Volume 9, Issue 4 (11-2022)
JROS 2022, 9(4): 239-248 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdolahzadeh B, Tabrizian P, Baradaran Jamili A, Bahaeddini M R. Pediatric Talus Head Fracture: A Case Report. JROS 2022; 9 (4) :239-248
URL: http://jros.iums.ac.ir/article-1-2226-en.html
URL: http://jros.iums.ac.ir/article-1-2226-en.html
1- Bone and Joint Reconstruction Research Center, Department of orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1729 kb]
(196 Downloads)
| Abstract (HTML) (728 Views)
Full-Text: (325 Views)
1. Introduction
Talus fractures are extremely uncommon in children and occur five times less frequently than in adults. This discrepancy can be attributed to the fact that children’s bones are more elastic and can withstand greater forces before fracturing. The most common mechanism of injury for talus fractures in children involves the talus axial loading against the anterior tibia during foot dorsiflexion [1, 2]. Such injuries in children are often associated with high-energy trauma, including high-altitude falls, car accidents, or sports injuries.
Among the fractures in the talus bone, the talar neck fracture predominates, followed by fractures in the talar body, and rarely observed, fractures in the talar head [3, 4].
Untreated talus fractures can lead to serious complications, such as avascular necrosis and osteoarthritis. Therefore, a high level of clinical suspicion is necessary to avoid missing these fractures, especially when they have minimal displacement. Treatment protocols should follow standard methods to prevent complications and promote proper bone remodeling for future growth [1, 5]. In this study, we report a rare case of talus head fracture in an 8-year-old child, who presented to our hospital 12 days post-injury.
2. Case Presentation
The main complaints
An 8-year-old boy, who experienced trauma following a 10-meter fall into a well, presented to the Emergency Department of Shafa Yahyaian Hospital after a twelve-day delay in seeking medical attention with local tenderness, swelling, and pain in his right ankle complaint. The patient did not receive any medical treatment during this period before hospital admission.
Physical examination results
During the clinical examination, local tenderness and swelling, as well as the inability to bear weight on the right foot were found without any open wounds. We thoroughly examined other parts of skeletal and internal systems and we found no significant case.
Laboratory examinations
The laboratory examinations, including the assessment of vitamin D levels, did not reveal any abnormalities.
Imaging examinations
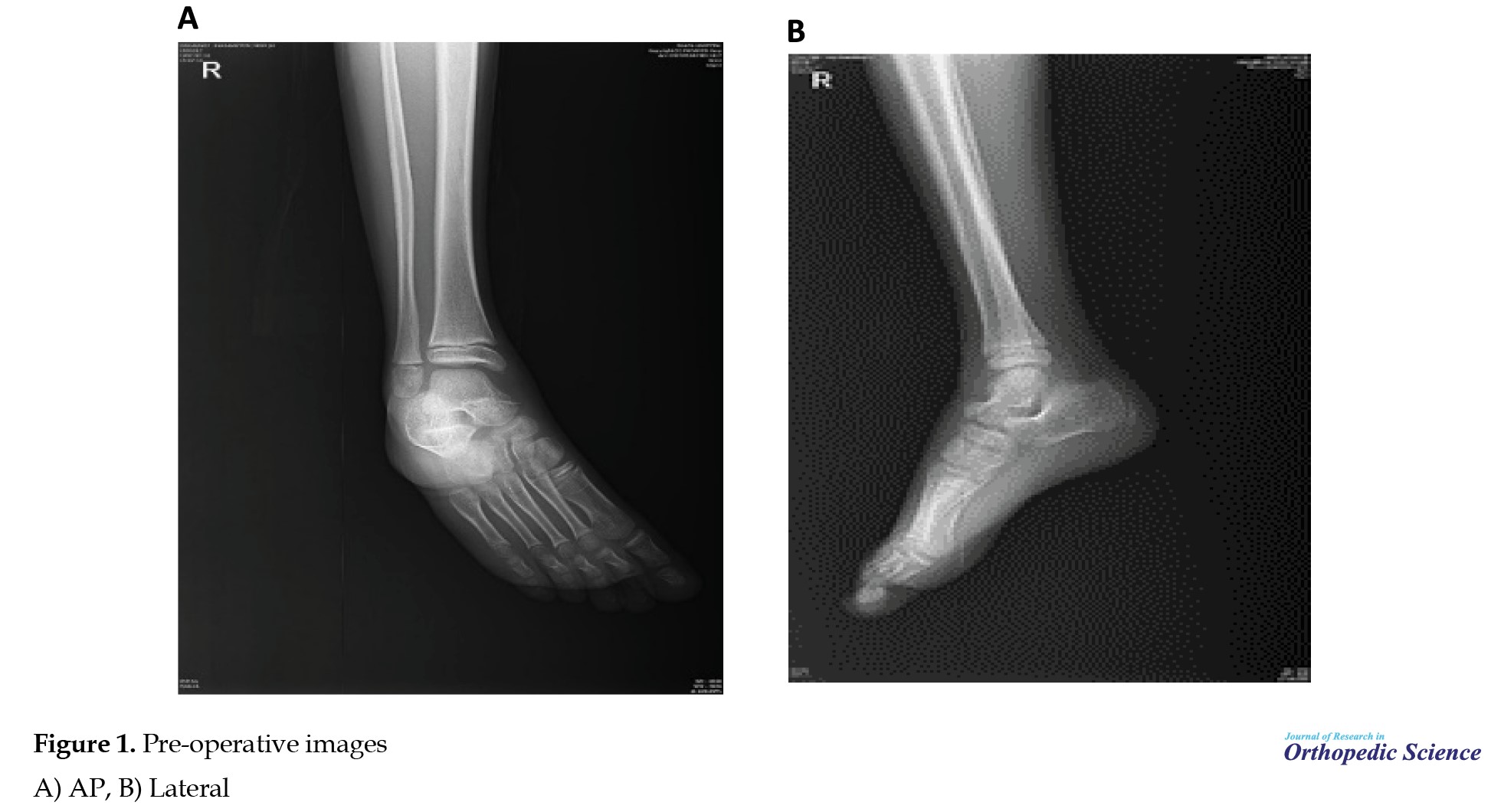
Following a comprehensive patient foot assessment through history taking, physical examination, and laboratory data, an x-ray was conducted on the right foot. The radiographic results revealed the presence of a talus head fracture (Figure 1). A computerized tomography (CT) scan was performed on the right ankle and showed that the patient had a talus head segmented fracture (Figure 2).
Final diagnosis
After taking the patient’s medical history, performing a precise physical examination, and assessing the images (x-ray and CT scan), the final diagnosis was a talus head segmented fracture.
Surgical approach
This operation was done with an anterior approach in such a way that he underwent general anesthesia, then in the supine position, a tourniquet was closed, and he underwent surgery after prep and drape. It should be noted that the duration of the tourniquet was 55 minutes.
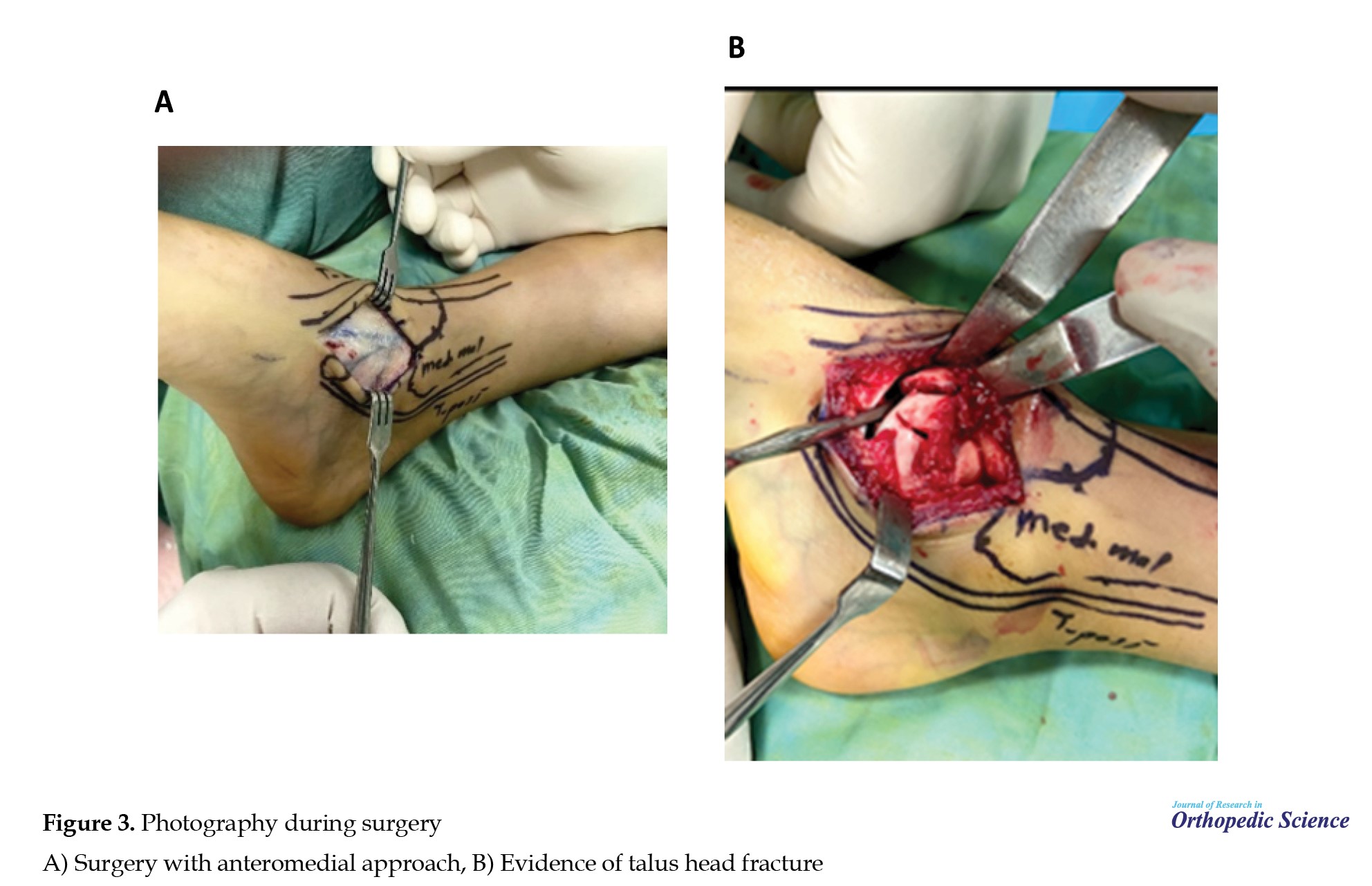
During surgery (Figure 3), a Herbert screw was used to promote compression and avoid fragment rotation, checked with C-Arm (Figure 4). Postoperatively, the ankle was protected with a lower leg cast.
Outcome and patient follow-up
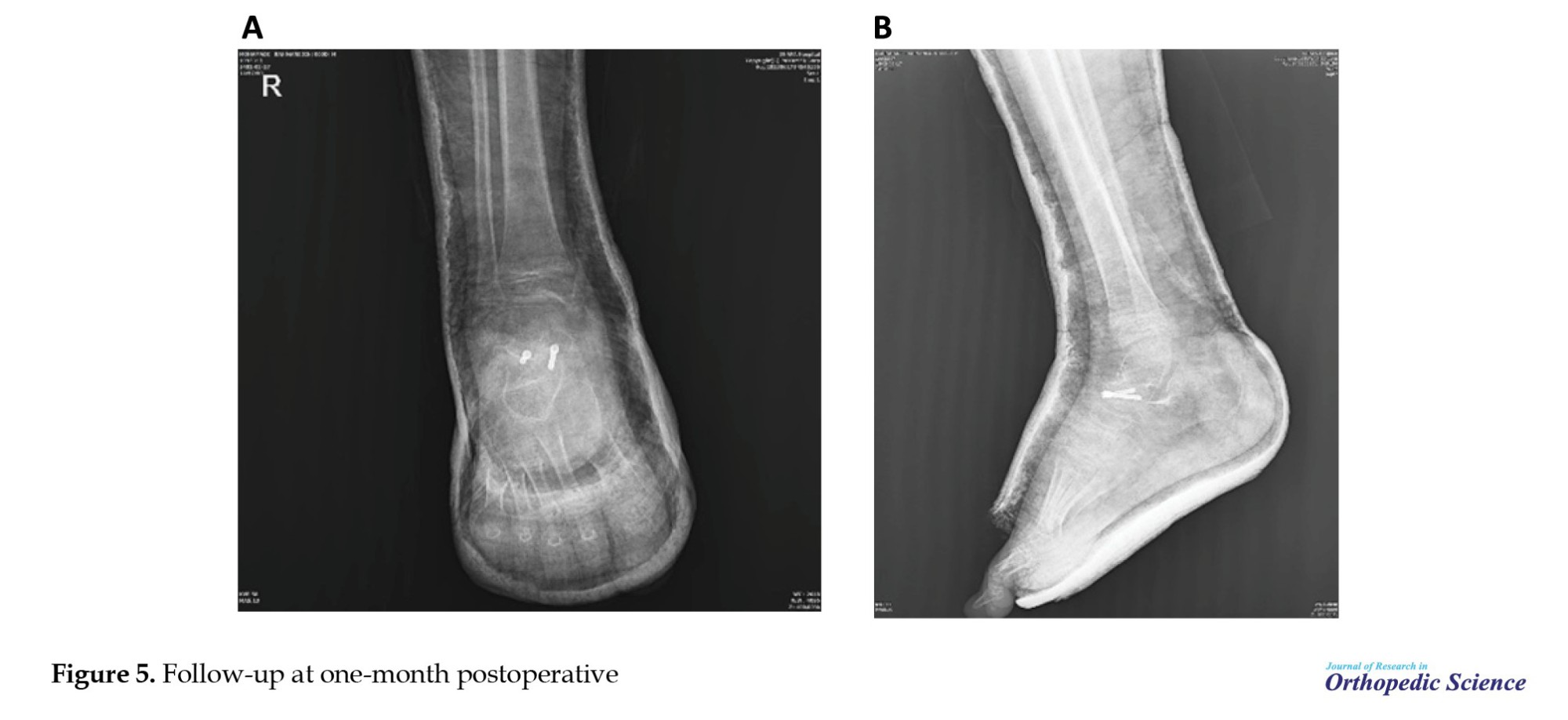
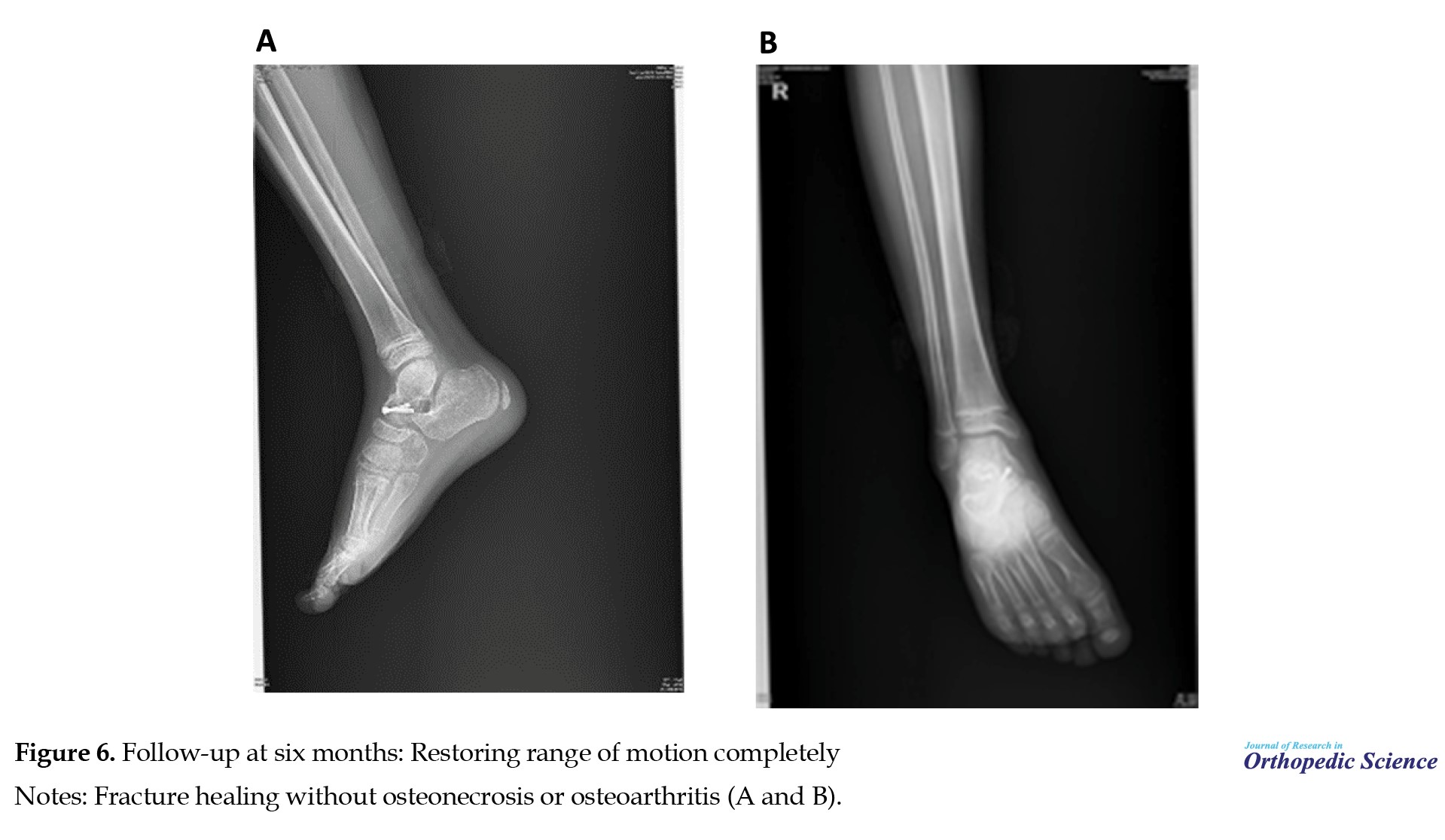
At the one-month follow-up, no wound complications were reported, and the patient revealed minimal pain (numeric rating scale [NRS]=2). Radiographs were taken (Figure 5). After six months, the young patient was practicing all sports without encountering any complications (NRS=0). Range of motion was fully restored and he reported no foot deformities or neurovascular deficits after the operation. Radiographs showed a :union: of the fracture without osteoarthritis or osteonecrosis (Figure 6).
Evaluation of the health status of the talus head when the screw was removed
In the seventh month after the surgery, after examining the patient screw removal was done. The assessment of the overall condition of the talus head after screw removal involves a comprehensive evaluation of various health-related factors affecting this specific anatomical region. This examination aims to determine the state of well-being and functionality of the talus head after the screw removal. Considering several indicators, such as range of motion, presence or absence of swelling, degree of tissue healing, extent of bone regeneration, and degree of pain experienced by the patient, this assessment aims to provide a comprehensive understanding of the health status of the talus head following screw extraction. A photograph taken seven months after surgery of the talus head fracture shows the proper :union: of the fractured area of the talus without swelling (Figure 7). Another examination was to check the patient’s range of motion (Figure 8). Figure 9 shows the full recovery of the range of motion of the patient’s ankle.
3. Discussion
Talar fractures are exceedingly rare during childhood, accounting for less than 1% of all fractures, with an estimated prevalence rate between 0.01% and 0.08%. Compared to adults, children experience talar fractures at a rate approximately five times lower [6, 7].
The severity of these fractures tends to be higher in older cases. Compared to children (under 12 years old) and adolescents (over 12 years old), Eberl et al. observed a higher prevalence of talar fractures in the latter group, possibly due to skeletal development. In younger children, the immature portion of the talus exhibits greater resistance to the fractures. Talar maturity typically occurs during adolescence, between the ages of 12 and 22. However, due to the absence of an epiphysis in the talus, determining its maturity is challenging. Therefore, the development of the talus is commonly assessed by the closure of metatarsals, which typically occurs between the ages of 14 and 21 years [5, 8]. The talus in children contains a substantial amount of cartilage tissue, which displays excellent elasticity. As age increases, the cartilage tissue proportion reduces. The ligaments and soft tissue surrounding the talus possess remarkable strength and extensibility, contributing to its significant impact resistance [9].
The talus fulfills a crucial biomechanical performance and is involved in the patient’s gait and walking patterns. Failure to properly reduce and stabilize a talus fracture can severely impair normal foot activity and function. Talus fractures are primarily caused by significant force, such as a traffic accident or a high fall, resulting in excessive dorsiflexion and ankle joint compression, ultimately leading to displacement, fracture, and separation [10, 11]. The mechanism of this trauma typically involves sudden dorsiflexion causing the talar head compression against the tibia anterior border, as first described by Anderson in 1919 [12]. Fractures of the talus can be categorized based on whether the head, neck, or body is involved, and further subdivisions can be made within the body. Various classification systems are employed to describe these fracture patterns and provide guidance for their management. Talar head fractures are not common talar fractures, accounting for 5%-10% of all talar fractures [12, 13].
Fractures of the head of the talus occur particularly at the talonavicular joint articular surface and may be accompanied by dislocation or subluxation of the talus as well as fractures of adjacent bones. No established classification system was observed to characterize this fracture, although two patterns have been identified, shear fractures and crush injuries of the articular surface with significant fragmentation [14]. Talar head fractures cause midfoot pain, focal tenderness and swelling over the talar head, and pain with motion at the midtarsal joint [15]. Radiographs of the foot are the most effective means of visualizing fractures of the talus head [17]. In this study, a patient presented with ankle pain and swelling following a fall from a height of 10 meters. After taking a thorough patient history and conducting a physical examination, an initial diagnosis of a talus fracture was made, prompting further investigation with radiographs. Subsequent imaging, including radiographs and a CT scan, confirmed the presence of a fracture involving the head of the talus.
Both non-displaced fractures of the talar head and surgically managing displaced fractures of the talar head have favorable outcomes in terms of patient recovery. The strong blood supply to the talar head contributes to its relatively positive prognosis compared to the talar neck and body. Non-displaced fractures of the talar head are treated conservatively, while surgical intervention is necessary for displaced fractures to realign the talonavicular joint and decrease the risk of osteonecrosis and osteoarthritis [14, 16, 17]. The complications, including avascular necrosis of the talus and osteoarthritis are related to the delicate blood supply and the extensive surface of cartilage in the body of the talus [17]. Talar osteonecrosis is typically caused by trauma to the delicate blood supply of the talus, with talar neck fractures being the most common etiology. Fracture of the talar head is another reason for talar osteonecrosis and osteoarthritis. Patients with talar osteonecrosis often experience progressive ankle pain and limited range of motion, and treatment options depend on the stage of the disease [18]. Despite advances in surgeries, complications following fractures are still common, including foot deformities, osteonecrosis, and post-traumatic osteoarthritis. Fractures and dislocations can lead to avascular necrosis of the talus, which typically occurs within a few weeks to 6 months after the injury [7, 19]. This condition can lead to significant disability and post-traumatic arthritis. In children with non-displaced talus fractures, the incidence of avascular necrosis can be 16%, which is significantly higher compared to adults [20]. However, this reported incidence can be due to initially overlooked and untreated fractures. Talus fractures can also lead to other complications, such as non:union:, mal:union:, loose bodies, infection, neuropraxia, and impaired wound healing [21].
In the past, immediate open reduction with internal fixation was suggested because it was believed that delayed surgery increased the risk factors. However, the more recent literature has found no significant association between the surgery timing and osteonecrosis or osteoarthritis development [18, 22-24].
If displaced fractures of the head or neck are not properly reduced, they can result in arthritis or secondary necrosis. However, in this particular case, the patient’s radiographs showed no signs of osteonecrosis or osteoarthritis during the one-month and six-month follow-up, indicating that the surgery was effective. We recommend the utilization of the anteromedial approach surgery as an effective treatment method for patients with segmented fractures of the talus head.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Talus fractures are extremely uncommon in children and occur five times less frequently than in adults. This discrepancy can be attributed to the fact that children’s bones are more elastic and can withstand greater forces before fracturing. The most common mechanism of injury for talus fractures in children involves the talus axial loading against the anterior tibia during foot dorsiflexion [1, 2]. Such injuries in children are often associated with high-energy trauma, including high-altitude falls, car accidents, or sports injuries.
Among the fractures in the talus bone, the talar neck fracture predominates, followed by fractures in the talar body, and rarely observed, fractures in the talar head [3, 4].
Untreated talus fractures can lead to serious complications, such as avascular necrosis and osteoarthritis. Therefore, a high level of clinical suspicion is necessary to avoid missing these fractures, especially when they have minimal displacement. Treatment protocols should follow standard methods to prevent complications and promote proper bone remodeling for future growth [1, 5]. In this study, we report a rare case of talus head fracture in an 8-year-old child, who presented to our hospital 12 days post-injury.
2. Case Presentation
The main complaints
An 8-year-old boy, who experienced trauma following a 10-meter fall into a well, presented to the Emergency Department of Shafa Yahyaian Hospital after a twelve-day delay in seeking medical attention with local tenderness, swelling, and pain in his right ankle complaint. The patient did not receive any medical treatment during this period before hospital admission.
Physical examination results
During the clinical examination, local tenderness and swelling, as well as the inability to bear weight on the right foot were found without any open wounds. We thoroughly examined other parts of skeletal and internal systems and we found no significant case.
Laboratory examinations
The laboratory examinations, including the assessment of vitamin D levels, did not reveal any abnormalities.
Imaging examinations
Following a comprehensive patient foot assessment through history taking, physical examination, and laboratory data, an x-ray was conducted on the right foot. The radiographic results revealed the presence of a talus head fracture (Figure 1). A computerized tomography (CT) scan was performed on the right ankle and showed that the patient had a talus head segmented fracture (Figure 2).
Final diagnosis
After taking the patient’s medical history, performing a precise physical examination, and assessing the images (x-ray and CT scan), the final diagnosis was a talus head segmented fracture.
Surgical approach
This operation was done with an anterior approach in such a way that he underwent general anesthesia, then in the supine position, a tourniquet was closed, and he underwent surgery after prep and drape. It should be noted that the duration of the tourniquet was 55 minutes.
During surgery (Figure 3), a Herbert screw was used to promote compression and avoid fragment rotation, checked with C-Arm (Figure 4). Postoperatively, the ankle was protected with a lower leg cast.
Outcome and patient follow-up
At the one-month follow-up, no wound complications were reported, and the patient revealed minimal pain (numeric rating scale [NRS]=2). Radiographs were taken (Figure 5). After six months, the young patient was practicing all sports without encountering any complications (NRS=0). Range of motion was fully restored and he reported no foot deformities or neurovascular deficits after the operation. Radiographs showed a :union: of the fracture without osteoarthritis or osteonecrosis (Figure 6).
Evaluation of the health status of the talus head when the screw was removed
In the seventh month after the surgery, after examining the patient screw removal was done. The assessment of the overall condition of the talus head after screw removal involves a comprehensive evaluation of various health-related factors affecting this specific anatomical region. This examination aims to determine the state of well-being and functionality of the talus head after the screw removal. Considering several indicators, such as range of motion, presence or absence of swelling, degree of tissue healing, extent of bone regeneration, and degree of pain experienced by the patient, this assessment aims to provide a comprehensive understanding of the health status of the talus head following screw extraction. A photograph taken seven months after surgery of the talus head fracture shows the proper :union: of the fractured area of the talus without swelling (Figure 7). Another examination was to check the patient’s range of motion (Figure 8). Figure 9 shows the full recovery of the range of motion of the patient’s ankle.
3. Discussion
Talar fractures are exceedingly rare during childhood, accounting for less than 1% of all fractures, with an estimated prevalence rate between 0.01% and 0.08%. Compared to adults, children experience talar fractures at a rate approximately five times lower [6, 7].
The severity of these fractures tends to be higher in older cases. Compared to children (under 12 years old) and adolescents (over 12 years old), Eberl et al. observed a higher prevalence of talar fractures in the latter group, possibly due to skeletal development. In younger children, the immature portion of the talus exhibits greater resistance to the fractures. Talar maturity typically occurs during adolescence, between the ages of 12 and 22. However, due to the absence of an epiphysis in the talus, determining its maturity is challenging. Therefore, the development of the talus is commonly assessed by the closure of metatarsals, which typically occurs between the ages of 14 and 21 years [5, 8]. The talus in children contains a substantial amount of cartilage tissue, which displays excellent elasticity. As age increases, the cartilage tissue proportion reduces. The ligaments and soft tissue surrounding the talus possess remarkable strength and extensibility, contributing to its significant impact resistance [9].
The talus fulfills a crucial biomechanical performance and is involved in the patient’s gait and walking patterns. Failure to properly reduce and stabilize a talus fracture can severely impair normal foot activity and function. Talus fractures are primarily caused by significant force, such as a traffic accident or a high fall, resulting in excessive dorsiflexion and ankle joint compression, ultimately leading to displacement, fracture, and separation [10, 11]. The mechanism of this trauma typically involves sudden dorsiflexion causing the talar head compression against the tibia anterior border, as first described by Anderson in 1919 [12]. Fractures of the talus can be categorized based on whether the head, neck, or body is involved, and further subdivisions can be made within the body. Various classification systems are employed to describe these fracture patterns and provide guidance for their management. Talar head fractures are not common talar fractures, accounting for 5%-10% of all talar fractures [12, 13].
Fractures of the head of the talus occur particularly at the talonavicular joint articular surface and may be accompanied by dislocation or subluxation of the talus as well as fractures of adjacent bones. No established classification system was observed to characterize this fracture, although two patterns have been identified, shear fractures and crush injuries of the articular surface with significant fragmentation [14]. Talar head fractures cause midfoot pain, focal tenderness and swelling over the talar head, and pain with motion at the midtarsal joint [15]. Radiographs of the foot are the most effective means of visualizing fractures of the talus head [17]. In this study, a patient presented with ankle pain and swelling following a fall from a height of 10 meters. After taking a thorough patient history and conducting a physical examination, an initial diagnosis of a talus fracture was made, prompting further investigation with radiographs. Subsequent imaging, including radiographs and a CT scan, confirmed the presence of a fracture involving the head of the talus.
Both non-displaced fractures of the talar head and surgically managing displaced fractures of the talar head have favorable outcomes in terms of patient recovery. The strong blood supply to the talar head contributes to its relatively positive prognosis compared to the talar neck and body. Non-displaced fractures of the talar head are treated conservatively, while surgical intervention is necessary for displaced fractures to realign the talonavicular joint and decrease the risk of osteonecrosis and osteoarthritis [14, 16, 17]. The complications, including avascular necrosis of the talus and osteoarthritis are related to the delicate blood supply and the extensive surface of cartilage in the body of the talus [17]. Talar osteonecrosis is typically caused by trauma to the delicate blood supply of the talus, with talar neck fractures being the most common etiology. Fracture of the talar head is another reason for talar osteonecrosis and osteoarthritis. Patients with talar osteonecrosis often experience progressive ankle pain and limited range of motion, and treatment options depend on the stage of the disease [18]. Despite advances in surgeries, complications following fractures are still common, including foot deformities, osteonecrosis, and post-traumatic osteoarthritis. Fractures and dislocations can lead to avascular necrosis of the talus, which typically occurs within a few weeks to 6 months after the injury [7, 19]. This condition can lead to significant disability and post-traumatic arthritis. In children with non-displaced talus fractures, the incidence of avascular necrosis can be 16%, which is significantly higher compared to adults [20]. However, this reported incidence can be due to initially overlooked and untreated fractures. Talus fractures can also lead to other complications, such as non:union:, mal:union:, loose bodies, infection, neuropraxia, and impaired wound healing [21].
In the past, immediate open reduction with internal fixation was suggested because it was believed that delayed surgery increased the risk factors. However, the more recent literature has found no significant association between the surgery timing and osteonecrosis or osteoarthritis development [18, 22-24].
If displaced fractures of the head or neck are not properly reduced, they can result in arthritis or secondary necrosis. However, in this particular case, the patient’s radiographs showed no signs of osteonecrosis or osteoarthritis during the one-month and six-month follow-up, indicating that the surgery was effective. We recommend the utilization of the anteromedial approach surgery as an effective treatment method for patients with segmented fractures of the talus head.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Byrne AM, Stephens M. Paediatric talus fracture. BMJ Case Rep. 2012; 2012:bcr1020115028. [DOI:10.1136/bcr.10.2011.5028] [PMID] [PMCID]
- Sidhu GAS, Hind J, Ashwood N, Kaur H, Lacon A. Talus fracture dislocation management with crossed kirschner wires in children. Cureus. 2021; 13(3):e13801. [DOI:10.7759/cureus.13801]
- Huang X, Ruan S, Lei Z, Cao H. Anteromedial cannulated screw fixation for Hawkins II/III talus fractures in children: A retrospective study. J Orthop Surg Res. 2023; 18(1):765. [DOI:10.1186/s13018-023-04253-y] [PMID] [PMCID]
- Thermann H, Schratt HE, Hüfner T, Tscherne H. [Fractures of the pediatric foot]. Unfallchirurg. 1998; 101(1):2-11.[DOI:10.1007/s001130050225] [PMID]
- Eberl R, Singer G, Schalamon J, Hausbrandt P, Hoellwarth ME. Fractures of the talus--differences between children and adolescents. J Trauma. 2010; 68(1):126-30. [DOI:10.1097/TA.0b013e3181a74667] [PMID]
- Bijukumar DR, McGeehan C, Mathew MT. Regenerative medicine strategies in biomedical implants. Curr Osteoporos Rep. 2018; 16(3):236-45. [DOI:10.1007/s11914-018-0441-0] [PMID] [PMCID]
- Meier R, Krettek C, Griensven M, Chawda M, Thermann H. Fractures of the talus in the pediatric patient. Foot Ankle Surg. 2005; 11(1):5-10. [DOI:10.1016/j.fas.2004.10.001]
- Monestier L, Riva G, Faoro L, Surace MF. Rare shear-type fracture of the talar head in a thirteen-year-old child - Is this a transitional fracture: A case report and review of the literature. World J Orthop. 2021; 12(5):329-37. [DOI:10.5312/wjo.v12.i5.329] [PMID] [PMCID]
- Chen H, Liu W, Deng L, Song W. The prognostic value of the hawkins sign and diagnostic value of MRI after talar neck fractures. Foot Ankle Int. 2014; 35(12):1255-61.[DOI:10.1177/1071100714547219] [PMID]
- Jensen L, Wester JU, Rasmussen F, Lindequist S, Schantz K. Prognosis of fracture of the talus in children: 21 (7-34)-year follow-up of 14 cases. Acta Orthop Scand. 1994; 65(4):398-400. [DOI:10.3109/17453679408995478] [PMID]
- Petnehazy T, Schalamon J, Hartwig C, Eberl R, Kraus T, Till H, et al. Fractures of the hallux in children. Foot Ankle Int. 2015; 36(1):60-3. [DOI:10.1177/1071100714552482] [PMID]
- Dale JD, Ha AS, Chew FS. Update on talar fracture patterns: A large level I trauma center study. AJR Am J Roentgenol. 2013; 201(5):1087-92. [DOI:10.2214/AJR.12.9918] [PMID]
- Coltart WD. Aviator’s astragalus. J Bone Joint Surg Br. 1952; 34-b(4):545-66. [DOI:10.1302/0301-620X.34B4.545] [PMID]
- Russell TG, Byerly DW. Talus Fracture. Treasure Island: StatPearls; 2023. [Link]
- Hawkins LG. Fracture of the lateral process of the talus. J Bone Joint Surg Am. 1965; 47(6):1170-5. [DOI:10.2106/00004623-196547060-00005] [PMID]
- Canale ST, Kelly FB, Jr. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J Bone Joint Surg Am. 1978; 60(2):143-56. [DOI:10.2106/00004623-197860020-00001] [PMID]
- Pearce DH, Mongiardi CN, Fornasier VL, Daniels TR. Avascular necrosis of the talus: A pictorial essay. Radiographics. 2005; 25(2):399-410. [DOI:10.1148/rg.252045709] [PMID]
- Parekh SG, Kadakia RJ. Avascular necrosis of the talus. J Am Acad Orthop Surg. 2021; 29(6):e267-8. [DOI:10.5435/JAAOS-D-20-00418] [PMID]
- Schmidt DM, Romash MM. Atraumatic avascular necrosis of the head of the talus: A case report. Foot Ankle. 1988; 8(4):208-11. [DOI:10.1177/107110078800800408] [PMID]
- Michel-Traverso A, Ngo TH, Bruyere C, Saglini M. Talus fracture in a 4-year-old child. BMJ Case Rep. 2017; 2017:bcr2016215063. [DOI:10.1136/bcr-2016-215063] [PMID] [PMCID]
- Smith JT, Curtis TA, Spencer S, Kasser JR, Mahan ST. Complications of talus fractures in children. J Pediatr Orthop. 2010; 30(8):779-84. [DOI:10.1097/BPO.0b013e3181f73e6e] [PMID]
- Ross JS, Rush SM, Todd NW, Jennings MM. Modified Blair tibiotalar arthrodesis for post-traumatic avascular necrosis of the talus: A case report. J Foot Ankle Surg. 2013; 52(6):776-80. [DOI:10.1053/j.jfas.2013.08.004] [PMID]
- Sferopoulos N, Corresponding. Talus fractures in children. ARC Journal of Research in Sports Medicine. 2017; 2:21-6.
- Metzger MJ, Levin JS, Clancy JT. Talar neck fractures and rates of avascular necrosis. J Foot Ankle Surg. 1999; 38(2):154-62. [DOI:10.1016/S1067-2516(99)80030-1] [PMID]
Type of Study: Case Report |
Subject:
Pediatrics
Received: 2022/03/16 | Accepted: 2022/05/2 | Published: 2022/11/1
Received: 2022/03/16 | Accepted: 2022/05/2 | Published: 2022/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |