Volume 9, Issue 3 (8-2022)
JROS 2022, 9(3): 141-148 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahadavi S M, Chehrassan M, Nikouei F, Shakeri M, Moeini J, Ghandhari H. Investigating Cervical Degenerative Disc Disease: An Iranian Population-based Demographic Analysis. JROS 2022; 9 (3) :141-148
URL: http://jros.iums.ac.ir/article-1-2217-en.html
URL: http://jros.iums.ac.ir/article-1-2217-en.html
Seyyed Mani Mahadavi1 
 , Mohammadreza Chehrassan1
, Mohammadreza Chehrassan1 

 , Farshad Nikouei1
, Farshad Nikouei1 
 , Mohammadreza Shakeri1
, Mohammadreza Shakeri1 
 , Javad Moeini1
, Javad Moeini1 

 , Hasan Ghandhari1
, Hasan Ghandhari1 


 , Mohammadreza Chehrassan1
, Mohammadreza Chehrassan1 

 , Farshad Nikouei1
, Farshad Nikouei1 
 , Mohammadreza Shakeri1
, Mohammadreza Shakeri1 
 , Javad Moeini1
, Javad Moeini1 

 , Hasan Ghandhari1
, Hasan Ghandhari1 

1- Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 503 kb]
(162 Downloads)
| Abstract (HTML) (535 Views)
Full-Text: (187 Views)
1. Introduction
The spine is a complex structure consisting of muscles, vertebrae, cartilage, discs, and ligaments that are degenerated with age. The discs act as supportive mattresses for the vertebrae [1-3]. Aging and exhaustion in the body’s natural process are the main factors in depreciating degenerative conditions of the spine. In addition to aging, many factors, in addition to time, can speed up these degenerative spinal disorders, including the following items: Arthritis, osteoporosis, trauma, infection, and repeated and vigorous movements, which usually occur in people with highly physical occupations [4, 5, 6, 7].
Over time, above the age of 35, the natural fluid in the disc gradually becomes dehydrated. A soft gelatinous substance that contains a lot of water gradually dries and loses its elasticity [8, 9].
Degenerative cervical disc disease can cause radiant pain, numbness, and weakness in the shoulders, arms, and hands [7]. The most common and obvious symptoms of cervical discopathy are neck pain and stiffness. When one of these conditions puts pressure on one or more nerves, they move out of the spinal cord [10].
Epidemiological data on cervical radiculopathy and cervical disc radiculopathy are rare. Previous studies have reported an annual cervical disc incidence rate of 83.2 per 100000 and a total of 107.3 for men and 63.5 for women. [6, 11] The incidence and prevalence of this disorder is higher in men compared to women [6]. The most affected age range for cases was reported in the fourth and fifth decades [12].
2. Methods
The study population consisted of 356 cases with definite diagnoses of cervical degenerative disease that underwent surgery in Shafa yahyaeian Hospital in Tehran from 2011 to 2020 and met the inclusion criteria. After evaluating the inclusion criteria, the records of 301 patients with cervical degenerative were evaluated for demographic and radiographic findings. The patients were selected by convenience sampling method and sequentially from among the patients referred to the hospital. The inclusion criteria comprised the following items: Having neck degenerative diseases that require surgery, including cervical disc, cervical osteophytes, patients with myelopathy problems caused by cervical disc degeneration; having posterior longitudinal ligament; having cervical spinal canal stenosis; and the availability of access to demographic and radiological findings of patients. Meanwhile, the exclusion criteria were as follows: Having other cervical diseases, such as trauma; having cervical bone tumors; having congenital deformities; and a lack of access or incomplete records or radiologic records of patients.
The data were collected using a two-part checklist. The first part consisted of demographic information (age, sex, body mass index, history of cervical disc in first-degree relatives, occupation, and education level of patients). Meanwhile, the second part included radiographic findings of patients (site of spine involvement, cervical lordosis, localized kyphosis determination, myelopathy, and severity of involvement). Radiographic findings were extracted and evaluated by referring to the imaging department and from the picture archiving and communication system. All the findings of patients were evaluated clinically by a spine surgery sub-specialist. The diagnosis of patients was based on the findings of magnetic resonance imaging. All findings were evaluated and classified by two independent physicians (an orthopedic surgeon and a radiologist).
Data analysis
After data collection, all patient data were analyzed using the SPSS software, version 22. Descriptive statistics, such as numbers and percentages were used to report qualitative variables. The normal distribution of quantitative variables, such as age, was assessed by the Kolmogorov-Smirnov test. Qualitative variables were analyzed by descriptive statistics (based on the number and percentage of its report). The chi-square test is used to evaluate qualitative variables. Also, P<0.05 are considered statistically significant.
3. Results
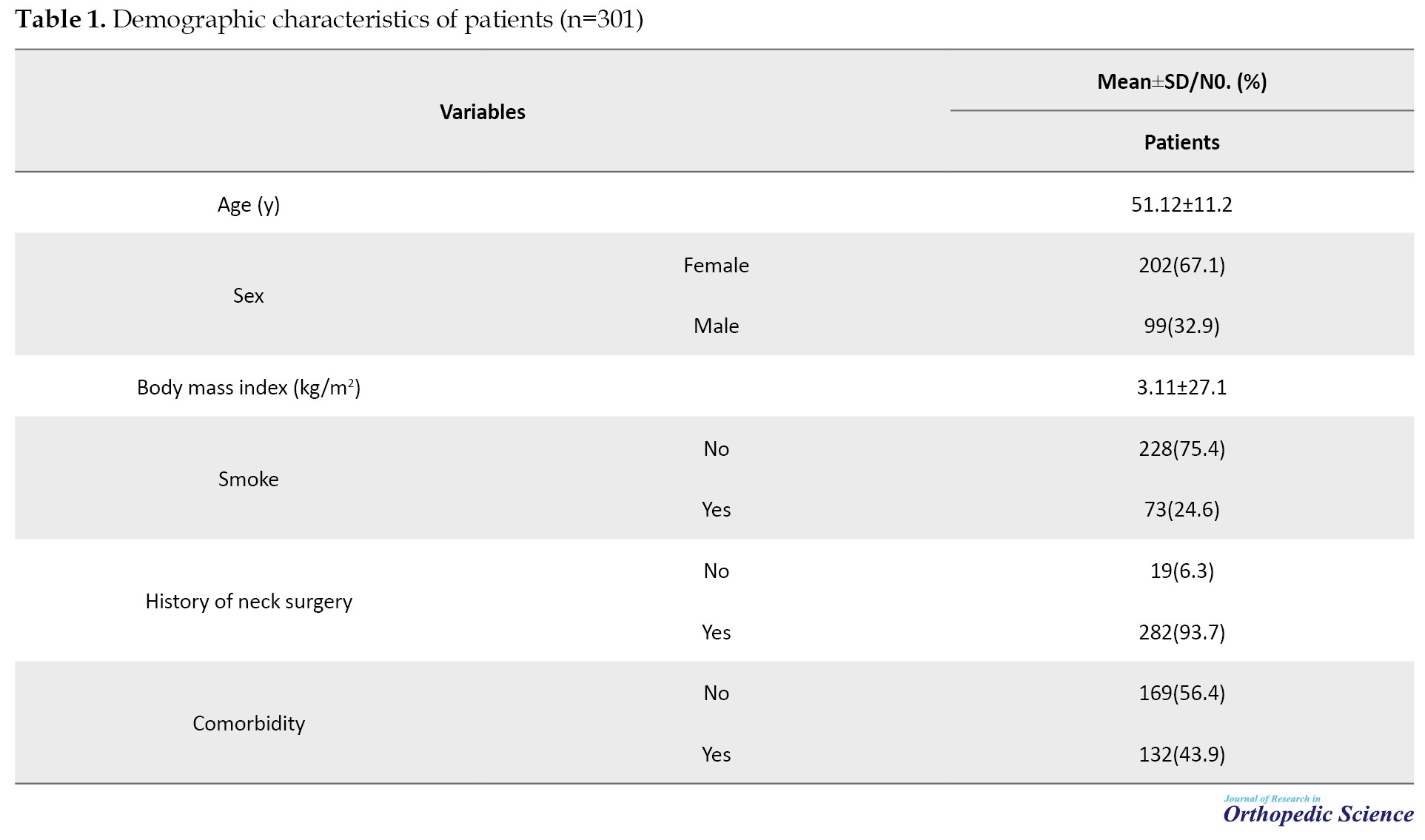
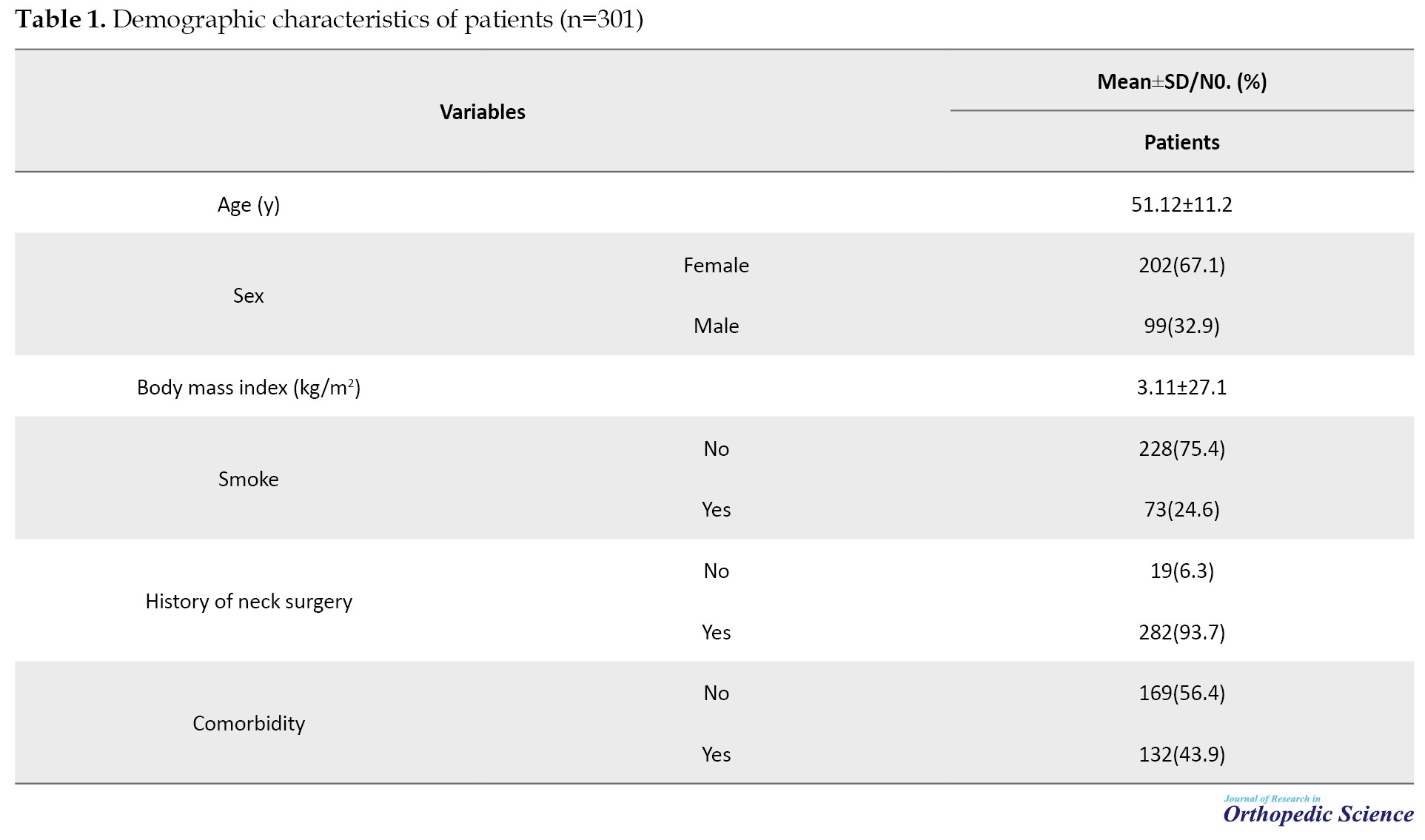
In this study, 301 patients who underwent degenerative surgery of cervical disc were reviewed. The mean age of patients was 51.12±11.2 years and ranged from 20 to 81 years. The median age of patients was 50 years. Overall, 202(67.1%) cases were female and the rest were male. Nearly, half of the patients had at least one underlying disease. The mean body mass index of patients was 3.11±27.1 kg/m2. A history of neck surgery was reported in nearly 6% of patients. A total of 24% of the patients were smokers or had a history of smoking. The demographic characteristics of patients are fully reported in Table 1.
In addition, 51.6% of patients had a higher education than a diploma. In terms of employment status and job type, more than half of the patients were employees or secretaries (Table 2).

Radiological findings
Based on the radiological findings, 147(48.8%) of patients had involvement in C5/C6 level. The frequency of involvement of C6/C7 and C4/C5 levels were 68(22.6%) and 56(18.6%), respectively. Spondylosis and disc herniation were the most common etiology of cervical pathology. Myelopathy was reported in 38% of cases. In terms of severity of the disease, the majority of patients were mild or moderate type (Table 3).

4. Discussion
Cervical degenerative disease is one of the most common causes of referring to orthopedic centers and they impose a heavy burden on health systematics. With increasing age, the chance of occurrence of this disorder increases significantly. In addition to direct costs, this disease imposes heavy costs on the health system by absenteeism in government and administrative centers. The recognition of demographic characteristics and radiological findings of this disorder is important, considering the aging of our population, and can help health policymakers. Given the importance of the issue, this study was designed to evaluate demographic and radiological findings in patients with degenerative cervical disease. The findings showed that the mean age of the patients was 51 years and more than half of the patients were less than 60 years, which indicates that the age range of these patients has declined. This study showed that patients have a high risk of developing the disease in most age groups; however, due to the nature of the disease in the fifth and sixth decades of life, the frequency of the disease increases significantly more. Nearly two-thirds of the patients were women, suggesting the prevalence of the disease was higher in women. The higher prevalence of this disease in women than men can be justified due to osteoporosis, as well as the role of hormones and the faster rate of bone loss in women than men. Nearly half of the patients had at least one underlying disease. The mean body mass index was 27.1 kg/m2 and more than half of the patients had body mass index higher than normal. More than 60 of the cases were overweight or obese. One in four patients had a smoking or history of smoking. The majority of patients had high school education and nearly half of the patients had academic education. The frequency of the disease was higher in employed people than in unemployed patients. Among the employed people, the frequency of the disease was much higher among individuals employed in administrative centers using computer systems. In other words, jobs and the use of computer systems are significantly associated with increased cervical disc. Radiologic findings showed that in more than half of patients C5, C6, and C7 levels were the most common levels of involvement for the cervical disc. In terms of etiology, spondylosis, cervical disc, or both was the most common cause of cervical disc disease and the patient’s need for surgery. The majority of patients had moderate and mild disease, which is consistent with the results of studies in this field [11-36]. In 2021, Tao et al. analyzed epidemiological and radiological findings in 1581 patients with cervical disc, the frequency of the disease was higher in women than men. The mean age of the patients was nearly 42 years. According to the findings of this study, more than half of the patients had mild to moderate degeneration. In our study, the rate of severe degeneration was slightly higher than in this study. Based on the results of this study, the highest level of involvement was C5/C6 and the lowest affected level was C2/C3 which confirmed the results of our study [37]. Radhakrishnan et al. investigated epidemiological characteristics of cervical radiculopathy in 561 patients, the mean age of patients was 47.6 years. The previous history of lumbar radiculopathy was present in 41%. C6 and C7 nerve roots were the most common levels of involvement that were in line with the results of our study. In 68.4% of patients, the cervical disc was related to spondylosis, disc, or both, which confirmed the results of our study. Pain recurrence occurred in 31.7% of patients and 26% underwent surgery for cervical disc radiculopathy. [11] In another study, Shimizu et al. looked at the prevalence and predictive factors of cervical disc disease in 121 patients with adult spinal deformities, showing an average age of 55.3, and matched the results of our study. In their study, they reported the average body mass index of patients to be close to 24.5 kg/m2, which was lower than the average body mass index in our study, which can be justified due to differences in the population under study as well as differences in patients’ lifestyles in the two studies [38]. In our study, the average body mass index was higher and the frequency of people with higher weight was higher in our study. Our results showed that the frequency of women with cervical disc disease was higher than men. In the study, 35 of the 41 patients were asymptomatic or had myelopathy. Cervical disc disease was more noticeable at C4 and 5 levels, which is in line with the results of our study.
5. Conclusion
The results of this study showed that cervical disc herniation frequency was higher in females especially in the fifth and sixth decades of life than in males. Based on radiologic findings, C5 and C6 were the most common levels of involvement. The frequency of cervical disc herniation in higher education and also employees was higher than in other professions. Prospective and extensive studies with appropriate control groups are recommended for the more accurate evaluation of these results for policy-making in the health sector.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants followed the ethical standards of the institutional and or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethic Committe of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.305). Meanwhile, there is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and study design, acquisition, data analysis and creation of new software used in the work: Seyyed Mani Mahdavi, Javad Moeini; Manuscript writing: Farshad Nikouei and Mohammadreza Shakeri; Investigating work integrity and data validation: Hasan Ghandhari; Revising and finalizing the manuscript: Mohammadreza Chehrassan and Mohammadreza Shakeri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank that he agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
The spine is a complex structure consisting of muscles, vertebrae, cartilage, discs, and ligaments that are degenerated with age. The discs act as supportive mattresses for the vertebrae [1-3]. Aging and exhaustion in the body’s natural process are the main factors in depreciating degenerative conditions of the spine. In addition to aging, many factors, in addition to time, can speed up these degenerative spinal disorders, including the following items: Arthritis, osteoporosis, trauma, infection, and repeated and vigorous movements, which usually occur in people with highly physical occupations [4, 5, 6, 7].
Over time, above the age of 35, the natural fluid in the disc gradually becomes dehydrated. A soft gelatinous substance that contains a lot of water gradually dries and loses its elasticity [8, 9].
Degenerative cervical disc disease can cause radiant pain, numbness, and weakness in the shoulders, arms, and hands [7]. The most common and obvious symptoms of cervical discopathy are neck pain and stiffness. When one of these conditions puts pressure on one or more nerves, they move out of the spinal cord [10].
Epidemiological data on cervical radiculopathy and cervical disc radiculopathy are rare. Previous studies have reported an annual cervical disc incidence rate of 83.2 per 100000 and a total of 107.3 for men and 63.5 for women. [6, 11] The incidence and prevalence of this disorder is higher in men compared to women [6]. The most affected age range for cases was reported in the fourth and fifth decades [12].
2. Methods
The study population consisted of 356 cases with definite diagnoses of cervical degenerative disease that underwent surgery in Shafa yahyaeian Hospital in Tehran from 2011 to 2020 and met the inclusion criteria. After evaluating the inclusion criteria, the records of 301 patients with cervical degenerative were evaluated for demographic and radiographic findings. The patients were selected by convenience sampling method and sequentially from among the patients referred to the hospital. The inclusion criteria comprised the following items: Having neck degenerative diseases that require surgery, including cervical disc, cervical osteophytes, patients with myelopathy problems caused by cervical disc degeneration; having posterior longitudinal ligament; having cervical spinal canal stenosis; and the availability of access to demographic and radiological findings of patients. Meanwhile, the exclusion criteria were as follows: Having other cervical diseases, such as trauma; having cervical bone tumors; having congenital deformities; and a lack of access or incomplete records or radiologic records of patients.
The data were collected using a two-part checklist. The first part consisted of demographic information (age, sex, body mass index, history of cervical disc in first-degree relatives, occupation, and education level of patients). Meanwhile, the second part included radiographic findings of patients (site of spine involvement, cervical lordosis, localized kyphosis determination, myelopathy, and severity of involvement). Radiographic findings were extracted and evaluated by referring to the imaging department and from the picture archiving and communication system. All the findings of patients were evaluated clinically by a spine surgery sub-specialist. The diagnosis of patients was based on the findings of magnetic resonance imaging. All findings were evaluated and classified by two independent physicians (an orthopedic surgeon and a radiologist).
Data analysis
After data collection, all patient data were analyzed using the SPSS software, version 22. Descriptive statistics, such as numbers and percentages were used to report qualitative variables. The normal distribution of quantitative variables, such as age, was assessed by the Kolmogorov-Smirnov test. Qualitative variables were analyzed by descriptive statistics (based on the number and percentage of its report). The chi-square test is used to evaluate qualitative variables. Also, P<0.05 are considered statistically significant.
3. Results
In this study, 301 patients who underwent degenerative surgery of cervical disc were reviewed. The mean age of patients was 51.12±11.2 years and ranged from 20 to 81 years. The median age of patients was 50 years. Overall, 202(67.1%) cases were female and the rest were male. Nearly, half of the patients had at least one underlying disease. The mean body mass index of patients was 3.11±27.1 kg/m2. A history of neck surgery was reported in nearly 6% of patients. A total of 24% of the patients were smokers or had a history of smoking. The demographic characteristics of patients are fully reported in Table 1.
In addition, 51.6% of patients had a higher education than a diploma. In terms of employment status and job type, more than half of the patients were employees or secretaries (Table 2).

Radiological findings
Based on the radiological findings, 147(48.8%) of patients had involvement in C5/C6 level. The frequency of involvement of C6/C7 and C4/C5 levels were 68(22.6%) and 56(18.6%), respectively. Spondylosis and disc herniation were the most common etiology of cervical pathology. Myelopathy was reported in 38% of cases. In terms of severity of the disease, the majority of patients were mild or moderate type (Table 3).

4. Discussion
Cervical degenerative disease is one of the most common causes of referring to orthopedic centers and they impose a heavy burden on health systematics. With increasing age, the chance of occurrence of this disorder increases significantly. In addition to direct costs, this disease imposes heavy costs on the health system by absenteeism in government and administrative centers. The recognition of demographic characteristics and radiological findings of this disorder is important, considering the aging of our population, and can help health policymakers. Given the importance of the issue, this study was designed to evaluate demographic and radiological findings in patients with degenerative cervical disease. The findings showed that the mean age of the patients was 51 years and more than half of the patients were less than 60 years, which indicates that the age range of these patients has declined. This study showed that patients have a high risk of developing the disease in most age groups; however, due to the nature of the disease in the fifth and sixth decades of life, the frequency of the disease increases significantly more. Nearly two-thirds of the patients were women, suggesting the prevalence of the disease was higher in women. The higher prevalence of this disease in women than men can be justified due to osteoporosis, as well as the role of hormones and the faster rate of bone loss in women than men. Nearly half of the patients had at least one underlying disease. The mean body mass index was 27.1 kg/m2 and more than half of the patients had body mass index higher than normal. More than 60 of the cases were overweight or obese. One in four patients had a smoking or history of smoking. The majority of patients had high school education and nearly half of the patients had academic education. The frequency of the disease was higher in employed people than in unemployed patients. Among the employed people, the frequency of the disease was much higher among individuals employed in administrative centers using computer systems. In other words, jobs and the use of computer systems are significantly associated with increased cervical disc. Radiologic findings showed that in more than half of patients C5, C6, and C7 levels were the most common levels of involvement for the cervical disc. In terms of etiology, spondylosis, cervical disc, or both was the most common cause of cervical disc disease and the patient’s need for surgery. The majority of patients had moderate and mild disease, which is consistent with the results of studies in this field [11-36]. In 2021, Tao et al. analyzed epidemiological and radiological findings in 1581 patients with cervical disc, the frequency of the disease was higher in women than men. The mean age of the patients was nearly 42 years. According to the findings of this study, more than half of the patients had mild to moderate degeneration. In our study, the rate of severe degeneration was slightly higher than in this study. Based on the results of this study, the highest level of involvement was C5/C6 and the lowest affected level was C2/C3 which confirmed the results of our study [37]. Radhakrishnan et al. investigated epidemiological characteristics of cervical radiculopathy in 561 patients, the mean age of patients was 47.6 years. The previous history of lumbar radiculopathy was present in 41%. C6 and C7 nerve roots were the most common levels of involvement that were in line with the results of our study. In 68.4% of patients, the cervical disc was related to spondylosis, disc, or both, which confirmed the results of our study. Pain recurrence occurred in 31.7% of patients and 26% underwent surgery for cervical disc radiculopathy. [11] In another study, Shimizu et al. looked at the prevalence and predictive factors of cervical disc disease in 121 patients with adult spinal deformities, showing an average age of 55.3, and matched the results of our study. In their study, they reported the average body mass index of patients to be close to 24.5 kg/m2, which was lower than the average body mass index in our study, which can be justified due to differences in the population under study as well as differences in patients’ lifestyles in the two studies [38]. In our study, the average body mass index was higher and the frequency of people with higher weight was higher in our study. Our results showed that the frequency of women with cervical disc disease was higher than men. In the study, 35 of the 41 patients were asymptomatic or had myelopathy. Cervical disc disease was more noticeable at C4 and 5 levels, which is in line with the results of our study.
5. Conclusion
The results of this study showed that cervical disc herniation frequency was higher in females especially in the fifth and sixth decades of life than in males. Based on radiologic findings, C5 and C6 were the most common levels of involvement. The frequency of cervical disc herniation in higher education and also employees was higher than in other professions. Prospective and extensive studies with appropriate control groups are recommended for the more accurate evaluation of these results for policy-making in the health sector.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants followed the ethical standards of the institutional and or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethic Committe of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.305). Meanwhile, there is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conception and study design, acquisition, data analysis and creation of new software used in the work: Seyyed Mani Mahdavi, Javad Moeini; Manuscript writing: Farshad Nikouei and Mohammadreza Shakeri; Investigating work integrity and data validation: Hasan Ghandhari; Revising and finalizing the manuscript: Mohammadreza Chehrassan and Mohammadreza Shakeri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
We thank that he agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Rothman RH, Simeone FA. The spine. J Pediatr Orthop. 1992; 12(4):549. [DOI:10.1097/01241398-199207000-00034]
- Frost BA, Camarero-Espinosa S, Foster EJ. Materials for the spine: Anatomy, problems, and solutions. Materials. 2019; 12(2):253. [DOI:10.3390/ma12020253] [PMID]
- Zander HJ, Graham RD, Anaya CJ, Lempka SF. Anatomical and technical factors affecting the neural response to epidural spinal cord stimulation. J Neural Eng. 2020; 17(3):036019. [DOI:10.1088/1741-2552/ab8fc4] [PMID]
- Dallaway A, Kite C, Griffen C, Duncan M, Tallis J, Renshaw D, et al. Age-related degeneration of the lumbar paravertebral muscles: Systematic review and three-level meta-regression. Exp Gerontol. 2020; 133:110856. [DOI:10.1016/j.exger.2020.110856] [PMID]
- Parenteau CS, Lau EC, Campbell IC, Courtney A. Prevalence of spine degeneration diagnosis by type, age, gender, and obesity using Medicare data. Sci Rep. 2021; 11(1):5389. [DOI:10.1038/s41598-021-84724-6] [PMID]
- Schoenfeld AJ, George AA, Bader JO, Caram PM Jr. Incidence and epidemiology of cervical radiculopathy in the United States military: 2000 to 2009. J Spinal Disord Tech. 2012; 25(1):17-22. [DOI:10.1097/BSD.0b013e31820d77ea] [PMID]
- Corey DL, Comeau D. Cervical radiculopathy. Med Clin North Am. 2014; 98(4):791-9, xii. [DOI:10.1016/j.mcna.2014.04.001] [PMID]
- Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934; 211(5):210-5. [DOI:10.1056/NEJM193408022110506]
- Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine. 2003; 28(17):2030-5. [DOI:10.1097/01.BRS.0000083325.27357.39] [PMID]
- Woods BI, Hilibrand AS. Cervical radiculopathy: Epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech. 2015; 28(5):E251-9. [DOI:10.1097/BSD.0000000000000284] [PMID]
- Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT. Epidemiology of cervical radiculopathy: A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994; 117 ( Pt 2):325-35. [DOI:10.1093/brain/117.2.325] [PMID]
- Jensen MV, Tüchsen F, Orhede E. Prolapsed cervical intervertebral disc in male professional drivers in Denmark, 1981-1990: A longitudinal study of hospitalizations. Spine. 1996; 21(20):2352-5. [DOI:10.1097/00007632-199610150-00009] [PMID]
- Badhiwala JH, Ahuja CS, Akbar MA, Witiw CD, Nassiri F, Furlan JC, et al. Degenerative cervical myelopathy-update and future directions. Nat Rev Neurol. 2020; 16(2):108-24. [DOI:10.1038/s41582-019-0303-0] [PMID]
- Plener J, Csiernik B, To D, da Silva-Oolup S, Hofkirchner C, Cox J, et al. Conservative management of cervical radiculopathy: A systematic review. Clin J Pain. 2023; 39(3):138-46. [DOI:10.1097/AJP.0000000000001092] [PMID]
- Kang KC, Lee HS, Lee JH. Cervical radiculopathy focus on characteristics and differential diagnosis. Asian Spine J. 2020; 14(6):921-30. [DOI:10.31616/asj.2020.0647] [PMID]
- Marco B, Evans D, Symonds N, Peolsson A, Coppieters MW, Jull G, et al. Determining the level of cervical radiculopathy: Agreement between visual inspection of pain drawings and magnetic resonance imaging. Pain Pract. 2023; 23(1):32-40. [DOI:10.1111/papr.13147] [PMID]
- Bono CM, Ghiselli G, Gilbert TJ, Kreiner DS, Reitman C, Summers JT, et al. An evidence-based clinical guideline for the diagnosis and treatment of cervical radiculopathy from degenerative disorders. Spine J. 2011; 11(1):64-72. [DOI:10.1016/j.spinee.2010.10.023] [PMID]
- Kuijper B, Tans JT, Schimsheimer RJ, van der Kallen BF, Beelen A, Nollet F, et al. Degenerative cervical radiculopathy: Diagnosis and conservative treatment. A review. Eur J Neurol. 2009; 16(1):15-20. [DOI:10.1111/j.1468-1331.2008.02365.x] [PMID]
- Shu W, Zhu H, Liu R, Li Y, Du T, Ni B, et al. Posterior percutaneous endoscopic cervical foraminotomy and discectomy for degenerative cervical radiculopathy using intraoperative O-arm imaging. Wideochir Inne Tech Maloinwazyjne. 2019; 14(4):551-9. [DOI:10.5114/wiitm.2019.88660] [PMID]
- Fakhoury J, Dowling TJ. Cervical degenerative disc disease. 2020. [PMID]
- Wang Z, Luo G, Yu H, Zhao H, Li T, Yang H, et al. Comparison of discover cervical disc arthroplasty and anterior cervical discectomy and fusion for the treatment of cervical degenerative disc diseases: A meta-analysis of prospective, randomized controlled trials. Front Surg. 2023; 10:1124423. [DOI:10.3389/fsurg.2023.1124423] [PMID]
- Shedid D, Benzel EC. Cervical spondylosis anatomy: Pathophysiology and biomechanics. Neurosurgery. 2007; 60(1 Supp1 1):S7-13. [DOI:10.1227/01.NEU.0000215430.86569.C4] [PMID]
- Williams AL, Murtagh FR, Rothman SL, Sze GK. Lumbar disc nomenclature: Version 2.0. AJNR Am J Neuroradiol. 2014; 35(11):2029. [DOI:10.3174/ajnr.A4108] [PMID]
- Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Journal of Physical Rehabilitation and Sports Medicine. 2021; 21(3):197-221. [Link]
- Battié MC, Videman T. Lumbar disc degeneration: Epidemiology and genetics.J Bone Joint Surg Am. 2006; 88 (Suppl 2):3-9. [DOI:10.2106/JBJS.E.01313] [PMID]
- Gore DR, Carrera GF, Glaeser ST. Smoking and degenerative changes of the cervical spine: A roentgenographic study. Spine J. 2006; 6(5):557-60. [DOI:10.1016/j.spinee.2005.12.003] [PMID]
- Okada E, Matsumoto M, Ichihara D, Chiba K, Toyama Y, Fujiwara H, et al. Aging of the cervical spine in healthy volunteers: A 10-year longitudinal magnetic resonance imaging study. Spine. 2009; 34(7):706-12. [DOI:10.1097/BRS.0b013e31819c2003] [PMID]
- Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg. 1990; 72(8):1178-84. [DOI:10.2106/00004623-199072080-00008]
- Lehto IJ, Tertti MO, Komu ME, Paajanen HE, Tuominen J, Kormano MJ. Age-related MRI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology.1994; 36(1):49-53. [DOI:10.1007/BF00599196] [PMID]
- Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998; 80-B(1):19-24. [DOI:10.1302/0301-620X.80B1.0800019]
- Lawrence JS. Disc degeneration. Its frequency and relationship to symptoms. Ann Rheum Dis. 1969; 28(2):121-38. [DOI:10.1136/ard.28.2.121] [PMID]
- Nilsson N. The prevalence of cervicogenic headache in a random population sample of 20-59 year olds. Spine. 1995; 20(17):1884-8. [DOI:10.1097/00007632-199509000-00008] [PMID]
- Holmes A, Wang C, Han ZH, Dang GT. The range and nature of flexion-extension motion in the cervical spine. Spine. 1994; 19(22):2505-10. [DOI:10.1097/00007632-199411001-00003] [PMID]
- Montgomery DM, Brower RS. Cervical spondylotic myelopathy: Clinical syndrome and natural history. Orthop Clin North Am. 1992; 23(3):487-93. [DOI:10.1016/S0030-5898(20)31760-0] [PMID]
- Iyer S, Kim HJ. Cervical radiculopathy. Curr Rev Musculoskelet Med. 2016; 9(3):272-80. [DOI:10.1007/s12178-016-9349-4] [PMID]
- Ulbrich EJ, Schraner C, Boesch C, Hodler J, Busato A, Anderson SE, et al. Normative MR cervical spinal canal dimensions. Radiology. 2014; 271(1):172-82. [DOI:10.1148/radiol.13120370] [PMID]
- Tao Y, Galbusera F, Niemeyer F, Samartzis D, Vogele D, Wilke HJ. Radiographic cervical spine degenerative findings: A study on a large population from age 18 to 97 years. Eur Spine J. 2021; 30(2):431-43. [DOI:10.1007/s00586-020-06615-0] [PMID]
- Shimizu T, Lehman RA Jr, Pongmanee S, Alex Sielatycki J, Leung E, Riew KD, et al. Prevalence and predictive factors of concurrent cervical spinal cord compression in adult spinal deformity. Spine. 2019; 44(15):1049-56. [DOI:10.1097/BRS.0000000000003007] [PMID]
Type of Study: Research Article |
Subject:
Spine surgery
Received: 2022/03/17 | Accepted: 2022/04/22 | Published: 2022/08/1
Received: 2022/03/17 | Accepted: 2022/04/22 | Published: 2022/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |