Volume 9, Issue 3 (8-2022)
JROS 2022, 9(3): 135-140 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najdmazhar F, Shariatzadeh H, Hamadiyan H, Motevallian Sajadi S M, Jafari B, Torab R. Epidemiologic Characteristics, Presentation and Management Outcomes of Glomus Tumor: A Retrospective Study. JROS 2022; 9 (3) :135-140
URL: http://jros.iums.ac.ir/article-1-2222-en.html
URL: http://jros.iums.ac.ir/article-1-2222-en.html
Farid Najdmazhar1 

 , Hooman Shariatzadeh1
, Hooman Shariatzadeh1 

 , Hosein Hamadiyan2
, Hosein Hamadiyan2 

 , Seyed Morteza Motevallian Sajadi2
, Seyed Morteza Motevallian Sajadi2 

 , Behnam Jafari2
, Behnam Jafari2 

 , Reza Torab1
, Reza Torab1 




 , Hooman Shariatzadeh1
, Hooman Shariatzadeh1 

 , Hosein Hamadiyan2
, Hosein Hamadiyan2 

 , Seyed Morteza Motevallian Sajadi2
, Seyed Morteza Motevallian Sajadi2 

 , Behnam Jafari2
, Behnam Jafari2 

 , Reza Torab1
, Reza Torab1 


1- Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 486 kb]
(323 Downloads)
| Abstract (HTML) (1134 Views)
Full-Text: (558 Views)
1. Introduction
Glomus bodies are normal structures composed of glomus cells, smooth muscle cells, and vasculature highly concentrated in the digits and are involved in regulating skin temperature [1]. Glomus tumors are benign perivascular neoplasms in the distal limbs, particularly in the nail bed [2, 3].
Patients generally present with long periods of pain. Clinically, a glomus tumor is a discoloration of the nail plate into bluish or pinkish red, with a classical triad of severe pain, localized tenderness, and cold sensitivity. Classic symptoms might not be present in all patients, necessitating differential diagnosis of other tumors. Diagnosis is generally based on clinical tests, including Love’s pin test, Hildreth’s test, and trans-illumination test, combined with imaging studies, such as magnetic resonance imaging (MRI), ultrasonography, and radiography [4]. However, mismanagement and delayed diagnosis are common [2].
When the glomus tumor is diagnosed, complete surgical excision is required to improve symptoms. Various surgical approaches could be selected depending on the anatomical location of the lesion. Incomplete excision can cause local recurrence; thus, a recurrence rate of up to 15% has been reported following the surgical excision [2, 4].
In this study, we described epidemiologic characteristics, clinical presentation, diagnosis management, post-operative complications, and recurrence of glomus tumors.
2. Methods
Patients who underwent surgical excision at Shafa Yahyaeian Hospital, Tehran, Iran between 2009 and 2021, were retrospectively reviewed. Inclusion criteria were histologic confirmation of glomus tumor diagnosis and a minimum follow-up of 12 months. Patients presented with a recurrence and lost to follow-up were excluded from the study. Of 66 patients with glomus tumors, 50 cases met the study criteria and were included in the analysis.
A senior hand surgeon managed all patients at the same orthopedic center. Digital nerve blocks were used for all patients with hand involvement. The translingual approach was used for patients with subungual involvement. The nail plate was removed using fine artery forceps in a standard fashion and carefully lifted off to prevent damage to the nail bed. After exposing the tumor, a longitudinal incision was made, and the tumor was completely excised under magnification. For tumors located in the volar pulp, the lesion was excised through a direct incision made over the volar pulp skin. Post-operatively, limb elevation was advised to prevent edema and swelling. Lesions in less frequent locations were excised as appropriate. Stitches were removed ten days after the operation.
Demographic characteristics, including age, sex, affected digit, dominant side, and clinical characteristics such as symptoms, pain duration, Hildreth’s sign, and tumor characteristics (size, location, and post-operative complications such as deformity, pain, numbness, oncologic outcomes), were collected. The largest diameter of lesion in gross histopathology was regarded as the tumor size. The detection of recurrence relied on clinical suspicion (recurrent pain), plain radiography, and MRI studies if necessary.
Statistics
Data were analyzed using SPSS software, version 22. Qualitative data were presented as numbers and percentages. Quantitative data were presented as Mean±SD. The mean values between the two groups were compared by an independent t-test or Mann–Whitney U test. A P≤0.05 was considered statistically significant.
3. Results
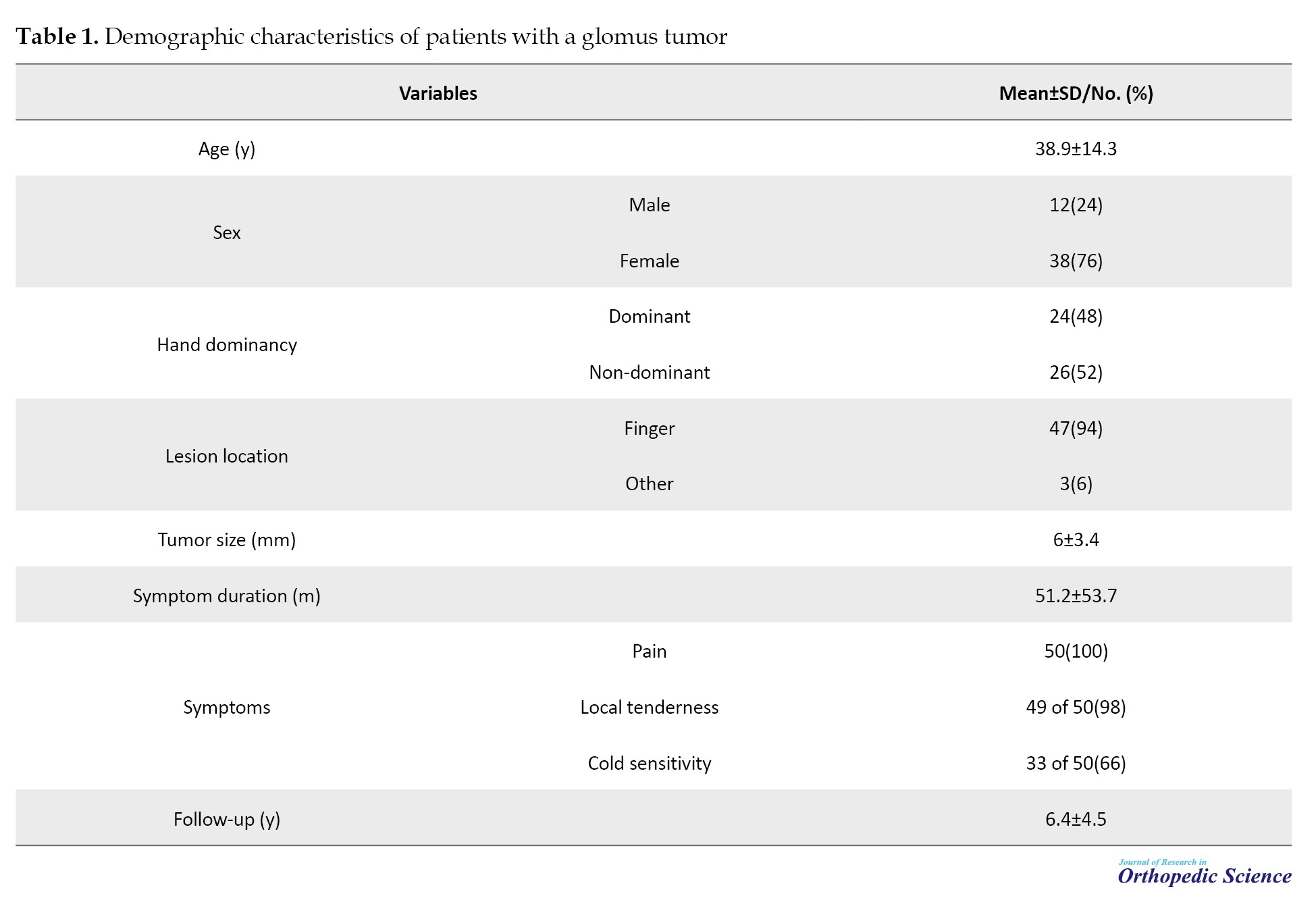
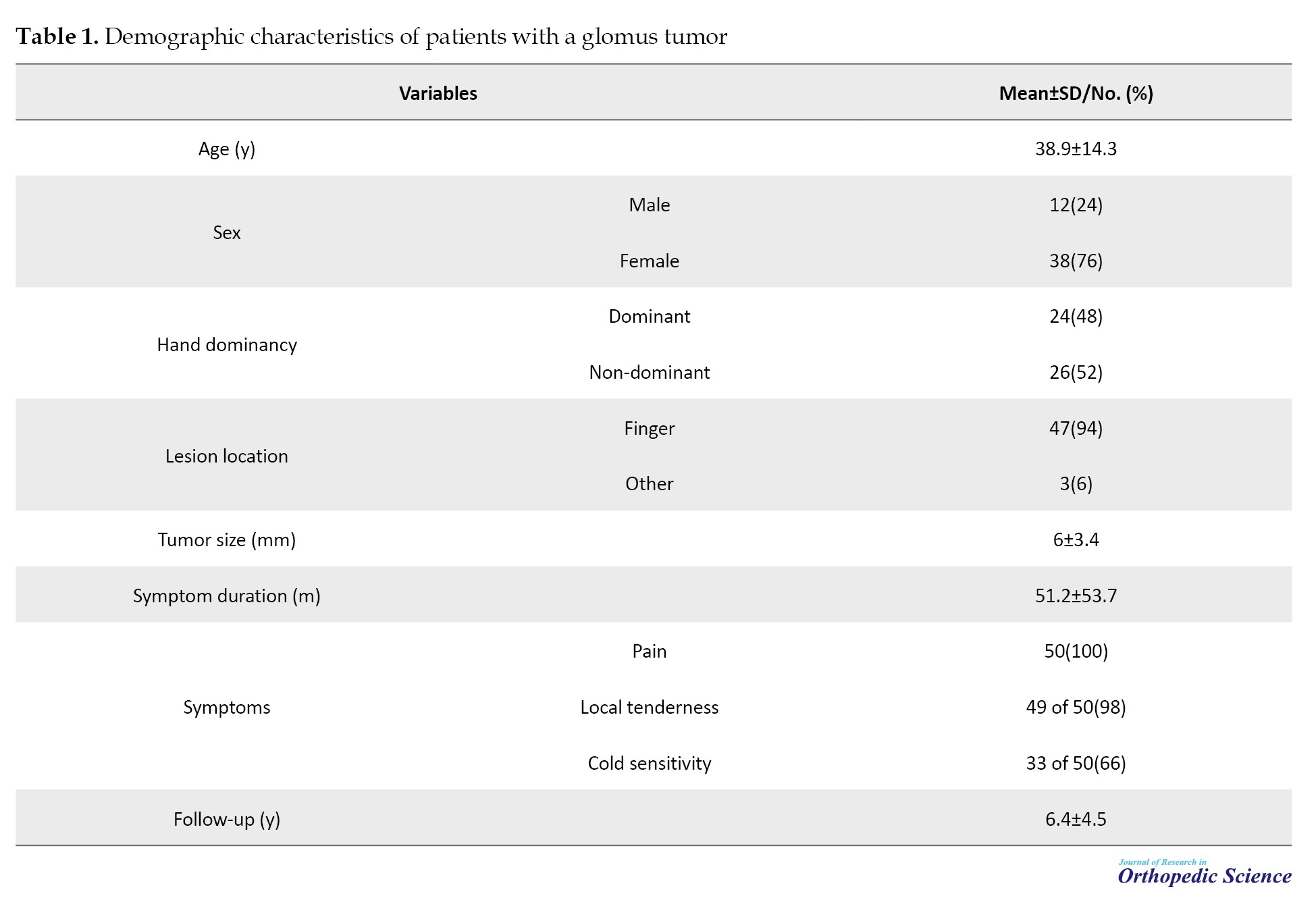
The study included 38(76%) females and 12(24%) males, with a mean patient age of 38.9±14.3 years (range: 16-75 years). There was no significant difference in mean age between male and female populations (36 years vs 40 years). The dominant side was affected in 24(48%) patients, while it was the non-dominant side in 26(52%) patients. Symptoms included pain in all patients (100%), local tenderness in 49 patients (98%), and cold sensitivity in 33 patients (66%). Hildreth’s test yielded positive results in all patients. The mean duration of symptoms was 51.2±53.7 months (range: 0.5-192 months), with no significant difference between males and females (55 months vs 50 months, P=0.73).
Ninety-four percent (47 cases) of the lesions were located in the fingers, while the remaining four were found in the wrist, forearm, and thigh. Among the 47 finger glomus tumor cases, 35(74.5%) were in the subungual region, 9(19.1%) were in the volar pulp, and 3(6.4%) were in other locations such as the intermediate phalange, proximal phalange, or web space. The first and fourth fingers were the most frequently affected (n=12 and n=13, respectively), while the fifth finger was the least frequently involved finger (n=4). The mean size of the tumor was 6±3.4 mm (range: 1-20 mm). The demographic characteristics of the patients are summarized in Table 1.
Post-operative complications
At a mean follow-up of 6.4±4.5 years (range: 1-16 years), tumor recurrence was observed in two patients (4%) in the finger. One recurrence occurred one year post-operation, while the other occurred three years post-operation, both of which underwent revision surgery. No further complications were recorded during the two-year follow-up of these patients. Seven patients (14%) experienced post-operative non-oncologic complications, including persistent pain in two patients, numbness in two patients, paresthesia in one patient, limited range of motion in one patient, and nail separation without replacement. Since the post-operative complications were minor, no intervention was required.
4. Discussion
This study evaluated the epidemiological characteristics and outcomes of surgical excision in a retrospective cohort of 50 patients. The frequency of glomus tumors in women was about 3.2 times higher than in men. Fingers were the most commonly affected site (94%), with the subungual region being the most common location (74.5%). Pain and tenderness were present in almost all patients, while cold sensitivity was present only in 66% of patients. Two recurrences occurred during the average 6.4-year follow-up. Seven patients experienced surgical complications, most of which were minor. The epidemiological characteristics and outcomes of glomus tumors have been reported in earlier studies as well. Chou et al. reported their experience with 50 patients diagnosed with glomus tumors over 20 years. The mean age of patients was 42.3 years, ranging from 9 to 61 years, with a female-to-male ratio of 3.2. Pain and tenderness were the main symptoms, while cold hypersensitivity was present in only 30% of patients [5]. Saaiq et al. reported on glomus tumors of the hand in 17 patients with a mean age of 41.2 years, a female-to-male ratio of 2.4, and the mean symptom duration of 18.9 months. Pain and tenderness were present in all patients, while cold sensitivity was present in 76.5%. Nail change was only present in two patients (11.76%) [6]. Fazwi et al. retrospectively reviewed their experience with 15 patients diagnosed over 15 years, reporting a female-to-male ratio of 1.5 and a mean age of 49.6 years. Tenderness, pain, and cold hypersensitivity were present in 63-100% of patients [2]. Geertruyden et al. reported glomus tumors of the hand in 51 patients with a mean age of 44 years and the female-to-male ratio of 6.2 [7]. This study’s mean age was 38.9 years (range: 16-75 years), with a female-to-male ratio of 4. Therefore, the epidemiologic characteristics of patients in the present study were similar to those reported in earlier studies. Similar to earlier studies, pain, tenderness, and cold hypersensitivity were the main symptoms at presentation in the present study. However, nail deformity was not observed in any patients. The mean symptom duration was 51.2 months, comparable to earlier reports. Since the classic triad of glomus tumors may not manifest in all patients, it is essential to differentially diagnose glomus tumors from other conditions, such as leiomyoma, hemangioma, neuroma, and osteochondroma, which can also cause severe fingertip pain [4]. Previous studies have reported recurrence rates for glomus tumors ranging from 5% to 15% [2, 8, 9, 10]. This variation can be attributed to factors such as location, size, and the possibility of complete excision [11-15]. Malignant transformation of glomus tumors can also increase the risk of local recurrence [5]. In the present study, two recurrences (4%) were observed, both in the subungual region. However, no instances of malignant transformation were recorded, and the rate of extradigital glomus tumors was significantly lower in the present study (6%). Surgical complications following glomus tumor excision vary depending on the tumor’s location. Nail deformity is a common post-operative complication in finger tumors, with reported incidences ranging from 3.3% to 26.3%, and nail deformity was recorded in two patients (4%) [4, 5]. In contrast, in a study, no post-operative nail deformity was recorded [6].
In this study, only one patient had a nail-related complication (nail separation), and complications, such as paresthesia, persistent pain stiffness, and limited range of movement occurred at a lower frequency, similar to another survey [16]. The epidemiologic characteristics and outcomes of glomus tumors in the present study were almost consistent with those reported in earlier studies, with minor differences in some characteristics, such as the incidence of extradigital glomus tumors [11-15].
5. Conclusion
Considering the incidence of glomus tumors, more awareness is required regarding its epidemiologic characteristics, clinical presentation, diagnosis, management, post-operative complications, and recurrence. According to our experience, glomus tumors are often found in the finger and are more prevalent in females. The diagnostic triad of glomus tumor, including pain, tenderness, and cold hypersensitivity, is present in most patients. Surgical excision is an effective treatment for local control, although recurrence may occur in a small subset of patients .
Study limitations
A limitation of this study was its retrospective design, which limited the scope of comprehensive outcome investigations, such as assessing pain improvement.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by review board of Iran University of Medical Sciences (Code: IR.IUMS.FMD.REC.1402.346).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Farid Najdmazhar, Hooman Shariatzadeh, and Reza Torab; Study design and manuscript preparation: Farid Najdmazhar, Hosein Hamadian, Behnam Jafari, Seyed Morteza Motevallian Sajadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to express their gratitude to all who contributed to the present research, especially the esteemed professors and personnel of the Shafa Yahyaeian Hospital, Tehran, Iran.
References
Glomus bodies are normal structures composed of glomus cells, smooth muscle cells, and vasculature highly concentrated in the digits and are involved in regulating skin temperature [1]. Glomus tumors are benign perivascular neoplasms in the distal limbs, particularly in the nail bed [2, 3].
Patients generally present with long periods of pain. Clinically, a glomus tumor is a discoloration of the nail plate into bluish or pinkish red, with a classical triad of severe pain, localized tenderness, and cold sensitivity. Classic symptoms might not be present in all patients, necessitating differential diagnosis of other tumors. Diagnosis is generally based on clinical tests, including Love’s pin test, Hildreth’s test, and trans-illumination test, combined with imaging studies, such as magnetic resonance imaging (MRI), ultrasonography, and radiography [4]. However, mismanagement and delayed diagnosis are common [2].
When the glomus tumor is diagnosed, complete surgical excision is required to improve symptoms. Various surgical approaches could be selected depending on the anatomical location of the lesion. Incomplete excision can cause local recurrence; thus, a recurrence rate of up to 15% has been reported following the surgical excision [2, 4].
In this study, we described epidemiologic characteristics, clinical presentation, diagnosis management, post-operative complications, and recurrence of glomus tumors.
2. Methods
Patients who underwent surgical excision at Shafa Yahyaeian Hospital, Tehran, Iran between 2009 and 2021, were retrospectively reviewed. Inclusion criteria were histologic confirmation of glomus tumor diagnosis and a minimum follow-up of 12 months. Patients presented with a recurrence and lost to follow-up were excluded from the study. Of 66 patients with glomus tumors, 50 cases met the study criteria and were included in the analysis.
A senior hand surgeon managed all patients at the same orthopedic center. Digital nerve blocks were used for all patients with hand involvement. The translingual approach was used for patients with subungual involvement. The nail plate was removed using fine artery forceps in a standard fashion and carefully lifted off to prevent damage to the nail bed. After exposing the tumor, a longitudinal incision was made, and the tumor was completely excised under magnification. For tumors located in the volar pulp, the lesion was excised through a direct incision made over the volar pulp skin. Post-operatively, limb elevation was advised to prevent edema and swelling. Lesions in less frequent locations were excised as appropriate. Stitches were removed ten days after the operation.
Demographic characteristics, including age, sex, affected digit, dominant side, and clinical characteristics such as symptoms, pain duration, Hildreth’s sign, and tumor characteristics (size, location, and post-operative complications such as deformity, pain, numbness, oncologic outcomes), were collected. The largest diameter of lesion in gross histopathology was regarded as the tumor size. The detection of recurrence relied on clinical suspicion (recurrent pain), plain radiography, and MRI studies if necessary.
Statistics
Data were analyzed using SPSS software, version 22. Qualitative data were presented as numbers and percentages. Quantitative data were presented as Mean±SD. The mean values between the two groups were compared by an independent t-test or Mann–Whitney U test. A P≤0.05 was considered statistically significant.
3. Results
The study included 38(76%) females and 12(24%) males, with a mean patient age of 38.9±14.3 years (range: 16-75 years). There was no significant difference in mean age between male and female populations (36 years vs 40 years). The dominant side was affected in 24(48%) patients, while it was the non-dominant side in 26(52%) patients. Symptoms included pain in all patients (100%), local tenderness in 49 patients (98%), and cold sensitivity in 33 patients (66%). Hildreth’s test yielded positive results in all patients. The mean duration of symptoms was 51.2±53.7 months (range: 0.5-192 months), with no significant difference between males and females (55 months vs 50 months, P=0.73).
Ninety-four percent (47 cases) of the lesions were located in the fingers, while the remaining four were found in the wrist, forearm, and thigh. Among the 47 finger glomus tumor cases, 35(74.5%) were in the subungual region, 9(19.1%) were in the volar pulp, and 3(6.4%) were in other locations such as the intermediate phalange, proximal phalange, or web space. The first and fourth fingers were the most frequently affected (n=12 and n=13, respectively), while the fifth finger was the least frequently involved finger (n=4). The mean size of the tumor was 6±3.4 mm (range: 1-20 mm). The demographic characteristics of the patients are summarized in Table 1.
Post-operative complications
At a mean follow-up of 6.4±4.5 years (range: 1-16 years), tumor recurrence was observed in two patients (4%) in the finger. One recurrence occurred one year post-operation, while the other occurred three years post-operation, both of which underwent revision surgery. No further complications were recorded during the two-year follow-up of these patients. Seven patients (14%) experienced post-operative non-oncologic complications, including persistent pain in two patients, numbness in two patients, paresthesia in one patient, limited range of motion in one patient, and nail separation without replacement. Since the post-operative complications were minor, no intervention was required.
4. Discussion
This study evaluated the epidemiological characteristics and outcomes of surgical excision in a retrospective cohort of 50 patients. The frequency of glomus tumors in women was about 3.2 times higher than in men. Fingers were the most commonly affected site (94%), with the subungual region being the most common location (74.5%). Pain and tenderness were present in almost all patients, while cold sensitivity was present only in 66% of patients. Two recurrences occurred during the average 6.4-year follow-up. Seven patients experienced surgical complications, most of which were minor. The epidemiological characteristics and outcomes of glomus tumors have been reported in earlier studies as well. Chou et al. reported their experience with 50 patients diagnosed with glomus tumors over 20 years. The mean age of patients was 42.3 years, ranging from 9 to 61 years, with a female-to-male ratio of 3.2. Pain and tenderness were the main symptoms, while cold hypersensitivity was present in only 30% of patients [5]. Saaiq et al. reported on glomus tumors of the hand in 17 patients with a mean age of 41.2 years, a female-to-male ratio of 2.4, and the mean symptom duration of 18.9 months. Pain and tenderness were present in all patients, while cold sensitivity was present in 76.5%. Nail change was only present in two patients (11.76%) [6]. Fazwi et al. retrospectively reviewed their experience with 15 patients diagnosed over 15 years, reporting a female-to-male ratio of 1.5 and a mean age of 49.6 years. Tenderness, pain, and cold hypersensitivity were present in 63-100% of patients [2]. Geertruyden et al. reported glomus tumors of the hand in 51 patients with a mean age of 44 years and the female-to-male ratio of 6.2 [7]. This study’s mean age was 38.9 years (range: 16-75 years), with a female-to-male ratio of 4. Therefore, the epidemiologic characteristics of patients in the present study were similar to those reported in earlier studies. Similar to earlier studies, pain, tenderness, and cold hypersensitivity were the main symptoms at presentation in the present study. However, nail deformity was not observed in any patients. The mean symptom duration was 51.2 months, comparable to earlier reports. Since the classic triad of glomus tumors may not manifest in all patients, it is essential to differentially diagnose glomus tumors from other conditions, such as leiomyoma, hemangioma, neuroma, and osteochondroma, which can also cause severe fingertip pain [4]. Previous studies have reported recurrence rates for glomus tumors ranging from 5% to 15% [2, 8, 9, 10]. This variation can be attributed to factors such as location, size, and the possibility of complete excision [11-15]. Malignant transformation of glomus tumors can also increase the risk of local recurrence [5]. In the present study, two recurrences (4%) were observed, both in the subungual region. However, no instances of malignant transformation were recorded, and the rate of extradigital glomus tumors was significantly lower in the present study (6%). Surgical complications following glomus tumor excision vary depending on the tumor’s location. Nail deformity is a common post-operative complication in finger tumors, with reported incidences ranging from 3.3% to 26.3%, and nail deformity was recorded in two patients (4%) [4, 5]. In contrast, in a study, no post-operative nail deformity was recorded [6].
In this study, only one patient had a nail-related complication (nail separation), and complications, such as paresthesia, persistent pain stiffness, and limited range of movement occurred at a lower frequency, similar to another survey [16]. The epidemiologic characteristics and outcomes of glomus tumors in the present study were almost consistent with those reported in earlier studies, with minor differences in some characteristics, such as the incidence of extradigital glomus tumors [11-15].
5. Conclusion
Considering the incidence of glomus tumors, more awareness is required regarding its epidemiologic characteristics, clinical presentation, diagnosis, management, post-operative complications, and recurrence. According to our experience, glomus tumors are often found in the finger and are more prevalent in females. The diagnostic triad of glomus tumor, including pain, tenderness, and cold hypersensitivity, is present in most patients. Surgical excision is an effective treatment for local control, although recurrence may occur in a small subset of patients .
Study limitations
A limitation of this study was its retrospective design, which limited the scope of comprehensive outcome investigations, such as assessing pain improvement.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by review board of Iran University of Medical Sciences (Code: IR.IUMS.FMD.REC.1402.346).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Farid Najdmazhar, Hooman Shariatzadeh, and Reza Torab; Study design and manuscript preparation: Farid Najdmazhar, Hosein Hamadian, Behnam Jafari, Seyed Morteza Motevallian Sajadi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to express their gratitude to all who contributed to the present research, especially the esteemed professors and personnel of the Shafa Yahyaeian Hospital, Tehran, Iran.
References
- Lawson W. Glomus bodies and tumors. N Y State J Med. 1980; 80(10):1567-75. [PMID]
- Fazwi R, Chandran PA, Ahmad TS. Glomus tumour: A retrospective review of 15 years experience in a single institution. Malays Orthop J. 2011; 5(3):8-12. [DOI:10.5704/MOJ.1111.007] [PMID]
- Najd Mazhar F, Shoushtarizadeh T, Mirzaei A. Intravascular glomus tumor of the wrist causing chronic wrist pain. J Hand Microsurg. 2018; 10(2):113-5.[DOI:10.1055/s-0038-1626683] [PMID]
- Morey VM, Garg B, Kotwal PP. Glomus tumours of the hand: Review of literature. J Clin Orthop Trauma. 2016; 7(4):286-91. [DOI:10.1016/j.jcot.2016.04.006] [PMID]
- Chou T, Pan SC, Shieh SJ, Lee JW, Chiu HY, Ho CL. Glomus Tumor: Twenty-year experience and literature review. Ann Plast Surg. 2016; 76 (Suppl 1):S35-40. [DOI:10.1097/SAP.0000000000000684] [PMID]
- Saaiq M. Presentation and management outcome of glomus tumors of the hand. Arch Bone Jt Surg. 2021; 9(3):312-8. [PMID]
- Van Geertruyden J, Lorea P, Goldschmidt D, de Fontaine S, Schuind F, Kinnen L, et al. Glomus tumours of the hand: A retrospective study of 51 cases. J Hand Surg. 1996; 21(2):257-60. [DOI:10.1016/S0266-7681(96)80110-0]
- Carroll RE, Berman AT. Glomus tumors of the hand: Review of the literature and report on twenty-eight cases. J Bone Joint Surg. 1972; 54(4):691-703. [DOI:10.2106/00004623-197254040-00001]
- Van Ruyssevelt CE, Vranckx P. Subungual glomus tumor: Emphasis on MR angiography. AJR Am J Roentgenol. 2004; 182(1):263-4. [DOI:10.2214/ajr.182.1.1820263] [PMID]
- Vasisht B, Watson HK, Joseph E, Lionelli GT. Digital glomus tumors: A 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004; 114(6):1486-9. [DOI:10.1097/01.PRS.0000138752.36175.D5] [PMID]
- Singal A, Bisherwal K, Agrawal S, Bhat S, Diwakar P. Clinico-epidemiological profile and management outcome of subungual digital glomus tumor-Indian experience. Dermatol Ther. 2022; 35(10):e15745. [DOI:10.1111/dth.15745]
- Netscher DT, Aburto J, Koepplinger M. Subungual glomus tumor. J Hand Surg Am. 2012; 37(4):821-3; quiz 824. [DOI:10.1016/j.jhsa.2011.10.026] [PMID]
- Takata H, Ikuta Y, Ishida O, Kimori K. Treatment of subungual glomus tumour. Hand Surg. 2001; 6(1):25-7. [DOI:10.1142/S0218810401000394] [PMID]
- Grover C, Khurana A, Jain R, Rathi V. Transungual surgical excision of subungual glomus tumour. J Cutan Aesthet Surg. 2013; 6(4):196-203. [DOI:10.4103/0974-2077.123401] [PMID]
- Farzan M, Neshan M, Farhoud AR, Abdoli A. Subungual glomus tumor: A review of 15 cases treated with partial nail plate excision technique. J Orthop Spine Trauma. 2021; 77-80. [DOI:10.18502/jost.v7i3.8102]
- Kim YJ, Kim DH, Park JS, Baek JH, Kim KJ, Lee JH. Factors affecting surgical outcomes of digital glomus tumour: A multicentre study. J Hand Surg Eur Vol. 2018; 43(6):652-8. [DOI:10.1177/1753193418774176] [PMID]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2022/02/25 | Accepted: 2022/05/12 | Published: 2022/08/1
Received: 2022/02/25 | Accepted: 2022/05/12 | Published: 2022/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |