Volume 9, Issue 4 (11-2022)
JROS 2022, 9(4): 219-224 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pisoudeh K, Gravandi S. Clinical Results, Tonnis Classification, and Stulberg Classification in Patients With Legg-Calvé-Perthes Disease Underwent Containment Surgeries. JROS 2022; 9 (4) :219-224
URL: http://jros.iums.ac.ir/article-1-2223-en.html
URL: http://jros.iums.ac.ir/article-1-2223-en.html
1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Legg–Calvé–Perthes disease (LCPD), Classification of Herring, Containment surgery, Stulberg’s classification
Full-Text [PDF 947 kb]
(139 Downloads)
| Abstract (HTML) (519 Views)
Full-Text: (164 Views)
1. Introduction
Legg-Calve-Perthes disease (LCPD) is osteonecrosis of the femoral head in children. The etiology of this disease is multi-factorial and causes a temporary disruption in the blood supply of the femoral head in the pelvic area, which occurs during childhood [1]. In this disease, the osteonecrosis changes, the new bone replaces the missing tissue, and the bone shape alters [2]. This pathophysiology of the disease forms the basis of containment surgeries. This treatment obtains a mobile and congruent joint [3, 4]. Classical treatment is performed based on age and Herring’s classification; accordingly, the treatment is the combination of the ability to remodel and the severity of the disease. The limitations of decision-making based on this classification include placing the patient in the fragmentation phase of the disease and disagreement among surgeons about patients who can benefit from surgical treatment. In children with Herring B and B/C involvement, many surgeons prefer osteotomy surgeries after the age of 8 years [5, 6]. The challenge is to decide for patients with greater severity of involvement (group C) [4, 7]. In a study, surgical and non-surgical containment treatments were compared in 6-8 year-old patients with more than 50% femoral head involvement. The results showed that although the radiographic results of the surgical group were better, Stulberg’s classification and clinical results (pain and range of motion) were not significantly different [8]. The results of another study have shown that containment surgery in the form of combined femoral and pelvic osteotomy is effective on both the radiographic and clinical results of Herring C patients [9]. According to the previous conflicting opinions and considering that the decision regarding the treatment method of Legg-Calvé-Perthes patients with Herring type C degree of involvement is still unclear, this study investigates the clinical results, the state of osteoarthritis based on Tonnis classification, and Stulberg deformity grade, in Legg-Calvé-Perthes patients with Herring type C involvement scores who underwent containment surgery.
2. Methods
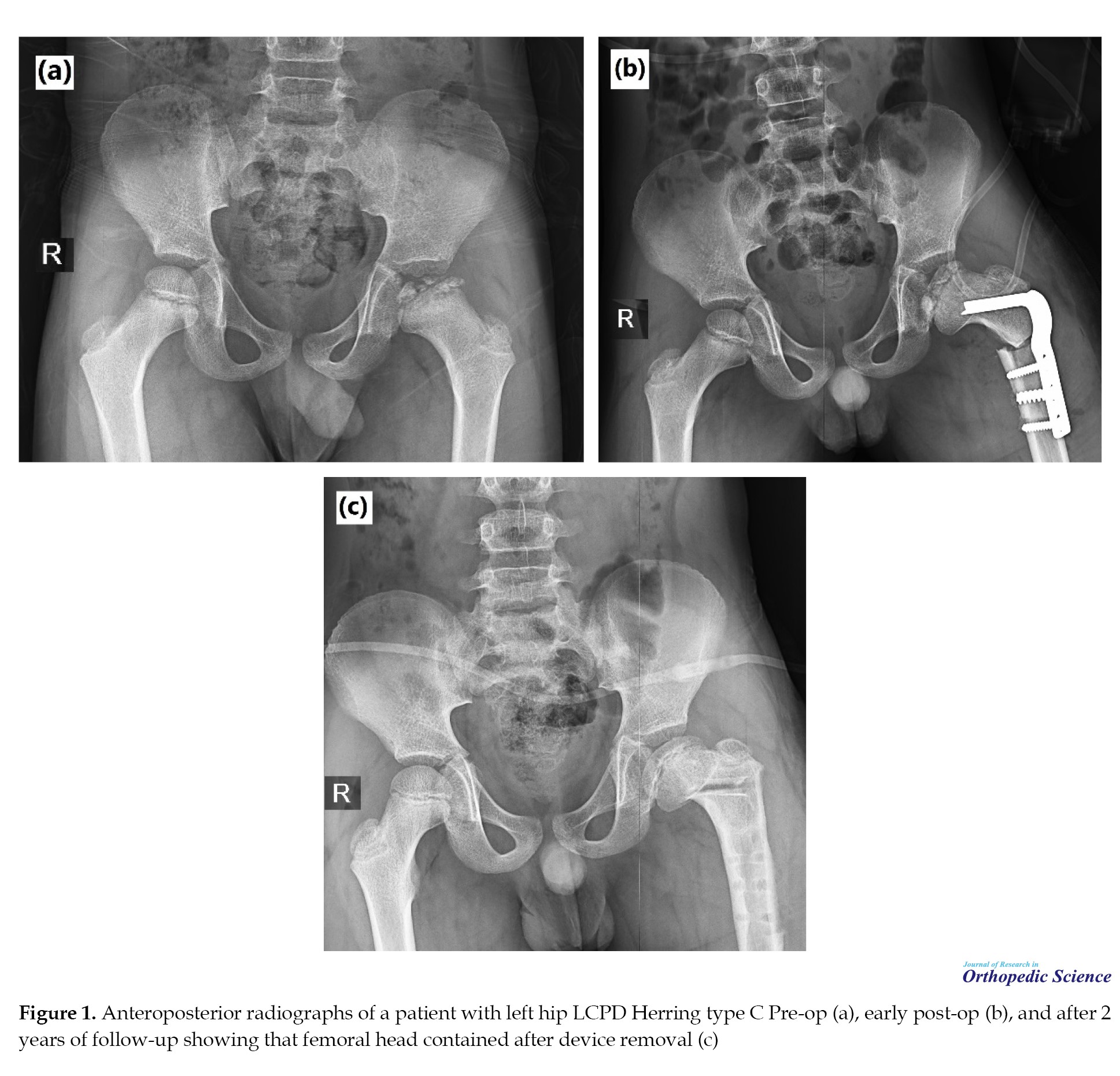
This retrospective study examined the medical profiles of LCPD patients referred to Shafa Yahyaeian Orthopedic Hospital from March 2011 to March 2021 and met the inclusion criteria. The inclusion criteria were a degree of Herring group C involvement, up to 12 years of diagnostic age (for remodelling capability), at least 2 years follow-up period, access to radiographs and patient records, and patient availability for new radiography and current examinations. The patients with a history of any type of hip surgery except for containment surgery were excluded from the study. Finally, 18 patients (19 hips) were qualified to enter the study. Containment surgery methods for these patients included femoral methods as follows: Femoral varus osteotomy (10 hips, 52.6%) which included the most surgeries (Figure 1a and 1b) and femoral valgus osteotomy (2 hips, 10.6%); pelvic methods: Salter osteotomy (2 hips, 10.5%), triple innominate osteotomy (3 hips, 15.6%); Ganz osteotomy (2 hips, 10.5%) which were operated by three senior hip surgeons of our institute. All patients, except one femoral valgus and one Ganz osteotomy case, had abduction casts after the surgery.
The patients’ information was collected using a checklist in two sections as follows: Demographic-biometric data, including age, follow-up period, gender, and surgical side which was completed from the medical profile and body mass index (weight(kg)/height(m)2) that was calculated during the current visit; clinical-radiographic data, including information that was measured before and after surgery (range of motion [ROM] in flexion, extension, internal rotation, external rotation, abduction, adduction [degree], hip joint tenderness, limping, Trendelenberg test, osteoarthritis status based on Tonnis classification, including grade 0 to 3 which was calculated by observing the radiograph during the first visit and the current patient’s radiograph) and information that was measured after surgery (hip function was calculated with the Merle d’Aubigne-Postel score of 18 points, lower limb discrepancy (LLD) was measured as the apparent length [anterior superior iliac spine to the medial malleolus], difference of two lower limbs in centimeter scale, Stulberg’s classification of each patient was also calculated by observing the patient’s current radiograph in the antroposterior and lateral cross table views from grade 1 to 5). To increase interobserver reliability, two researchers followed the patients’ radiographs separately to determine the Tonnis and Stulberg classification.
The patients’ information was analyzed using the SPSS software, version 22. Central tendencies Mean±SD were used to report quantitative variables. Frequency (%) was used to report qualitative variables. The distribution normality of the variables was determined using the Kolmogorov-Smirnov test. For comparison, a parametric t-test was used, assuming the variables had a normal distribution, and the non-parametric Mann-Whitney test was used if the distribution of variables was not normal. Meanwhile, the chi-squared test was used for statistical analysis of qualitative variables. A P<0.05 was considered the significance level.
3. Results
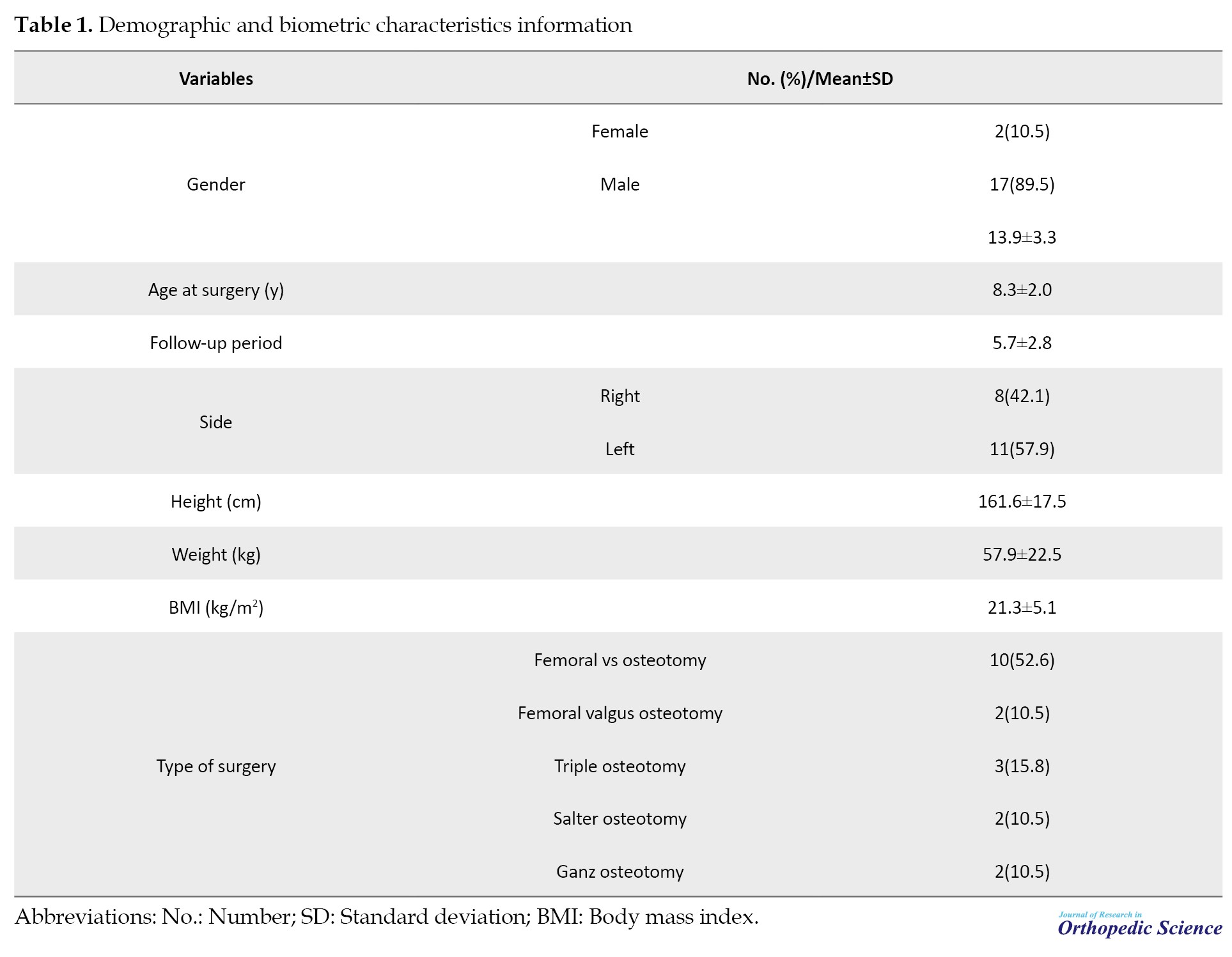
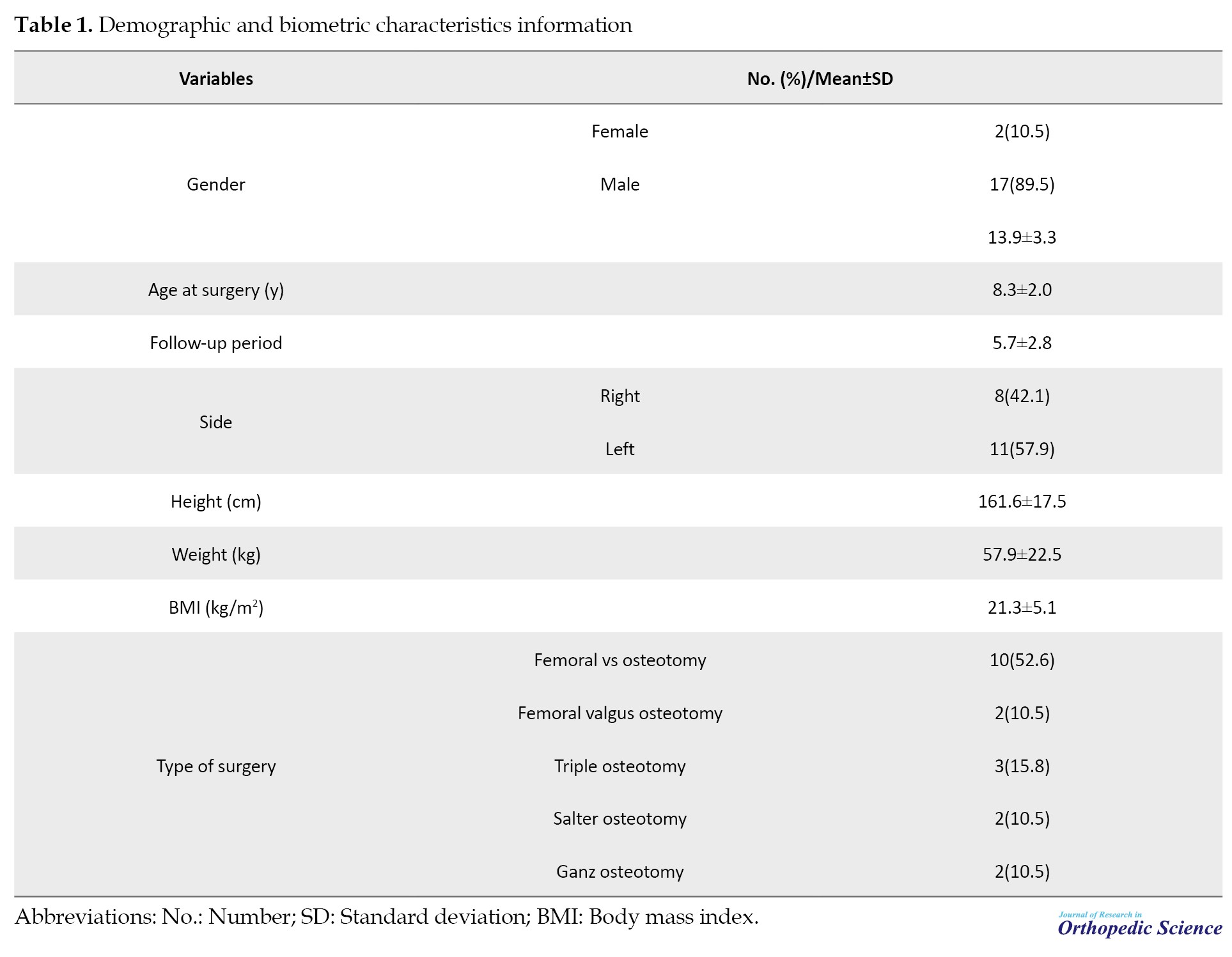
A total of 18 patients (19 hips) were included in the study, of which two hips belonged to one female patient (10.5%) and 18 hips belonged to 18 male patients (89.5%). The mean patients’ current age was 13.9 years (8 to 22 years), and the mean age when the patients underwent surgery was 8.3 years (5 to 12 years). The follow-up period was 5.7 years on average (2 to 10 years). The left side was the most frequently involved (57.9%). The mean body mass index was 21.3 kg/m2. More detailed demographic and biometric characteristics information are described in Table 1.
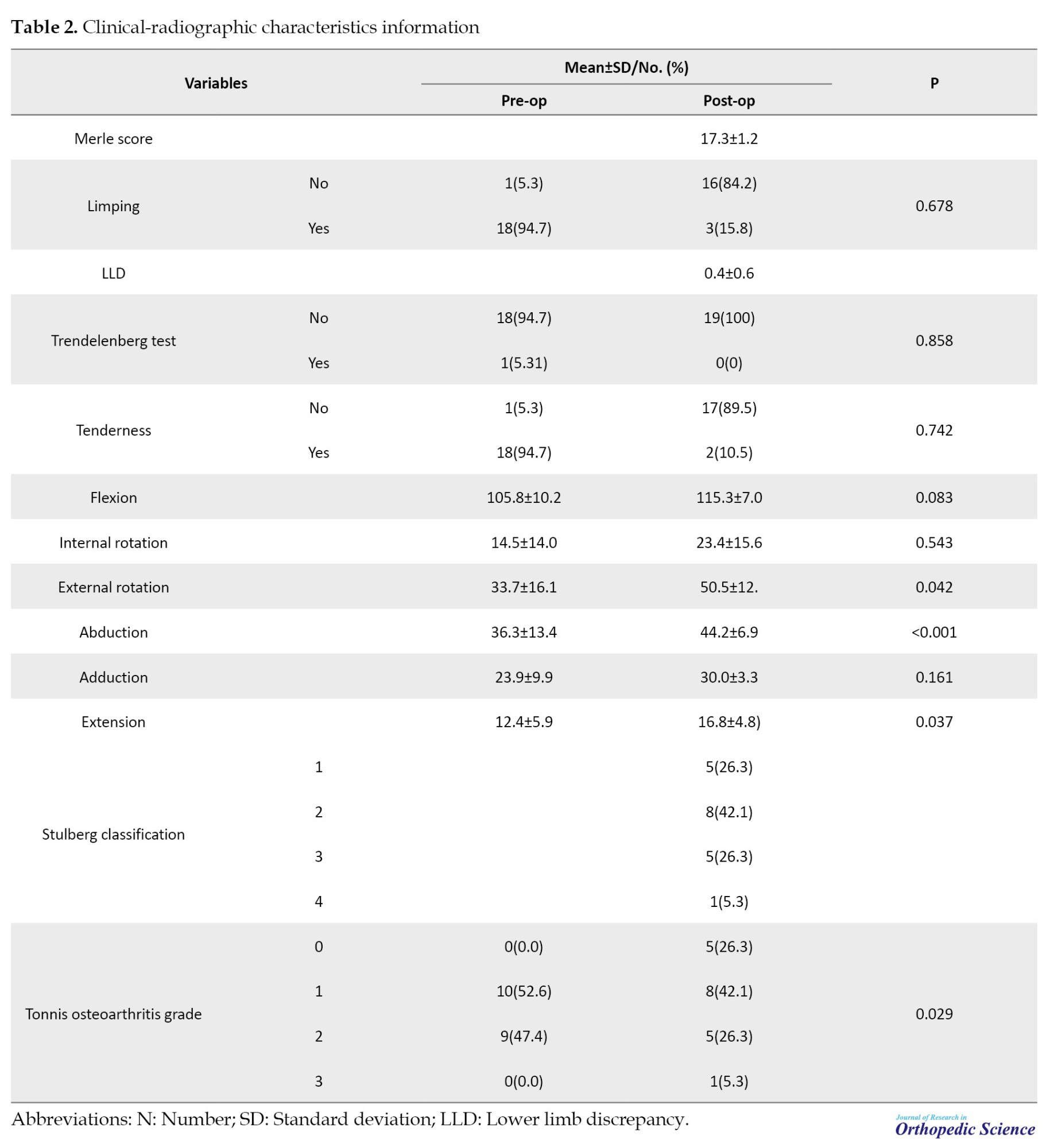
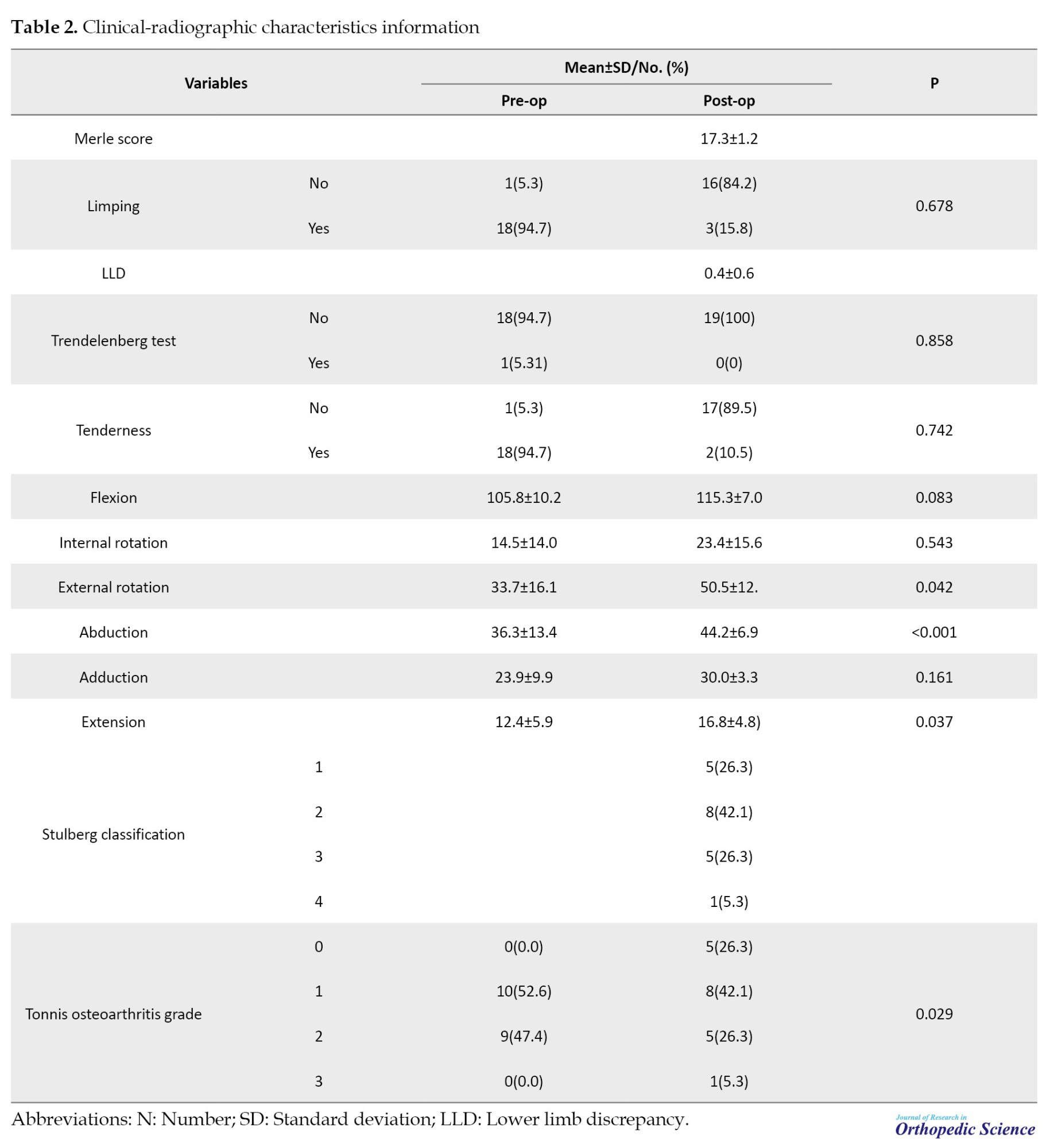
In the hip ROM examination, the mean patient’s hip abduction increased from 36.3° pre-op to 44.2° post-op (P<0.001). Also, the external rotation increased from 33.7° to 50.5° (P=0.042). Also, extension increased from 12.4° to 16.8° (P=0.037), which were all significant. Although improvement was observed in flexion, internal rotation, and adduction, they were insignificant (P=0.083, 0.543, 0.161, respectively).
Before surgery, 18 patients (94.7%) had hip tenderness, but after surgery, 2 patients (10.5%) had tenderness during examination (P=0.742). In addition, 18 patients (94.7%) had pre-op limping, and limping was observed in 2 patients (10.5%) post-op (P=0.678). Before surgery, the Trendelenberg test was positive in one patient (5.3%), but none had a positive post-op test (P=0.858). Post-op Merle d’Aubigne-Postel score of the patients was 17.3±1.2, indicating proper hip joint function. The mean post-op LLD was 0.4±0.6 cm.
Pre-op osteoarthritis status based on Tonnis classification was as follows: 10 patients (52.6%) were in class 1, and 9 patients (47.4%) were in class 2. After surgery, 5 hips (26.3%) were in class 0, 8 hips (42.1%) were in class 1, and 5 hips (26.2%) were in class 2, in addition to 1 hip (5.3%) that was in class 3, which indicated a significant improvement in the osteoarthritis condition (P=0.029).
In addition, post-op femoral head deformity grades according to Stulberg class were as follows: 5 hips (26.5%)=class 1, 8 hips (42.1%)=class 2, 5 hips (26.5%)=class 3, 1 hip (5.3%)=class 4; meanwhile, no hip was placed in class 5. More detailed information about the clinical-radiographic characteristics is described in Table 2.
4. Discussion
This study examined the clinical results, osteoarthritis status based on the Tonnis classification and Stulberg’s deformity grade of LCPD patients with Herring C involvement scores who underwent various containment surgeries. Based on this research, ROM significantly improved the abduction, extension and external rotation directions. The mean post-op Merle score of patients was 17.3, which indicates proper hip function. The grade of osteoarthritis based on Tonnis’s classification also improved significantly after surgery. According to Stulberg’s classification, the highest frequency was related to class 2 (42.1%, 8 patients) and no patient was placed in class 5.
In a study, Siebenrock et al. investigated the effect of head reduction osteotomy with additional containment surgery in LCPD patients. Over 10 years, the authors performed femoral head reduction osteotomies in 11 hips with severe LCPD. In addition, 5 out of 11 hips had containment surgery. The patients were followed for five years. Merle’s score was 14.5 vs 15.7. Also, ROM (flexion, internal and external rotation in 90° of flexion) was not improved. No avascular necrosis of the femoral head occurred [10]. The results of the present study also showed that the grade of hip osteoarthritis caused by femoral head osteonecrosis decreased significantly after surgery.
In a study, Gharanizadeh et al. investigated the results of the simultaneous combination of femoral head reduction osteotomy and periacetabular osteotomy. In this research, four patients in stage 4 of Waldenstrom (mean age 10.5) and severe femoral head asphericity had a combination surgery and 2 years follow-up. The Harris hip score improved by 27 points. ROM was increased from 222° to 267°. There was no osteonecrosis [11]. The findings of the mentioned study are consistent with the present study’s findings in increasing the ROM of patients after surgery.
In another meta-analysis study, the time aspect of intervention has been investigated. Kadhim et al. reviewed 11 studies on LCPD patients. They concluded that Stulberg’s scale rating was lower in children who underwent surgery earlier than in those who underwent surgery later (84% Grade 1 in the surgical group compared to 63% grade 3 and above in the non-surgical group) [12]. The present study is also consistent with the findings of the meta-analysis mentioned earlier study, in which none of the patients of the surgical group was classified as grade 5, and only one patient was grade 4, which indicates that the progression of hip joint deformity has stopped.
Also, regarding non-surgical interventions, a recently published systematic review study examining 15 studies (1745 patients) concluded that the bias and heterogeneity in the studies that examined non-surgical interventions were high and did not provide usable results [13].
5. Conclusion
Although increasing age and more severe involvement of the lateral pillar, according to Herring’s classification (group C), are effective on the LCPD patients’ prognosis, if the patient’s age still allows femoral head remodelling, they should not be deprived of the containment surgeries benefits simply because of Herring’s high grade. This study showed that all types of containment surgeries can be useful in patients with LCPD group C at the age of onset under 12 years. We observed an increase in ROM, an improvement in the osteoarthritis grade based on Tonnis classification, as well as a high hip function score based on the Merle score and a decrease in the Stulberg’s deformity grade in the studied patients during a mean of 5.7 years post-op follow.
The limitations of this study include the relatively limited number of patients and its retrospective design. Considering the ethical considerations and research conditions, designing and implementing a clinical trial study has its difficulties.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.507).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualisation and study design: Karim Pisoudeh; Data collection and data analysis: Sohail Gravandi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Legg-Calve-Perthes disease (LCPD) is osteonecrosis of the femoral head in children. The etiology of this disease is multi-factorial and causes a temporary disruption in the blood supply of the femoral head in the pelvic area, which occurs during childhood [1]. In this disease, the osteonecrosis changes, the new bone replaces the missing tissue, and the bone shape alters [2]. This pathophysiology of the disease forms the basis of containment surgeries. This treatment obtains a mobile and congruent joint [3, 4]. Classical treatment is performed based on age and Herring’s classification; accordingly, the treatment is the combination of the ability to remodel and the severity of the disease. The limitations of decision-making based on this classification include placing the patient in the fragmentation phase of the disease and disagreement among surgeons about patients who can benefit from surgical treatment. In children with Herring B and B/C involvement, many surgeons prefer osteotomy surgeries after the age of 8 years [5, 6]. The challenge is to decide for patients with greater severity of involvement (group C) [4, 7]. In a study, surgical and non-surgical containment treatments were compared in 6-8 year-old patients with more than 50% femoral head involvement. The results showed that although the radiographic results of the surgical group were better, Stulberg’s classification and clinical results (pain and range of motion) were not significantly different [8]. The results of another study have shown that containment surgery in the form of combined femoral and pelvic osteotomy is effective on both the radiographic and clinical results of Herring C patients [9]. According to the previous conflicting opinions and considering that the decision regarding the treatment method of Legg-Calvé-Perthes patients with Herring type C degree of involvement is still unclear, this study investigates the clinical results, the state of osteoarthritis based on Tonnis classification, and Stulberg deformity grade, in Legg-Calvé-Perthes patients with Herring type C involvement scores who underwent containment surgery.
2. Methods
This retrospective study examined the medical profiles of LCPD patients referred to Shafa Yahyaeian Orthopedic Hospital from March 2011 to March 2021 and met the inclusion criteria. The inclusion criteria were a degree of Herring group C involvement, up to 12 years of diagnostic age (for remodelling capability), at least 2 years follow-up period, access to radiographs and patient records, and patient availability for new radiography and current examinations. The patients with a history of any type of hip surgery except for containment surgery were excluded from the study. Finally, 18 patients (19 hips) were qualified to enter the study. Containment surgery methods for these patients included femoral methods as follows: Femoral varus osteotomy (10 hips, 52.6%) which included the most surgeries (Figure 1a and 1b) and femoral valgus osteotomy (2 hips, 10.6%); pelvic methods: Salter osteotomy (2 hips, 10.5%), triple innominate osteotomy (3 hips, 15.6%); Ganz osteotomy (2 hips, 10.5%) which were operated by three senior hip surgeons of our institute. All patients, except one femoral valgus and one Ganz osteotomy case, had abduction casts after the surgery.
The patients’ information was collected using a checklist in two sections as follows: Demographic-biometric data, including age, follow-up period, gender, and surgical side which was completed from the medical profile and body mass index (weight(kg)/height(m)2) that was calculated during the current visit; clinical-radiographic data, including information that was measured before and after surgery (range of motion [ROM] in flexion, extension, internal rotation, external rotation, abduction, adduction [degree], hip joint tenderness, limping, Trendelenberg test, osteoarthritis status based on Tonnis classification, including grade 0 to 3 which was calculated by observing the radiograph during the first visit and the current patient’s radiograph) and information that was measured after surgery (hip function was calculated with the Merle d’Aubigne-Postel score of 18 points, lower limb discrepancy (LLD) was measured as the apparent length [anterior superior iliac spine to the medial malleolus], difference of two lower limbs in centimeter scale, Stulberg’s classification of each patient was also calculated by observing the patient’s current radiograph in the antroposterior and lateral cross table views from grade 1 to 5). To increase interobserver reliability, two researchers followed the patients’ radiographs separately to determine the Tonnis and Stulberg classification.
The patients’ information was analyzed using the SPSS software, version 22. Central tendencies Mean±SD were used to report quantitative variables. Frequency (%) was used to report qualitative variables. The distribution normality of the variables was determined using the Kolmogorov-Smirnov test. For comparison, a parametric t-test was used, assuming the variables had a normal distribution, and the non-parametric Mann-Whitney test was used if the distribution of variables was not normal. Meanwhile, the chi-squared test was used for statistical analysis of qualitative variables. A P<0.05 was considered the significance level.
3. Results
A total of 18 patients (19 hips) were included in the study, of which two hips belonged to one female patient (10.5%) and 18 hips belonged to 18 male patients (89.5%). The mean patients’ current age was 13.9 years (8 to 22 years), and the mean age when the patients underwent surgery was 8.3 years (5 to 12 years). The follow-up period was 5.7 years on average (2 to 10 years). The left side was the most frequently involved (57.9%). The mean body mass index was 21.3 kg/m2. More detailed demographic and biometric characteristics information are described in Table 1.
In the hip ROM examination, the mean patient’s hip abduction increased from 36.3° pre-op to 44.2° post-op (P<0.001). Also, the external rotation increased from 33.7° to 50.5° (P=0.042). Also, extension increased from 12.4° to 16.8° (P=0.037), which were all significant. Although improvement was observed in flexion, internal rotation, and adduction, they were insignificant (P=0.083, 0.543, 0.161, respectively).
Before surgery, 18 patients (94.7%) had hip tenderness, but after surgery, 2 patients (10.5%) had tenderness during examination (P=0.742). In addition, 18 patients (94.7%) had pre-op limping, and limping was observed in 2 patients (10.5%) post-op (P=0.678). Before surgery, the Trendelenberg test was positive in one patient (5.3%), but none had a positive post-op test (P=0.858). Post-op Merle d’Aubigne-Postel score of the patients was 17.3±1.2, indicating proper hip joint function. The mean post-op LLD was 0.4±0.6 cm.
Pre-op osteoarthritis status based on Tonnis classification was as follows: 10 patients (52.6%) were in class 1, and 9 patients (47.4%) were in class 2. After surgery, 5 hips (26.3%) were in class 0, 8 hips (42.1%) were in class 1, and 5 hips (26.2%) were in class 2, in addition to 1 hip (5.3%) that was in class 3, which indicated a significant improvement in the osteoarthritis condition (P=0.029).
In addition, post-op femoral head deformity grades according to Stulberg class were as follows: 5 hips (26.5%)=class 1, 8 hips (42.1%)=class 2, 5 hips (26.5%)=class 3, 1 hip (5.3%)=class 4; meanwhile, no hip was placed in class 5. More detailed information about the clinical-radiographic characteristics is described in Table 2.
4. Discussion
This study examined the clinical results, osteoarthritis status based on the Tonnis classification and Stulberg’s deformity grade of LCPD patients with Herring C involvement scores who underwent various containment surgeries. Based on this research, ROM significantly improved the abduction, extension and external rotation directions. The mean post-op Merle score of patients was 17.3, which indicates proper hip function. The grade of osteoarthritis based on Tonnis’s classification also improved significantly after surgery. According to Stulberg’s classification, the highest frequency was related to class 2 (42.1%, 8 patients) and no patient was placed in class 5.
In a study, Siebenrock et al. investigated the effect of head reduction osteotomy with additional containment surgery in LCPD patients. Over 10 years, the authors performed femoral head reduction osteotomies in 11 hips with severe LCPD. In addition, 5 out of 11 hips had containment surgery. The patients were followed for five years. Merle’s score was 14.5 vs 15.7. Also, ROM (flexion, internal and external rotation in 90° of flexion) was not improved. No avascular necrosis of the femoral head occurred [10]. The results of the present study also showed that the grade of hip osteoarthritis caused by femoral head osteonecrosis decreased significantly after surgery.
In a study, Gharanizadeh et al. investigated the results of the simultaneous combination of femoral head reduction osteotomy and periacetabular osteotomy. In this research, four patients in stage 4 of Waldenstrom (mean age 10.5) and severe femoral head asphericity had a combination surgery and 2 years follow-up. The Harris hip score improved by 27 points. ROM was increased from 222° to 267°. There was no osteonecrosis [11]. The findings of the mentioned study are consistent with the present study’s findings in increasing the ROM of patients after surgery.
In another meta-analysis study, the time aspect of intervention has been investigated. Kadhim et al. reviewed 11 studies on LCPD patients. They concluded that Stulberg’s scale rating was lower in children who underwent surgery earlier than in those who underwent surgery later (84% Grade 1 in the surgical group compared to 63% grade 3 and above in the non-surgical group) [12]. The present study is also consistent with the findings of the meta-analysis mentioned earlier study, in which none of the patients of the surgical group was classified as grade 5, and only one patient was grade 4, which indicates that the progression of hip joint deformity has stopped.
Also, regarding non-surgical interventions, a recently published systematic review study examining 15 studies (1745 patients) concluded that the bias and heterogeneity in the studies that examined non-surgical interventions were high and did not provide usable results [13].
5. Conclusion
Although increasing age and more severe involvement of the lateral pillar, according to Herring’s classification (group C), are effective on the LCPD patients’ prognosis, if the patient’s age still allows femoral head remodelling, they should not be deprived of the containment surgeries benefits simply because of Herring’s high grade. This study showed that all types of containment surgeries can be useful in patients with LCPD group C at the age of onset under 12 years. We observed an increase in ROM, an improvement in the osteoarthritis grade based on Tonnis classification, as well as a high hip function score based on the Merle score and a decrease in the Stulberg’s deformity grade in the studied patients during a mean of 5.7 years post-op follow.
The limitations of this study include the relatively limited number of patients and its retrospective design. Considering the ethical considerations and research conditions, designing and implementing a clinical trial study has its difficulties.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1400.507).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualisation and study design: Karim Pisoudeh; Data collection and data analysis: Sohail Gravandi; Final approval: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Kim HK. Legg-Calvé-Perthes disease. J Am Acad Orthop Surg. 2010; 18(11):676-86. [DOI:10.5435/00124635-201011000-00005] [PMID]
- Kessler JI, Cannamela PC. What are the demographics and epidemiology of Legg-Calvé-Perthes disease in a large Southern California integrated health system? Clin Orthop Relat Res. 2018; 476(12):2344-50. [DOI:10.1097/CORR.0000000000000490] [PMID]
- Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Jt Surg. 1981; 63(7):1095-108. [DOI:10.2106/00004623-198163070-00006]
- Mazloumi SM, Ebrahimzadeh MH, Kachooei AR. Evolution in diagnosis and treatment of Legg-Calve-Perthes disease. Arch Bone Jt Surg. 2014; 2(2):86-92. [PMID]
- Kim HK. Pathophysiology and new strategies for the treatment of Legg-Calvé-Perthes disease.J Bone Joint Surg Am. 2012; 94(7):659-69. [DOI:10.2106/JBJS.J.01834] [PMID]
- Herring JA. The treatment of Legg-Calvé-Perthes disease. A critical review of the literature. J Bone Joint Surg Am. 1994; 76(3):448-58. [DOI:10.2106/00004623-199403000-00017] [PMID]
- Sponseller PD, Desai SS, Millis M. Comparison of femoral and innominate osteotomies for the treatment of Legg-Calvé-Perthes disease. J Bone Jt Surg. 1988; 70(8):1131-9. [DOI:10.2106/00004623-198870080-00003]
- Kaneko H, Kitoh H, Mishima K, Matsushita M, Hattori T, Noritake K, et al. Comparison of surgical and nonsurgical containment methods for patients with Legg-Calve-Perthes disease of the onset ages between 6.0 and 8.0 years: Salter osteotomy versus a non-weight-bearing hip flexion-abduction brace. J Pediatr Orthop B. 2020; 29(6):542-9. [DOI:10.1097/BPB.0000000000000710] [PMID]
- Kamegaya M, Morita M, Saisu T, Kakizaki J, Oikawa Y, Segawa Y. Single versus combined procedures for severely involved Legg-Calvé-Perthes disease. J Pediatr Orthop. 2018; 38(6):312-9. [PMID]
- Siebenrock KA, Anwander H, Zurmühle CA, Tannast M, Slongo T, Steppacher SD. Head reduction osteotomy with additional containment surgery improves sphericity and containment and reduces pain in Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2015; 473(4):1274-83. [DOI:10.1007/s11999-014-4048-1] [PMID]
- Gharanizadeh K, Ravanbod H, Aminian A, Mirghaderi SP. Simultaneous femoral head reduction osteotomy (FHRO) combined with periacetabular osteotomy (PAO) for the treatment of severe femoral head asphericity in Perthes disease. J Orthop Surg Res. 2022; 17(1):461. [DOI:10.1186/s13018-022-03351-7] [PMID]
- Kadhim M, Holmes L Jr, Bowen JR. The role of shelf acetabuloplasty in early and late stages of Perthes disease: A meta-analysis of observational studies. J Child Orthop. 2012; 6(5):379-90. [DOI:10.1007/s11832-012-0436-9] [PMID]
- Galloway AM, van-Hille T, Perry DC, Holton C, Mason L, Richards S, et al. A systematic review of the non-surgical treatment of Perthes’ disease. Bone Jt Open. 2020; 1(12):720-30. [DOI:10.1302/2633-1462.112.BJO-2020-0138.R1] [PMID]
Type of Study: Research Article |
Subject:
Hip surgery
Received: 2022/02/17 | Accepted: 2022/03/12 | Published: 2022/11/1
Received: 2022/02/17 | Accepted: 2022/03/12 | Published: 2022/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |