Volume 9, Issue 3 (8-2022)
JROS 2022, 9(3): 165-172 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Amirlou P, Aminian A. Comparing Cephalomedullary Nailing and Dynamic Hip Screw Methods Among type A2 Intertrochanteric Fractures. JROS 2022; 9 (3) :165-172
URL: http://jros.iums.ac.ir/article-1-2219-en.html
URL: http://jros.iums.ac.ir/article-1-2219-en.html
1- Student Research Committee, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Intertrochanteric fractures, Dynamic hip screw, Cephalomedullary nailing, Harris hip score
Full-Text [PDF 549 kb]
(257 Downloads)
| Abstract (HTML) (998 Views)
Full-Text: (347 Views)
1. Introduction
Hip fractures, a condition with serious negative impacts on health status and quality of life are estimated to affect 4.5 million people annually worldwide by the year 2050 [1-3]. Intertrochanteric fracture is responsible for about 42% of hip fractures and directly imposes a cost of US $2.63 billion to the healthcare system in the United States [4]. This subgroup of hip fracture is further classified into three types, namely A1, A2, and A3 based on AO foundation/orthopedic trauma association classification, which type A2 forms about 49% of intertrochanteric fracture cases [5].
The primary management of this type of fracture includes surgical internal fixation either through a cephalomedullary nail (CMN) or a dynamic hip screw (DHS) [6]. While the use of CMN was associated with a higher risk of femoral shaft fracture as a complication of fixation surgery when compared with DHS in earlier studies, this difference was not observed in more recent studies, as the biomechanical design of the nails was improved [7]. For patients with stable intertrochanteric fractures (i.e. type A1 or A 2.1), DHS is preferred over CMN, as it presents comparable patient outcomes with a lower cost. However, in randomized controlled trials (RCT) comparing these two fixation devices, the use of a CMN showed more favorable outcome regarding the early mobility of patients in individuals with unstable intertrochanteric fractures (type A2.2 or A2.3) or with reverse obliquity (type A3). Hence, in these types of intertrochanteric fractures, the surgical fixation device of choice is CMN [8-16]. This study compares radiological and clinical outcomes of patients with type A2 intertrochanteric fractures who underwent surgery with either CMN or DHS devices.
2. Methods
This single-center retrospective cohort study was performed on adult patients with type A2 intertrochanteric fracture who were hospitalized at Shafa yahyaeian Hospital, Tehran, from 2014 to 2023. Included participants comprised all patients who were hospitalized with an intertrochanteric fracture within the defined period were screened and subjects with a definite diagnosis of type A2 intertrochanteric fracture based on hip x-ray who underwent surgical fixation with the collaboration of three hip surgeons by use of either a CMN or a DHS device based on recommendations of the American Academy of Orthopedic Surgeons [17], within the first 48 h of admission and had at least one follow-up x-ray with an interval of three month or more with their index surgery. The patients with non-A2-type intertrochanteric fractures, non-optimal fixation surgery leading to reoperation, multiple fractures previous conditions with significant disability, or use of other methods and devices for fracture fixation were excluded from the study. All participants were divided based on the device used for their baseline fixation surgery into two groups of CMN and DHS.
Follow-up x-ray of each patient was evaluated in terms of the presence of the radiologic outcomes by an assigned independent orthopedic expert. Radiologic outcomes were considered in this study as the presence of non:union:, varus mal:union:, :union: failure (defined as a composite outcome of non-:union: and varus mal:union:), and femoral-medialization. We determined follow-up radiography as the last radiography of a patient documented in the hospital system and with at least a 3-month interval with the index surgery. Furthermore, all participants were followed retrospectively via a telephone interview from November 2022 to February 2023, regarding the assessment of clinical outcomes, including the incidence of pulmonary-thromboembolism or deep vein thrombosis, following the index surgery, and overall modified Harris hip score (mHHS) [18]. All telephone follow-ups had at least 5-month intervals with the index surgery for each patient. Furthermore, subjects who underwent revision surgery and the fixation device was altered to another one were excluded from the analysis of clinical outcomes.
The normality of continuous variables was assessed via the Kolmogorov-Smirnov test and the data were reported as Mean±SD in case of normal distribution, and median (interquartile ranges) for non-normally distributed variables. The categorical variables were shown as frequencies (%). We performed the independent samples t-test, or its non-parametric equivalent (Mann-Whitney U test) to compare quantitative variables between the CMN and DHS groups. The chi-square test was done to compare the incidence rate of categorical outcomes between the groups. In case of the violation of the chi-square test assumptions, the Fisher exact test or maximum likelihood ratio chi-square test was used as a substitute, based on appropriateness for variable categories. Moreover, a relative risk with a 95% confidence interval (95%) was calculated to compare the risk of incidence of categorical pre-specified radiologic outcomes between both groups. A P<0.05 was considered significant. All statistical analyses were performed via the SPSS software, version 22 for Windows (SPSS Inc. Chicago, Illinois).
3. Result
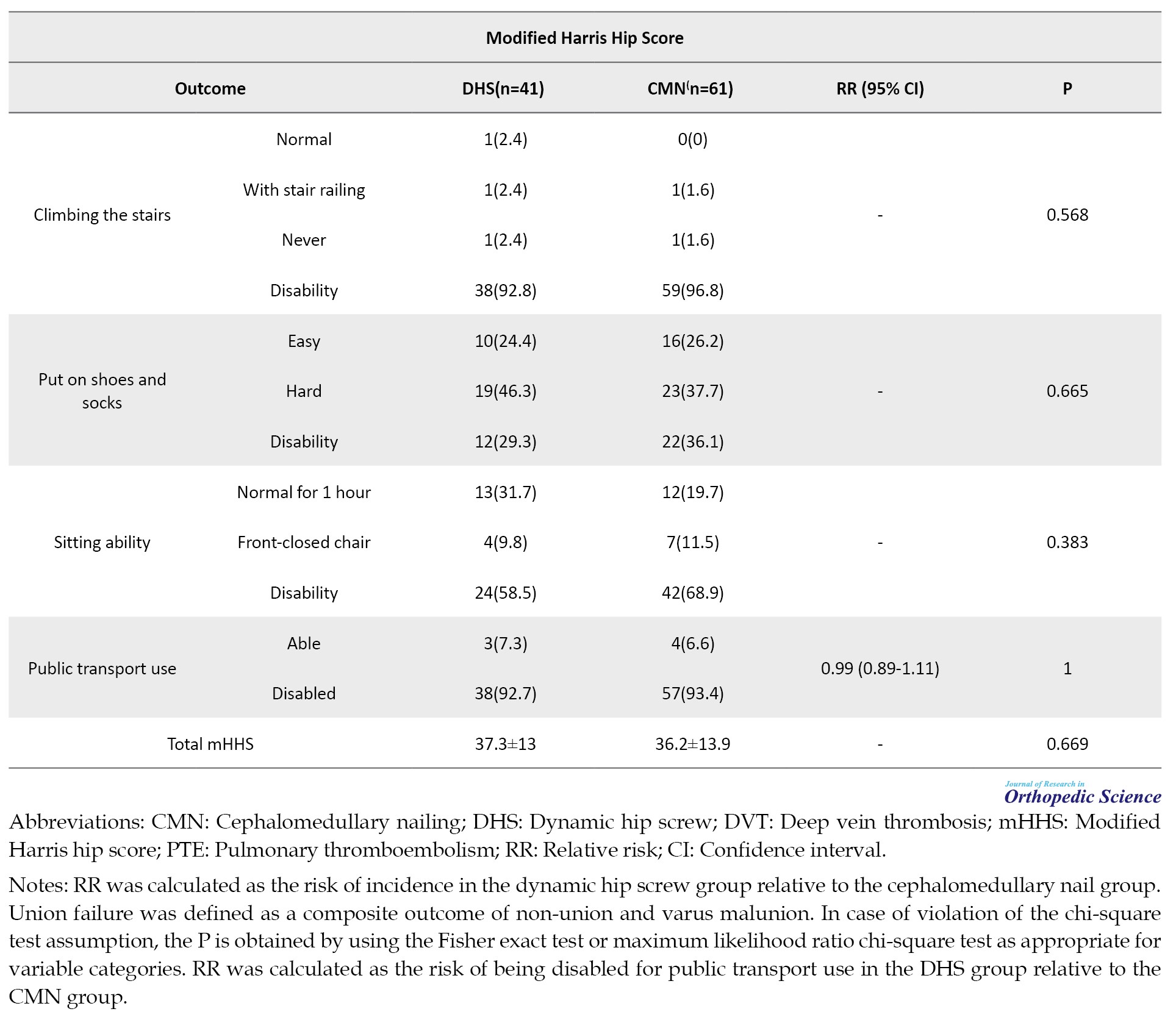
A total number of 713 hospitalized patients with intertrochanteric fracture between 2014 and 2023 were screened in terms of the eligibility criteria and after the exclusion of 519 patients (365 patients with non-A2-type intertrochanteric fracture, 5 patients with non-optimal surgery, 12 patients with multiple fractures, 93 patients with prior significant disability, and 44 patients with a fixation method other than CMN or DHS), a final number of 194 patients formed the study population, with 119 patients in CMN group and 75 patients with DHS group (Figure 1). The median (interquartile range) age of patients had no significant difference between both groups (73 [60-79] vs 70 [62-78] in CMN and DHS groups, respectively; P=0.61). Other demographic and baseline characteristics of patients are demonstrated in Table 1.
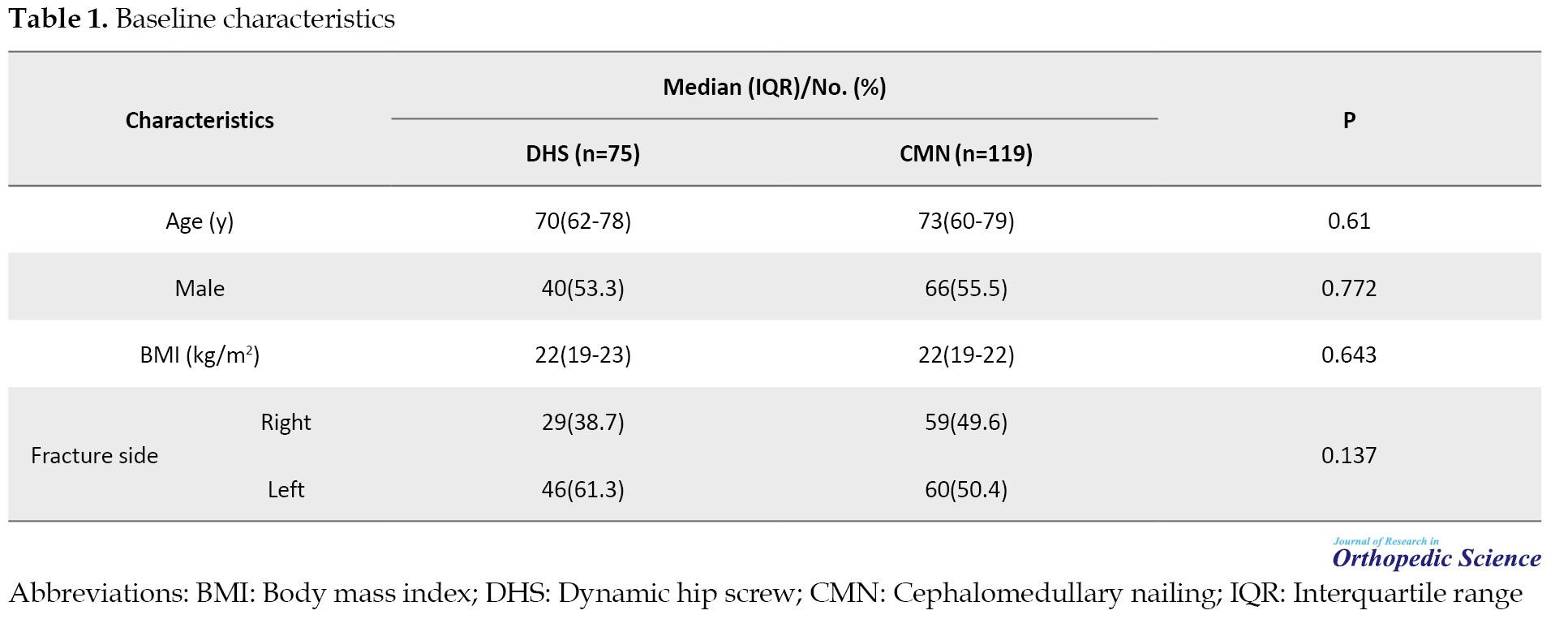
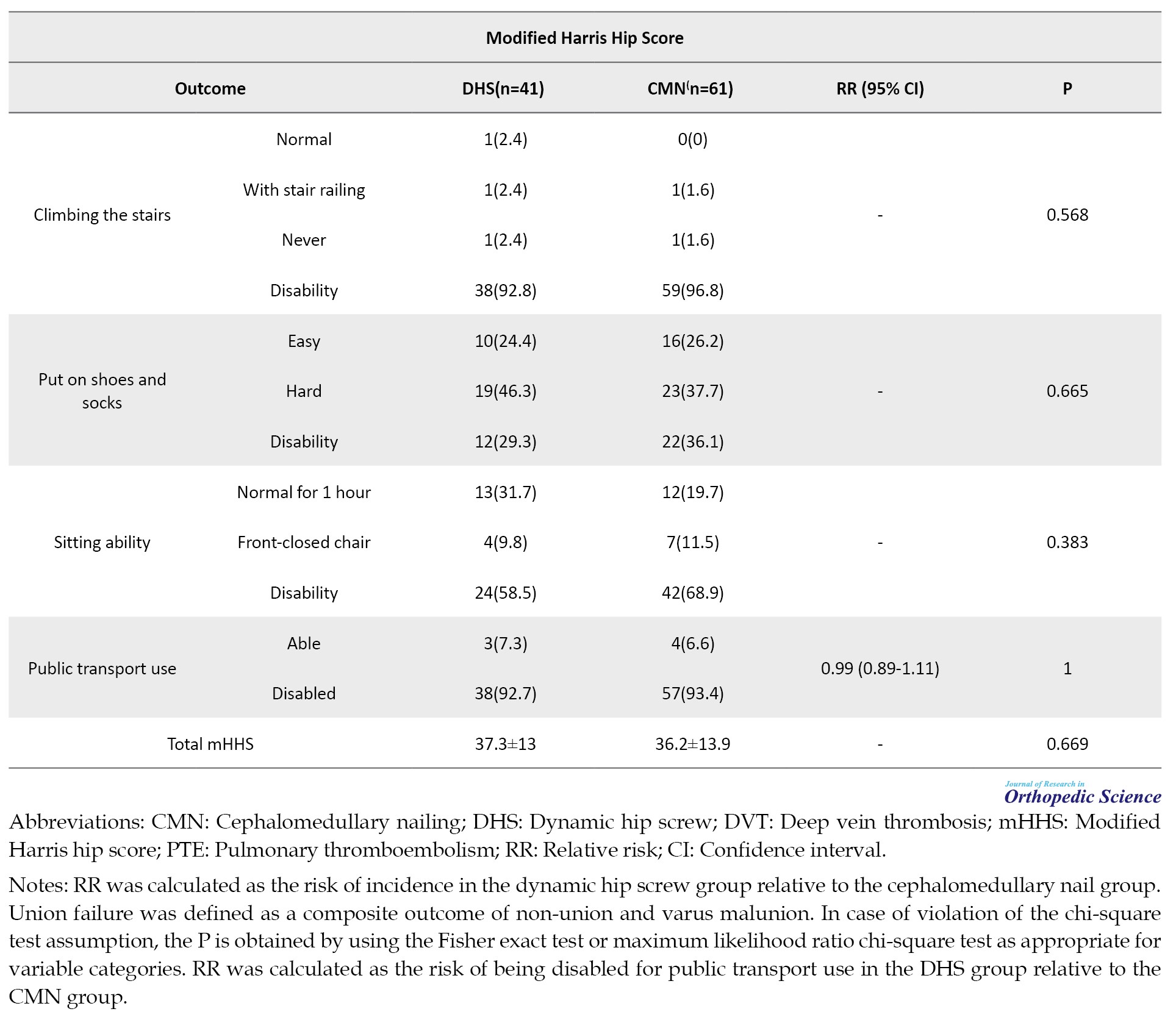
The total number of participants who were available for phone call follow-up of clinical outcomes was 102 patients, including 61 patients in CMN and 41 patients in DHS groups. During the follow-up period of patients, one deep vein thrombosis case in each group (1.6% in CMN and 2.4% in DHS groups respectively, relative risk [RR]=1.49 [95% CI, 0.9%, 23.12%]; P=1) and one pulmonary-thromboembolism in each group (1.6% in CMN and 2.4% in DHS groups, respectively; RR=1.49 [95% CI, 0.9%, 23.12%]; P=1) occurred. The mean of total mHHS in patients in the DHS group (37.3 [13]) was slightly higher compared to subjects in the CMN group (36.2 [13.9]). Nevertheless, this difference was not statistically significant (P=0.669). Regarding the items of the mHHS system, the walking distance status of patients after the surgery showed a significant difference between the two groups (P=0.043) (Table 2).

The median time interval between index fixation surgery and follow-up radiography was comparable between the two groups (4 [3-7] months in CMN compared to 4 [3-11] months in DHS groups; P=0.535). Comparing radiologic outcomes, the risk of incidence of non:union: (27 patients [22.7%] vs 14 patients [18.7%] in CMN and DHS groups, respectively; RR=0.82 [95% CI, 0.46%, 1.46%]; P=0.504), :union:-failure (59 patients [49.6%] vs 29 patients [38.7%] in CMN and DHS groups, respectively; RR=0.78 [95% CI, 0.56%, 1.09%]; P=0.137) did not have a significant difference between the groups. However, patients who had undergone DHS surgery as the fixation method of their fracture had a meaningfully lower risk for incidence of varus mal:union: compared to those with CMN device (45 patients [37.8%] vs 15 patients [20%] in CMN and DHS groups, respectively; RR=0.53 [95% CI, 0.32%, 0.88%]; P=0.009). Both methods showed comparable results regarding the median of femoral medialization percentage (0 [0-0] percent in CMN and 0 [0-0] percent in DHS groups; P=0.684) in the follow-up radiographs of patients (Table 2).
4. Discussion
This retrospective cohort compared CMN and DHS, as two main surgical fixation devices for type A2 intertrochanteric fractures by using both radiologic and patient-level outcomes. The use of radiologic outcomes provides an objective measurement for comparison of the two methods.
Based on previous RCTs, comparing these two devices for fixation operation based on follow-up radiographs, both devices have shown strictly comparable results. In our study, the incidence risk of non:union: and :union: failure did not have a significant difference between both groups. However, the incidence rate of these outcomes was considerably higher compared to those reported in prior RCTs assessed the radiologic findings [10-14]. A contributing factor in the differences between the incidence rates is related to different study designs, as this was a retrospective study with defined single follow-up radiography, while RCTs have utilized multiple radiographs through the study follow-up prospectively. Furthermore, we found a meaningful difference in the incidence of varus mal:union:. In previous trials, only one study reported the incidence of varus mal:union:, which had no significant difference between CMN and hip screw strategies [14]. Despite multiple prospective radiographic assessments of patients through the follow-up period, the incidence of varus mal:union: was still lower than the rate in our study. Moreover, the population of the current study was only limited to patients with type A2 intertrochanteric fractures, unlike previous RCTs that assessed the overall population of patients with intertrochanteric fractures of any type. Based on a pilot RCT, the use of DHS as the fixation device was associated with a significantly higher incidence of femoral-medialization [19]. However, while the percentage of femoral medialization has not been reported in this study, our findings did not show a significant difference in the percentage of femoral medialization between the groups.
Most prospective RCTs comparing fixation devices in intertrochanteric fracture have suggested better results in favor of nailing-based strategies regarding early mobilization and walking ability of patients [9, 10, 12, 13, 15]. Our findings regarding to patient-level outcomes, as measured by mHHS, demonstrated no meaningful difference between both groups. Consistent with this finding, a pilot RCT comparing DHS and proximal femoral nails showed no significant difference in the total Harris hip score at the end of 1-year follow-up [19]. Another prospective study on 39 patients with stable and unstable intertrochanteric fractures who had undergone surgical fixation with proximal femoral nail reported an average of 89 for Harris hip score at the end of 1-year follow-up [20]. However, these two recent studies have used the original version of the Harris hip score, which contains a maximum of more than 9 points in the total score compared to the modified version used in this study. Furthermore, these differences between the total scores could be a result of different study designs and sample sizes. However, a network meta-analysis on 36 RCTs revealed that among various fixation devices used for intertrochanteric fractures, proximal femoral nail anti-rotating has had significantly more favorable results regarding to total Harris hip score compared to other fixation devices [21].
5. Conclusion
Despite better outcomes of DHS regarding lower incidence of varus mal:union: and walking distance status, other outcomes did not show any significant difference between groups. However, more prospective studies with multiple systematic follow-ups and radiographies are needed to robust these findings.
Study limitations
This study was faced with several limitations. First, this study used a single follow-up radiography for the assessment of radiologic outcomes, leading to a variable time interval between the index fixation surgeries and follow-up radiographs. As a result, this difference in recovery time may affect the incidence of radiologic findings. Second, mHHS was evaluated retrospectively and with different recovery times after the index surgery. Next, an assessment of mHHS was performed via phone call follow-up, and a considerable loss to follow-up, which can affect our findings regarding clinical outcomes and mHHS. On the other hand, in our study, we did not separate patients with A2 intertrochanteric fractures into stable or unstable ones which could affect the results of our study. Hence, further studies are needed to better compare between two groups.
Ethical Considerations
Compliance with ethical guidelines ...
The Ethics Committee of Iran University of Medical Sciences approved the study (Code: IR.IUMS.1400.407), and the study was performed following the ethical principles of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and review & editing: Amir Aminian; Methodology, investigation, manuscript writing and data analysis: Parsa Amirlou; Data collection: Parsa Amirlou and Amir Aminian.
Conflict of interest
The authors declared no conflict of interest.
References
Hip fractures, a condition with serious negative impacts on health status and quality of life are estimated to affect 4.5 million people annually worldwide by the year 2050 [1-3]. Intertrochanteric fracture is responsible for about 42% of hip fractures and directly imposes a cost of US $2.63 billion to the healthcare system in the United States [4]. This subgroup of hip fracture is further classified into three types, namely A1, A2, and A3 based on AO foundation/orthopedic trauma association classification, which type A2 forms about 49% of intertrochanteric fracture cases [5].
The primary management of this type of fracture includes surgical internal fixation either through a cephalomedullary nail (CMN) or a dynamic hip screw (DHS) [6]. While the use of CMN was associated with a higher risk of femoral shaft fracture as a complication of fixation surgery when compared with DHS in earlier studies, this difference was not observed in more recent studies, as the biomechanical design of the nails was improved [7]. For patients with stable intertrochanteric fractures (i.e. type A1 or A 2.1), DHS is preferred over CMN, as it presents comparable patient outcomes with a lower cost. However, in randomized controlled trials (RCT) comparing these two fixation devices, the use of a CMN showed more favorable outcome regarding the early mobility of patients in individuals with unstable intertrochanteric fractures (type A2.2 or A2.3) or with reverse obliquity (type A3). Hence, in these types of intertrochanteric fractures, the surgical fixation device of choice is CMN [8-16]. This study compares radiological and clinical outcomes of patients with type A2 intertrochanteric fractures who underwent surgery with either CMN or DHS devices.
2. Methods
This single-center retrospective cohort study was performed on adult patients with type A2 intertrochanteric fracture who were hospitalized at Shafa yahyaeian Hospital, Tehran, from 2014 to 2023. Included participants comprised all patients who were hospitalized with an intertrochanteric fracture within the defined period were screened and subjects with a definite diagnosis of type A2 intertrochanteric fracture based on hip x-ray who underwent surgical fixation with the collaboration of three hip surgeons by use of either a CMN or a DHS device based on recommendations of the American Academy of Orthopedic Surgeons [17], within the first 48 h of admission and had at least one follow-up x-ray with an interval of three month or more with their index surgery. The patients with non-A2-type intertrochanteric fractures, non-optimal fixation surgery leading to reoperation, multiple fractures previous conditions with significant disability, or use of other methods and devices for fracture fixation were excluded from the study. All participants were divided based on the device used for their baseline fixation surgery into two groups of CMN and DHS.
Follow-up x-ray of each patient was evaluated in terms of the presence of the radiologic outcomes by an assigned independent orthopedic expert. Radiologic outcomes were considered in this study as the presence of non:union:, varus mal:union:, :union: failure (defined as a composite outcome of non-:union: and varus mal:union:), and femoral-medialization. We determined follow-up radiography as the last radiography of a patient documented in the hospital system and with at least a 3-month interval with the index surgery. Furthermore, all participants were followed retrospectively via a telephone interview from November 2022 to February 2023, regarding the assessment of clinical outcomes, including the incidence of pulmonary-thromboembolism or deep vein thrombosis, following the index surgery, and overall modified Harris hip score (mHHS) [18]. All telephone follow-ups had at least 5-month intervals with the index surgery for each patient. Furthermore, subjects who underwent revision surgery and the fixation device was altered to another one were excluded from the analysis of clinical outcomes.
The normality of continuous variables was assessed via the Kolmogorov-Smirnov test and the data were reported as Mean±SD in case of normal distribution, and median (interquartile ranges) for non-normally distributed variables. The categorical variables were shown as frequencies (%). We performed the independent samples t-test, or its non-parametric equivalent (Mann-Whitney U test) to compare quantitative variables between the CMN and DHS groups. The chi-square test was done to compare the incidence rate of categorical outcomes between the groups. In case of the violation of the chi-square test assumptions, the Fisher exact test or maximum likelihood ratio chi-square test was used as a substitute, based on appropriateness for variable categories. Moreover, a relative risk with a 95% confidence interval (95%) was calculated to compare the risk of incidence of categorical pre-specified radiologic outcomes between both groups. A P<0.05 was considered significant. All statistical analyses were performed via the SPSS software, version 22 for Windows (SPSS Inc. Chicago, Illinois).
3. Result
A total number of 713 hospitalized patients with intertrochanteric fracture between 2014 and 2023 were screened in terms of the eligibility criteria and after the exclusion of 519 patients (365 patients with non-A2-type intertrochanteric fracture, 5 patients with non-optimal surgery, 12 patients with multiple fractures, 93 patients with prior significant disability, and 44 patients with a fixation method other than CMN or DHS), a final number of 194 patients formed the study population, with 119 patients in CMN group and 75 patients with DHS group (Figure 1). The median (interquartile range) age of patients had no significant difference between both groups (73 [60-79] vs 70 [62-78] in CMN and DHS groups, respectively; P=0.61). Other demographic and baseline characteristics of patients are demonstrated in Table 1.
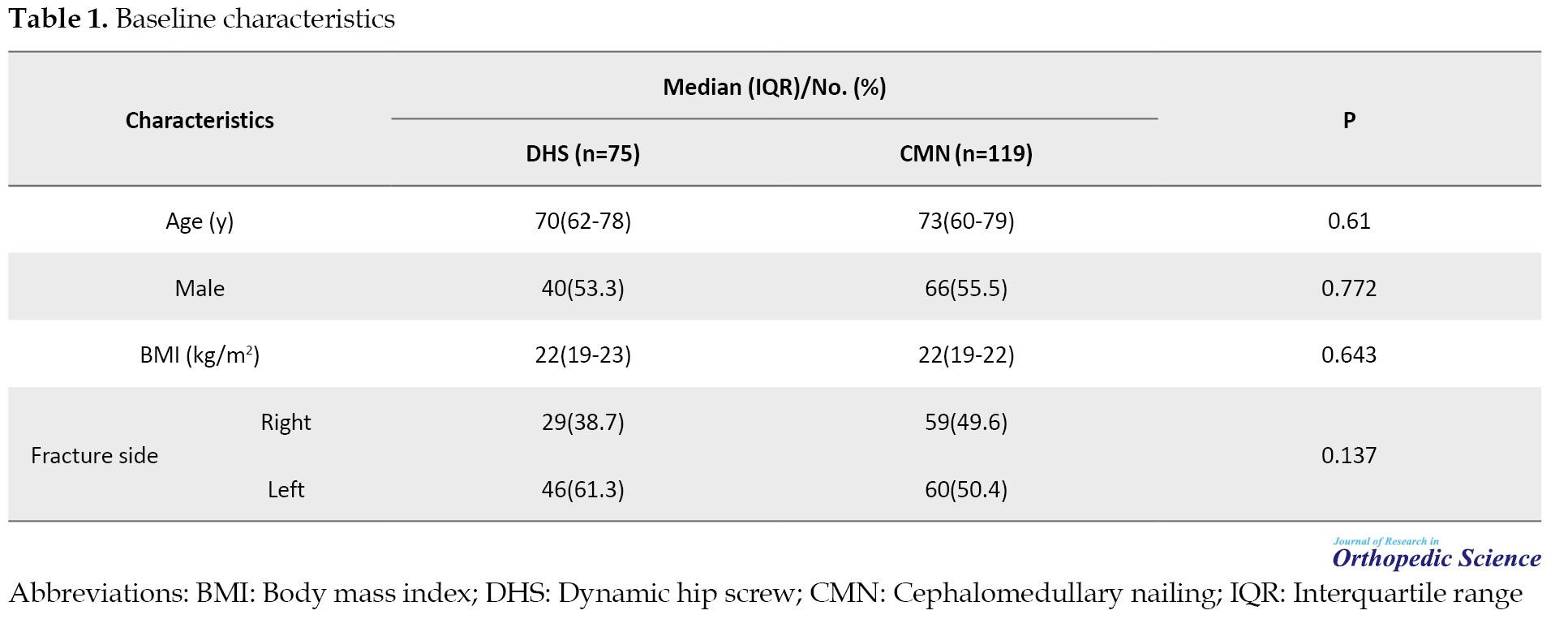
The total number of participants who were available for phone call follow-up of clinical outcomes was 102 patients, including 61 patients in CMN and 41 patients in DHS groups. During the follow-up period of patients, one deep vein thrombosis case in each group (1.6% in CMN and 2.4% in DHS groups respectively, relative risk [RR]=1.49 [95% CI, 0.9%, 23.12%]; P=1) and one pulmonary-thromboembolism in each group (1.6% in CMN and 2.4% in DHS groups, respectively; RR=1.49 [95% CI, 0.9%, 23.12%]; P=1) occurred. The mean of total mHHS in patients in the DHS group (37.3 [13]) was slightly higher compared to subjects in the CMN group (36.2 [13.9]). Nevertheless, this difference was not statistically significant (P=0.669). Regarding the items of the mHHS system, the walking distance status of patients after the surgery showed a significant difference between the two groups (P=0.043) (Table 2).

The median time interval between index fixation surgery and follow-up radiography was comparable between the two groups (4 [3-7] months in CMN compared to 4 [3-11] months in DHS groups; P=0.535). Comparing radiologic outcomes, the risk of incidence of non:union: (27 patients [22.7%] vs 14 patients [18.7%] in CMN and DHS groups, respectively; RR=0.82 [95% CI, 0.46%, 1.46%]; P=0.504), :union:-failure (59 patients [49.6%] vs 29 patients [38.7%] in CMN and DHS groups, respectively; RR=0.78 [95% CI, 0.56%, 1.09%]; P=0.137) did not have a significant difference between the groups. However, patients who had undergone DHS surgery as the fixation method of their fracture had a meaningfully lower risk for incidence of varus mal:union: compared to those with CMN device (45 patients [37.8%] vs 15 patients [20%] in CMN and DHS groups, respectively; RR=0.53 [95% CI, 0.32%, 0.88%]; P=0.009). Both methods showed comparable results regarding the median of femoral medialization percentage (0 [0-0] percent in CMN and 0 [0-0] percent in DHS groups; P=0.684) in the follow-up radiographs of patients (Table 2).
4. Discussion
This retrospective cohort compared CMN and DHS, as two main surgical fixation devices for type A2 intertrochanteric fractures by using both radiologic and patient-level outcomes. The use of radiologic outcomes provides an objective measurement for comparison of the two methods.
Based on previous RCTs, comparing these two devices for fixation operation based on follow-up radiographs, both devices have shown strictly comparable results. In our study, the incidence risk of non:union: and :union: failure did not have a significant difference between both groups. However, the incidence rate of these outcomes was considerably higher compared to those reported in prior RCTs assessed the radiologic findings [10-14]. A contributing factor in the differences between the incidence rates is related to different study designs, as this was a retrospective study with defined single follow-up radiography, while RCTs have utilized multiple radiographs through the study follow-up prospectively. Furthermore, we found a meaningful difference in the incidence of varus mal:union:. In previous trials, only one study reported the incidence of varus mal:union:, which had no significant difference between CMN and hip screw strategies [14]. Despite multiple prospective radiographic assessments of patients through the follow-up period, the incidence of varus mal:union: was still lower than the rate in our study. Moreover, the population of the current study was only limited to patients with type A2 intertrochanteric fractures, unlike previous RCTs that assessed the overall population of patients with intertrochanteric fractures of any type. Based on a pilot RCT, the use of DHS as the fixation device was associated with a significantly higher incidence of femoral-medialization [19]. However, while the percentage of femoral medialization has not been reported in this study, our findings did not show a significant difference in the percentage of femoral medialization between the groups.
Most prospective RCTs comparing fixation devices in intertrochanteric fracture have suggested better results in favor of nailing-based strategies regarding early mobilization and walking ability of patients [9, 10, 12, 13, 15]. Our findings regarding to patient-level outcomes, as measured by mHHS, demonstrated no meaningful difference between both groups. Consistent with this finding, a pilot RCT comparing DHS and proximal femoral nails showed no significant difference in the total Harris hip score at the end of 1-year follow-up [19]. Another prospective study on 39 patients with stable and unstable intertrochanteric fractures who had undergone surgical fixation with proximal femoral nail reported an average of 89 for Harris hip score at the end of 1-year follow-up [20]. However, these two recent studies have used the original version of the Harris hip score, which contains a maximum of more than 9 points in the total score compared to the modified version used in this study. Furthermore, these differences between the total scores could be a result of different study designs and sample sizes. However, a network meta-analysis on 36 RCTs revealed that among various fixation devices used for intertrochanteric fractures, proximal femoral nail anti-rotating has had significantly more favorable results regarding to total Harris hip score compared to other fixation devices [21].
5. Conclusion
Despite better outcomes of DHS regarding lower incidence of varus mal:union: and walking distance status, other outcomes did not show any significant difference between groups. However, more prospective studies with multiple systematic follow-ups and radiographies are needed to robust these findings.
Study limitations
This study was faced with several limitations. First, this study used a single follow-up radiography for the assessment of radiologic outcomes, leading to a variable time interval between the index fixation surgeries and follow-up radiographs. As a result, this difference in recovery time may affect the incidence of radiologic findings. Second, mHHS was evaluated retrospectively and with different recovery times after the index surgery. Next, an assessment of mHHS was performed via phone call follow-up, and a considerable loss to follow-up, which can affect our findings regarding clinical outcomes and mHHS. On the other hand, in our study, we did not separate patients with A2 intertrochanteric fractures into stable or unstable ones which could affect the results of our study. Hence, further studies are needed to better compare between two groups.
Ethical Considerations
Compliance with ethical guidelines ...
The Ethics Committee of Iran University of Medical Sciences approved the study (Code: IR.IUMS.1400.407), and the study was performed following the ethical principles of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and review & editing: Amir Aminian; Methodology, investigation, manuscript writing and data analysis: Parsa Amirlou; Data collection: Parsa Amirlou and Amir Aminian.
Conflict of interest
The authors declared no conflict of interest.
References
- Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: A review. Clin Interv Aging. 2018; 13:143-150. [DOI:10.2147/CIA.S150067] [PMID]
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002; 359(9319):1761-7. [DOI:10.1016/S0140-6736(02)08657-9] [PMID]
- Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997; 7(5):407-13. [DOI:10.1007/PL00004148] [PMID]
- Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture: A medicare claims database analysis. JB JS Open Access. 2019; 4(1):e0045. [DOI:10.2106/JBJS.OA.18.00045] [PMID]
- Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: Data from the Swedish fracture register. BMC Musculoskelet Disord. 2018; 19(1):369. [DOI:10.1186/s12891-018-2276-3] [PMID]
- Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017; 377(21):2053-62. [DOI:10.1056/NEJMcp1611090] [PMID]
- Bhandari M, Schemitsch E, Jönsson A, Zlowodzki M, Haidukewych GJ. Gamma nails revisited: Gamma nails versus compression hip screws in the management of intertrochanteric fractures of the hip: A meta-analysis. J Orthop Trauma. 2009; 23(6):460-4. [DOI:10.1097/BOT.0b013e318162f67f] [PMID]
- Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: Rationale, evidence, and recommendations. Bone Joint J. 2017; 99-B(1):128-33. [DOI:10.1302/0301-620X.99B1.BJJ-2016-0134.R1] [PMID]
- Little NJ, Verma V, Fernando C, Elliott DS, Khaleel A. A prospective trial comparing the Holland nail with the dynamic hip screw in the treatment of intertrochanteric fractures of the hip. J Bone Joint Surg Br. 2008; 90(8):1073-8. [DOI:10.1302/0301-620X.90B8.20825] [PMID]
- Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998; 80(5):618-30. [DOI:10.2106/00004623-199805000-00002] [PMID]
- Saudan M, Lübbeke A, Sadowski C, Riand N, Stern R, Hoffmeyer P. Pertrochanteric fractures: Is there an advantage to an intramedullary nail?: A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma. 2002; 16(6):386-93. [DOI:10.1097/00005131-200207000-00004] [PMID]
- Parker MJ, Bowers TR, Pryor GA. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: A randomised trial of 600 fractures. J Bone Joint Surg Br. 2012; 94(3):391-7. [DOI:10.1302/0301-620X.94B3.28406] [PMID]
- Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010; 38(4):1266-75. [DOI:10.1177/147323001003800408] [PMID]
- Utrilla AL, Reig JS, Muñoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: A randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005; 19(4):229-33. [DOI:10.1097/01.bot.0000151819.95075.ad] [PMID]
- Aktselis I, Kokoroghiannis C, Fragkomichalos E, Koundis G, Deligeorgis A, Daskalakis E, et al. Prospective randomised controlled trial of an intramedullary nail versus a sliding hip screw for intertrochanteric fractures of the femur. Int Orthop. 2014; 38(1):155-61. [DOI:10.1007/s00264-013-2196-7] [PMID]
- Lu Y, Uppal HS. Hip Fractures: Relevant anatomy, classification, and biomechanics of fracture and fixation.Geriatr Orthop Surg Rehabil. 2019; 10:2151459319859139. [DOI:10.1177/2151459319859139] [PMID]
- Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015; 23(2):131-7. [DOI:10.5435/JAAOS-D-14-00432] [PMID]
- Kumar P, Sen R, Aggarwal S, Agarwal S, Rajnish RK. Reliability of modified harris hip score as a tool for outcome evaluation of total hip replacements in Indian population. J Clin Orthop Trauma. 2019; 10(1):128-30. [DOI:10.1016/j.jcot.2017.11.019] [PMID]
- Chechik O, Amar E, Khashan M, Pritsch T, Drexler M, Goldstein Y, et al. Favorable radiographic outcomes using the expandable proximal femoral nail in the treatment of hip fractures - A randomized controlled trial. J Orthop. 2014; 11(2):103-9. [DOI:10.1016/j.jor.2014.04.004] [PMID]
- Paul O, Barker JU, Lane JM, Helfet DL, Lorich DG. Functional and radiographic outcomes of intertrochanteric hip fractures treated with calcar reduction, compression, and trochanteric entry nailing. J Orthop Trauma. 2012; 26(3):148-54. [DOI:10.1097/BOT.0b013e31821e3f8c] [PMID]
- Cheng YX, Sheng X. Optimal surgical methods to treat intertrochanteric fracture: A Bayesian network meta-analysis based on 36 randomized controlled trials. J Orthop Surg Res. 2020; 15(1):402. [DOI:10.1186/s13018-020-01943-9] [PMID]
Type of Study: Research Article |
Subject:
Hip surgery
Received: 2022/06/2 | Accepted: 2022/07/1 | Published: 2022/08/1
Received: 2022/06/2 | Accepted: 2022/07/1 | Published: 2022/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |