J, Leroux J, Boudjouraf N, Abou-Daher A, El Hayek T. Elastic stable intramedullary nailing of tibial shaft fractures in children. J Child Orthop. 2011; 5(4):297-304. [DOI:10.1007/s11832-011-0343-5] [PMID] [PMCID]
- O'Brien T, Weisman DS, Ronchetti P, Piller CP, Maloney M. Flexible titanium nailing fo r the treatment of the unstable pediatric tibial fracture. J Pediatr Orthop. 2004; 24(6):601-9. [DOI:10.1097/01241398-200411000-00001] [PMID]
- Goodbody CM, Lee J, Flynn JM, Sankar WN. Titianium elastic nailing for pediatric tibia fractures: Do older, heavier kids do worse? J Pediatr Orthop. 2016; 36(5):472-7. [DOI:10.1097/BPO.0000000000000483] [PMID]
- Pandya NK, Edmonds EW, Mubarak SJ. The incidence of compartment syndrome after flexible nailing of pediatric tibial shaft fractures. J Child Orthop. 2011; 5(6):439-47. [DOI:10.1007/s11832-011-0374-y] [PMID] [PMCID]
- Gordon JE, Gregush RV, Schoenecker PL, Dobbs MB, Luhmann SJ. Complications after titanium elastic nailing of pediatric tibial fractures. J Pediatr Orthop. 2007; 27(4):442-6. [DOI:10.1097/01.bpb.0000271333.66019.5c] [PMID]
- Ho CA. Tibia Shaft fractures in adolescents: How and when can they be managedsuccessfully with cast treatment? J Pediatr Orthop. 2016; 36(Suppl 1):S15-8. [DOI:10.1097/BPO.0000000000000762] [PMID]
- Hoaglund FT, States JD. Factors influencing the rate of healing in tibial shaft fractures. Surg Gynecol Obstet. 1967; 124(1):71-6. [PMID]
- Heinrich SD, Mooney JF. Fractures of the shaft of the tibia and fibula. In: Wilkins KE, Beaty JH, editors. Rockwood and Wilkin‘ s fractures in children. Riverwoods: Lippincott Williams & Wilkins; 2006.
- Vittas D, Larsen E, Torp-Pedersen S. Angular remodeling of midshaft forearm fractures in children. Clin Orthop Relat Res. 1991; 265:261-4. [DOI:10.1097/00003086-199104000-00030]
- Dwyer AJ, John B, Krishen M, Hora R. Remodeling of tibial fractures in children younger than 12 years. Orthopedics. 2007; 30(5):393-6. [DOI:10.3928/01477447-20070501-13] [PMID]
- Jung ST, Park H, Lee JH, Kim JR. Residual angulation of distal tibial diaphyseal fractures in children younger than ten years. J Orthop Surg Res. 2014; 9:84. [DOI:10.1186/s13018-014-0084-5] [PMID] [PMCID]
- Sarmiento A, Sharpe FE, Ebramzadeh E, Normand P, Shankwiler J. Factors influencing the outcome of closed tibial fractures treated with functional bracing. Clin Orthop Relat Res. 1995; 315:8-24. [DOI:10.1097/00003086-199506000-00003]
- Herman MJ, Martinek MA, Abzug JM. Complications of tibial eminence and diaphyseal fractures in children: Prevention and treatment. J Am Acad Orthop Surg. 2014; 22(11):730-41. [DOI:10.5435/JAAOS-22-11-730] [PMID]
- Hadizie D, Munajat I. Both-Bone forearm fractures in children with minimum four years of growth remaining: Can cast achieve a good outcome at skeletal maturity?Malays Orthop J. 2017; 11(3):1-9. [DOI:10.5704/MOJ.1711.009] [PMID] [PMCID]
- Cozen L. Fracture of the proximal portion of the tibia in children followed by valgus deformity. Surg Gynecol Obstet. 1953; 97(2):183-8. [PMID]
- Sarmiento A. On the behavior of closed tibial fractures: Clinical / radiological correlations. J Orthop Trauma. 2000; 14(3):199-205. [DOI:10.1097/00005131-200003000-00010] [PMID]
- Ho CA, Dammann G, Podeszwa DA, Levy J. Tibial shaft fractures in adolescents: Analysis of cast treatment successes and failures. J Pediatr Orthop B. 2015; 24(2):114-7 [DOI:10.1097/BPB.0000000000000144] [PMID]
- Gordon JE, O’Donnell JC. Tibia fractures: What should be fixed? J Pediatr Orthop. 2012; 32(Suppl 1):S52-61. [DOI:10.1097/BPO.0b013e318254c7be] [PMID]
- Stenroos A, Laaksonen T, Nietosvaara N, Jalkanen J, Nietosvaara Y. One in three of pediatric tibia shaft fractures is currently treated operatively: A 6-year epidemiological study in two university hospitals in Finland Treatment of Pediatric Tibia Shaft Fractures. Scand J Surg. 2018; 107(3):269-74. [DOI:10.1177/1457496917748227] [PMID]
- Swaan JW, Oppers VM. Crural fractures in children. A study of the incidence of changes of the axial position and of enhanced longitudinal growth of the tibia after healing of crural fractures. Arch Chir Neerl. 1971; 23(4):259-72. [PMID]
- Hansen BA, Greiff J, Bergmann F. Fractures of the tibia in children. Acta Orthop Scand. 1976; 47(4):448-53 [DOI:10.3109/17453677608988718] [PMID]
- Steinert V, Bennek J. [Tibial fractures in children (German)]. Zentralbl Chir. 1966; 91(38):1387-92. [PMID]
Type of Study: Research Article |
Subject:
Pediatrics
Received: 2022/09/1 | Accepted: 2023/08/26 | Published: 2022/05/1
Received: 2022/09/1 | Accepted: 2023/08/26 | Published: 2022/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |