Volume 9, Issue 3 (8-2022)
JROS 2022, 9(3): 123-134 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yalfani A, Ahadi F, Ahmadi M. Investigating the Effect of Active and Passive Proximal Interventions on Dynamic Knee Valgus in Patients With Patellofemoral Pain: A Systematic Review. JROS 2022; 9 (3) :123-134
URL: http://jros.iums.ac.ir/article-1-2215-en.html
URL: http://jros.iums.ac.ir/article-1-2215-en.html
1- Department of Sport Injuries and Corrective Exercises, Faculty of Sport Sciences, Bu-Ali Sina University, Hamadan, Iran.
Full-Text [PDF 824 kb]
(198 Downloads)
| Abstract (HTML) (651 Views)
Full-Text: (225 Views)
1. Introduction
Patellofemoral pain (PFP) describes pain around or behind the patella [1, 2]. The key symptom of PFP is worsening pain during the patellofemoral joint (PFJ) loading [3, 4]. The PFJ loading increases in activities that require knee flexion [5, 6, 7]. PFP includes 37% of knee injuries [8]. The prevalence of PFP is reported at 22.7% in the general population and 35.7% among athletes [9, 10]. The prevalence of PFP in male and female populations is 15.5% and 29.2%, respectively [11]. Despite the high prevalence, the gold standard treatment for PFP has been unclear and 70% of patients report symptoms of recurrence after rehabilitation [12, 13]. Meanwhile, 74% of PFP patients have restrictions in daily activities, work, and sports participation [14]. Also, 31% of physical therapists advise patients to prevent sports activities when experiencing PFP [15]. In addition, 45% of subjects with a history of PFP may be at risk of developing patellofemoral osteoarthritis in the future [16]. However, the etiology of PFP remains unknown and has been considered an interaction between biomechanical, anatomical, and psychological factors [17].
In the biomechanical field, one of the main hypotheses accepted in the etiology of PFP is the increase in PFJ stress [18]. Overall, PFJ mechanics are influenced by proximal and distal mechanics [19]. PFP patients show faulty PFJ mechanics and proximal and distal poor dynamic control [20]. Changes in lower extremity mechanics can increase the PFJ stress and lead to the PFP occurrence [6, 21]. Dynamic knee valgus (DKV) is one of the faulty lower limb movement patterns that can increase PFJ stress [21-23]. DKV is defined as a combination of adduction and internal rotation of the hip, knee abduction, internal rotation, and abduction of the tibia and foot pronation. Ahmadi et al. reported that a normal DKV angle should be in the range of 5 to 12 for women and 1 to 9 for men [24]. Consequently, if the subjects have DKV angles beyond this range, it has a harmful outcome to the PFJ and the anterior cruciate ligament [25]. Overall, Herrington (2014) reported that PFP patients have higher DKV angles compared to healthy controls, which, if not corrected, may lead to increased PFJ stress [21]. Waiteman et al. (2018) reported that knee valgus and high knee abduction moment cause patella external tracking and the PFJ contact area increases in the external area and causes the PFJ cartilage destruction [26]. In this regard, Powers (2010) believes that DKV in the frontal plane should be prevented because it leads to unequal stress distribution in the PFJ and contributes to the etiology or exacerbation of PFP symptoms [27].
In a systematic review of the latest PFP research, Lankhorst et al. (2012) argued that multimodal treatment protocols, in addition to the quadriceps muscle, consider the segmental around the PFJ [28]. Proximal disorders have received extensive attention during the past decade [14]. Muscle weakness and faulty kinematics of the hip and trunk in the frontal plane may contribute to the increase of DKV and subsequently to the PFP occurrence [29]. Overall, adduction and internal rotation of the hip lead to medial knee displacement, which causes tibia abduction and foot pronation, resulting in DKV [6, 29]; therefore, poor hip control leads to patellar external tracking, high PFJ stress, and subsequent PFJ cartilage damage [20, 30]. Accordingly, clinicians have focused on gluteal muscle weakness and poor dynamic control of the lower extremities in the assessment, treatment, and prevention of PFP.
In recent years, the role of hip stabilizers has been in the studies of subjects and rehabilitation protocols. Meanwhile, researchers at the fifth consensus of the international PFP research meeting, held in Manchester in 2015, recommended a combination of hip and knee exercises to reduce pain and improve function [12]. However, few studies have investigated the biomechanical effects of proximal-focused rehabilitation programs on the dynamic alignment of the lower extremities [29]. Lower extremity faulty biomechanics can be corrected with active interventions, such as exercise programs and movement retraining, or with passive interventions, such as brace and tape [1]. Publishing sufficient details of active and passive proximal interventions will enable physiotherapists to make better decisions in designing a comprehensive protocol [12]. Therefore, the aim of the systematic review is to the effect of active and passive proximal interventions on DKV in PFP patients. These recommendations can be utilized by athletic trainers and physical therapists to make evidence-based decisions about which exercises and passive interventions should be included in PFP rehabilitation and prevention programs.
2. Methods
Study protocols
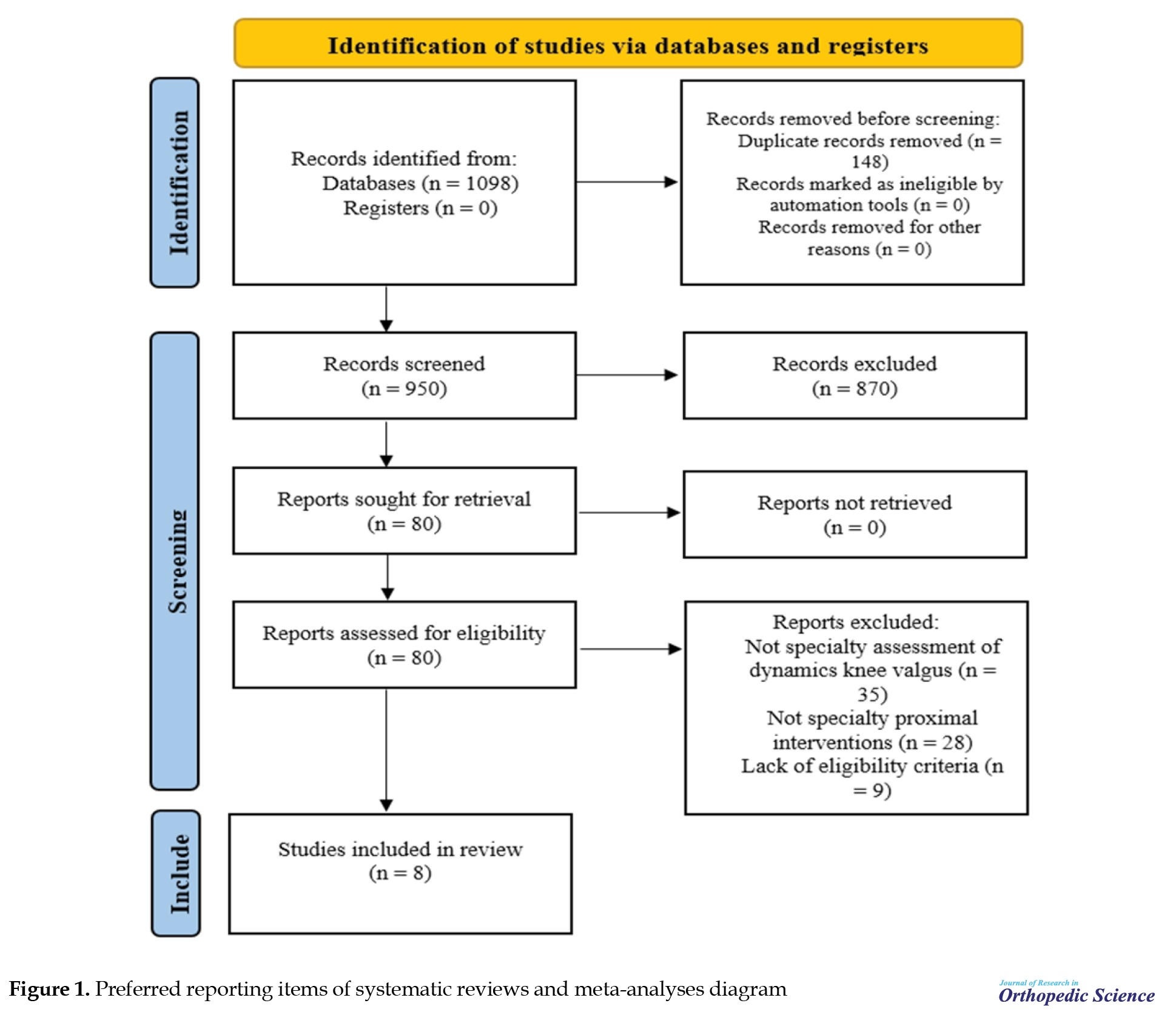
We followed the guidelines of preferred reporting items of systematic reviews and meta-analyses (PRISMA) 2020 for reporting systematic review and meta-analysis studies [31]. Since the PRISMA statement was designed for systematic review and meta-analysis studies, we only addressed items related to review systematic [32-34]. A comprehensive search was performed in PROSPERO and Cochrane library databases to identify previous similar studies. As a result, the detailed protocol of this systematic review has not been previously published or registered.
Eligibility criteria
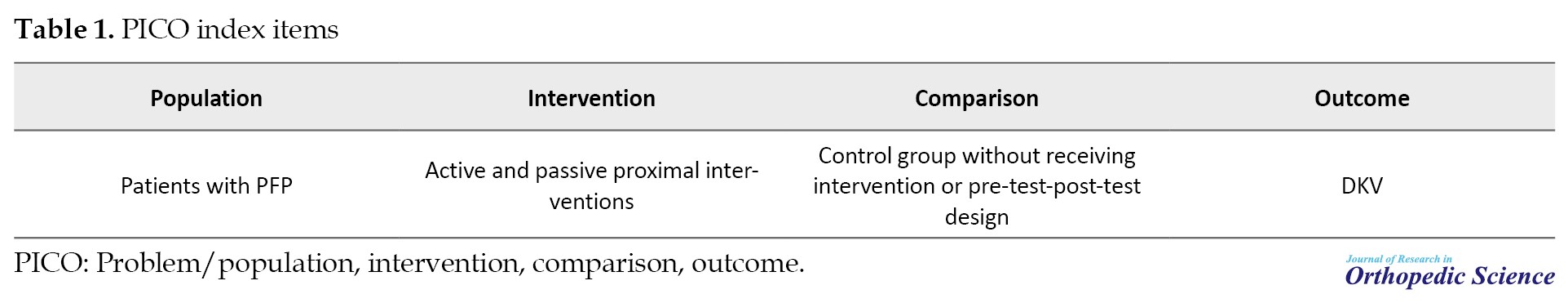
Table 1 summarizes the problem/population, intervention, comparison, and outcome items to define the inclusion and exclusion criteria.
The inclusion criteria were as follows: Clinical trial articles (experimental and control or pre-test-post-test design), cohort studies, case-control, case series, active and passive proximal interventions in PFP patients, articles in English, assessment of two-dimensional or three-dimensional DKV angle, articles limited to the period of 2000 to 2022, and participants who were PFP patients without other musculoskeletal problems. There was no limitation in the PFP patient population. The exclusion criteria were as follows: Review articles, editorials, abstracts, conferences, articles related to PFJ osteoarthritis, gray literature, interventions not specifically focused on the hip, and non-English articles.
Search strategy
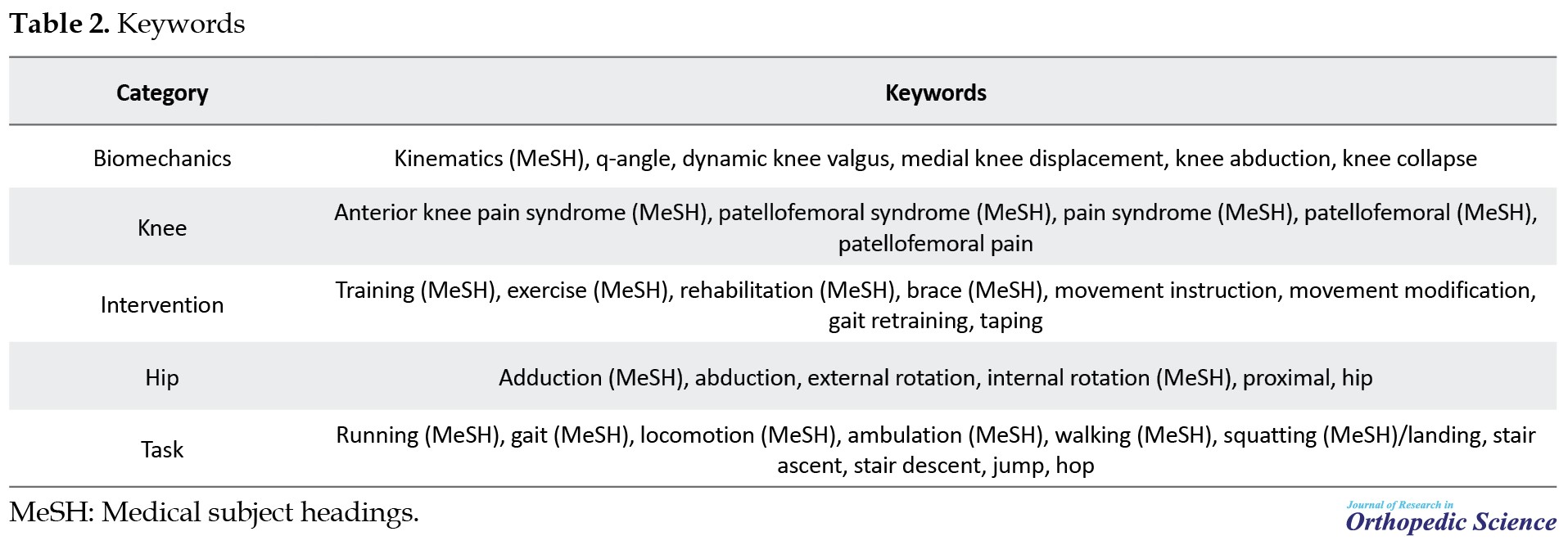
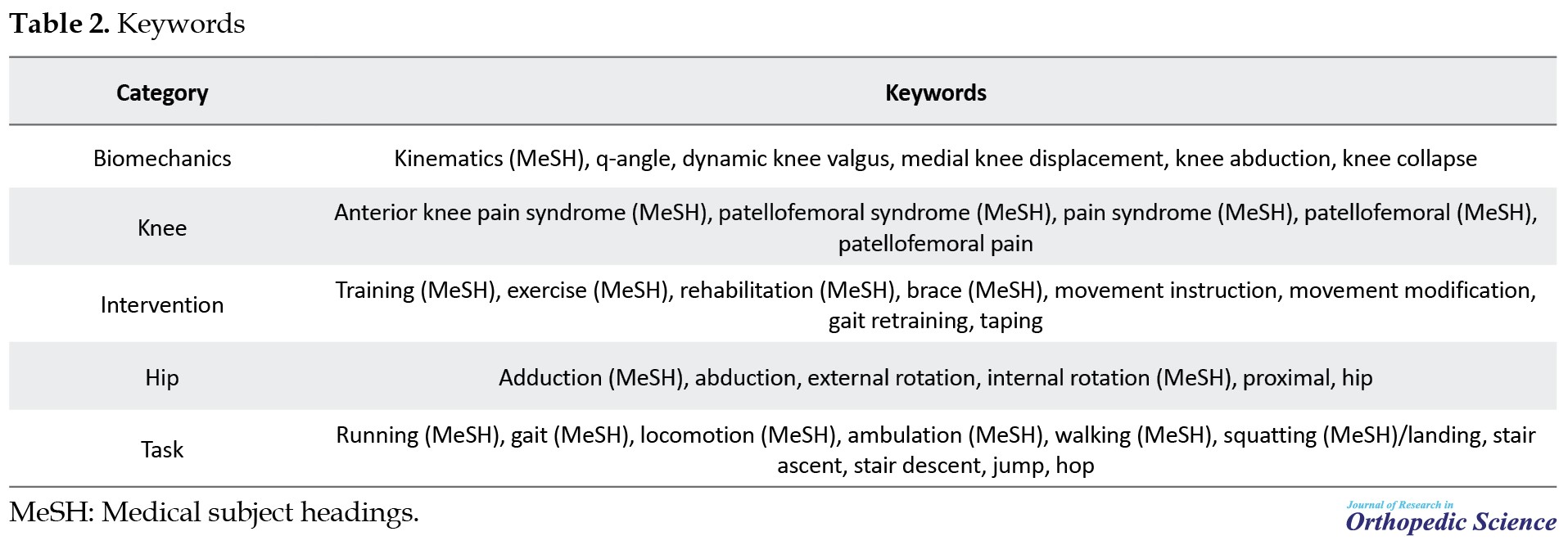
The search strategy was conducted independently by two rehabilitation specialists (FA & MA). Researchers used PubMed, Scopus, Web of Science, BioMed Central, Since Direct, Springer, and Cochrane Library databases for the online search. Also, Google Scholar was used as a complementary search engine. The articles were limited to the period of 2000 to 2022. To search, we used a combination of the medical subject headings (MeSH) framework and the keywords related to the study topic because many articles are listed in PubMed long before they are listed with MeSH terms [35]. The operative term “OR” was used to connect synonyms and the term “AND” was used to connect categories. According to the recommendation of the Cochrane Handbook, a manual search of the reference lists of previous systematic reviews and a citation search of the original record using the Web of Science were conducted [36]. Table 2 demonstrates the keywords used in the databases.
Study selection
The screening process of articles was conducted by two reviewers (FA & MA) independently in three stages. First, all the identified articles were saved in the reference software of Mendeley management. Articles were listed alphabetically and duplicate articles were removed by the software from the library. Then, according to the checklist prepared from the include and exclude criteria, the title and abstract of the articles were screened. Third, the full text of the articles that did not provide sufficient information from the title and abstract were reviewed.
Data extraction
Two reviewers (FA & MA) independently extracted the data using a predetermined extraction form that included the following items: Demographic information (name of the author, year of the publication, purpose, task, sample size); patients’ characteristics (statistical population, including general people or athletes with PFP); type of interventions (hip strengthening exercises, hip movement retraining, brace and tape of the hip); period (duration of protocol execution); motion analysis (two-dimensional or three-dimensional); outcome measurement (DKV angle assessment); results (the effect of interventions on DKV).
Quality assessment
Two reviewers (FA & MA) independently assessed the quality of articles using the Downs and Black checklist. A systematic review reported proper re-test ability (r=0.88), interrater reliability (r=0.75), and high internal consistency (KR-20=0.54) for the Downs and Black checklist [37]. Reporting, internal validity, external validity, and confounding internal validity are items of the Downs and Black checklist. The Downs and Black checklist consists of 27 items. Items 1 to 10 are related to reporting, 11 to 13 are external validity, 14 to 20 include internal validity, 21 to 26 are confounding internal validity, and 27 is power. The scoring of each item was considered 0 (no), 1 (yes). Items 4 and 5 were scored as 0 (no), 1 (somewhat), and 2 (yes) [38]. According to the previous study, the quality of articles was classified into three categories: High (≥70%), medium (40-69%), and low (<40%) [38].
3. Results
Study selection
The search in the electronic databases identified a total of 1098 articles from 2000 and 2022; however, 148 duplicate articles were removed from the library by the software. In total, 950 articles remained, of which 123 were gray literature, 164 abstracts, and conferences, 327 non-English language articles, 113 were related to osteoarthritis, and 215 articles did not assess the effect of proximal interventions on DKV and were excluded. Finally, 8 articles that met the eligibility criteria were selected for the systematic review [1, 16, 20, 29, 39-42]. Figure 1 shows the PRISMA diagram.
Study characteristics
Table 3 shows the summary of the demographic characteristics of the 8 included articles.
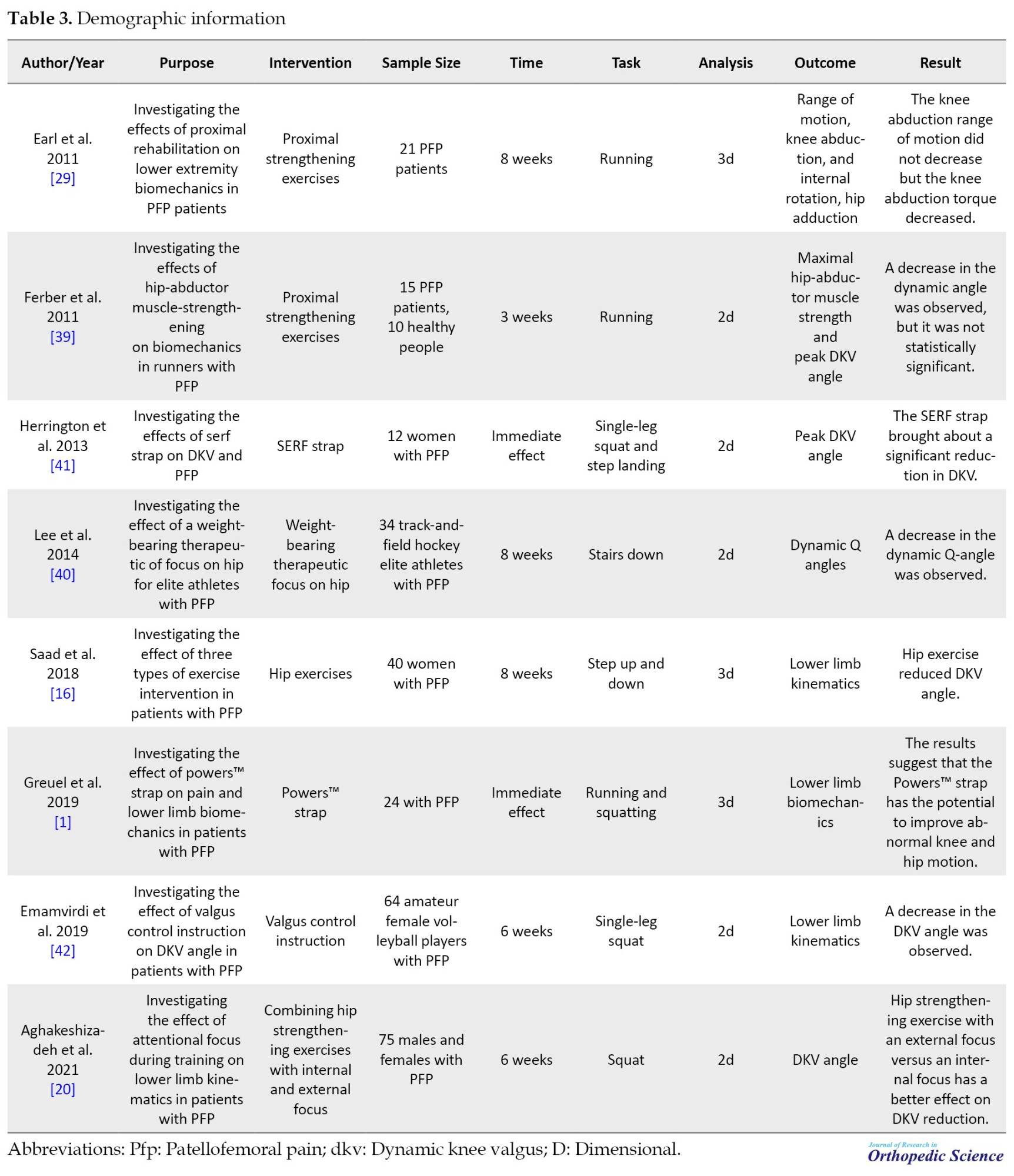
A total of 4 articles assessed the effect of proximal strengthening exercises [16, 29, 39, 40], 2 articles examined the effect of strengthening exercises combined with movement retraining [20, 42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of valgus control instruction (VCI), and 2 articles investigated the effect of brace and strap-on DKV [1, 41]. Overall, 285 patients with PFP and 10 healthy subjects participated in the studies. In active interventions, 4 articles used two-dimensional motion analysis [39, 40] and 2 articles used three-dimensional motion analysis [16, 29]. In passive interventions, 1 article used two-dimensional motion analysis [41] and 1 article used three-dimensional motion analysis [1].
Quality assessment
Table 4 shows the quality of the included articles.
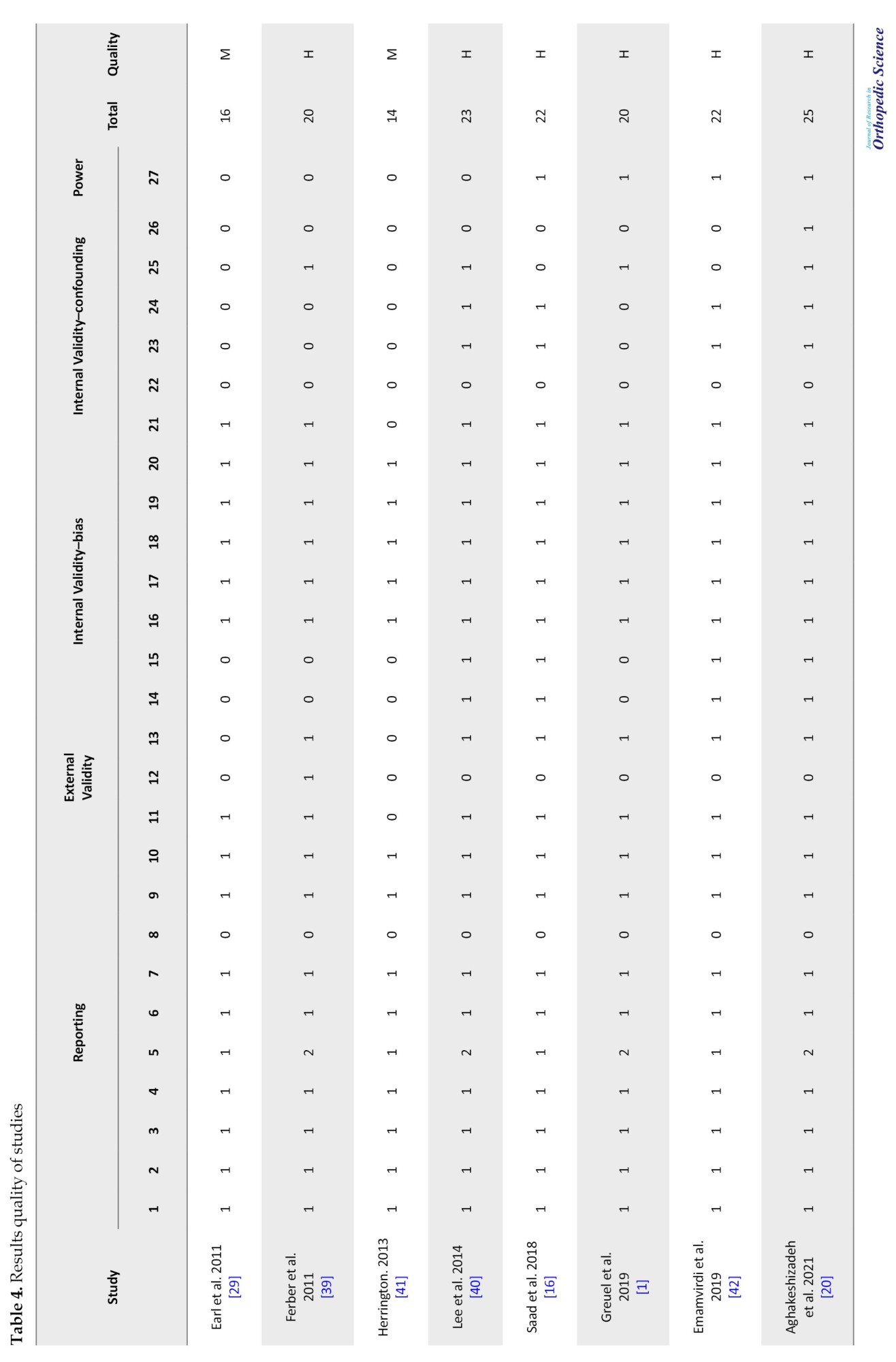
The average quality was 74% (in the range of 59% to 92%), which indicates the high quality of the articles. Of the total of included articles, 75% of articles (6 articles) were of high quality [1, 16, 20, 39, 40, 42] and 25% of articles (2 articles) were of medium quality [29, 41]. The strengths of the included articles are related to reporting and internal validity- bias. In item 8 of reporting, all articles had a significant weakness. Other weaknesses of the included articles were related to external validity (item 12) and internal validity-confounding (items 22 and 26). In addition, power (item 27) was reported in only 4 articles [1, 16, 20, 42].
Outcomes measurement
Active interventions
Exercise
In total, 4 articles investigated the effect of hip strengthening exercises on DKV, of which 3 articles had high quality [16, 39, 40] and 1 article had moderate quality [29]. Three articles investigated the effect of 8 weeks of proximal strengthening exercises on DKV [16, 29, 40]. One article reported after 8 weeks of proximal exercise, no significant effect was observed in reducing knee abduction range of motion during running; however, the knee abduction moment was decreased [29]. In contrast, 2 articles reported that the DKV angle decreased after 8 weeks of hip strengthening exercises [16, 40]. In addition, 1 article reported no significant difference in the reduction of the DKV angle after 3 weeks of hip strengthening exercises [39].
Exercise combining with movement retraining
In total, 2 articles investigated the effect of exercises and feedback on DKV, both of which had high quality [20, 42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. The protocol of movement retraining was as follows. The patients were taught to keep the pelvis at a symmetrical level during the exercises and to avoid adduction and internal rotation of the hip. Verbal feedback was provided early in the training sessions, but the feedback was repeated if the patient did not maintain the correct position during training. Feedback was removed over time to encourage self-correction [20, 42] function, strength, and kinematics in males and females with PFP. The results of 2 articles showed that the DKV angle decreased after 6 weeks.
Passive interventions
Strap and brace
In total, 2 articles investigated the effect of PowersTM and strap of the hip on DKV which 1 article had high quality [1] and 1 article had moderate quality [41]. Greuel et al. (2019) reported that the PowersTM brace had no significant effect despite the reduction in the knee adduction angle; however, the adduction moment increased significantly [1]. In contrast, Herrington (2013) reported that the strap significantly reduced the DKV angle [41]. Nevertheless, both articles examined the immediate effect of the strap [41] and PowersTM [1].
4. Discussion
This systematic review provided an overview of the potential effect of active and passive proximal interventions on DKV in PFP patients. In summary, the 8 articles were included [1, 16, 29, 39-41], of which 4 articles were related to proximal strengthening exercises [16, 29, 39, 40], 2 articles to the combination of exercises with movement retraining [20, 42] function, strength, and kinematics in males and females with PFP, and 2 articles to the use of strap and brace [1, 41]. In the following section, we will discuss the mechanism of proximal interventions.
Sichanowski et al. [2007] and Ireland et al. (2003) reported that lower extremity kinematics may be altered due to hip muscle weakness [43, 44]. In terms of biomechanics, the moment arm of the gluteus medius muscle is longer than other lower extremity muscles and controls the frontal plane movement [45]. The hip muscle weakness, especially the abductor and external rotator muscles causes DKV because hip abductors cannot control hip adduction with eccentric contraction [42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. The theoretical basis for proximal strengthening in the treatment of PFP is that hip weakness causes poor dynamic control of the lower extremities and increases PFJ stress [29]. Overall, conflicting results on the effectiveness of hip strengthening on DKV have been reported. For example, in active interventions, Ferber et al. (2011) reported that PFP patients showed a 32.69% improvement in hip abductor strength after 3 weeks of proximal strengthening exercises [39]. They report that the increase in muscle strength in this short period is largely attributed to changes in neural adaptation [39]. However, despite the decrease in the DKV angle, no statistically significant difference was observed. In contrast, Lee et al. (2014) reported that dynamic Q angle decreased after 8 weeks of proximal strengthening exercises [40]. Therefore, the period of Ferber et al. protocol to be effective was short [39]. In this regard, interventions with a period of 12 weeks or more will be more effective than interventions that are less than 12 weeks [46].
Neamatallah et al. (2020) showed that the kinetic and kinematic variables of the hip and knee related to the development of DKV are influenced by gluteal muscle strength and electromyography activity [47]. The DKV is mainly controlled by the gluteus maximus and gluteus medius muscles [48]. The action of the gluteus maximus is to extension and external rotation of the hip, while the gluteus medius is primarily a hip abductor [49]. In total, both muscles coordinately produce a force to prevent DKV [47]. In this regard, Bolgla et al. (2008) showed that the normal strength of the hip abductor and external rotator prevents the hip internal rotation [50]. Proximal strengthening exercises alone may not be sufficient to change movement patterns [20]. Sahrmann (2017) argued that exercise programs focusing on correcting abnormal movement patterns are effective in treating overuse injuries [51]. In this regard, the results of recent studies show that the combination of proximal strengthening exercises with movement retraining may be a promising approach to improve the clinical symptoms of PFP patients [20, 42, 52].
Aghakashizadeh et al. (2020) showed that hip strengthening exercises combined with movement retraining increase hip abductor muscle strength and decrease DKV [20]. In addition, Emamvirdi et al. (2019) reported that valgus control exercises significantly reduce pain and DKV [42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. Feedback can be with internal or external focus [20]. Internal focus requires the individual to focus on the movement patterns, while external focus provides indication related to the environment or movement outcome [20, 42] function, strength, and kinematics in males and females with PFP. In a systematic review, Lankhorst et al. (2012) reported that using external focus compared to internal focus led to the promotion of motor function and motor technique [28]. As a result, providing feedback to subjects during movements can help them to be movements aware and focus on the space between the knees and compensatory movements. This approach can encourage patients to control hip and knee movements by changing the neuromuscular control of the gluteal muscles, especially the gluteus medius as the most important stabilizers of the hip in the frontal and transverse planes [20]. External focus facilitates motor learning by using unconscious or automatic processes [20, 42] function, strength, and kinematics in males and females with PFP. The benefits of neuromuscular exercises for the treatment of overuse injuries are time-consuming and become apparent after 6 weeks [41]. Therefore, clinicians are looking for methods to immediately improve the lower extremity alignment and reduce the PFJ stress [41]. Passive interventions are relatively inexpensive and can be used during sports and recreational activities [1]. The aim of hip brace and tape is to reduce the adduction and internal rotation of the hip in PFP patients [[1, 53]. Greuel et al. (2019) showed that after the application of a PowersTM brace in PFP patients, the hip external rotation increased significantly during running and single-leg squats. The increase in hip external rotation with the PowersTM brace ranged from 3.5° to 6.4° [1]. Although pain was significantly reduced with large effect sizes, biomechanical changes were with small to moderate effect sizes. A hip brace increases hip external rotation and reduces hip adduction; Therefore, DKV decreases and ultimately leads to a decrease in PFJ stress [1, 53]. In this regard, Herrington (2013) reported that after using the strap, pain and DKV decreased [41]. Also, Greuel et al. (2019) showed that the PowersTM brace led to an increase in the knee adduction moment during running and single-leg squats [1]. Therefore, hip correction in the transverse plane leads to decreased pain and DKV angle [1].
5. Conclusion
Active and passive proximal interventions are effective in reducing pain and DKV angle in PFP patients. Compared to passive interventions, active exercises require multi-joint movements that stimulate proprioception and facilitate muscle recruitment patterns. As a result, it should be emphasized that passive interventions are not recommended as an independent treatment and it is better combined with exercise therapy. Therefore, PFP rehabilitation and preventive programs should be a combination of active and passive interventions.
Study limitations
This study faced some limitations. Firstly, the sample size was small. Secondly, the statistical population of some articles was only men or women. Thirdly, the intervention period was short and the long-term effectiveness was not determined. Next, in some articles, two-dimensional motion analysis was used for kinematic assessment, which has relatively low accuracy compared to three-dimensional motion analysis. It is recommended that future studies investigate the effect of passive and active proximal interventions in both genders, have a longer follow-up period, and examine a three-dimensional motion analysis system as it increases kinematic accuracy.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors have equally contributed to the design and conduction of this study.
Conflict of interest
The authors declared no conflict of interest.
References
Patellofemoral pain (PFP) describes pain around or behind the patella [1, 2]. The key symptom of PFP is worsening pain during the patellofemoral joint (PFJ) loading [3, 4]. The PFJ loading increases in activities that require knee flexion [5, 6, 7]. PFP includes 37% of knee injuries [8]. The prevalence of PFP is reported at 22.7% in the general population and 35.7% among athletes [9, 10]. The prevalence of PFP in male and female populations is 15.5% and 29.2%, respectively [11]. Despite the high prevalence, the gold standard treatment for PFP has been unclear and 70% of patients report symptoms of recurrence after rehabilitation [12, 13]. Meanwhile, 74% of PFP patients have restrictions in daily activities, work, and sports participation [14]. Also, 31% of physical therapists advise patients to prevent sports activities when experiencing PFP [15]. In addition, 45% of subjects with a history of PFP may be at risk of developing patellofemoral osteoarthritis in the future [16]. However, the etiology of PFP remains unknown and has been considered an interaction between biomechanical, anatomical, and psychological factors [17].
In the biomechanical field, one of the main hypotheses accepted in the etiology of PFP is the increase in PFJ stress [18]. Overall, PFJ mechanics are influenced by proximal and distal mechanics [19]. PFP patients show faulty PFJ mechanics and proximal and distal poor dynamic control [20]. Changes in lower extremity mechanics can increase the PFJ stress and lead to the PFP occurrence [6, 21]. Dynamic knee valgus (DKV) is one of the faulty lower limb movement patterns that can increase PFJ stress [21-23]. DKV is defined as a combination of adduction and internal rotation of the hip, knee abduction, internal rotation, and abduction of the tibia and foot pronation. Ahmadi et al. reported that a normal DKV angle should be in the range of 5 to 12 for women and 1 to 9 for men [24]. Consequently, if the subjects have DKV angles beyond this range, it has a harmful outcome to the PFJ and the anterior cruciate ligament [25]. Overall, Herrington (2014) reported that PFP patients have higher DKV angles compared to healthy controls, which, if not corrected, may lead to increased PFJ stress [21]. Waiteman et al. (2018) reported that knee valgus and high knee abduction moment cause patella external tracking and the PFJ contact area increases in the external area and causes the PFJ cartilage destruction [26]. In this regard, Powers (2010) believes that DKV in the frontal plane should be prevented because it leads to unequal stress distribution in the PFJ and contributes to the etiology or exacerbation of PFP symptoms [27].
In a systematic review of the latest PFP research, Lankhorst et al. (2012) argued that multimodal treatment protocols, in addition to the quadriceps muscle, consider the segmental around the PFJ [28]. Proximal disorders have received extensive attention during the past decade [14]. Muscle weakness and faulty kinematics of the hip and trunk in the frontal plane may contribute to the increase of DKV and subsequently to the PFP occurrence [29]. Overall, adduction and internal rotation of the hip lead to medial knee displacement, which causes tibia abduction and foot pronation, resulting in DKV [6, 29]; therefore, poor hip control leads to patellar external tracking, high PFJ stress, and subsequent PFJ cartilage damage [20, 30]. Accordingly, clinicians have focused on gluteal muscle weakness and poor dynamic control of the lower extremities in the assessment, treatment, and prevention of PFP.
In recent years, the role of hip stabilizers has been in the studies of subjects and rehabilitation protocols. Meanwhile, researchers at the fifth consensus of the international PFP research meeting, held in Manchester in 2015, recommended a combination of hip and knee exercises to reduce pain and improve function [12]. However, few studies have investigated the biomechanical effects of proximal-focused rehabilitation programs on the dynamic alignment of the lower extremities [29]. Lower extremity faulty biomechanics can be corrected with active interventions, such as exercise programs and movement retraining, or with passive interventions, such as brace and tape [1]. Publishing sufficient details of active and passive proximal interventions will enable physiotherapists to make better decisions in designing a comprehensive protocol [12]. Therefore, the aim of the systematic review is to the effect of active and passive proximal interventions on DKV in PFP patients. These recommendations can be utilized by athletic trainers and physical therapists to make evidence-based decisions about which exercises and passive interventions should be included in PFP rehabilitation and prevention programs.
2. Methods
Study protocols
We followed the guidelines of preferred reporting items of systematic reviews and meta-analyses (PRISMA) 2020 for reporting systematic review and meta-analysis studies [31]. Since the PRISMA statement was designed for systematic review and meta-analysis studies, we only addressed items related to review systematic [32-34]. A comprehensive search was performed in PROSPERO and Cochrane library databases to identify previous similar studies. As a result, the detailed protocol of this systematic review has not been previously published or registered.
Eligibility criteria
Table 1 summarizes the problem/population, intervention, comparison, and outcome items to define the inclusion and exclusion criteria.
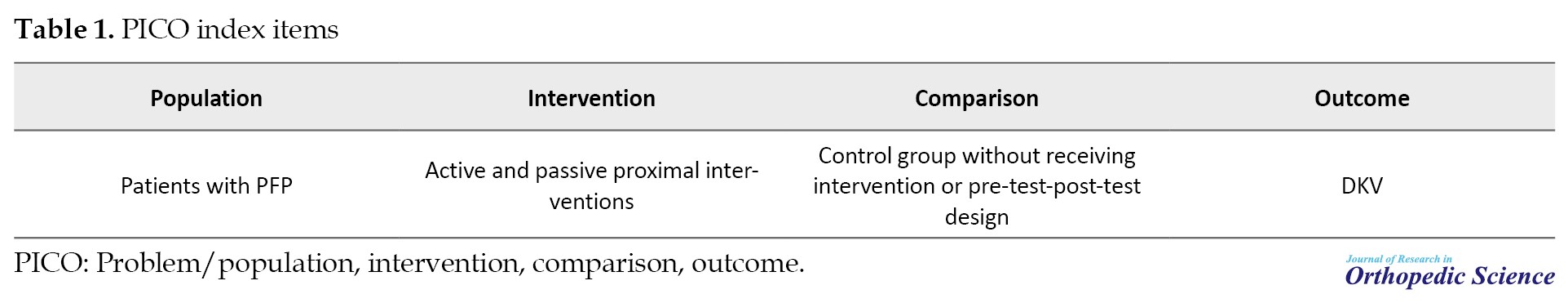
The inclusion criteria were as follows: Clinical trial articles (experimental and control or pre-test-post-test design), cohort studies, case-control, case series, active and passive proximal interventions in PFP patients, articles in English, assessment of two-dimensional or three-dimensional DKV angle, articles limited to the period of 2000 to 2022, and participants who were PFP patients without other musculoskeletal problems. There was no limitation in the PFP patient population. The exclusion criteria were as follows: Review articles, editorials, abstracts, conferences, articles related to PFJ osteoarthritis, gray literature, interventions not specifically focused on the hip, and non-English articles.
Search strategy
The search strategy was conducted independently by two rehabilitation specialists (FA & MA). Researchers used PubMed, Scopus, Web of Science, BioMed Central, Since Direct, Springer, and Cochrane Library databases for the online search. Also, Google Scholar was used as a complementary search engine. The articles were limited to the period of 2000 to 2022. To search, we used a combination of the medical subject headings (MeSH) framework and the keywords related to the study topic because many articles are listed in PubMed long before they are listed with MeSH terms [35]. The operative term “OR” was used to connect synonyms and the term “AND” was used to connect categories. According to the recommendation of the Cochrane Handbook, a manual search of the reference lists of previous systematic reviews and a citation search of the original record using the Web of Science were conducted [36]. Table 2 demonstrates the keywords used in the databases.
Study selection
The screening process of articles was conducted by two reviewers (FA & MA) independently in three stages. First, all the identified articles were saved in the reference software of Mendeley management. Articles were listed alphabetically and duplicate articles were removed by the software from the library. Then, according to the checklist prepared from the include and exclude criteria, the title and abstract of the articles were screened. Third, the full text of the articles that did not provide sufficient information from the title and abstract were reviewed.
Data extraction
Two reviewers (FA & MA) independently extracted the data using a predetermined extraction form that included the following items: Demographic information (name of the author, year of the publication, purpose, task, sample size); patients’ characteristics (statistical population, including general people or athletes with PFP); type of interventions (hip strengthening exercises, hip movement retraining, brace and tape of the hip); period (duration of protocol execution); motion analysis (two-dimensional or three-dimensional); outcome measurement (DKV angle assessment); results (the effect of interventions on DKV).
Quality assessment
Two reviewers (FA & MA) independently assessed the quality of articles using the Downs and Black checklist. A systematic review reported proper re-test ability (r=0.88), interrater reliability (r=0.75), and high internal consistency (KR-20=0.54) for the Downs and Black checklist [37]. Reporting, internal validity, external validity, and confounding internal validity are items of the Downs and Black checklist. The Downs and Black checklist consists of 27 items. Items 1 to 10 are related to reporting, 11 to 13 are external validity, 14 to 20 include internal validity, 21 to 26 are confounding internal validity, and 27 is power. The scoring of each item was considered 0 (no), 1 (yes). Items 4 and 5 were scored as 0 (no), 1 (somewhat), and 2 (yes) [38]. According to the previous study, the quality of articles was classified into three categories: High (≥70%), medium (40-69%), and low (<40%) [38].
3. Results
Study selection
The search in the electronic databases identified a total of 1098 articles from 2000 and 2022; however, 148 duplicate articles were removed from the library by the software. In total, 950 articles remained, of which 123 were gray literature, 164 abstracts, and conferences, 327 non-English language articles, 113 were related to osteoarthritis, and 215 articles did not assess the effect of proximal interventions on DKV and were excluded. Finally, 8 articles that met the eligibility criteria were selected for the systematic review [1, 16, 20, 29, 39-42]. Figure 1 shows the PRISMA diagram.
Study characteristics
Table 3 shows the summary of the demographic characteristics of the 8 included articles.
A total of 4 articles assessed the effect of proximal strengthening exercises [16, 29, 39, 40], 2 articles examined the effect of strengthening exercises combined with movement retraining [20, 42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of valgus control instruction (VCI), and 2 articles investigated the effect of brace and strap-on DKV [1, 41]. Overall, 285 patients with PFP and 10 healthy subjects participated in the studies. In active interventions, 4 articles used two-dimensional motion analysis [39, 40] and 2 articles used three-dimensional motion analysis [16, 29]. In passive interventions, 1 article used two-dimensional motion analysis [41] and 1 article used three-dimensional motion analysis [1].
Quality assessment
Table 4 shows the quality of the included articles.
The average quality was 74% (in the range of 59% to 92%), which indicates the high quality of the articles. Of the total of included articles, 75% of articles (6 articles) were of high quality [1, 16, 20, 39, 40, 42] and 25% of articles (2 articles) were of medium quality [29, 41]. The strengths of the included articles are related to reporting and internal validity- bias. In item 8 of reporting, all articles had a significant weakness. Other weaknesses of the included articles were related to external validity (item 12) and internal validity-confounding (items 22 and 26). In addition, power (item 27) was reported in only 4 articles [1, 16, 20, 42].
Outcomes measurement
Active interventions
Exercise
In total, 4 articles investigated the effect of hip strengthening exercises on DKV, of which 3 articles had high quality [16, 39, 40] and 1 article had moderate quality [29]. Three articles investigated the effect of 8 weeks of proximal strengthening exercises on DKV [16, 29, 40]. One article reported after 8 weeks of proximal exercise, no significant effect was observed in reducing knee abduction range of motion during running; however, the knee abduction moment was decreased [29]. In contrast, 2 articles reported that the DKV angle decreased after 8 weeks of hip strengthening exercises [16, 40]. In addition, 1 article reported no significant difference in the reduction of the DKV angle after 3 weeks of hip strengthening exercises [39].
Exercise combining with movement retraining
In total, 2 articles investigated the effect of exercises and feedback on DKV, both of which had high quality [20, 42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. The protocol of movement retraining was as follows. The patients were taught to keep the pelvis at a symmetrical level during the exercises and to avoid adduction and internal rotation of the hip. Verbal feedback was provided early in the training sessions, but the feedback was repeated if the patient did not maintain the correct position during training. Feedback was removed over time to encourage self-correction [20, 42] function, strength, and kinematics in males and females with PFP. The results of 2 articles showed that the DKV angle decreased after 6 weeks.
Passive interventions
Strap and brace
In total, 2 articles investigated the effect of PowersTM and strap of the hip on DKV which 1 article had high quality [1] and 1 article had moderate quality [41]. Greuel et al. (2019) reported that the PowersTM brace had no significant effect despite the reduction in the knee adduction angle; however, the adduction moment increased significantly [1]. In contrast, Herrington (2013) reported that the strap significantly reduced the DKV angle [41]. Nevertheless, both articles examined the immediate effect of the strap [41] and PowersTM [1].
4. Discussion
This systematic review provided an overview of the potential effect of active and passive proximal interventions on DKV in PFP patients. In summary, the 8 articles were included [1, 16, 29, 39-41], of which 4 articles were related to proximal strengthening exercises [16, 29, 39, 40], 2 articles to the combination of exercises with movement retraining [20, 42] function, strength, and kinematics in males and females with PFP, and 2 articles to the use of strap and brace [1, 41]. In the following section, we will discuss the mechanism of proximal interventions.
Sichanowski et al. [2007] and Ireland et al. (2003) reported that lower extremity kinematics may be altered due to hip muscle weakness [43, 44]. In terms of biomechanics, the moment arm of the gluteus medius muscle is longer than other lower extremity muscles and controls the frontal plane movement [45]. The hip muscle weakness, especially the abductor and external rotator muscles causes DKV because hip abductors cannot control hip adduction with eccentric contraction [42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. The theoretical basis for proximal strengthening in the treatment of PFP is that hip weakness causes poor dynamic control of the lower extremities and increases PFJ stress [29]. Overall, conflicting results on the effectiveness of hip strengthening on DKV have been reported. For example, in active interventions, Ferber et al. (2011) reported that PFP patients showed a 32.69% improvement in hip abductor strength after 3 weeks of proximal strengthening exercises [39]. They report that the increase in muscle strength in this short period is largely attributed to changes in neural adaptation [39]. However, despite the decrease in the DKV angle, no statistically significant difference was observed. In contrast, Lee et al. (2014) reported that dynamic Q angle decreased after 8 weeks of proximal strengthening exercises [40]. Therefore, the period of Ferber et al. protocol to be effective was short [39]. In this regard, interventions with a period of 12 weeks or more will be more effective than interventions that are less than 12 weeks [46].
Neamatallah et al. (2020) showed that the kinetic and kinematic variables of the hip and knee related to the development of DKV are influenced by gluteal muscle strength and electromyography activity [47]. The DKV is mainly controlled by the gluteus maximus and gluteus medius muscles [48]. The action of the gluteus maximus is to extension and external rotation of the hip, while the gluteus medius is primarily a hip abductor [49]. In total, both muscles coordinately produce a force to prevent DKV [47]. In this regard, Bolgla et al. (2008) showed that the normal strength of the hip abductor and external rotator prevents the hip internal rotation [50]. Proximal strengthening exercises alone may not be sufficient to change movement patterns [20]. Sahrmann (2017) argued that exercise programs focusing on correcting abnormal movement patterns are effective in treating overuse injuries [51]. In this regard, the results of recent studies show that the combination of proximal strengthening exercises with movement retraining may be a promising approach to improve the clinical symptoms of PFP patients [20, 42, 52].
Aghakashizadeh et al. (2020) showed that hip strengthening exercises combined with movement retraining increase hip abductor muscle strength and decrease DKV [20]. In addition, Emamvirdi et al. (2019) reported that valgus control exercises significantly reduce pain and DKV [42] as well as knee valgus during weight bearing activities in females. Research on injury prevention and rehabilitation strategies has shown the positive effects of VCI. Feedback can be with internal or external focus [20]. Internal focus requires the individual to focus on the movement patterns, while external focus provides indication related to the environment or movement outcome [20, 42] function, strength, and kinematics in males and females with PFP. In a systematic review, Lankhorst et al. (2012) reported that using external focus compared to internal focus led to the promotion of motor function and motor technique [28]. As a result, providing feedback to subjects during movements can help them to be movements aware and focus on the space between the knees and compensatory movements. This approach can encourage patients to control hip and knee movements by changing the neuromuscular control of the gluteal muscles, especially the gluteus medius as the most important stabilizers of the hip in the frontal and transverse planes [20]. External focus facilitates motor learning by using unconscious or automatic processes [20, 42] function, strength, and kinematics in males and females with PFP. The benefits of neuromuscular exercises for the treatment of overuse injuries are time-consuming and become apparent after 6 weeks [41]. Therefore, clinicians are looking for methods to immediately improve the lower extremity alignment and reduce the PFJ stress [41]. Passive interventions are relatively inexpensive and can be used during sports and recreational activities [1]. The aim of hip brace and tape is to reduce the adduction and internal rotation of the hip in PFP patients [[1, 53]. Greuel et al. (2019) showed that after the application of a PowersTM brace in PFP patients, the hip external rotation increased significantly during running and single-leg squats. The increase in hip external rotation with the PowersTM brace ranged from 3.5° to 6.4° [1]. Although pain was significantly reduced with large effect sizes, biomechanical changes were with small to moderate effect sizes. A hip brace increases hip external rotation and reduces hip adduction; Therefore, DKV decreases and ultimately leads to a decrease in PFJ stress [1, 53]. In this regard, Herrington (2013) reported that after using the strap, pain and DKV decreased [41]. Also, Greuel et al. (2019) showed that the PowersTM brace led to an increase in the knee adduction moment during running and single-leg squats [1]. Therefore, hip correction in the transverse plane leads to decreased pain and DKV angle [1].
5. Conclusion
Active and passive proximal interventions are effective in reducing pain and DKV angle in PFP patients. Compared to passive interventions, active exercises require multi-joint movements that stimulate proprioception and facilitate muscle recruitment patterns. As a result, it should be emphasized that passive interventions are not recommended as an independent treatment and it is better combined with exercise therapy. Therefore, PFP rehabilitation and preventive programs should be a combination of active and passive interventions.
Study limitations
This study faced some limitations. Firstly, the sample size was small. Secondly, the statistical population of some articles was only men or women. Thirdly, the intervention period was short and the long-term effectiveness was not determined. Next, in some articles, two-dimensional motion analysis was used for kinematic assessment, which has relatively low accuracy compared to three-dimensional motion analysis. It is recommended that future studies investigate the effect of passive and active proximal interventions in both genders, have a longer follow-up period, and examine a three-dimensional motion analysis system as it increases kinematic accuracy.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors have equally contributed to the design and conduction of this study.
Conflict of interest
The authors declared no conflict of interest.
References
- Greuel H, Herrington L, Liu A, Jones RK. Influence of the Powers™ strap on pain and lower limb biomechanics in individuals with patellofemoral pain. Knee. 2019; 26(6):1210-9. [DOI:10.1016/j.knee.2019.03.005] [PMID]
- Yalfani A, Ahmadi M. Patients with patellofemoral pain exhibiting decrease vertical ground reaction force compared to healthy individuals during weight bearing tasks: A systematic reviews and meta-analysis. Iran J Public Health. 2023; 52(2):254-64. [DOI:10.18502/ijph.v52i2.11879] [PMID]
- Rathleff MS, Holden S, Krommes K, Winiarski L, Hölmich P, Salim TJ, et al. The 45-second anterior knee pain provocation test: A quick test of knee pain and sporting function in 10-14-year-old adolescents with patellofemoral pain. Phys Ther Sport. 2022; 53:28-33. [DOI:10.1016/j.ptsp.2021.11.002] [PMID]
- Yalfani A, Ahmadi MR, Gandomi F, Bigdeli N. [An investigation of the lower extremity kinematics during stair ambulation in people with patellofemoral pain syndrome: A systematic review (Persian)]. J Paramed Sci Rehabil. 2021; 9(4):115-25. [DOI:10.22038/JPSR.2021.41722.1987]
- Soares A, Lopes Ferreira C, Glaviano NR, Rabelo NDDA, Lucareli PRG. Is there a correlation between isometric muscle strength and the kinematics of the pelvis, hip and knee during functional tasks in women with patellofemoral pain? Phys Ther Sport. 2022; 57:33-9. [DOI:10.1016/j.ptsp.2022.07.003] [PMID]
- Haghighat F, Ebrahimi S, Rezaie M, Shafiee E, Shokouhyan SM, Motealleh A, et al. Trunk, pelvis, and knee kinematics during running in females with and without patellofemoral pain. Gait Posture. 2021; 89:80-85. [DOI:10.1016/j.gaitpost.2021.06.023] [PMID]
- Ahmadi M, Yalfani A. Do patellofemoral pain patients have higher loading rate compared to healthy indivalues? A systematic review and meta-analysis. Phys Treat Phys Ther. 2022; 12(1):13-22. [DOI:10.32598/ptj.12.1.442.2]
- Muniz AMS, Zeitoune G, Alvim F, Grassi GBA, Britto PAA, Nadal J. Do exist differences in kinematics and EMG of the hip and knee between male runners with and without patellofemoral pain in different running speeds? Phys Ther Sport. 2023; 59:122-9. [DOI:10.1016/j.ptsp.2022.12.006] [PMID]
- Almeida GPL, Rodrigues HLDN, Coelho BAL, Rodrigues CAS, Lima POP. Anteromedial versus posterolateral hip musculature strengthening with dose-controlled in women with patellofemoral pain: A randomized controlled trial. Phys Ther Sport. 2021; 49:149-56. [DOI:10.1016/j.ptsp.2021.02.016] [PMID]
- Briani RV, Cannon J, Ducatti MHM, Priore LBD, Botta AFB, Magalhães FH, et al. Exacerbating patellofemoral pain alters trunk and lower limb coordination patterns and hip-knee mechanics. J Biomech. 2022; 141:111215. [DOI:10.1016/j.jbiomech.2022.111215] [PMID]
- Waiteman MC, de Oliveira Silva D, Azevedo FM, Pazzinatto MF, Briani RV, Bazett-Jones DM. Women with patellofemoral pain and knee crepitus have reduced knee flexion angle during stair ascent. Phys Ther Sport. 2021; 48:60-6. [DOI:10.1016/j.ptsp.2020.12.013] [PMID]
- Topdemir E, Birinci T, Taşkıran H, Mutlu EK. The effectiveness of Kinesio taping on playing-related pain, function and muscle strength in violin players: A randomized controlled clinical trial. Phys Ther Sport. 2021; 52:121-31. [DOI:10.1016/j.ptsp.2021.08.010] [PMID]
- Alsaleh SA, Murphy NA, Miller SC, Morrissey D, Lack SD. Local neuromuscular characteristics associated with patellofemoral pain: A systematic review and meta-analysis. Clin Biomech (Bristol, Avon). 2021; 90:105509. [DOI:10.1016/j.clinbiomech.2021.105509] [PMID]
- Van Cant J, Declève P, Garnier A, Roy JS. Influence of symptom frequency and severity on hip abductor strength and endurance in individuals with patellofemoral pain. Phys Ther Sport. 2021; 49:83-9. [DOI:10.1016/j.ptsp.2021.02.001] [PMID]
- Willy RW, Hoglund LT, Glaviano NR, Bolgla LA, Bazett-Jones DM. Survey of confidence and knowledge to manage patellofemoral pain in readers versus nonreaders of the physical therapy clinical practice guideline.Phys Ther Sport. 2022; 55:218-28. [DOI:10.1016/j.ptsp.2022.04.009] [PMID]
- Saad MC, Vasconcelos RA, Mancinelli LVO, Munno MSB, Liporaci RF, Grossi DB. Is hip strengthening the best treatment option for females with patellofemoral pain? A randomized controlled trial of three different types of exercises. Braz J Phys Ther. 2018; 22(5):408-16. [DOI:10.1016/j.bjpt.2018.03.009] [PMID]
- de Albuquerque CE, Bibin F, Bussarolo JM, Dalmolin EB, Ricardo Flor Bertolini G, Nuñez SC. The influence of iliotibial tract thickness on clinical outcomes in women with patellofemoral pain. Knee. 2022; 39:319-24. [DOI:10.1016/j.knee.2022.10.007] [PMID]
- Selhorst M, Hoehn J, Degenhart T, Schmitt L, Fernandez-Fernandez A. Psychologically-informed video reduces maladaptive beliefs in adolescents with patellofemoral pain. Phys Ther Sport. 2020; 41:23-8. [DOI:10.1016/j.ptsp.2019.10.009] [PMID]
- Rathleff MS, Richter C, Brushøj C, Bencke J, Bandholm T, Hölmich P, et al. Increased medial foot loading during drop jump in subjects with patellofemoral pain. Knee Surg Sports Traumatol Arthrosc. 2014; 22(10):2301-7. [DOI:10.1007/s00167-014-2943-3] [PMID]
- Aghakeshizadeh F, Letafatkar A, Thomas AC. Internal and external focus show similar effect on the gait kinematics in patients with patellofemoral pain: A randomised controlled trial. Gait Posture. 2021; 84(1):155-61. [DOI:10.1016/j.gaitpost.2020.11.030] [PMID]
- Herrington L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee. 2014; 21(2):514-7. [DOI:10.1016/j.knee.2013.11.011] [PMID]
- Graci V, Salsich GB. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J Sci Med Sport. 2015; 18(3):343-7. [DOI:10.1016/j.jsams.2014.04.011] [PMID]
- Yalfani A, Ahmadi M, Gandomi F. The effects of 12-weeks of sensorimotor exercise on pain, strength, pelvic drop, and dynamic knee valgus in males with patellofemoral pain syndrome. Phys Treat Specif Phys Ther J. 2020; 10(3):159-68. [DOI:10.32598/ptj.10.3.442.1]
- Ahmadi M, Yalfani A, Gandomi F, Rashid K. [The effect of twelve week neurofeedback training on perceptual pain intensity, fear of pain, pelvic drop, and dynamic knee valgus index in men with patellofemoral pain syndrome: A randomized double-blind clinical trial (Persian)]. Sadra Med J. 2020; 8(2):151-64. [Link]
- Herrington L, Munro A. Drop jump landing knee valgus angle; normative data in a physically active population. PPhys Ther Sport. 2010; 11(2):56-9. [DOI:10.1016/j.ptsp.2009.11.004] [PMID]
- Waiteman MC, Briani RV, Pazzinatto MF, Ferreira AS, Ferrari D, de Oliveira Silva D, et al. Relationship between knee abduction moment with patellofemoral joint reaction force, stress and self-reported pain during stair descent in women with patellofemoral pain. Clin Biomech (Bristol, Avon). 2018; 59:110-6. [DOI:10.1016/j.clinbiomech.2018.09.012] [PMID]
- Powers CM. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J Orthop Sport Phys Ther. 2010; 40(2):42-51. [DOI:10.2519/jospt.2010.3337] [PMID]
- Lankhorst NE, Bierma-Zeinstra SM, van Middelkoop M. Risk factors for patellofemoral pain syndrome: A systematic review. J Orthop Sports Phys Ther. 2012; 42(2):81-94. [DOI:10.2519/jospt.2012.3803] [PMID]
- Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011; 39(1):154-63. [DOI:10.1177/0363546510379967] [PMID]
- Baldon Rde M, Serrão FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: A randomized clinical trial. J Orthop Sport Phys Ther. 2014; 44(4):240-51. [DOI:10.2519/jospt.2014.4940] [PMID]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021; 88:105906. [DOI:10.1016/j.ijsu.2021.105906] [PMID]
- Alingh JF, Groen BE, Van Asseldonk EHF, Geurts ACH, Weerdesteyn V. Effectiveness of rehabilitation interventions to improve paretic propulsion in individuals with stroke-A systematic review. Clin Biomech (Bristol, Avon). 2020; 71:176-88. [DOI:10.1016/j.clinbiomech.2019.10.021] [PMID]
- Ahmadi M, Yalfani A. Interlimb asymmetry of vertical ground reaction force as a risk factor for re-injury and knee oseteoarthritis following anterior cruciate ligament reconstruction: A systematic review. J Res Orthop Sci. 2022; 9(1):15-24. [DOI:10.32598/JROSJ.9.1.857.1]
- Yalfani A, Ahmadi M, Asgarpoor A. [Investigate the plantar pressure distribution in PFP patients: A systematic review (Persian)]. J Res Sport Rehabil. 2022; 9(17):73-83. [DOI:10.22084/RSR.2022.25484.1610]
- Mullally EM, Atack AC, Glaister M, Clark NC. Situations and mechanisms of non-contact knee injury in adult netball: A systematic review. Phys Ther Sport. 2021; 47:193-200. [DOI:10.1016/j.ptsp.2020.12.004] [PMID]
- Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration. http://www. cochrane-handbook. org. 2008. [DOI:10.1002/9780470712184]
- Barton CJ, Levinger P, Menz HB, Webster KE. Kinematic gait characteristics associated with patellofemoral pain syndrome : A systematic review. Gait Posture. 2009; 30(4):405-16. [DOI:10.1016/j.gaitpost.2009.07.109] [PMID]
- Sancho I, Malliaras P, Barton C, Willy RW, Morrissey D. Biomechanical alterations in individuals with Achilles tendinopathy during running and hopping: A systematic review with meta-analysis. Gait Posture. 2019; 73(1):189-201. [DOI:10.1016/j.gaitpost.2019.07.121] [PMID]
- Ferber R, Kendall KD, Farr L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011; 46(2):142-9. [DOI:10.4085/1062-6050-46.2.142] [PMID]
- Lee J, Lee H, Lee W. Effect of weight-bearing therapeutic exercise on the Q-angle and muscle activity onset times of elite athletes with patellofemoral pain syndrome: A randomized controlled trial. J Phys Ther Sci. 2014; 26(7):989-92. [DOI:10.1589/jpts.26.989] [PMID]
- Herrington L. Effect of a SERF strap on pain and knee-valgus angle during unilateral squat and step landing in patellofemoral patients. J Sport Rehabil. 2013; 22(1):27-32. [DOI:10.1123/jsr.22.1.27] [PMID]
- Emamvirdi M, Letafatkar A, Khaleghi Tazji M. The effect of valgus control instruction exercises on pain, strength, and functionality in active females with patellofemoral pain syndrome. Sports Health. 2019; 11(3):223-37. [DOI:10.1177/1941738119837622] [PMID]
- Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007; 39(8):1227-32. [DOI:10.1249/mss.0b013e3180601109] [PMID]
- Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003; 33(11):671-6. [DOI:10.2519/jospt.2003.33.11.671] [PMID]
- Lee SP, Souza RB, Powers CM. The influence of hip abductor muscle performance on dynamic postural stability in females with patellofemoral pain. Gait Posture. 2012; 36(3):425-9. [DOI:10.1016/j.gaitpost.2012.03.024] [PMID]
- Crossley KM, van Middelkoop M, Barton CJ, Culvenor AG. Rethinking patellofemoral pain: Prevention, management and long-term consequences. Best Pract Res Clin Rheumatol. 2019; 33(1):48-65. [DOI:10.1016/j.berh.2019.02.004] [PMID]
- Neamatallah Z, Herrington L, Jones R. An investigation into the role of gluteal muscle strength and EMG activity in controlling HIP and knee motion during landing tasks. Phys Ther Sport. 2020; 43:230-5. [DOI:10.1016/j.ptsp.2019.12.008] [PMID]
- Hollman JH, Ginos BE, Kozuchowski J, Vaughn AS, Krause DA, Youdas JW. Relationships between knee valgus, hip-muscle strength, and hip-muscle recruitment during a single-limb step-down. J Sport Rehabil. 2009; 18(1):104-17. [DOI:10.1123/jsr.18.1.104] [PMID]
- Neumann DA. Kinesiology of the hip: A focus on muscular actions. J Orthop Sports Phys Ther. 2010; 40(2):82-94. [DOI:10.2519/jospt.2010.3025] [PMID]
- Bolgla LA, Malone TR, Umberger BR, Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008; 38(1):12-8. [DOI:10.2519/jospt.2008.2462] [PMID]
- Sahrmann S, Azevedo DC, Dillen LV. Diagnosis and treatment of movement system impairment syndromes. Braz J Phys Ther. 2017; 21(6):391-9. [DOI:10.1016/j.bjpt.2017.08.001] [PMID]
- Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011; 45(9):691-6. [DOI:10.1136/bjsm.2009.069112] [PMID]
- Song CY, Lin JJ, Chang AH. Effects of femoral rotational taping on dynamic postural stability in female patients with patellofemoral pain. Clin J Sport Med. 2017; 27(5):438-43.[DOI:10.1097/JSM.0000000000000392] [PMID]
Type of Study: Review Paper |
Subject:
Knee surgery
Received: 2022/03/13 | Accepted: 2022/07/2 | Published: 2022/08/1
Received: 2022/03/13 | Accepted: 2022/07/2 | Published: 2022/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |