Volume 9, Issue 4 (11-2022)
JROS 2022, 9(4): 197-200 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tahririan M A, Akbari Aghdam H, Salehi S A, Shahsavan M, Jalili A, Jokar F. Early Versus Delayed Surgery Outcomes of Intertrochanteric Fractures. JROS 2022; 9 (4) :197-200
URL: http://jros.iums.ac.ir/article-1-2208-en.html
URL: http://jros.iums.ac.ir/article-1-2208-en.html
Mohammad Ali Tahririan1 

 , Hossein Akbari Aghdam1
, Hossein Akbari Aghdam1 

 , Seyed Ashkan Salehi1
, Seyed Ashkan Salehi1 

 , Mohammad Shahsavan1
, Mohammad Shahsavan1 

 , Ashkan Jalili1
, Ashkan Jalili1 

 , Farnaz Jokar2
, Farnaz Jokar2 




 , Hossein Akbari Aghdam1
, Hossein Akbari Aghdam1 

 , Seyed Ashkan Salehi1
, Seyed Ashkan Salehi1 

 , Mohammad Shahsavan1
, Mohammad Shahsavan1 

 , Ashkan Jalili1
, Ashkan Jalili1 

 , Farnaz Jokar2
, Farnaz Jokar2 


1- Department of Orthopedic Surgery, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Physical Therapy, School of Rehabilitation, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Physical Therapy, School of Rehabilitation, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 427 kb]
(313 Downloads)
| Abstract (HTML) (996 Views)
Full-Text: (374 Views)
1. Introduction
Intertrochanteric fracture is common among the elderly, especially those with osteoporosis [1-5]. While the mortality rate related to intertrochanteric fracture has reduced due to medical care advancements in recent years [6], this kind of fracture still accompanies a considerable mortality rate among the elderly. Early mortality (within one month) among these patients has been reported to range between 10%-30% in various studies [7-12].
Several factors contribute to the mortality of patients with intertrochanteric fractures, including advancing age, delays in operative treatment, underlying diseases, duration of surgery, and anesthesia methods [13]. Additionally, studies have mentioned the influence of surgeons’ experience, hospital patient load [14], and obesity [5] on mortality rates.
Due to the uncertainty of mortality causes and lack of comprehensive studies on this subject, this study was conducted to compare the short and long-term mortality rates and the hospitalization duration in intertrochanteric fracture patients receiving early and delayed surgical treatment.
2. Methods
The utilized data from patients with femoral intertrochanteric fractures who were referred to Ayatollah Kashani Hospital, Isfahan City, Iran from 2018 to 2020.
The inclusion criteria included patients with intertrochanteric fractures who underwent surgery between 2018 and 2020 and had adequate information available in their medical records or accessible through family members.
We collected demographic data, underlying diseases, duration from admission to surgery, surgery duration, and length of hospital stay after surgery from the related documents. Patients were categorized into two groups based on surgical delay, those with delay (surgery initiated more than 48 hours after hospital admission), and those without delay.
Patients’ mortality status, post-surgery complications, and the period after surgery to their death were obtained through phone calls. Patients’ death was classified into short-term (within one month after surgery), and long-term (within one year after surgery).
Data were analyzed using SPSS software, version 26 with the chi-square test and t-test.
3. Results
A total of 308 patients with intertrochanteric fractures with a mean age of 62.35±10.15 years were selected. Among them, 230 patients (74.7%) were men and 78 patients (25.3%) were women. Also, 8.4% of them had underlying diseases. The mean duration of surgery was 1.23±0.57 hours, and the mean length of hospital stay was 13.99±3.27 days. Delayed surgery was observed in 47 patients (15.3%), and 261(84.7%) underwent surgery without delay. Furthermore, 7 patients (2.3%) died within one month post-surgery, and 13 patients (4.2%) died within one year after surgery.
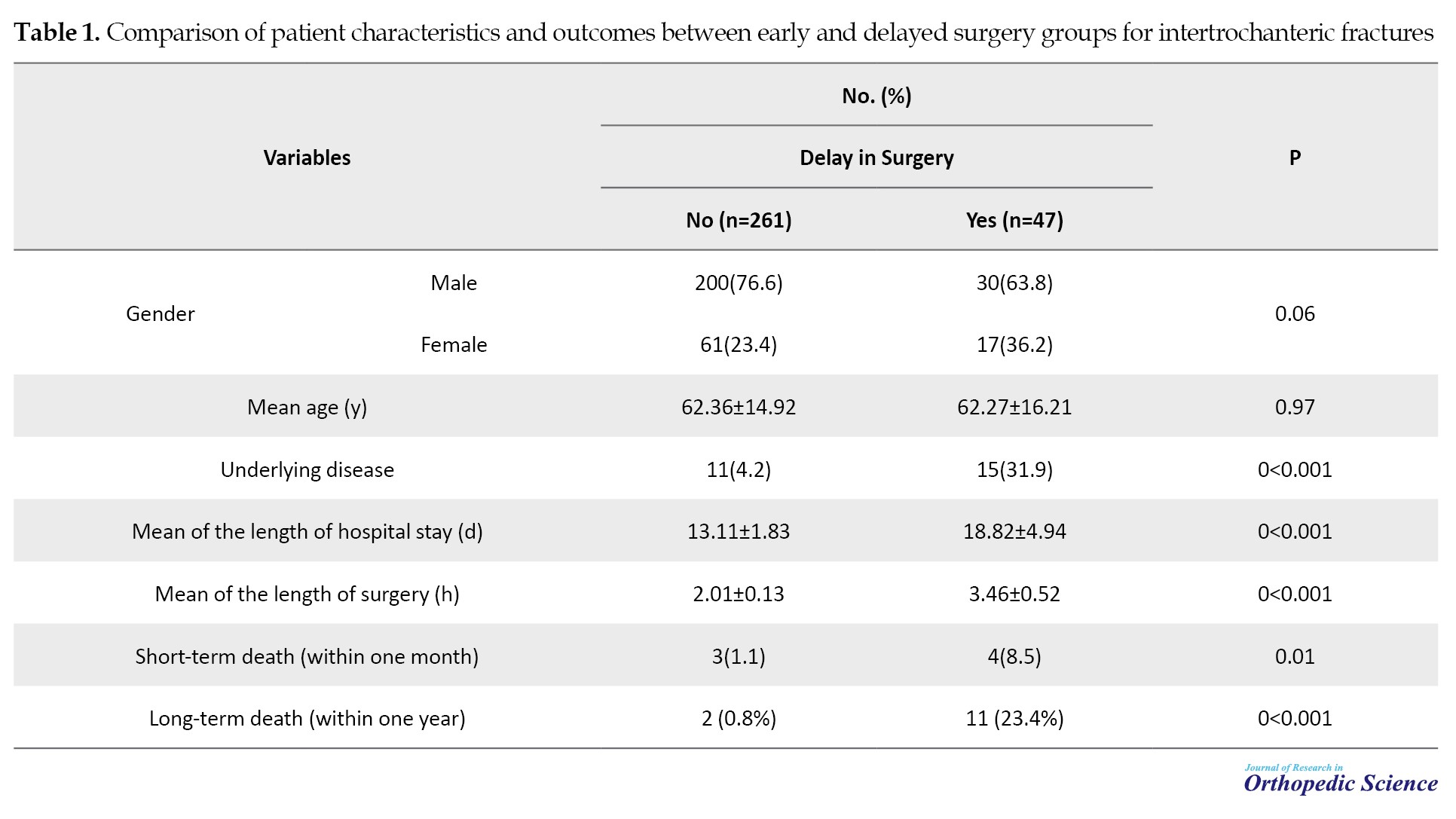
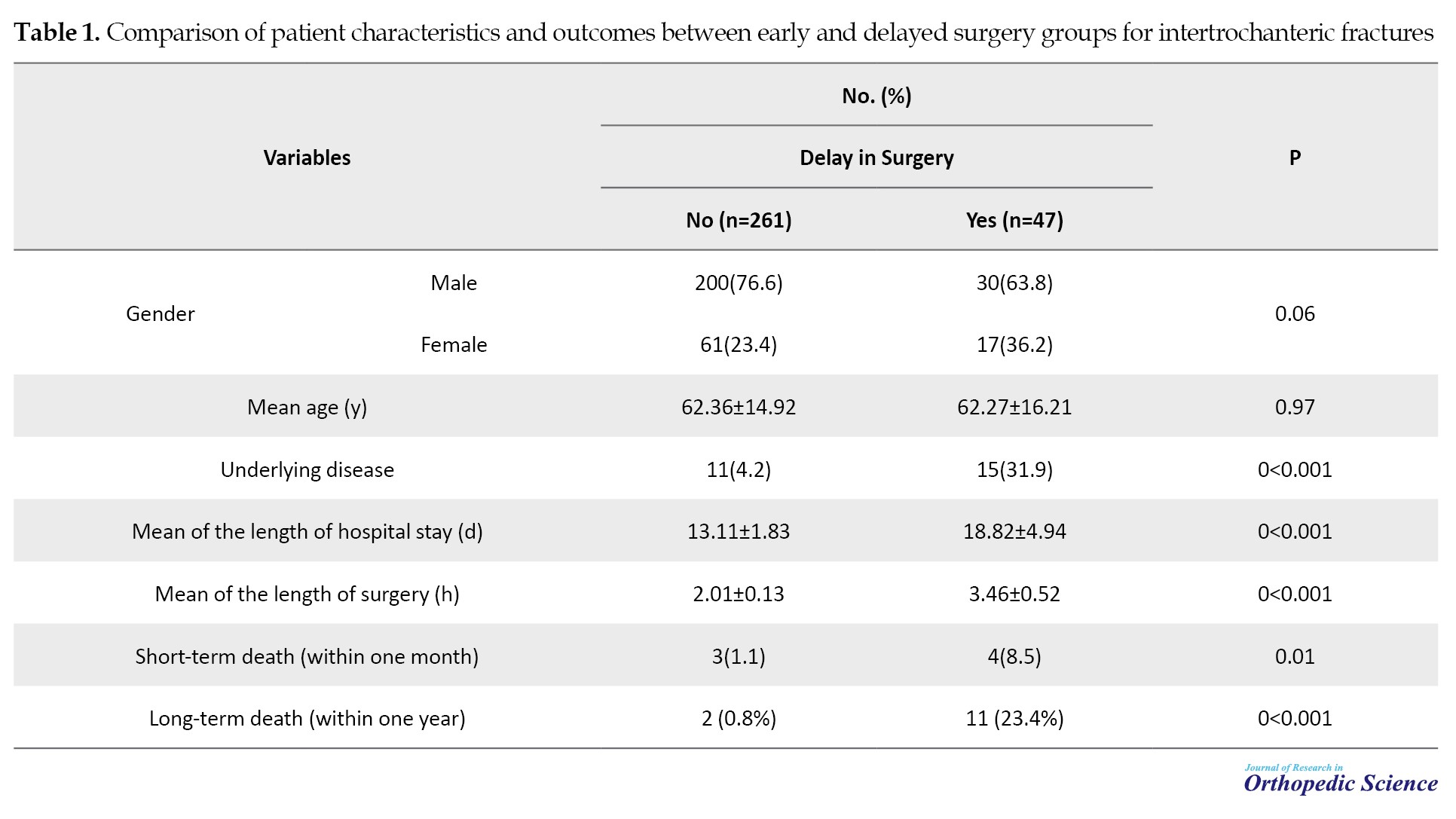
The subjects in the two groups had no significant difference in their age and gender, but the existence of underlying disease was significantly higher in the group with delayed surgery (P<0.001). Moreover, the mean length of hospital stay (P<0.001), duration of surgery (P<0.001), short-term mortality (P=0.01), and long-term mortality (P<0.001) were significantly higher in the delayed surgery group (Table 1).
4. Discussion
While delaying surgery for a femoral intertrochanteric fracture may allow for more comprehensive patient evaluation and medical optimization, it also introduces various complications, such as bed sore, thromboembolism, infection, delayed rehabilitation, prolonged hospital stay, and increased mortality rates.
In our study, we observed higher short and long-term mortality rates among patients with delayed surgery. There is controversy in recent studies concerning the correlation between delayed surgery and mortality rates. Leung et al. reviewed 42 studies and found that early surgery was associated with lower side effects, mortality rates, bed sores, and hospitalization duration. However, evidence of short and long-term mortality was diverse [15]. This is probably due to the small sample size, diverse definitions of delayed surgery, and failure to evaluate the cause of the surgery [16]. Daugaard et al. investigated 38,020 patients from 2003 to 2010 and reported that delayed surgery after acute pelvic fracture accompanies with a considerable increase in short-term mortality (odds ratio (OR)=1.3 in 24-hour delay) [16]. Similarly, Poór et al. found that increased comorbidity significantly increased mortality in patients with hip fractures, highlighting the critical nature of timely surgery [17]. Rosso et al. concluded that surgical treatment for pelvic fractures should be performed within 48 hours [18].
In our study, gender and age were not related to delayed surgery, but patients with underlying diseases were more likely to experience delayed surgeries, with longer surgical durations and hospitalizations observed in this group.
A study by Cha et al., similar to ours, found a correlation between delay in surgery and mortality rate in patients with intertrochanteric fracture [19]. While investigating factors contributing to surgical delays, they did not explore the impact of surgery duration on delays or the effect of delay in surgery on the length of postoperative hospitalization. By investigating the cause of the delayed surgery, they found that age (P=0.312) and gender (P=0.7102) were not determining factors for the kind of surgery (early or delayed). In addition, they found that factors like medications and comorbidities, such as pneumonia or heart disease (OR=2.780, 95% confidence interval [CI], 1.012%, 7.640%, P=0.047), have a significant relationship with the mortality rate related to pelvic fracture. Charlson’s comorbidity index has shown increased marginal mortality (OR=1.431, 95% CI, 0.958%, 2.137%, P=0.080) in these patients compared to delay in surgery due to hospitalization factors, such as hospitalization on weekends or holidays, or delay due to the surgery schedule or consultation with other specialties. Therefore, the trigger of the higher rate of mortality in patients with delayed surgery may be in part due to the inappropriateness of the patient’s health status, such as drugs or medical status.
5. Conclusion
Most patients with underlying disease who undergo delayed intertrochanteric fracture surgeries experience more length of hospitalization and surgery duration. This delay brings about more short and long-term mortality rates among patients. Timely surgical intervention is crucial to improve outcomes in these patients.
Ethical Considerations
Compliance with ethical guidelines
This retrospective cross-sectional study, approved by the Ethics Committee of Isfahan University of Medical Sciences (Code: IR.MUI.MED.REC.1398.439).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, and supervision: Mohammad Ali Tahririan and Hossein Akbari Aghdam; Formal analysis: Mohammad Ali Tahririan and Mohammad Shahsavan; Methodology, and the original draft preparation: Hossein Akbari Aghdam and Mohammad Shahsavan; Project administration: Farnaz Jokar and Ashkan Jalili; Review and editing: Mohammad Ali Tahririan, Hossein Akbari Aghdam, and Mohammad Shahsavan; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank Ayatollah Kashani Hospital, Isfahan, for their support and access to essential data. The authors are also grateful to their colleagues and all who contributed to this research.
References
Intertrochanteric fracture is common among the elderly, especially those with osteoporosis [1-5]. While the mortality rate related to intertrochanteric fracture has reduced due to medical care advancements in recent years [6], this kind of fracture still accompanies a considerable mortality rate among the elderly. Early mortality (within one month) among these patients has been reported to range between 10%-30% in various studies [7-12].
Several factors contribute to the mortality of patients with intertrochanteric fractures, including advancing age, delays in operative treatment, underlying diseases, duration of surgery, and anesthesia methods [13]. Additionally, studies have mentioned the influence of surgeons’ experience, hospital patient load [14], and obesity [5] on mortality rates.
Due to the uncertainty of mortality causes and lack of comprehensive studies on this subject, this study was conducted to compare the short and long-term mortality rates and the hospitalization duration in intertrochanteric fracture patients receiving early and delayed surgical treatment.
2. Methods
The utilized data from patients with femoral intertrochanteric fractures who were referred to Ayatollah Kashani Hospital, Isfahan City, Iran from 2018 to 2020.
The inclusion criteria included patients with intertrochanteric fractures who underwent surgery between 2018 and 2020 and had adequate information available in their medical records or accessible through family members.
We collected demographic data, underlying diseases, duration from admission to surgery, surgery duration, and length of hospital stay after surgery from the related documents. Patients were categorized into two groups based on surgical delay, those with delay (surgery initiated more than 48 hours after hospital admission), and those without delay.
Patients’ mortality status, post-surgery complications, and the period after surgery to their death were obtained through phone calls. Patients’ death was classified into short-term (within one month after surgery), and long-term (within one year after surgery).
Data were analyzed using SPSS software, version 26 with the chi-square test and t-test.
3. Results
A total of 308 patients with intertrochanteric fractures with a mean age of 62.35±10.15 years were selected. Among them, 230 patients (74.7%) were men and 78 patients (25.3%) were women. Also, 8.4% of them had underlying diseases. The mean duration of surgery was 1.23±0.57 hours, and the mean length of hospital stay was 13.99±3.27 days. Delayed surgery was observed in 47 patients (15.3%), and 261(84.7%) underwent surgery without delay. Furthermore, 7 patients (2.3%) died within one month post-surgery, and 13 patients (4.2%) died within one year after surgery.
The subjects in the two groups had no significant difference in their age and gender, but the existence of underlying disease was significantly higher in the group with delayed surgery (P<0.001). Moreover, the mean length of hospital stay (P<0.001), duration of surgery (P<0.001), short-term mortality (P=0.01), and long-term mortality (P<0.001) were significantly higher in the delayed surgery group (Table 1).
4. Discussion
While delaying surgery for a femoral intertrochanteric fracture may allow for more comprehensive patient evaluation and medical optimization, it also introduces various complications, such as bed sore, thromboembolism, infection, delayed rehabilitation, prolonged hospital stay, and increased mortality rates.
In our study, we observed higher short and long-term mortality rates among patients with delayed surgery. There is controversy in recent studies concerning the correlation between delayed surgery and mortality rates. Leung et al. reviewed 42 studies and found that early surgery was associated with lower side effects, mortality rates, bed sores, and hospitalization duration. However, evidence of short and long-term mortality was diverse [15]. This is probably due to the small sample size, diverse definitions of delayed surgery, and failure to evaluate the cause of the surgery [16]. Daugaard et al. investigated 38,020 patients from 2003 to 2010 and reported that delayed surgery after acute pelvic fracture accompanies with a considerable increase in short-term mortality (odds ratio (OR)=1.3 in 24-hour delay) [16]. Similarly, Poór et al. found that increased comorbidity significantly increased mortality in patients with hip fractures, highlighting the critical nature of timely surgery [17]. Rosso et al. concluded that surgical treatment for pelvic fractures should be performed within 48 hours [18].
In our study, gender and age were not related to delayed surgery, but patients with underlying diseases were more likely to experience delayed surgeries, with longer surgical durations and hospitalizations observed in this group.
A study by Cha et al., similar to ours, found a correlation between delay in surgery and mortality rate in patients with intertrochanteric fracture [19]. While investigating factors contributing to surgical delays, they did not explore the impact of surgery duration on delays or the effect of delay in surgery on the length of postoperative hospitalization. By investigating the cause of the delayed surgery, they found that age (P=0.312) and gender (P=0.7102) were not determining factors for the kind of surgery (early or delayed). In addition, they found that factors like medications and comorbidities, such as pneumonia or heart disease (OR=2.780, 95% confidence interval [CI], 1.012%, 7.640%, P=0.047), have a significant relationship with the mortality rate related to pelvic fracture. Charlson’s comorbidity index has shown increased marginal mortality (OR=1.431, 95% CI, 0.958%, 2.137%, P=0.080) in these patients compared to delay in surgery due to hospitalization factors, such as hospitalization on weekends or holidays, or delay due to the surgery schedule or consultation with other specialties. Therefore, the trigger of the higher rate of mortality in patients with delayed surgery may be in part due to the inappropriateness of the patient’s health status, such as drugs or medical status.
5. Conclusion
Most patients with underlying disease who undergo delayed intertrochanteric fracture surgeries experience more length of hospitalization and surgery duration. This delay brings about more short and long-term mortality rates among patients. Timely surgical intervention is crucial to improve outcomes in these patients.
Ethical Considerations
Compliance with ethical guidelines
This retrospective cross-sectional study, approved by the Ethics Committee of Isfahan University of Medical Sciences (Code: IR.MUI.MED.REC.1398.439).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, and supervision: Mohammad Ali Tahririan and Hossein Akbari Aghdam; Formal analysis: Mohammad Ali Tahririan and Mohammad Shahsavan; Methodology, and the original draft preparation: Hossein Akbari Aghdam and Mohammad Shahsavan; Project administration: Farnaz Jokar and Ashkan Jalili; Review and editing: Mohammad Ali Tahririan, Hossein Akbari Aghdam, and Mohammad Shahsavan; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank Ayatollah Kashani Hospital, Isfahan, for their support and access to essential data. The authors are also grateful to their colleagues and all who contributed to this research.
References
- Tahririan MA, Motififard M, Omidian A, Aghdam HA, Esmaeali A. Relationship between bone mineral density and serum vitamin D with Low energy hip and distal radius fractures: A case-control study. Arch Bone Jt Surg. 2017; 5(1):22-7. [DOI:10.22038/abjs.2016.7936]
- World Health O. WHO global status report on road safety 2013: Supporting a decade of action. Geneva: World Health Organization; 2013. [Link]
- Ebrahimzadeh MH. National trauma registry center, as a backbone of trauma management and research. Arch Trauma Res. 2012; 1(3):87-8. [DOI:10.5812/atr.8487] [PMID] [PMCID]
- Kazemian M, Movahhedi M, Movahhed F. [Facial fracture types in motorcyclists with and without helmet in southeast of Iran (Persian)]. J Mashhad Dent Sch. 2019; 43(3):295-303. [DOI:10.22038/jmds.2019.13842]
- Kempegowda H, Richard R, Borade A, Tawari A, Graham J, Suk M, et al. Obesity is associated with high perioperative complications among surgically treated intertrochanteric fracture of the femur. J Orthop Trauma. 2017; 31(7):352-7. [DOI:10.1097/BOT.0000000000000825] [PMID]
- Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop. 2014; 85(1):54-9. [DOI:10.3109/17453674.2013.878831] [PMID] [PMCID]
- Mant M, de la Cova C, Ives R, Brickley MB. Perimortem fracture manifestations and mortality after hip fracture in a documented skeletal series. Int J Paleopathol. 2019; 27:56-65.[DOI:10.1016/j.ijpp.2019.09.002] [PMID]
- Downey C, Kelly M, Quinlan JF. Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop. 2019; 10(3):166-75. [DOI:10.5312/wjo.v10.i3.166] [PMID] [PMCID]
- Albrecht JS, Al Kibria G, Gruber-Baldini A, Magaziner J. Risk of mortality in individuals with hip fracture and traumatic brain injury. J Am Geriatr Soc. 2019; 67(1):124-7. [DOI:10.1111/jgs.15661] [PMID] [PMCID]
- Hao L, Carson JL, Schlussel Y, Noveck H, Shapses SA. Vitamin D deficiency is associated with reduced mobility after hip fracture surgery: A prospective study. Am J Clin Nutr. 2020; 112(3):613-8. [DOI:10.1093/ajcn/nqaa029] [PMID] [PMCID]
- Abraham DS, Barr E, Ostir GV, Hebel JR, Golden J, Gruber-Baldini AL, et al. Residual disability, mortality, and nursing home placement after hip fracture over 2 decades. Arch Phys Med Rehabil. 2019; 100(5):874-82. [DOI:10.1016/j.apmr.2018.10.008] [PMID] [PMCID]
- Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: Is delay before surgery important? J Bone Joint Surg Am. 2005; 87(3):483-9. [DOI:10.2106/JBJS.D.01796] [PMID]
- Kesmezacar H, Ayhan E, Unlu MC, Seker A, Karaca S. Predictors of mortality in elderly patients with an intertrochanteric or a femoral neck fracture. J Trauma. 2010; 68(1):153-8. [DOI:10.1097/TA.0b013e31819adc50] [PMID]
- Browne JA, Pietrobon R, Olson SA. Hip fracture outcomes: Does surgeon or hospital volume really matter? J Trauma. 2009; 66(3):809-14. [DOI:10.1097/TA.0b013e31816166bb] [PMID]
- Leung F, Lau TW, Kwan K, Chow SP, Kung AW. Does timing of surgery matter in fragility hip fractures? Osteoporos Int. 2010; 21(Suppl 4):S529-34. [DOI:10.1007/s00198-010-1391-2] [PMID] [PMCID]
- Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012; 83(6):609-13. [DOI:10.3109/17453674.2012.747926] [PMID] [PMCID]
- Poór G, Atkinson EJ, O’Fallon WM, Melton LJ, 3rd. Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res. 1995(319):260-5. [DOI:10.1097/00003086-199510000-00028]
- Rosso F, Dettoni F, Bonasia DE, Olivero F, Mattei L, Bruzzone M, et al. Prognostic factors for mortality after hip fracture: Operation within 48 hours is mandatory. Injury. 2016; 47 Suppl 4:S91-7. [DOI:10.1016/j.injury.2016.07.055] [PMID]
- Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017; 137(5):625-30. [DOI:10.1007/s00402-017-2674-2] [PMID]
Type of Study: Research Article |
Subject:
Hip surgery
Received: 2022/02/21 | Accepted: 2022/05/2 | Published: 2022/11/1
Received: 2022/02/21 | Accepted: 2022/05/2 | Published: 2022/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |