Volume 9, Issue 4 (11-2022)
JROS 2022, 9(4): 233-238 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sabaghzadeh A, Biglari F, Barazandeh Rad S, Ghassemi A, Sadighi M, Nouroozi M, et al . The Impact of a Short Video Versus Face-to-face Patient Education in Reverse Sural Flap Surgery. JROS 2022; 9 (4) :233-238
URL: http://jros.iums.ac.ir/article-1-2212-en.html
URL: http://jros.iums.ac.ir/article-1-2212-en.html
Amir Sabaghzadeh1 

 , Farsad Biglari1
, Farsad Biglari1 

 , Saber Barazandeh Rad1
, Saber Barazandeh Rad1 

 , Ali Ghassemi2
, Ali Ghassemi2 
 , Mehrdad Sadighi1
, Mehrdad Sadighi1 

 , Mohammad Nouroozi1
, Mohammad Nouroozi1 

 , Meisam Jafari Kafiabadi1
, Meisam Jafari Kafiabadi1 

 , Adel Ebrahimpour1
, Adel Ebrahimpour1 




 , Farsad Biglari1
, Farsad Biglari1 

 , Saber Barazandeh Rad1
, Saber Barazandeh Rad1 

 , Ali Ghassemi2
, Ali Ghassemi2 
 , Mehrdad Sadighi1
, Mehrdad Sadighi1 

 , Mohammad Nouroozi1
, Mohammad Nouroozi1 

 , Meisam Jafari Kafiabadi1
, Meisam Jafari Kafiabadi1 

 , Adel Ebrahimpour1
, Adel Ebrahimpour1 


1- Department of Orthopedic Surgery, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Young Researchers and Elite Club, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran.
2- Young Researchers and Elite Club, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran.
Full-Text [PDF 2425 kb]
(129 Downloads)
| Abstract (HTML) (576 Views)
Full-Text: (190 Views)
1. Introduction
Soft tissue reconstruction with a reverse sural artery flap (RSAF) is a useful way to reconstruct soft tissue defects around the ankle, distal tibia, and heel [1, 2]. Due to the complexity of the surgical procedure and the need for patient compliance with post-operation care, it is crucial to properly educate patients undergoing this surgery [3]. Traditionally, patient education is performed orally (face-to-face) and may be supplemented with pamphlets. Recently, supplementing video education with oral and written information is an appropriate method for patients for surgery and helps improve short-term outcomes in an enhanced recovery program [4, 5].
This study aims to evaluate the impact of short video versus face-to-face education in patients undergoing reverse sural flap (RSAF) surgery in a tertiary referral center.
2. Methods
This study was a prospective randomized clinical trial performed between August 2019 and August 2022 after the approval of the relevant Shahid Beheshti University of Medical Sciences, Tehran, Iran. This study included 30 male patients with soft tissue defects around the ankle and distal tibia between the ages of 15 to 70 years who underwent the RSAF surgery. The soft tissue defects occurred as complications of Achilles tendon repair (Figure 1), excision of soft tissue mass (Figure 2), spoke wheel injury (Figure 3), open fracture (Figure 4), and open reduction and internal fixation of ankle fractures (Figure 5). The exclusion criteria included patients with chronic untreated osteomyelitis, complex regional pain syndrome, vascular injuries, and heavy smokers with major medical comorbidity, and a patient who did not know Farsi. All the patients underwent the same surgical technique by the same surgeon. Before the surgery, patients were randomized by simple randomization into two groups:
Group A: In this group, the post-operative cure process was described to them and they were accompanied orally and face-to-face by their surgeon.
Group B: In the second group, we used a short video to give them the information about post-operative cure process.
The media used was a short 6-minute video containing an explanation of the procedure, post-operative care, and what to expect after surgery on a real patient undergoing sural flap surgery.
Before initiation of the surgery, to reduce the possibility of bias, we asked accompanies of the group B patients about the video, especially those of advanced age or unfamiliar with visual learning via videos. In the noted group, the surgeon also checked the accuracy and correctness of post-operative orders. The provided video contained some advice to improve healing, such as staying in a warm room, prohibition smoking and alcohol consumption, a suitable amount of sleep, all the procedures for wound dressing, prohibition showering until 5 days after surgery, the necessity of walking with a cane one day after surgery. Particular emphasis was placed on the patient’s position on the bed which must be prone or lateral to make sure that the flap pedicle is not under pressure. All the contents were comprehensively explained for all levels of education. This short video was made in a clinical space in the hospital by the surgeon himself. After all, the correctness and accuracy of the information and orders were checked if patients had correctly learned them by their surgeon. During the post-operation period, the integrity of procedure-learning by patients and flap condition was checked by the educated nurse in the surgical ward every 2 hours in the first 24 hours and every 4 hours on the following day.
Two groups of patients were compared in specific variables which include flap failure, days between surgery to discharge, and flap congestion classified into 4 levels based on the gloss units (GU) scale [6]. All data were analyzed with SPSS software, version 26. Blood transfusion, infection, flap failure, and flap congestion level were examined by Fisher’s exact test, and the days between surgery to discharge variable among the 2 groups was examined by the Mann-Whitney test.
3. Results
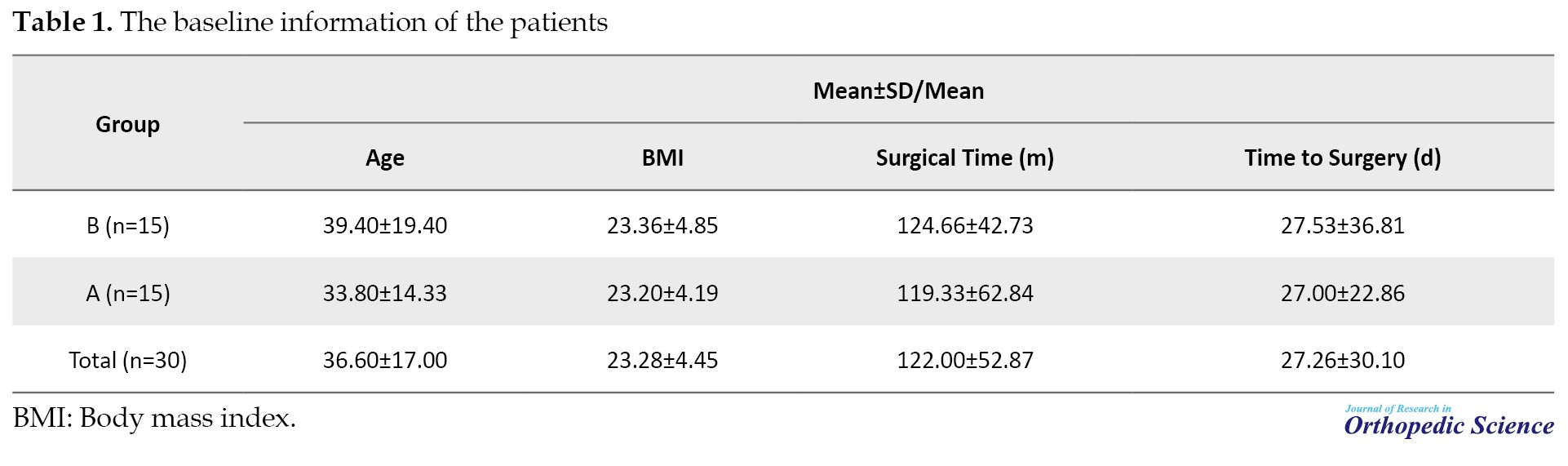
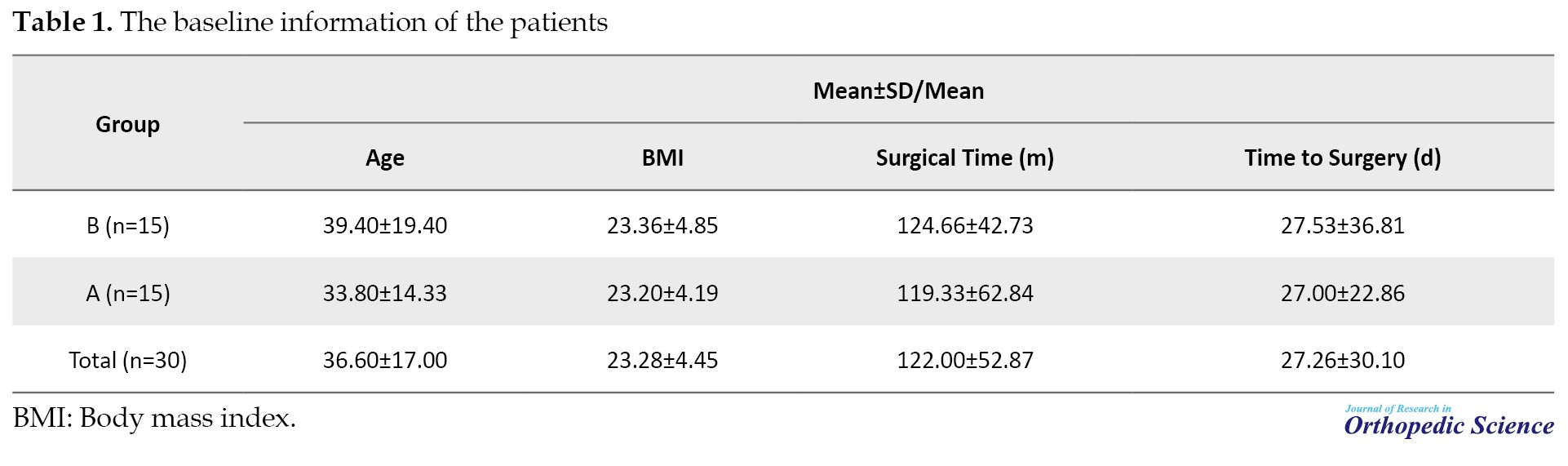
Table 1 presents the baseline information of the patients.
Among 30 patients, we had 12 patients (40%) with different levels of flap congestion. In these patients, the rate of grade IV flap congestion was equal in the two groups (6.70% in each group). Other grades of flap congestion were more frequent in patients of group A (Table 2).
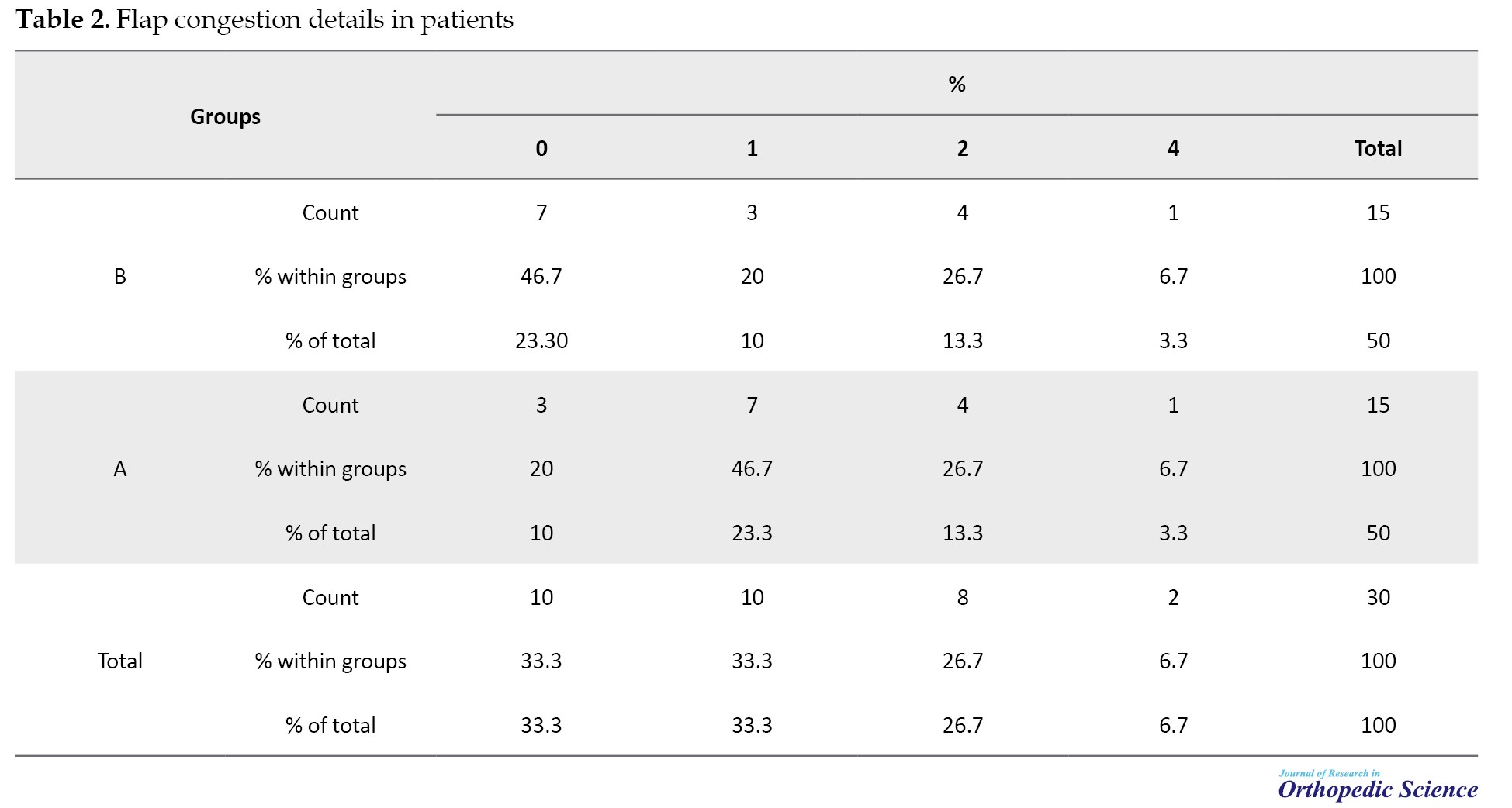
None of our participants experienced grade III congestion. To summarize the grade of congestion was not significantly different between the two groups (P>0.05); however, more patients in group A experienced variable grades of congestion. The mean days from surgery to discharge were 8.4 days in group A and 10.06 days in group B showing no meaningful difference (P>0.05). None of our patients experienced major complications, such as deep vein thrombosis, infection, and flap failure.
4. Discussion
Giving sufficient information about post-operative care is an essential part of successful surgeries, especially in reconstructive surgeries in which patients must be careful about the reconstructed areas of contaminations, congestion, and other probable findings that may lead to poor outcomes. RSAF operation is a sophisticated surgery with complicated post-operative care. In this procedure, we usually face challenges that may affect this information, such as the difficulty of this information for patients, or forgetfulness for either patients or surgeons. Therefore, using a reserved source can help us to overcome these challenges. Several methods are available to increase the patients’ knowledge, such as short videos, social media, pamphlets, mobile applications, and web-based education [7].
The informative video presents a modern and cost-effective method for the justified and detailed education of the patient about the postoperative care of complicated procedures, such as RSAF. Improved patient perception of treatment directly improves conditions of surgical care and leads to a better postoperative quality of life (QoL) [8]. According to our result, the instructional video was effective in increasing post-operative knowledge and care of patients [9]. Our result showed no meaningful difference in outcomes and complications related to RSAF surgery between face-to-face and short video education. Our result is compatible with previous studies on pelvic organ prolapse undergoing reconstructive surgery, liver transplantation, and breast cancer [10, 11].
A study conducted by Godwin reported a low recall rate (almost 50%) of information given to patients about probable complications after plastic surgeries [12]. In this regard, the application of social media for patient education may improve treatment outcomes, especially in young patients who comprise most orthopedic patients [13]. The possibility of repeated explanations for patients is another advantage of using media in post-operation care [14].
The application of social media also decreases healthcare costs since it reduces the need for face-to-face visits, and improves the accuracy of information provided by the surgeon about the procedure and probable complications. However, we cannot overlook some disadvantages of using media as the only method of patient education instead of face-to-face interaction, such as the lack of direct patient-physician communication [15]. We recommend improving such by using social networks and updated applications to avoid any possible misunderstanding for patients. Although rapid growth in the usage of social media networks, such as YouTube, Facebook, and WhatsApp may assist physicians in reaching out to their patients they bring out novel challenges, such as the reckless sharing of fake news and disinformation [16].
5. Conclusion
The current evidence shows that postoperative virtual clinical education via video is non-inferior to traditional in-office clinical encounters with high levels of short-term patient satisfaction [17]. We recommend a combination of face-to-face education and the aid of video resources to ensure optimum patient education in complicated procedures, such as RSAFs. Further studies with larger sample sizes and on patients undergoing other surgical procedures are recommended to determine the best method of education for patients undergoing challenging procedures, such as RSAF.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethic Committee of Shahid Beheshti University of Medical Sciences (Code: (IR.SBMU.RETECH.REC.1400.1195).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Meisam Jafari Kafiabadi; Data acquisition: Amir Sabaghzadeh, Saber Barazandeh Rad, and Mehrdad Sadighi; Data analysis: Ali Ghassemi, Farsad Biglari; Final approval: Meisam Jafari Kafiabadi, and Adel Ebrahimpour.
Conflict of interest
The authors declared no conflict of interest.
References
Soft tissue reconstruction with a reverse sural artery flap (RSAF) is a useful way to reconstruct soft tissue defects around the ankle, distal tibia, and heel [1, 2]. Due to the complexity of the surgical procedure and the need for patient compliance with post-operation care, it is crucial to properly educate patients undergoing this surgery [3]. Traditionally, patient education is performed orally (face-to-face) and may be supplemented with pamphlets. Recently, supplementing video education with oral and written information is an appropriate method for patients for surgery and helps improve short-term outcomes in an enhanced recovery program [4, 5].
This study aims to evaluate the impact of short video versus face-to-face education in patients undergoing reverse sural flap (RSAF) surgery in a tertiary referral center.
2. Methods
This study was a prospective randomized clinical trial performed between August 2019 and August 2022 after the approval of the relevant Shahid Beheshti University of Medical Sciences, Tehran, Iran. This study included 30 male patients with soft tissue defects around the ankle and distal tibia between the ages of 15 to 70 years who underwent the RSAF surgery. The soft tissue defects occurred as complications of Achilles tendon repair (Figure 1), excision of soft tissue mass (Figure 2), spoke wheel injury (Figure 3), open fracture (Figure 4), and open reduction and internal fixation of ankle fractures (Figure 5). The exclusion criteria included patients with chronic untreated osteomyelitis, complex regional pain syndrome, vascular injuries, and heavy smokers with major medical comorbidity, and a patient who did not know Farsi. All the patients underwent the same surgical technique by the same surgeon. Before the surgery, patients were randomized by simple randomization into two groups:
Group A: In this group, the post-operative cure process was described to them and they were accompanied orally and face-to-face by their surgeon.
Group B: In the second group, we used a short video to give them the information about post-operative cure process.
The media used was a short 6-minute video containing an explanation of the procedure, post-operative care, and what to expect after surgery on a real patient undergoing sural flap surgery.
Before initiation of the surgery, to reduce the possibility of bias, we asked accompanies of the group B patients about the video, especially those of advanced age or unfamiliar with visual learning via videos. In the noted group, the surgeon also checked the accuracy and correctness of post-operative orders. The provided video contained some advice to improve healing, such as staying in a warm room, prohibition smoking and alcohol consumption, a suitable amount of sleep, all the procedures for wound dressing, prohibition showering until 5 days after surgery, the necessity of walking with a cane one day after surgery. Particular emphasis was placed on the patient’s position on the bed which must be prone or lateral to make sure that the flap pedicle is not under pressure. All the contents were comprehensively explained for all levels of education. This short video was made in a clinical space in the hospital by the surgeon himself. After all, the correctness and accuracy of the information and orders were checked if patients had correctly learned them by their surgeon. During the post-operation period, the integrity of procedure-learning by patients and flap condition was checked by the educated nurse in the surgical ward every 2 hours in the first 24 hours and every 4 hours on the following day.
Two groups of patients were compared in specific variables which include flap failure, days between surgery to discharge, and flap congestion classified into 4 levels based on the gloss units (GU) scale [6]. All data were analyzed with SPSS software, version 26. Blood transfusion, infection, flap failure, and flap congestion level were examined by Fisher’s exact test, and the days between surgery to discharge variable among the 2 groups was examined by the Mann-Whitney test.
3. Results
Table 1 presents the baseline information of the patients.
Among 30 patients, we had 12 patients (40%) with different levels of flap congestion. In these patients, the rate of grade IV flap congestion was equal in the two groups (6.70% in each group). Other grades of flap congestion were more frequent in patients of group A (Table 2).
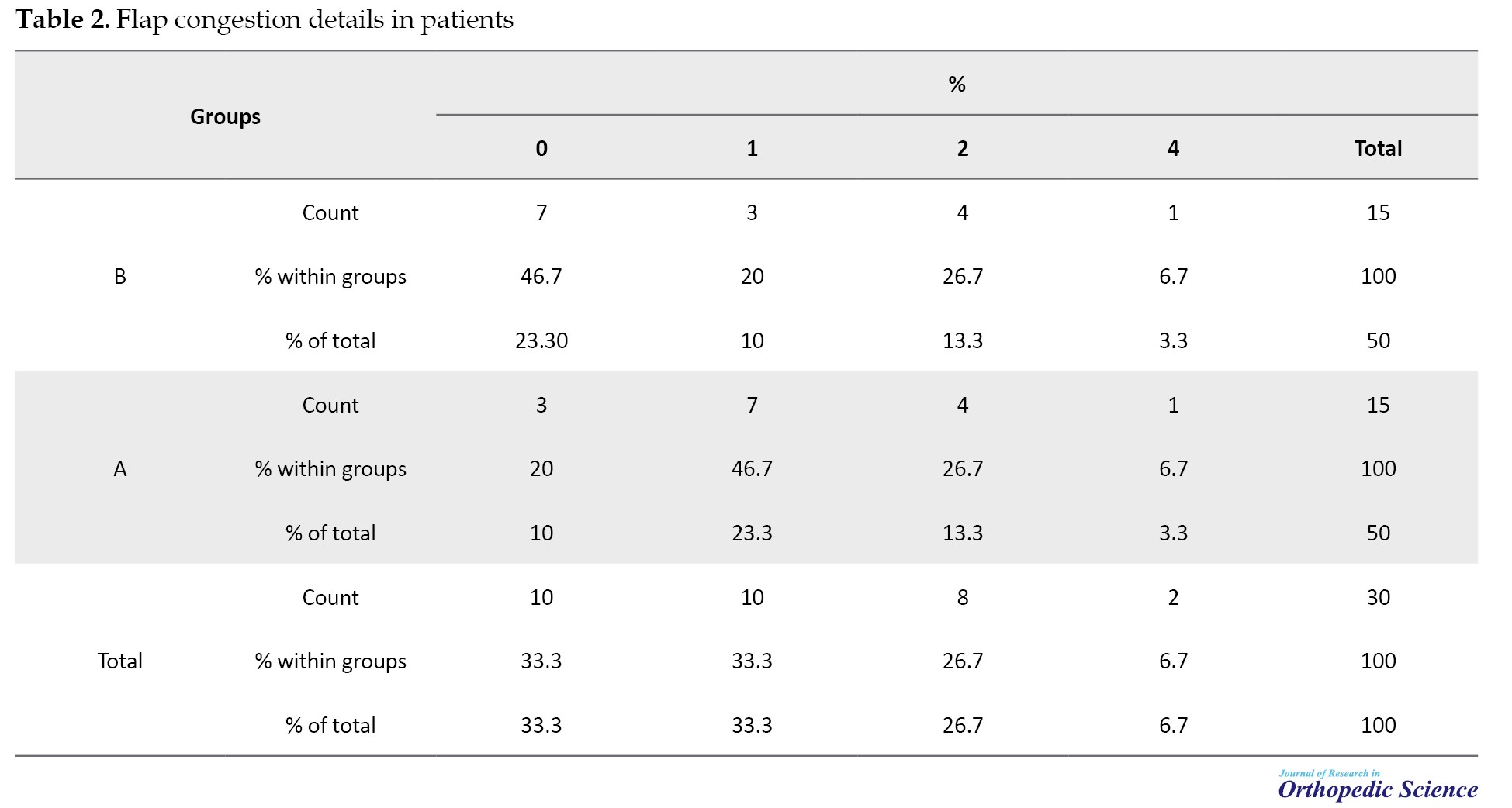
None of our participants experienced grade III congestion. To summarize the grade of congestion was not significantly different between the two groups (P>0.05); however, more patients in group A experienced variable grades of congestion. The mean days from surgery to discharge were 8.4 days in group A and 10.06 days in group B showing no meaningful difference (P>0.05). None of our patients experienced major complications, such as deep vein thrombosis, infection, and flap failure.
4. Discussion
Giving sufficient information about post-operative care is an essential part of successful surgeries, especially in reconstructive surgeries in which patients must be careful about the reconstructed areas of contaminations, congestion, and other probable findings that may lead to poor outcomes. RSAF operation is a sophisticated surgery with complicated post-operative care. In this procedure, we usually face challenges that may affect this information, such as the difficulty of this information for patients, or forgetfulness for either patients or surgeons. Therefore, using a reserved source can help us to overcome these challenges. Several methods are available to increase the patients’ knowledge, such as short videos, social media, pamphlets, mobile applications, and web-based education [7].
The informative video presents a modern and cost-effective method for the justified and detailed education of the patient about the postoperative care of complicated procedures, such as RSAF. Improved patient perception of treatment directly improves conditions of surgical care and leads to a better postoperative quality of life (QoL) [8]. According to our result, the instructional video was effective in increasing post-operative knowledge and care of patients [9]. Our result showed no meaningful difference in outcomes and complications related to RSAF surgery between face-to-face and short video education. Our result is compatible with previous studies on pelvic organ prolapse undergoing reconstructive surgery, liver transplantation, and breast cancer [10, 11].
A study conducted by Godwin reported a low recall rate (almost 50%) of information given to patients about probable complications after plastic surgeries [12]. In this regard, the application of social media for patient education may improve treatment outcomes, especially in young patients who comprise most orthopedic patients [13]. The possibility of repeated explanations for patients is another advantage of using media in post-operation care [14].
The application of social media also decreases healthcare costs since it reduces the need for face-to-face visits, and improves the accuracy of information provided by the surgeon about the procedure and probable complications. However, we cannot overlook some disadvantages of using media as the only method of patient education instead of face-to-face interaction, such as the lack of direct patient-physician communication [15]. We recommend improving such by using social networks and updated applications to avoid any possible misunderstanding for patients. Although rapid growth in the usage of social media networks, such as YouTube, Facebook, and WhatsApp may assist physicians in reaching out to their patients they bring out novel challenges, such as the reckless sharing of fake news and disinformation [16].
5. Conclusion
The current evidence shows that postoperative virtual clinical education via video is non-inferior to traditional in-office clinical encounters with high levels of short-term patient satisfaction [17]. We recommend a combination of face-to-face education and the aid of video resources to ensure optimum patient education in complicated procedures, such as RSAFs. Further studies with larger sample sizes and on patients undergoing other surgical procedures are recommended to determine the best method of education for patients undergoing challenging procedures, such as RSAF.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethic Committee of Shahid Beheshti University of Medical Sciences (Code: (IR.SBMU.RETECH.REC.1400.1195).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and study design: Meisam Jafari Kafiabadi; Data acquisition: Amir Sabaghzadeh, Saber Barazandeh Rad, and Mehrdad Sadighi; Data analysis: Ali Ghassemi, Farsad Biglari; Final approval: Meisam Jafari Kafiabadi, and Adel Ebrahimpour.
Conflict of interest
The authors declared no conflict of interest.
References
- Tripathee S, Basnet SJ, Lamichhane A, Hariani L. How safe is reverse sural flap?: A systematic review. Eplasty. 2022; 22:e18. [PMID]
- Khoshnevis J, Dashti T, Azargashb E, Kalantar Motamedi MR. How much can we do by reverse superficial sural artery flap to potentiate its effects: Introducing spout sural flap as a new modification. World J Plast Surg. 2017; 6(3):343-50. [PMID]
- Mahmoud WH. Foot and ankle reconstruction using the distally based sural artery flap versus the medial plantar flap: A comparative study. J Foot Ankle Surg. 2017; 56(3):514-8. [DOI:10.1053/j.jfas.2017.01.019] [PMID]
- Juo YY, Freeby MJ, Arguello V, Liu L, Huang E, Dutson E, et al. Efficacy of video-based education program in improving metabolic surgery perception among patients with obesity and diabetes. Surg Obes Relat Dis. 2018; 14(9):1246-53. [DOI:10.1016/j.soard.2018.05.019] [PMID]
- Ihedioha U, Vaughan S, Mastermann J, Singh B, Chaudhri S. Patient education videos for elective colorectal surgery: Results of a randomized controlled trial. Colorectal Dis. 2013; 15(11):1436-41. [DOI:10.1111/codi.12348] [PMID]
- Chang SM, Wang X, Huang YG, Zhu XZ, Tao YL, Zhang YQ. Distally based perforator propeller sural flap for foot and ankle reconstruction: A modified flap dissection technique. Ann Plast Surg. 2014; 72(3):340-5. [DOI:10.1097/SAP.0b013e31826108f1] [PMID]
- Curry E, Li X, Nguyen J, Matzkin E. Prevalence of internet and social media usage in orthopedic surgery. Orthop Rev (Pavia). 2014; 6(3):5483. [DOI:10.4081/or.2014.5483]
- Zieren J, Menenakos C, Mueller JM. Does an informative video before inguinal hernia surgical repair influence postoperative quality of life? Results of a prospective randomized study. Qual Life Res. 2007; 16(5):725-9. [DOI:10.1007/s11136-007-9171-y] [PMID]
- Ong J, Miller PS, Appleby R, Allegretto R, Gawlinski A. Effect of a preoperative instructional digital video disc on patient knowledge and preparedness for engaging in postoperative care activities. Nurs Clin North Am. 2009; 44(1):103-15, xii. [DOI:10.1016/j.cnur.2008.10.014] [PMID]
- Wilkins EG, Lowery JC, Copeland LA, Goldfarb SL, Wren PA, Janz NK. Impact of an educational video on patient decision making in early breast cancer treatment. Med Decis Making. 2006; 26(6):589-98. [DOI:10.1177/0272989X06295355] [PMID]
- Ertel AE, Kaiser TE, Abbott DE, Shah SA. Use of video-based education and tele-health home monitoring after liver transplantation: Results of a novel pilot study. Surgery. 2016; 160(4):869-76. [DOI:10.1016/j.surg.2016.06.016] [PMID]
- Godwin Y. Do they listen? A review of information retained by patients following consent for reduction mammoplasty. Br J Plast Surg. 2000; 53(2):121-5. [DOI:10.1054/bjps.1999.3220] [PMID]
- Lander ST, Sanders J, Cook PC, O’Malley NT. Social media in pediatric orthopedics. J Pediatr Orthop. 2017; 37(7):e436-9. [DOI:10.1097/BPO.0000000000001032] [PMID] [PMCID]
- McCormick JR, Patel MS, Hodakowski AJ, Rea PM, Naik KP, Cohn MR, et al. Social media use by shoulder and elbow surgeons increases the number of ratings on physician review websites. J Shoulder Elbow Surg. 2021; 30(12):e713-23. [DOI:10.1016/j.jse.2021.06.018] [PMID]
- Saleh J, Robinson BS, Kugler NW, Illingworth KD, Patel P, Saleh KJ. Effect of social media in health care and orthopedic surgery. Orthopedics. 2012; 35(4):294-7. [DOI:10.3928/01477447-20120327-05] [PMID]
- Araghi F, Etesami I, Ohadi L, Dadkhahfar S. Social media and dermatology: Current and upcoming perspectives. J Cosmet Dermatol. 2022; 21(1):414. [DOI:10.1111/jocd.14638] [PMID]
- Lee DD, Arya LA, Andy UU, Harvie HS. Video virtual clinical encounters versus office visits for postoperative care after pelvic organ prolapse surgery: A randomized clinical trial. Female Pelvic Med Reconstr Surg. 2021; 27(7):432-8. [DOI:10.1097/SPV.0000000000000909] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Trauma
Received: 2022/03/17 | Accepted: 2022/05/3 | Published: 2022/11/1
Received: 2022/03/17 | Accepted: 2022/05/3 | Published: 2022/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |











