Volume 10, Issue 2 (5-2023)
JROS 2023, 10(2): 81-88 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najdmazhar F, Shariatzadeh H, Hamadiyan H, Ibrahim Hasasn A, Layeghi A. Comparison of Anterior Transposition of the Ulnar Nerve by Subcutaneous and Transmuscular Methods in the Treatment of Cubital Tunnel Syndrome. JROS 2023; 10 (2) :81-88
URL: http://jros.iums.ac.ir/article-1-2225-en.html
URL: http://jros.iums.ac.ir/article-1-2225-en.html
Farid Najdmazhar1 

 , Hooman Shariatzadeh1
, Hooman Shariatzadeh1 

 , Hosein Hamadiyan2
, Hosein Hamadiyan2 

 , Ahmad Ibrahim Hasasn1
, Ahmad Ibrahim Hasasn1 

 , Abdorrasoul Layeghi1
, Abdorrasoul Layeghi1 




 , Hooman Shariatzadeh1
, Hooman Shariatzadeh1 

 , Hosein Hamadiyan2
, Hosein Hamadiyan2 

 , Ahmad Ibrahim Hasasn1
, Ahmad Ibrahim Hasasn1 

 , Abdorrasoul Layeghi1
, Abdorrasoul Layeghi1 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Anterior transposition, Ulnar nerve, Subcutaneous, Transmuscular, Cubital tunnel syndrome, Wilson and Krout criteria
Full-Text [PDF 521 kb]
(249 Downloads)
| Abstract (HTML) (1089 Views)
Full-Text: (763 Views)
Introduction
Cubital tunnel syndrome, also known as ulnar neuropathy at the elbow, is the second peripheral nerve entrapment neuropathy after carpal tunnel syndrome [1-5]. The prevalence of cubital tunnel syndrome in men is twice as high as in women, with an annual incidence of approximately twenty-five cases per 100000 individuals [1]. The population has an incidence rate of up to 1% [6].
Various surgical techniques have been established to treat ulnar neuropathy at the elbow, such as simple decompressionmpression, anterior transposition of the ulnar nerve, and medial epicondylectomy [7]. Anterior transposition of the ulnar nerve involves relocating the nerve either subcutaneously, within the muscle, or beneath it [1]. However, it is unclear whether the comparative efficacy of subcutaneous and intramuscular transfers can be determined regarding clinical improvement. Existing research on the most effective technique for anterior transfer of the ulnar nerve, whether subcutaneous or submuscular, has presented inconsistent findings. Unfortunately, the limited quality of studies and small sample sizes have hindered the determination of the most effective anterior ulnar nerve transfer technique for cubital tunnel syndrome [7].
Therefore, this study was conducted to evaluate the clinical outcomes of subcutaneous and intramuscular anterior ulnar nerve transfers in a substantial patient cohort, to provide robust and reliable data on the best approach.
Methods
This study included patients diagnosed with cubital tunnel syndrome who underwent anterior transposition of the ulnar nerve (subcutaneous or transmuscular) from 2016 to 2022. The exclusion criteria included patients with cubital tunnel deformity resulting from prior elbow injuries and those with recurrent cubital tunnel syndrome following previous surgical intervention. The minimum follow-up duration was 12 months.
Surgical procedure and postoperative protocol
Both surgical techniques were applied to the tourniquets. A longitudinal 10-12 cm incision at the medial side of the elbow was made to examine the ulnar nerve. Both techniques included release of the ligament strutter in the proximal region, excision of the intermuscular septum, and release of the Osborn ligament while preserving the ulnar nerve’s interarticular branch. In the subcutaneous technique, the nerve was advanced and positioned within the subcutaneous adipose tissue, with the fat being applied to the nerve and secured with absorbable sutures. The transmuscular approach involved repositioning the nerve in front and securing it beneath the fascia of the insertion site of the flexor and pronator muscles. The muscles were opened in a z-shaped pattern. The two ends of fascia were sutured with vicryl thread to provide unrestricted movement of the underlying nerve. Ultimately, the tourniquet was deflated, and bleeding was controlled with cautery.
In both techniques, the elbow was immobilized at a 90° angle with a splint, worn for one week, and sutures were removed after 14 days. The procedures were performed under general anesthesia by two experienced hand surgeons, each surgeon using one of the surgical techniques at a single orthopedic facility.
Evaluations
Demographic data, including age, sex, clinical signs and symptoms (such as pain, numbness, and paresthesia), and symptom duration, were collected from the patients’ files. Treatment outcomes at the latest follow-up were categorized as excellent, good, acceptable, or bad using the Wilson and Krout scores [8]. Surgical complications, such as surgical site infection and hematoma, were also documented.
Statistical analysis
The data were analyzed using SPSS software, version 22. Descriptive statistics are presented as Mean±SD for quantitative variables and frequency numbers with percentages for qualitative variables. Statistical tests, including chi-square, Fisher’s exact test, Kruskal-Wallis test, and Mann-Whitney U test were used to compare and determine the relationship between variables. A significance level of P≤0.05 was considered statistically significant.
Results
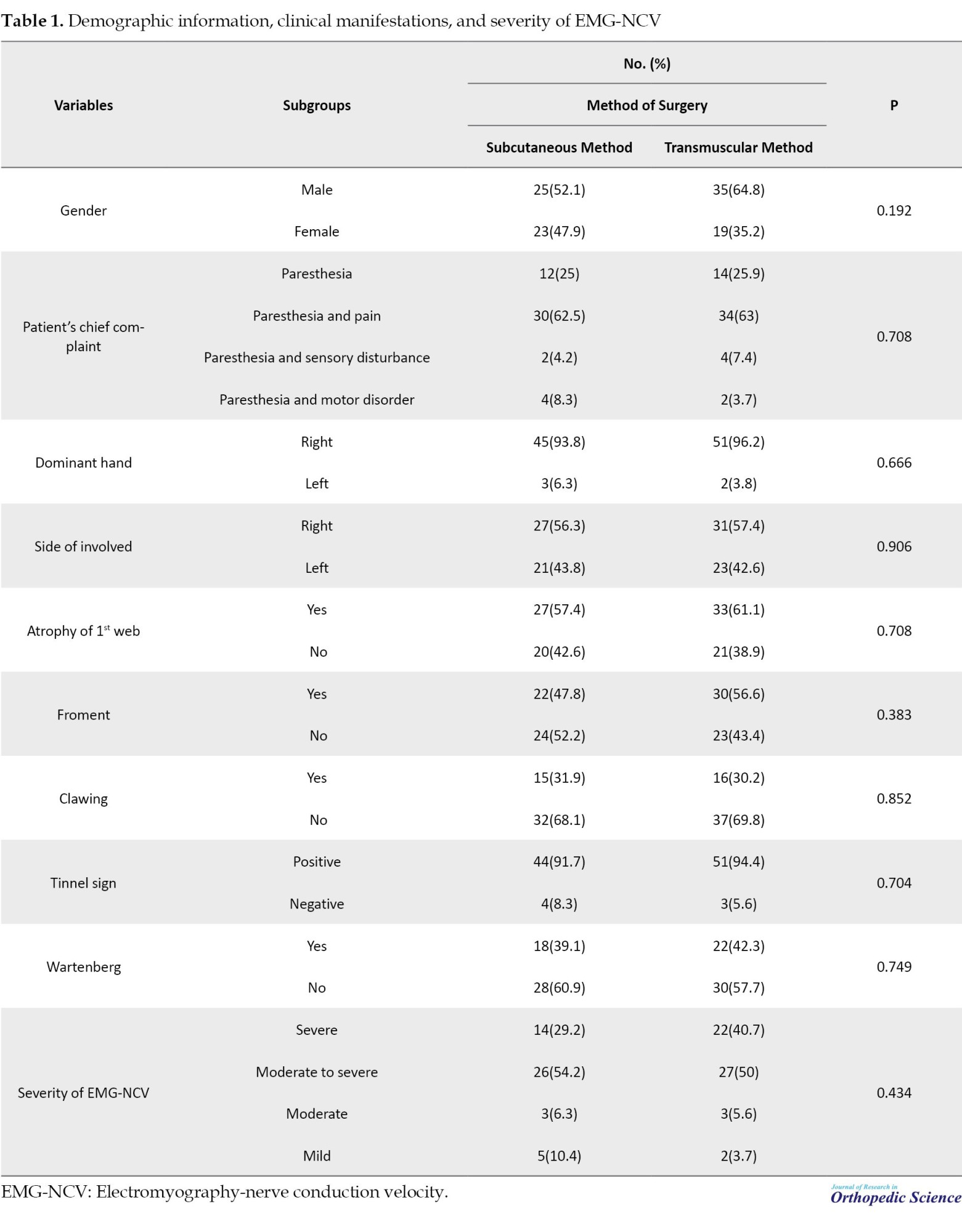
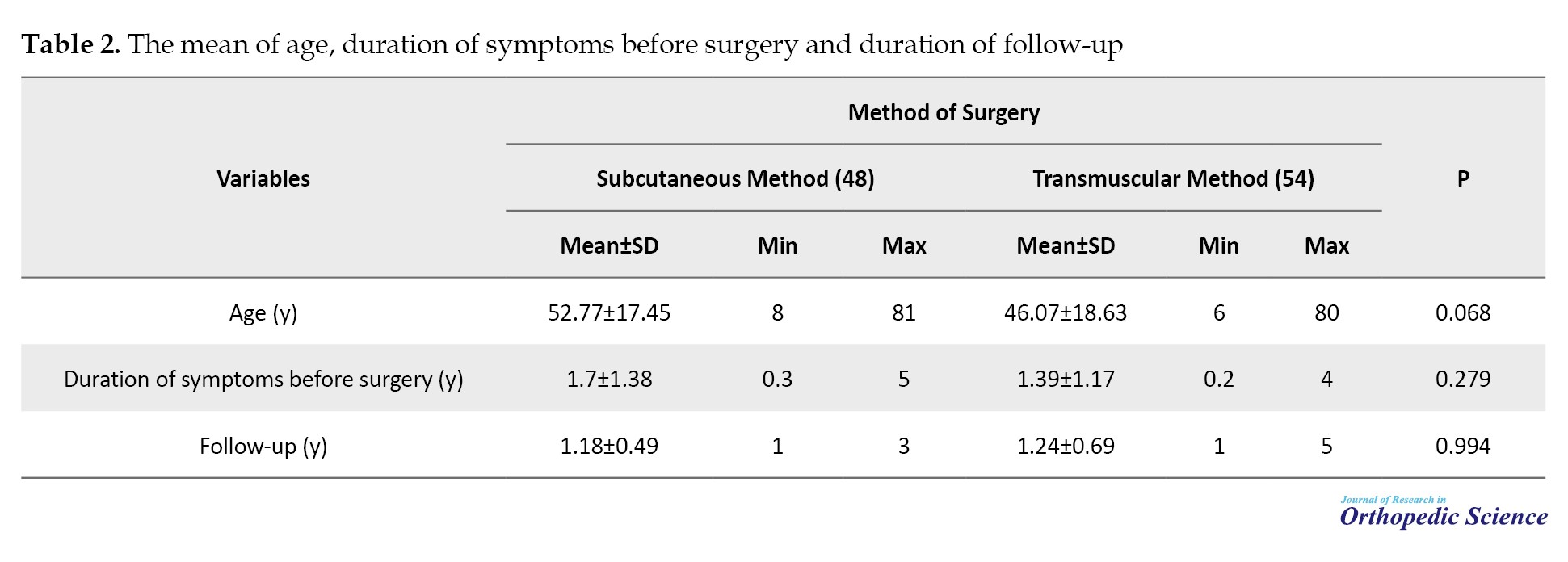
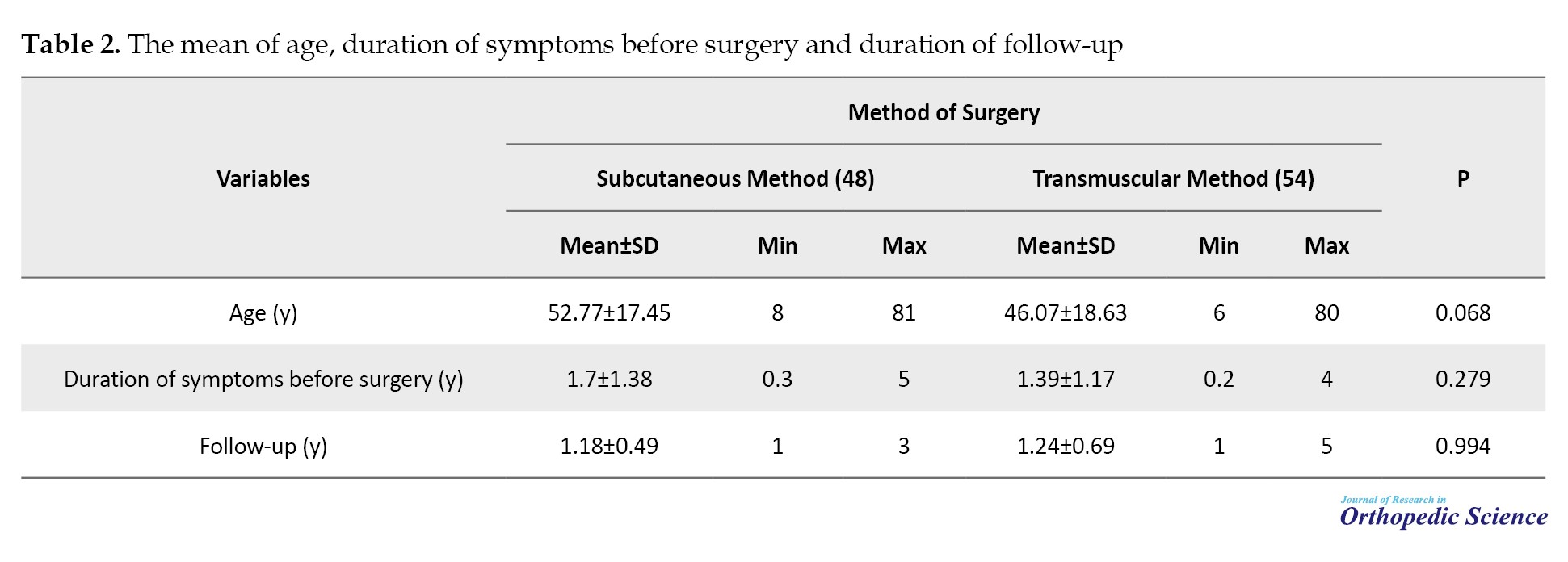
A total of 98 individuals were included in the study, and 102 upper limbs were analyzed. Among these patients, four had bilateral involvement, and in two cases, a different surgical approach was utilized for each limb. Fifty-eight individuals (59.2%) were men. The average age was 50.43 years, with a standard deviation of 18.10. Surgical procedures were performed using the transmuscular method in 54 patients (52.9%), while the remaining patients underwent surgery using the subcutaneous method. Tables 1 and 2 summarize both surgical approaches’ demographic characteristics, clinical manifestation, and details.
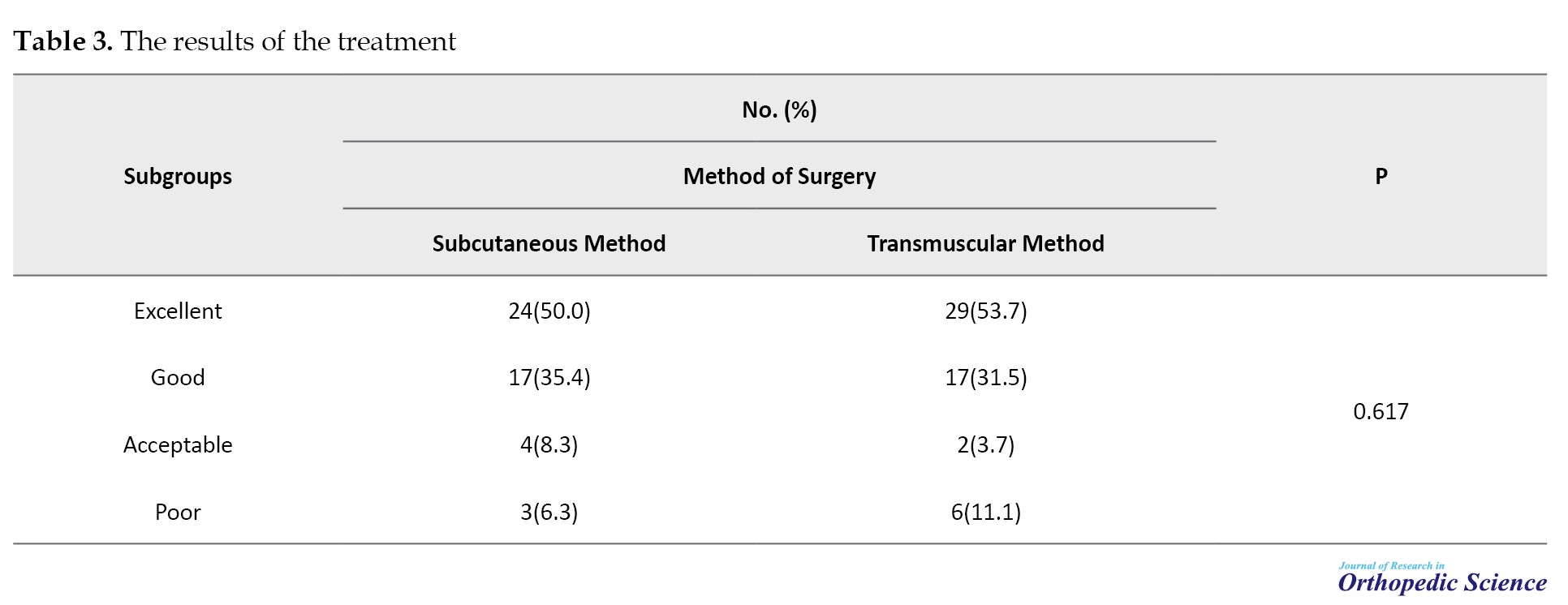
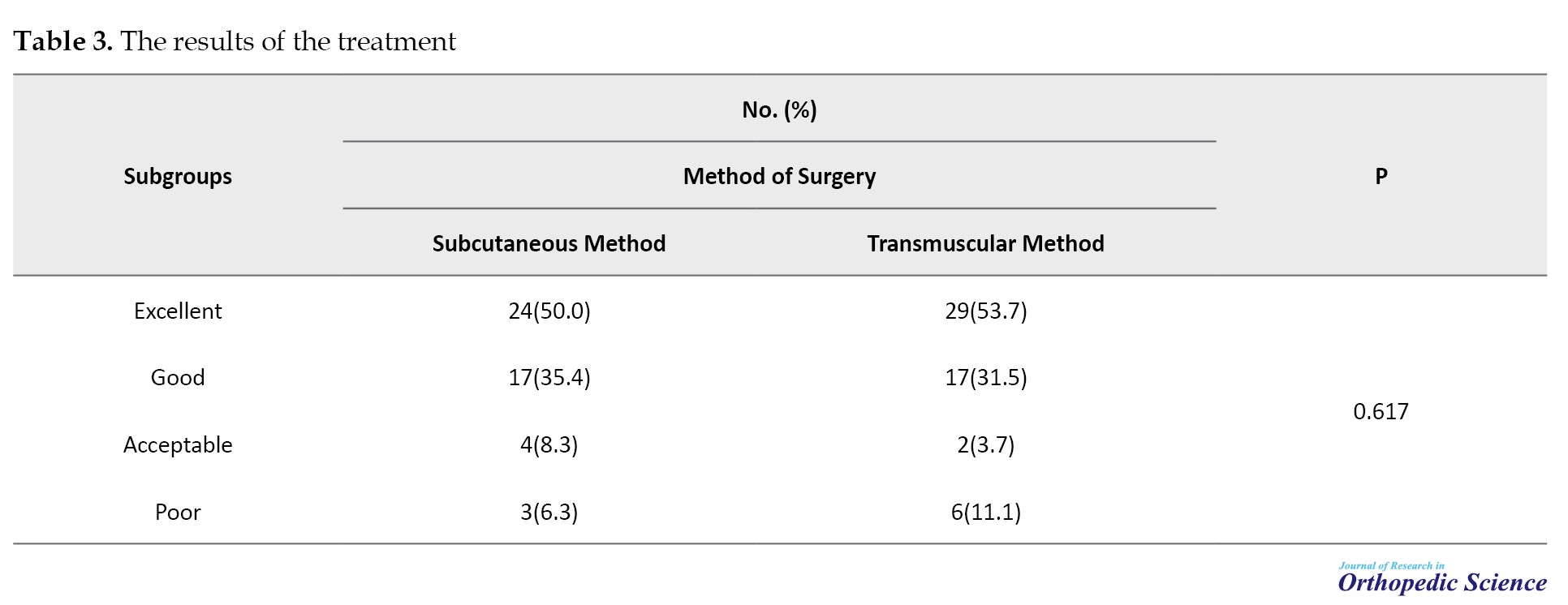
The analysis revealed no statistically significant correlation between treatment outcomes and surgical approach (P=0.617) (Table 3).
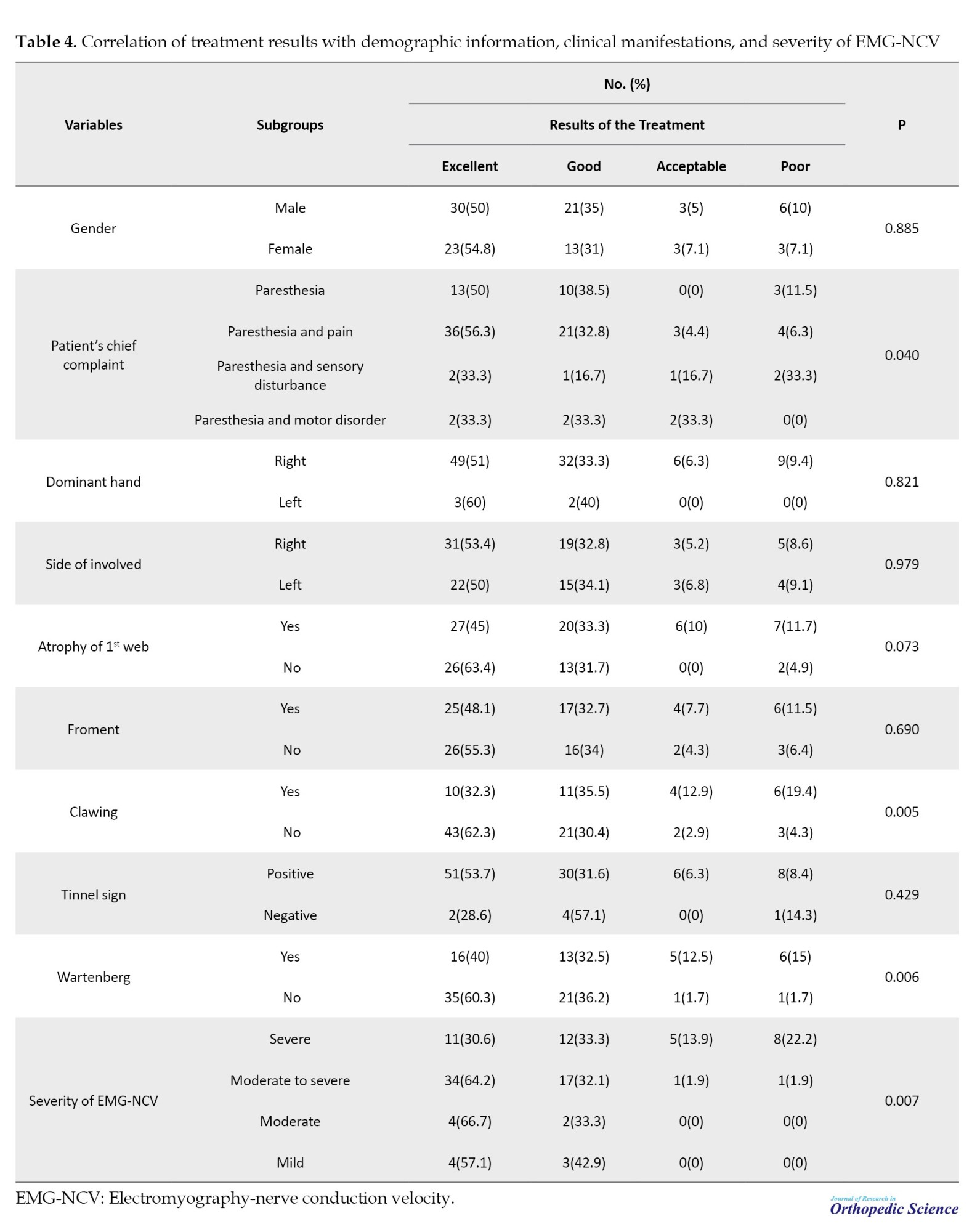
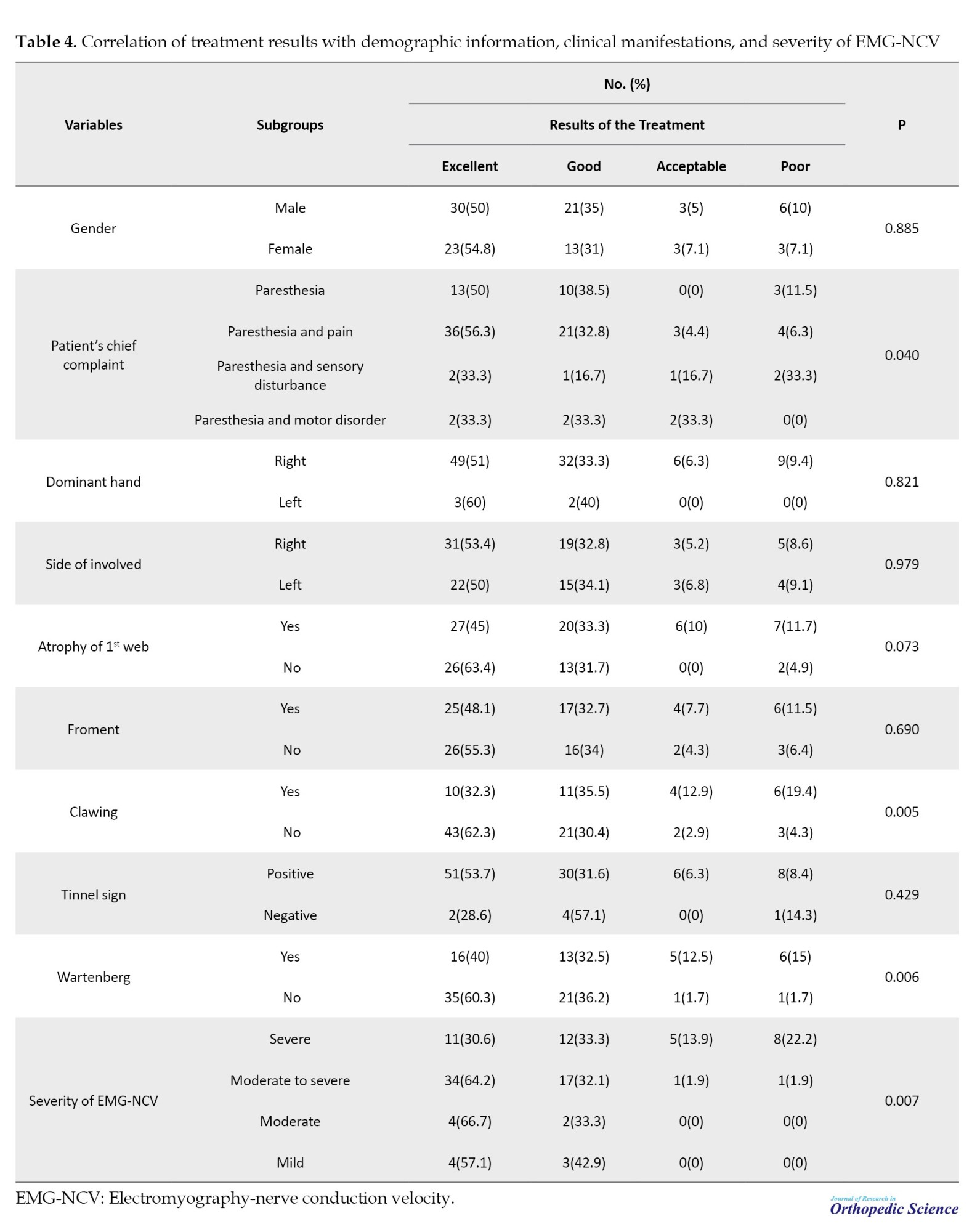
However, significant associations were found between treatment outcomes and the patient’s primary complaint, Clawing, Wartenberg’s sign, and severity of electromyography nerve conduction velocity (EMG-NCV) (Table 4).
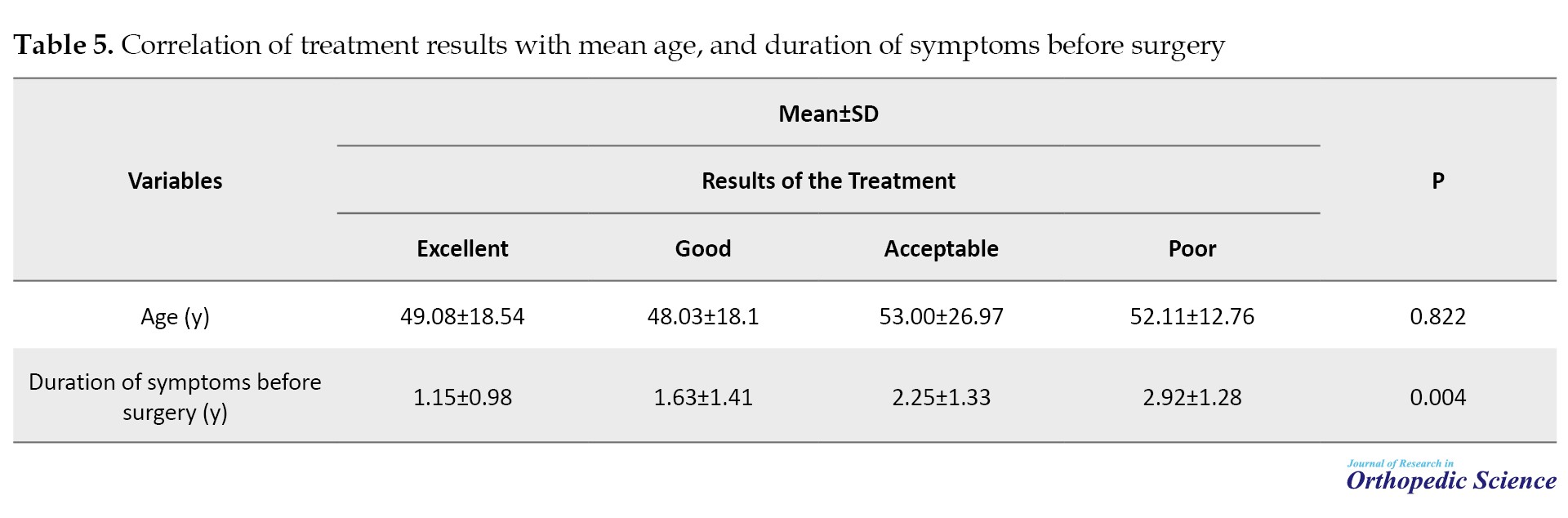
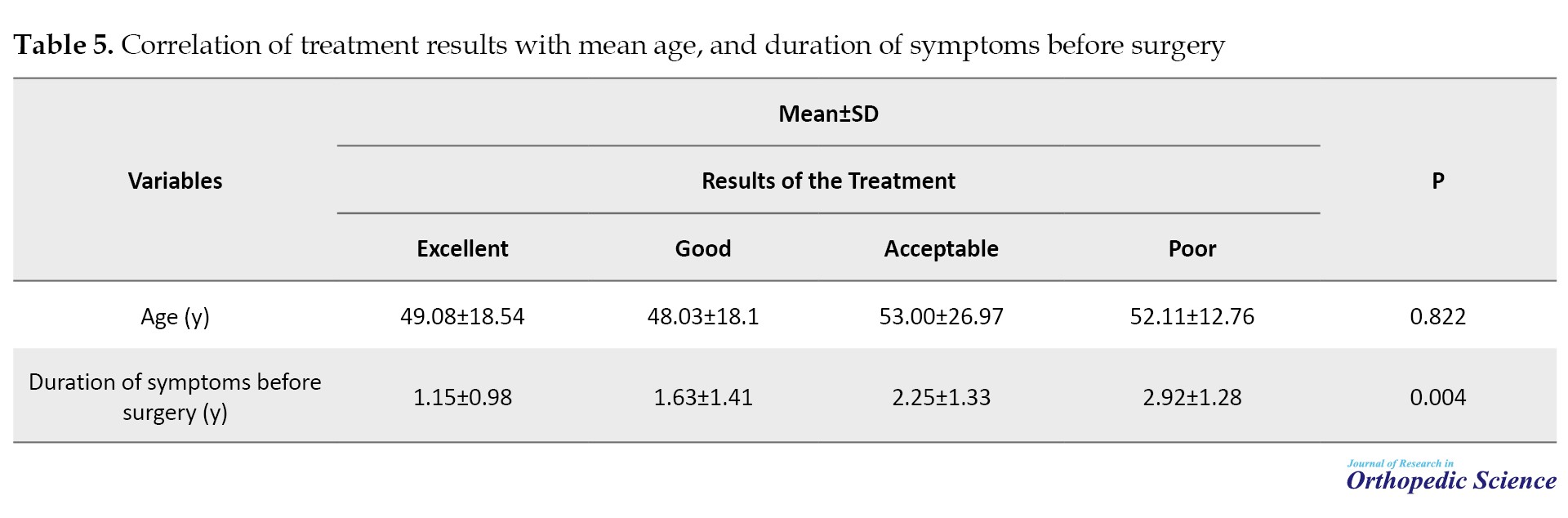
Furthermore, a statistically significant relationship (P=0.004) was observed between the duration of symptoms before surgery and treatment outcomes (Table 5).
Discussion
Several studies have compared subcutaneous and transmuscular methods with anterior ulnar nerve transposition, revealing disparities in outcomes [9, 10]. While some studies have demonstrated the superiority of one method over the other [2, 11-14], others have shown conflicting results; some favor the subcutaneous approach [2, 11, 13], and others have shown conflicting results [12, 14].
In our study, both surgical groups exhibited similar characteristics, and no statistically significant difference was observed in treatment outcomes between the two surgical methods. Therefore, both surgical methods yielded comparable results. In a comprehensive review and meta-analysis, Liu et al. concluded that insufficient data is available to determine the optimal anterior transposition approach for treating cubital tunnel syndrome. Their research results suggested that both subcutaneous and submuscular anterior transposition techniques may have comparable efficacy in treating individuals with cubital tunnel syndrome [1]. However, the incidence of adverse events was significantly lower in a subcutaneous group than in the submuscular group. Boers et al., in a prospective study, compared anterior transposition of the ulnar nerve between primary and revision groups using the submuscular approach. They reported good treatment outcomes (Likert 1 and 2) at 6 weeks, 67% in the revision group and 85% in the primary group [15]. The current study found that the combined percentage of excellent and good outcomes for transmuscular therapy was 85.2%, consistent with the results of two previous studies. According to Wever et al., who evaluated the effects of submuscular transposition with musculo-fascial lengthening for chronic or recurrent cubital tunnel syndrome, 21 of 34 patients showed improvement following surgery [16].
In Huang et al.’s study, patients with anterior subcutaneous transfer of the ulnar nerve achieved excellent treatment outcomes in 58% of cases, good outcomes in 25%, fair outcomes in 11%, and poor outcomes in 6%. The percentage of excellence and goodness was 83% [17]. In the current study, the percentage of excellence and goodness was 85.4%, indicating that the results of both investigations were comparable.
Our results also suggest that motor and sensory disorders before surgery are associated with worse treatment outcomes, and this association was statistically significant. The occurrence of clawing and Wartenberg’s sign strongly correlates with unfavorable treatment outcomes. Additionally, as indicated by EMG-NCV reports, severe nerve involvement was associated with less favorable treatment outcomes. Atrophy in the first web was related to poorer outcomes; although this relationship was not statistically significant, it was near the significance threshold. Moreover, a statistically significant correlation was observed between the length of symptoms before surgery and treatment outcome, with a longer duration of symptoms leading to worse results.
Compared to Huang et al.’s research, patients with fair and lousy treatment outcomes exhibited advanced age, reduced nerve conduction velocity, and diminished action potential amplitude. These findings indicate that the anterior subcutaneous transposition of the ulnar nerve is a reliable and secure method for managing moderate to severe cubital tunnel syndrome. Therapy success may be influenced by factors, such as initial severity of the condition, patient age, and specific electrophysiological measurements [17].
Conclusion
The present study compared the outcomes of cubital syndrome treatment using two surgical methods: Subcutaneous and transmuscular anterior transposition of the ulnar nerve. Our results are consistent with those of previous studies, indicating similar treatment outcomes for both methods. Therefore, the surgeon can select either method based on the patient’s condition. Factors such as sensory and motor impairments, clawing, Wartenberg sign, atrophy of the first web, the extent of nerve involvement in EMG-NCV, and the prolonged duration of clinical symptoms before surgery impacted treatment outcomes. Therefore, patients and orthopedic surgeons should be encouraged to pursue early surgical interventions to manage cubital syndrome.
An outstanding aspect of this research was its substantial sample size, which allowed for a comprehensive comparison of two surgical techniques for anterior transposition of the ulnar nerve. In addition, this study investigated the correlation between clinical observations and treatment outcomes. A significant limitation of the present investigation was its retrospective design, which hindered exact control over the enrolled patients and the absence of frequent and detailed follow-up assessments. Another drawback was the absence of a thorough analysis and comparison of the postoperative complications between the two groups.
Ethical Considerations
Compliance with ethical guidelines
The Institutional Ethics Board of Iran University of Medical Sciences, Tehran, Iran approved this retrospective cohort study (Code: IR.IUMS.REC.1402.216).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to those who contributed to the present research project, especially the esteemed professors and personnel of Shafayahyaeian Hospital in Tehran Province, Iran.
References
Cubital tunnel syndrome, also known as ulnar neuropathy at the elbow, is the second peripheral nerve entrapment neuropathy after carpal tunnel syndrome [1-5]. The prevalence of cubital tunnel syndrome in men is twice as high as in women, with an annual incidence of approximately twenty-five cases per 100000 individuals [1]. The population has an incidence rate of up to 1% [6].
Various surgical techniques have been established to treat ulnar neuropathy at the elbow, such as simple decompressionmpression, anterior transposition of the ulnar nerve, and medial epicondylectomy [7]. Anterior transposition of the ulnar nerve involves relocating the nerve either subcutaneously, within the muscle, or beneath it [1]. However, it is unclear whether the comparative efficacy of subcutaneous and intramuscular transfers can be determined regarding clinical improvement. Existing research on the most effective technique for anterior transfer of the ulnar nerve, whether subcutaneous or submuscular, has presented inconsistent findings. Unfortunately, the limited quality of studies and small sample sizes have hindered the determination of the most effective anterior ulnar nerve transfer technique for cubital tunnel syndrome [7].
Therefore, this study was conducted to evaluate the clinical outcomes of subcutaneous and intramuscular anterior ulnar nerve transfers in a substantial patient cohort, to provide robust and reliable data on the best approach.
Methods
This study included patients diagnosed with cubital tunnel syndrome who underwent anterior transposition of the ulnar nerve (subcutaneous or transmuscular) from 2016 to 2022. The exclusion criteria included patients with cubital tunnel deformity resulting from prior elbow injuries and those with recurrent cubital tunnel syndrome following previous surgical intervention. The minimum follow-up duration was 12 months.
Surgical procedure and postoperative protocol
Both surgical techniques were applied to the tourniquets. A longitudinal 10-12 cm incision at the medial side of the elbow was made to examine the ulnar nerve. Both techniques included release of the ligament strutter in the proximal region, excision of the intermuscular septum, and release of the Osborn ligament while preserving the ulnar nerve’s interarticular branch. In the subcutaneous technique, the nerve was advanced and positioned within the subcutaneous adipose tissue, with the fat being applied to the nerve and secured with absorbable sutures. The transmuscular approach involved repositioning the nerve in front and securing it beneath the fascia of the insertion site of the flexor and pronator muscles. The muscles were opened in a z-shaped pattern. The two ends of fascia were sutured with vicryl thread to provide unrestricted movement of the underlying nerve. Ultimately, the tourniquet was deflated, and bleeding was controlled with cautery.
In both techniques, the elbow was immobilized at a 90° angle with a splint, worn for one week, and sutures were removed after 14 days. The procedures were performed under general anesthesia by two experienced hand surgeons, each surgeon using one of the surgical techniques at a single orthopedic facility.
Evaluations
Demographic data, including age, sex, clinical signs and symptoms (such as pain, numbness, and paresthesia), and symptom duration, were collected from the patients’ files. Treatment outcomes at the latest follow-up were categorized as excellent, good, acceptable, or bad using the Wilson and Krout scores [8]. Surgical complications, such as surgical site infection and hematoma, were also documented.
Statistical analysis
The data were analyzed using SPSS software, version 22. Descriptive statistics are presented as Mean±SD for quantitative variables and frequency numbers with percentages for qualitative variables. Statistical tests, including chi-square, Fisher’s exact test, Kruskal-Wallis test, and Mann-Whitney U test were used to compare and determine the relationship between variables. A significance level of P≤0.05 was considered statistically significant.
Results
A total of 98 individuals were included in the study, and 102 upper limbs were analyzed. Among these patients, four had bilateral involvement, and in two cases, a different surgical approach was utilized for each limb. Fifty-eight individuals (59.2%) were men. The average age was 50.43 years, with a standard deviation of 18.10. Surgical procedures were performed using the transmuscular method in 54 patients (52.9%), while the remaining patients underwent surgery using the subcutaneous method. Tables 1 and 2 summarize both surgical approaches’ demographic characteristics, clinical manifestation, and details.
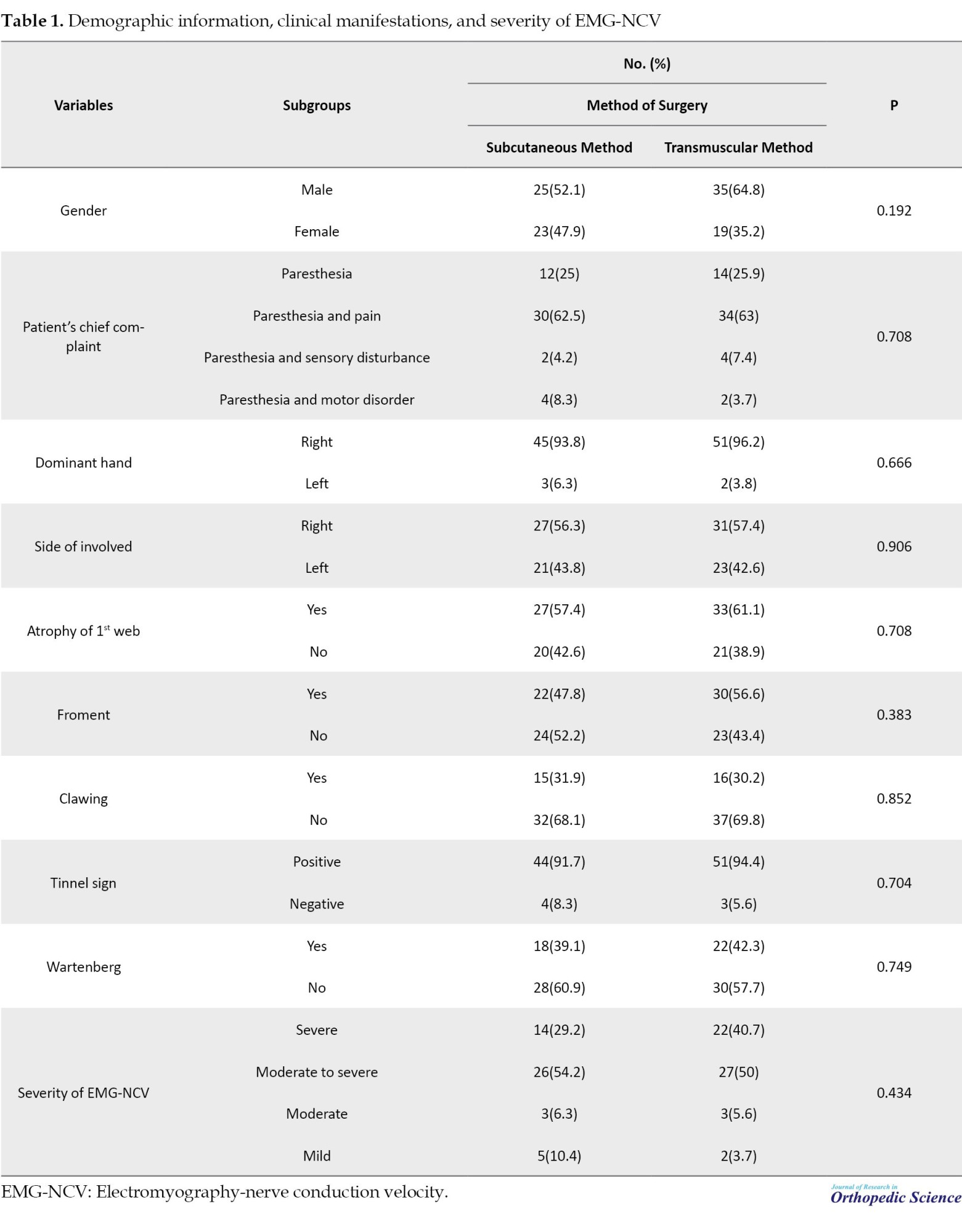
The analysis revealed no statistically significant correlation between treatment outcomes and surgical approach (P=0.617) (Table 3).
However, significant associations were found between treatment outcomes and the patient’s primary complaint, Clawing, Wartenberg’s sign, and severity of electromyography nerve conduction velocity (EMG-NCV) (Table 4).
Furthermore, a statistically significant relationship (P=0.004) was observed between the duration of symptoms before surgery and treatment outcomes (Table 5).
Discussion
Several studies have compared subcutaneous and transmuscular methods with anterior ulnar nerve transposition, revealing disparities in outcomes [9, 10]. While some studies have demonstrated the superiority of one method over the other [2, 11-14], others have shown conflicting results; some favor the subcutaneous approach [2, 11, 13], and others have shown conflicting results [12, 14].
In our study, both surgical groups exhibited similar characteristics, and no statistically significant difference was observed in treatment outcomes between the two surgical methods. Therefore, both surgical methods yielded comparable results. In a comprehensive review and meta-analysis, Liu et al. concluded that insufficient data is available to determine the optimal anterior transposition approach for treating cubital tunnel syndrome. Their research results suggested that both subcutaneous and submuscular anterior transposition techniques may have comparable efficacy in treating individuals with cubital tunnel syndrome [1]. However, the incidence of adverse events was significantly lower in a subcutaneous group than in the submuscular group. Boers et al., in a prospective study, compared anterior transposition of the ulnar nerve between primary and revision groups using the submuscular approach. They reported good treatment outcomes (Likert 1 and 2) at 6 weeks, 67% in the revision group and 85% in the primary group [15]. The current study found that the combined percentage of excellent and good outcomes for transmuscular therapy was 85.2%, consistent with the results of two previous studies. According to Wever et al., who evaluated the effects of submuscular transposition with musculo-fascial lengthening for chronic or recurrent cubital tunnel syndrome, 21 of 34 patients showed improvement following surgery [16].
In Huang et al.’s study, patients with anterior subcutaneous transfer of the ulnar nerve achieved excellent treatment outcomes in 58% of cases, good outcomes in 25%, fair outcomes in 11%, and poor outcomes in 6%. The percentage of excellence and goodness was 83% [17]. In the current study, the percentage of excellence and goodness was 85.4%, indicating that the results of both investigations were comparable.
Our results also suggest that motor and sensory disorders before surgery are associated with worse treatment outcomes, and this association was statistically significant. The occurrence of clawing and Wartenberg’s sign strongly correlates with unfavorable treatment outcomes. Additionally, as indicated by EMG-NCV reports, severe nerve involvement was associated with less favorable treatment outcomes. Atrophy in the first web was related to poorer outcomes; although this relationship was not statistically significant, it was near the significance threshold. Moreover, a statistically significant correlation was observed between the length of symptoms before surgery and treatment outcome, with a longer duration of symptoms leading to worse results.
Compared to Huang et al.’s research, patients with fair and lousy treatment outcomes exhibited advanced age, reduced nerve conduction velocity, and diminished action potential amplitude. These findings indicate that the anterior subcutaneous transposition of the ulnar nerve is a reliable and secure method for managing moderate to severe cubital tunnel syndrome. Therapy success may be influenced by factors, such as initial severity of the condition, patient age, and specific electrophysiological measurements [17].
Conclusion
The present study compared the outcomes of cubital syndrome treatment using two surgical methods: Subcutaneous and transmuscular anterior transposition of the ulnar nerve. Our results are consistent with those of previous studies, indicating similar treatment outcomes for both methods. Therefore, the surgeon can select either method based on the patient’s condition. Factors such as sensory and motor impairments, clawing, Wartenberg sign, atrophy of the first web, the extent of nerve involvement in EMG-NCV, and the prolonged duration of clinical symptoms before surgery impacted treatment outcomes. Therefore, patients and orthopedic surgeons should be encouraged to pursue early surgical interventions to manage cubital syndrome.
An outstanding aspect of this research was its substantial sample size, which allowed for a comprehensive comparison of two surgical techniques for anterior transposition of the ulnar nerve. In addition, this study investigated the correlation between clinical observations and treatment outcomes. A significant limitation of the present investigation was its retrospective design, which hindered exact control over the enrolled patients and the absence of frequent and detailed follow-up assessments. Another drawback was the absence of a thorough analysis and comparison of the postoperative complications between the two groups.
Ethical Considerations
Compliance with ethical guidelines
The Institutional Ethics Board of Iran University of Medical Sciences, Tehran, Iran approved this retrospective cohort study (Code: IR.IUMS.REC.1402.216).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors express their gratitude to those who contributed to the present research project, especially the esteemed professors and personnel of Shafayahyaeian Hospital in Tehran Province, Iran.
References
- Liu CH, Chen CX, Xu J, Wang HL, Ke XB, Zhuang ZY, et al. Anterior subcutaneous versus submuscular transposition of the ulnar nerve for cubital tunnel syndrome: A systematic review and meta-analysis. Plos One. 2015; 10(6):e0130843. [DOI:10.1371/journal.pone.0130843] [PMID] [PMCID]
- Jaddue DA, Saloo SA, Sayed-Noor AS. Subcutaneous vs submuscular ulnar nerve transposition in moderate cubital tunnel syndrome. Open Orthop J. 2009; 3:78-82. [DOI:10.2174/1874325000903010078] [PMID] [PMCID]
- Yahya A, Malarkey AR, Eschbaugh RL, Bamberger HB. Trends in the surgical treatment for cubital tunnel syndrome: A survey of members of the American society for surgery of the hand. Hand. 2018; 13(5):516-521. [DOI:10.1177/1558944717725377] [PMID] [PMCID]
- Dowdle SB, Chalmers PN. Management of the ulnar nerve in throwing athletes. Curr Rev Musculoskelet Med. 2020; 13(4):449-56. [DOI:10.1007/s12178-020-09639-7] [PMID] [PMCID]
- Mitchell J, Dunn JC, Kusnezov N, Bader J, Ipsen DF, Forthman CL, et al. The effect of operative technique on ulnar nerve strain following surgery for cubital tunnel syndrome. Hand. 2015; 10(4):707-11. [DOI:10.1007/s11552-015-9770-y] [PMID] [PMCID]
- Izadpanah A, Gibbs C, Spinner RJ, Kakar S. Comparison of in situ versus subcutaneous versus submuscular transpositions in the management of mcgowan stage III cubital tunnel syndrome. Hand. 2021; 16(1):45-9. [DOI:10.1177/1558944719831387] [PMID] [PMCID]
- Liu CH, Wu SQ, Ke XB, Wang HL, Chen CX, Lai ZL, et al. Subcutaneous versus submuscular anterior transposition of the ulnar nerve for cubital tunnel syndrome: A systematic review and meta-analysis of randomized controlled trials and observational studies. Medicine. 2015; 94(29):e1207. [DOI:10.1097/MD.0000000000001207] [PMID] [PMCID]
- Schnabl SM, Kisslinger F, Schramm A, Dragu A, Kneser U, Unglaub F, et al. Subjective outcome, neurophysiological investigations, postoperative complications and recurrence rate of partial medial epicondylectomy in cubital tunnel syndrome. Arch Orthop Trauma Surg. 2011; 131(8):1027-33. [DOI:10.1007/s00402-010-1250-9] [PMID]
- Gaspar MP, Gorica Z, Osterman AL, Culp RW, Kane PM. Anterior subcutaneous versus submuscular transposition of the ulnar nerve for idiopathic cubital tunnel syndrome: A matched retrospective comparative study: Level 4 evidence. J Hand Surg. 2018; 43(9):S10-1. [DOI:10.1016/j.jhsa.2018.06.039]
- Charles YP, Coulet B, Rouzaud JC, Daures JP, Chammas M. Comparative clinical outcomes of submuscular and subcutaneous transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Am. 2009; 34(5):866-74. [DOI:10.1016/j.jhsa.2009.01.008] [PMID]
- Sorg H, Krämer R, Reinke JM, Knobloch K. Surgical outcome of cubital tunnel syndrome using the MHQ and DASH: A retrospective patient-reported assessment. J Surg Oper Care. 2015; 1(1):103. [DOI:10.15744/2455-7617.1.103]
- Zarezadeh A, Shemshaki H, Nourbakhsh M, Etemadifar MR, Moeini M, Mazoochian F. Comparison of anterior subcutaneous and submuscular transposition of ulnar nerve in treatment of cubital tunnel syndrome: A prospective randomized trial. J Res Med Sci. 2012; 17(8):745-9. [PMID]
- Stuffer M, Jungwirth W, Hussl H, Schmutzhardt E. Subcutaneous or submuscular anterior transposition of the ulnar nerve? J Hand Surg. 1992; 17(3):248-50. [DOI:10.1016/0266-7681(92)90107-D]
- Lee SK, Sharma S, Silver BA, Kleinman G, Hausman MR. Submuscular versus subcutaneous anterior ulnar nerve transposition: A rat histologic study. J Hand Surg Am. 2009; 34(10):1811-4. [DOI:10.1016/j.jhsa.2009.08.007] [PMID]
- Boers N, Buijnsters ZA, Boer-Vreeke K, Wever N, Coert JH, de Ruiter GCW. Submuscular transposition of the ulnar nerve for persistent or recurrent cubital tunnel syndrome: Results of a prospective case series. J Plast Reconstr Aesthet Surg. 2022; 75(9):3260-8. [DOI:10.1016/j.bjps.2022.04.045] [PMID]
- Wever N, de Ruiter GCW, Coert JH. Submuscular transposition with musculofascial lengthening for persistent or recurrent cubital tunnel syndrome in 34 patients. J Hand Surg Eur Vol. 2018; 43(3):310-5. [DOI:10.1177/1753193417729602] [PMID]
- Huang W, Zhang PX, Peng Z, Xue F, Wang TB, Jiang BG. Anterior subcutaneous transposition of the ulnar nerve improves neurological function in patients with cubital tunnel syndrome. Neural Regen Res. 2015; 10(10):1690-5. [DOI:10.4103/1673-5374.167770] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2022/02/13 | Accepted: 2023/03/14 | Published: 2023/05/8
Received: 2022/02/13 | Accepted: 2023/03/14 | Published: 2023/05/8
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |