Volume 9, Issue 4 (11-2022)
JROS 2022, 9(4): 225-232 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najdmazhar F, Shariatzadeh H, Roozbehi A, Bahaeddini M R, Jafari B, Hamadiyan H et al . Closed Reduction and Percutaneous Pinning Treatment for Dorsal Fracture-dislocation of the Proximal Interphalangeal Joint. JROS 2022; 9 (4) :225-232
URL: http://jros.iums.ac.ir/article-1-2227-en.html
URL: http://jros.iums.ac.ir/article-1-2227-en.html
Farid Najdmazhar1 

 , Hooman Shariatzadeh2
, Hooman Shariatzadeh2 

 , Amrollah Roozbehi2
, Amrollah Roozbehi2 
 , Mohammad Reza Bahaeddini1
, Mohammad Reza Bahaeddini1 
 , Behnam Jafari3
, Behnam Jafari3 
 , Hosein Hamadiyan3
, Hosein Hamadiyan3 

 , Reza Torab1
, Reza Torab1 




 , Hooman Shariatzadeh2
, Hooman Shariatzadeh2 

 , Amrollah Roozbehi2
, Amrollah Roozbehi2 
 , Mohammad Reza Bahaeddini1
, Mohammad Reza Bahaeddini1 
 , Behnam Jafari3
, Behnam Jafari3 
 , Hosein Hamadiyan3
, Hosein Hamadiyan3 

 , Reza Torab1
, Reza Torab1 


1- Bone and Joint Reconstruction Research Center, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Cellular and Molecular Research Center, Yasuj University of Medical Sciences, Yasuj, Iran.
3- Department of Orthopedic, School of Medicine, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Cellular and Molecular Research Center, Yasuj University of Medical Sciences, Yasuj, Iran.
3- Department of Orthopedic, School of Medicine, Shafa Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Proximal interphalangeal (PIP) joint, Dorsal fracture- dislocation, Closed reduction, Percutaneous pinning
Full-Text [PDF 807 kb]
(156 Downloads)
| Abstract (HTML) (487 Views)
Full-Text: (151 Views)
1. Introduction
Dorsal fracture-dislocations of the proximal interphalangeal (PIP) joint are among the most common hand injuries, which can result in permanent disability, subluxation, decreased range of motion (ROM), stiffness, osteoarthritis, and severe pain [1-3]. The fracture of the middle phalanx (P2 volar base) is the main type of PIP joint dorsal fracture-dislocation injuries [4, 5]. Given that joint instability is a primary complication of these injuries, achieving concentric reduction and stable fixation of the fracture fragments is crucial to prevent subsequent complications [5, 6, 7].
The treatment approach for PIP joint dorsal fracture-dislocations largely depends on the size of the fracture fragments. Fracture-dislocation with volar fragments less than 30% of the articular surface is managed conservatively; mainly using PIP flexion and dorsal block splinting. Fractures involving 30%-50% of the articular surface are managed surgically only if the reduction is not achieved by PIP flexion or when increasing flexion is required to preserve the congruent reduction. For fractures involving more than 50% of the articular surface, surgical intervention is necessary [3].
Several surgical strategies have been introduced, including open reduction and internal fixation, extension block pinning, closed reduction percutaneous pinning, volar plate arthroplasty, and hemi-hamate arthroplasty [8, 9, 10]. Although various surgical techniques have been described, no clear consensus exists on the best surgical procedure for PIP joint dorsal fracture-dislocation treatment [8]. Closed reduction and percutaneous pinning is a simple and minimally invasive surgical option to achieve PIP joint reduction using a percutaneous Kirschner wire (K-wire) [11]. This study aims to evaluate the clinical and radiologic outcomes of closed reduction and percutaneous pinning in the treatment of unstable PIP joint dorsal fracture-dislocations.
2. Methods
We retrospectively reviewed the medical profiles of patients with dorsal fracture-dislocations of PIP joint, who were referred to our hospital between 2018 and 2021, and underwent closed reduction and percutaneous pinning for treatment. The inclusion criteria included treatment in the acute phase (within two weeks of injury) and a minimum follow-up of one year. The exclusion criteria included patients with prior injury or surgery on the affected digit, as well as those with concomitant fractures on the same affected digit. Twelve patients who met the study criteria were included in the final analysis.
Surgical technique
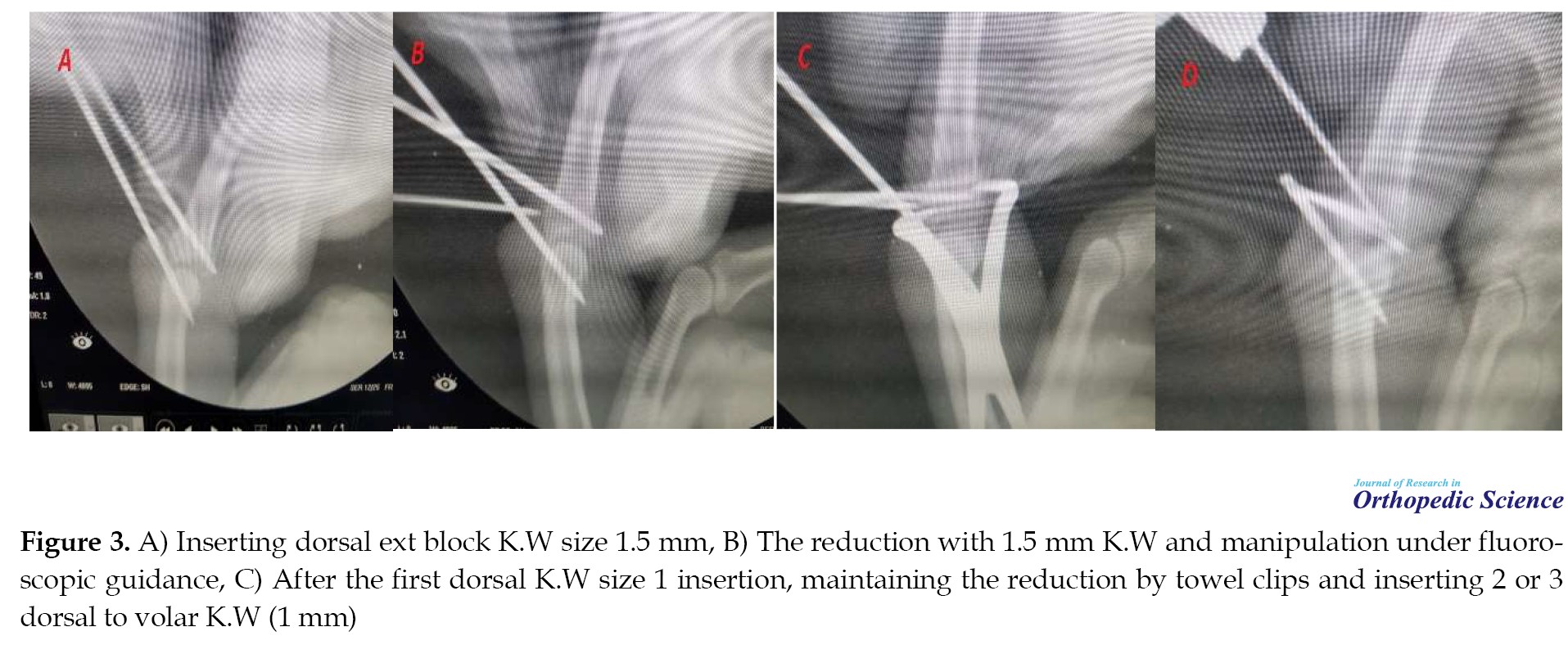
All operations were performed by a single senior hand surgeon (Farid Najdmazhar). The procedure was conducted under fluoroscopic guidance. The PIP joint fracture-dislocation involved a fracture at the base of the P2 volar base, with the cortex remaining intact (Figure 1a). Closed reduction was achieved under general anesthesia or digital block by applying a dorsal to volar force while the PIP joint was flexed (Figure 1b). Subsequently, a K-wire as an extension block pin (one or one and a half millimeters K-wire), was inserted with an angle of 45 degrees, positioned at the dorsal cortico-articular junction of the distal end of the proximal phalanx (Figure 1c). Fractured fragments and depressed articular surfaces were restored through manipulation with a k-wire under fluoroscopic guidance (Figure 1d). The reduction was then maintained with gentle force using towel clips (non-tipped side) (Figure 1e). After achieving reduction, the fracture was fixed with two or three 1 mm K-wires inserted from dorsal to volar (Figure 1f). Patients were discharged with a static volar splint which they were instructed to wear for three to four weeks.
Outcome evaluation
The clinical evaluations included the assessment of PIP joint pain, function, ROM, grip strength, and pinch strength. The PIP joint pain was evaluated using a visual analog scale (VAS) for pain, scored between 0 and 10, representing “no pain” to “worst possible pain”, respectively. The PIP joint function was assessed with quick disabilities of the arm, shoulder, and hand (Quick-DASH) questionnaire, the validity and reliability of which were previously evaluated [12]. Each patient received a score between 0 and 100, with higher scores indicating worse function. Grip strength was measured using a standard dynamometer (Hydraulic Hand Dynamometer SH5001, Saehan Corporation, Masan, Korea). Pinch strength was assessed using a standard pinch gauge (Hydraulic Pinch Gauge SH5005, Saehan Corporation, Masan, Korea). All clinical evaluations were performed by an orthopedist who was not involved in the patient’s care. Radiographic evaluation was performed by a musculoskeletal radiologist and included the assessment of posttraumatic arthritis using the Kellgren and Lawrence classification [13]. Accordingly, the patients were classified into five grades ranging from 0 to 4, representing no PIP joint degeneration to the most severe degeneration, respectively. For example, the treatment steps of one of the patients are depicted (Figures 2, 3 and 4).
Statistical analysis
Statistical analysis was conducted using SPSS for Windows, version 16 (SPSS Inc., Chicago, Ill., USA). Descriptive statistics were demonstrated by Mean±SD or numbers with percentages for quantitative and qualitative variables, respectively. The paired t test was utilized to compare pinch and grip strength relative to the opposite side. A P<0.05 was considered statistically significant.
3. Results
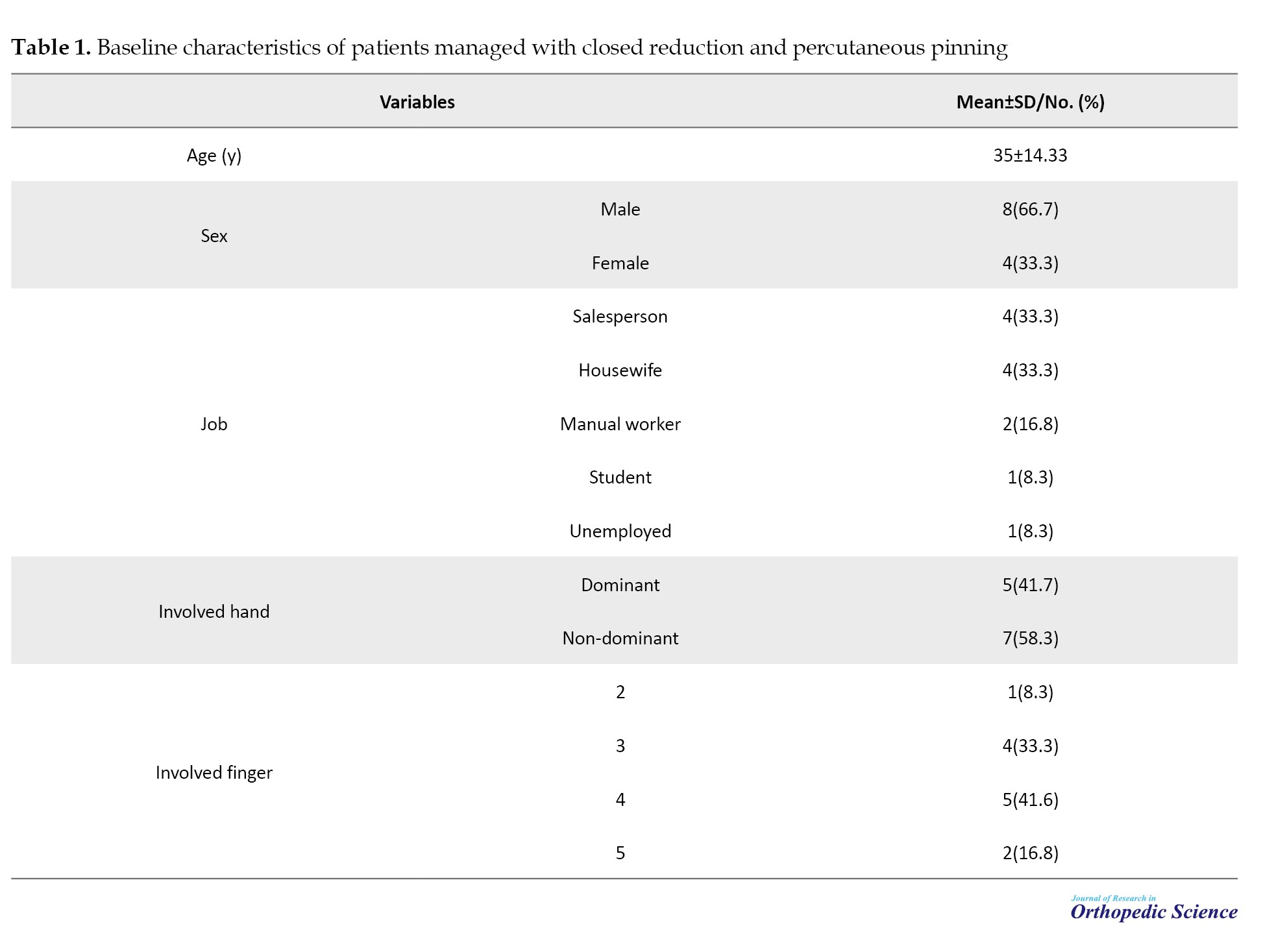
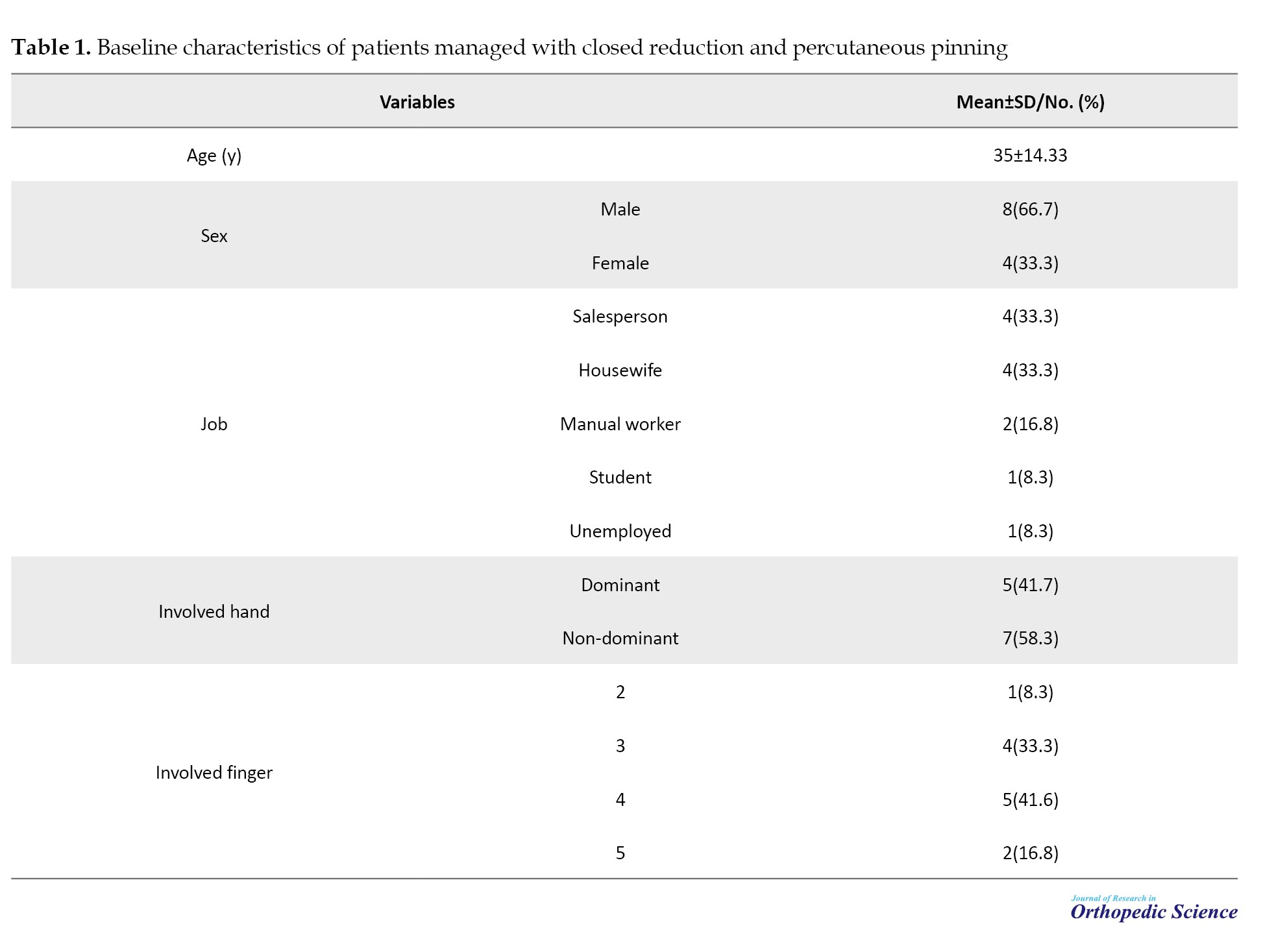
In this study, 19 patients were initially included, based on the inclusion and exclusion criteria. However, three patients were excluded due to incomplete follow-up, two due to a change of address, one due to lack of consent to participate, and one due to simultaneous bony Mellat fracture. Therefore, the final study population included eight males and four females, with a mean age of 35±14.33 years, ranging from 19 to 63 years. The injury affected the non-dominant hand in seven (58.3%) patients. The mean time from injury to surgery was 3.4±2 days (range 2-9), and the mean follow-up period was 18.5 months (range 12 to 37). Table 1 presents further details regarding the baseline characteristics of the patients.
The mean PIP joint ROM was 99±5.3° (range 90-110), representing approximately 90.2% of the contralateral hand (P=0.31). The mean flexion contracture was 6.7±3.2º (range 5-15). The mean extension lag was 6.3±3.1º (range 5-15). All patients experienced some degree of PIP joint, with a mean VAS score of 3.3±1.5 (range 1-6). The mean Quick-DASH score was 10.8±6.1 points (range 5-25). The mean pinch strength of the involved hand averaged 80.4% of the noninvolved hand (P=0.19), while the mean grip strength averaged 92.29% (P=0.28). Table 2 presents further clinical outcomes.

Radiographic evaluation revealed a concentric reduction in all cases. The fracture :union: was evident in all patients. No patient experienced a subluxation or dislocation. Postoperative arthritic changes were observed in the final radiographs of the patients, which were grade 1 in seven patients (58.3%) and grade 2 in five patients (41.7%). No other postoperative complications, such as wound infection, were recorded in this series.
4. Discussion
This study was conducted to evaluate the outcomes of close reduction and percutaneous pinning in the treatment of PIP joint dorsal fracture-dislocation. At the last follow-up, the PIP joint ROM was within an acceptable range compared to the contralateral hand. Also, the mean grip and pinch strength of the involved hand were not significantly different from the contralateral hand. All patients experienced some degree of PIP joint pain, which was mild in the majority of them. Degenerative changes were observed in the final PIP joint radiographs of all patients; however, they were clinically asymptomatic. No instances of subluxation or dislocation occurred during the mean follow-up of 18.6 months.
The outcomes of close reduction and percutaneous pinning in the treatment of PIP joint dorsal fracture-dislocation have been reported in a few earlier studies. Newington et al. reviewed the outcomes of closed reduction and percutaneous fixation (Trans-articular K-wire) in the treatment of 10 patients (11 fingers) with dorsal PIP joint fracture-dislocation [14]. At the 16-year follow-up, seven patients had no finger pain or stiffness, with a mean flexion contracture of 8º and a mean ROM of 85º. Mild joint space narrowing was observed in some patients. They concluded that this technique is a reliable treatment providing satisfactory long-term results. Although the mean follow-up in our study was significantly shorter (18.6 months), the mean flexion contracture and ROM of the PIP joint were superior to those reported by Newington et al.
Vitale et al. reported the short-term postoperative results of closed reduction, percutaneous fracture reduction, and pinning in the treatment of six patients with unstable dorsal PIP joint fracture-dislocation [15]. During the average 18.7-month follow-up, no subluxation or dislocation of the PIP joint was recorded. Radiographic evaluation revealed concentric reduction and :union: in all patients. The mean DASH score and VAS score were 8 and 1.4, respectively. They concluded that the percutaneous technique provides a stable PIP joint and results in excellent clinical and radiographic outcomes. Similarly, in the present study, the percutaneous technique yielded acceptable clinical and radiographic outcomes. However, the mean VAS score for pain was higher in our study.
Haseth et al. reported the outcomes of closed reduction and percutaneous pinning (Trans-articular K-Wire) in the treatment of nine patients with acute dorsal PIP joint fracture-dislocations [11]. At a mean follow-up of 6.5 months, all patients exhibited painless but fusiform and swollen PIP joints. The mean ROM of the PIP joint ranged from 4º extension to 106º flexion. The mean extension lag and flexion contracture were 10º and 15º, respectively. Radiographically, all patients had a concentric PIP joint with the :union:. Additionally, two patients showed radiographic evidence of PIP joint degenerative changes that were asymptomatic. They concluded that close reduction and percutaneous pinning, as a minimally invasive technique, provide satisfactory outcomes in the short to mid-term. The mean flexion contracture and extension lag were 6.7º and 6.3º, respectively, in the present study, which was remarkably lower than those reported by Haseth et al. However, all patients in our study exhibited radiographic evidence of joint degeneration that was asymptomatic.
Gianakos et al. systematically reviewed the outcomes of different surgical methods in the treatment of acute PIP joint fracture-dislocations [16]. They found that open reduction and internal fixation had the highest revision rate (19.7%), while closed reduction and percutaneous pinning, as well as volar plate arthroplasty, exhibited the lowest complication rates, alongside good clinical and functional outcomes. However, they also noted that the overall outcomes of PIP joint dorsal fracture-dislocations remarkably depend on the severity of the injury.
We believe that closed reduction and percutaneous pinning represent a valuable minimally invasive method in the treatment of PIP joint dorsal fracture-dislocation. However, the present study was not without limitations. These included its respective design, a small study population, and the absence of a control group of patients treated by other methods. Therefore, future prospective studies involving larger patient populations and adequate control groups are required to further explore the value of the present technique in the treatment of PIP joint fracture-dislocation.
5. Conclusion
Closed reduction and percutaneous pinning is a simple, accessible, and minimally invasive method for managing the PIP joint dorsal fracture-dislocations. Clinical and radiographic outcomes range from good to excellent, providing a stable and concentric joint, at least in mid-term follow-up, with a low rate of postoperative complications. Therefore, this technique can be considered a valuable surgical option in the treatment of PIP joint dorsal fracture-dislocations.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethical board of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1401.71).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
Dorsal fracture-dislocations of the proximal interphalangeal (PIP) joint are among the most common hand injuries, which can result in permanent disability, subluxation, decreased range of motion (ROM), stiffness, osteoarthritis, and severe pain [1-3]. The fracture of the middle phalanx (P2 volar base) is the main type of PIP joint dorsal fracture-dislocation injuries [4, 5]. Given that joint instability is a primary complication of these injuries, achieving concentric reduction and stable fixation of the fracture fragments is crucial to prevent subsequent complications [5, 6, 7].
The treatment approach for PIP joint dorsal fracture-dislocations largely depends on the size of the fracture fragments. Fracture-dislocation with volar fragments less than 30% of the articular surface is managed conservatively; mainly using PIP flexion and dorsal block splinting. Fractures involving 30%-50% of the articular surface are managed surgically only if the reduction is not achieved by PIP flexion or when increasing flexion is required to preserve the congruent reduction. For fractures involving more than 50% of the articular surface, surgical intervention is necessary [3].
Several surgical strategies have been introduced, including open reduction and internal fixation, extension block pinning, closed reduction percutaneous pinning, volar plate arthroplasty, and hemi-hamate arthroplasty [8, 9, 10]. Although various surgical techniques have been described, no clear consensus exists on the best surgical procedure for PIP joint dorsal fracture-dislocation treatment [8]. Closed reduction and percutaneous pinning is a simple and minimally invasive surgical option to achieve PIP joint reduction using a percutaneous Kirschner wire (K-wire) [11]. This study aims to evaluate the clinical and radiologic outcomes of closed reduction and percutaneous pinning in the treatment of unstable PIP joint dorsal fracture-dislocations.
2. Methods
We retrospectively reviewed the medical profiles of patients with dorsal fracture-dislocations of PIP joint, who were referred to our hospital between 2018 and 2021, and underwent closed reduction and percutaneous pinning for treatment. The inclusion criteria included treatment in the acute phase (within two weeks of injury) and a minimum follow-up of one year. The exclusion criteria included patients with prior injury or surgery on the affected digit, as well as those with concomitant fractures on the same affected digit. Twelve patients who met the study criteria were included in the final analysis.
Surgical technique
All operations were performed by a single senior hand surgeon (Farid Najdmazhar). The procedure was conducted under fluoroscopic guidance. The PIP joint fracture-dislocation involved a fracture at the base of the P2 volar base, with the cortex remaining intact (Figure 1a). Closed reduction was achieved under general anesthesia or digital block by applying a dorsal to volar force while the PIP joint was flexed (Figure 1b). Subsequently, a K-wire as an extension block pin (one or one and a half millimeters K-wire), was inserted with an angle of 45 degrees, positioned at the dorsal cortico-articular junction of the distal end of the proximal phalanx (Figure 1c). Fractured fragments and depressed articular surfaces were restored through manipulation with a k-wire under fluoroscopic guidance (Figure 1d). The reduction was then maintained with gentle force using towel clips (non-tipped side) (Figure 1e). After achieving reduction, the fracture was fixed with two or three 1 mm K-wires inserted from dorsal to volar (Figure 1f). Patients were discharged with a static volar splint which they were instructed to wear for three to four weeks.
Outcome evaluation
The clinical evaluations included the assessment of PIP joint pain, function, ROM, grip strength, and pinch strength. The PIP joint pain was evaluated using a visual analog scale (VAS) for pain, scored between 0 and 10, representing “no pain” to “worst possible pain”, respectively. The PIP joint function was assessed with quick disabilities of the arm, shoulder, and hand (Quick-DASH) questionnaire, the validity and reliability of which were previously evaluated [12]. Each patient received a score between 0 and 100, with higher scores indicating worse function. Grip strength was measured using a standard dynamometer (Hydraulic Hand Dynamometer SH5001, Saehan Corporation, Masan, Korea). Pinch strength was assessed using a standard pinch gauge (Hydraulic Pinch Gauge SH5005, Saehan Corporation, Masan, Korea). All clinical evaluations were performed by an orthopedist who was not involved in the patient’s care. Radiographic evaluation was performed by a musculoskeletal radiologist and included the assessment of posttraumatic arthritis using the Kellgren and Lawrence classification [13]. Accordingly, the patients were classified into five grades ranging from 0 to 4, representing no PIP joint degeneration to the most severe degeneration, respectively. For example, the treatment steps of one of the patients are depicted (Figures 2, 3 and 4).
Statistical analysis
Statistical analysis was conducted using SPSS for Windows, version 16 (SPSS Inc., Chicago, Ill., USA). Descriptive statistics were demonstrated by Mean±SD or numbers with percentages for quantitative and qualitative variables, respectively. The paired t test was utilized to compare pinch and grip strength relative to the opposite side. A P<0.05 was considered statistically significant.
3. Results
In this study, 19 patients were initially included, based on the inclusion and exclusion criteria. However, three patients were excluded due to incomplete follow-up, two due to a change of address, one due to lack of consent to participate, and one due to simultaneous bony Mellat fracture. Therefore, the final study population included eight males and four females, with a mean age of 35±14.33 years, ranging from 19 to 63 years. The injury affected the non-dominant hand in seven (58.3%) patients. The mean time from injury to surgery was 3.4±2 days (range 2-9), and the mean follow-up period was 18.5 months (range 12 to 37). Table 1 presents further details regarding the baseline characteristics of the patients.
The mean PIP joint ROM was 99±5.3° (range 90-110), representing approximately 90.2% of the contralateral hand (P=0.31). The mean flexion contracture was 6.7±3.2º (range 5-15). The mean extension lag was 6.3±3.1º (range 5-15). All patients experienced some degree of PIP joint, with a mean VAS score of 3.3±1.5 (range 1-6). The mean Quick-DASH score was 10.8±6.1 points (range 5-25). The mean pinch strength of the involved hand averaged 80.4% of the noninvolved hand (P=0.19), while the mean grip strength averaged 92.29% (P=0.28). Table 2 presents further clinical outcomes.

Radiographic evaluation revealed a concentric reduction in all cases. The fracture :union: was evident in all patients. No patient experienced a subluxation or dislocation. Postoperative arthritic changes were observed in the final radiographs of the patients, which were grade 1 in seven patients (58.3%) and grade 2 in five patients (41.7%). No other postoperative complications, such as wound infection, were recorded in this series.
4. Discussion
This study was conducted to evaluate the outcomes of close reduction and percutaneous pinning in the treatment of PIP joint dorsal fracture-dislocation. At the last follow-up, the PIP joint ROM was within an acceptable range compared to the contralateral hand. Also, the mean grip and pinch strength of the involved hand were not significantly different from the contralateral hand. All patients experienced some degree of PIP joint pain, which was mild in the majority of them. Degenerative changes were observed in the final PIP joint radiographs of all patients; however, they were clinically asymptomatic. No instances of subluxation or dislocation occurred during the mean follow-up of 18.6 months.
The outcomes of close reduction and percutaneous pinning in the treatment of PIP joint dorsal fracture-dislocation have been reported in a few earlier studies. Newington et al. reviewed the outcomes of closed reduction and percutaneous fixation (Trans-articular K-wire) in the treatment of 10 patients (11 fingers) with dorsal PIP joint fracture-dislocation [14]. At the 16-year follow-up, seven patients had no finger pain or stiffness, with a mean flexion contracture of 8º and a mean ROM of 85º. Mild joint space narrowing was observed in some patients. They concluded that this technique is a reliable treatment providing satisfactory long-term results. Although the mean follow-up in our study was significantly shorter (18.6 months), the mean flexion contracture and ROM of the PIP joint were superior to those reported by Newington et al.
Vitale et al. reported the short-term postoperative results of closed reduction, percutaneous fracture reduction, and pinning in the treatment of six patients with unstable dorsal PIP joint fracture-dislocation [15]. During the average 18.7-month follow-up, no subluxation or dislocation of the PIP joint was recorded. Radiographic evaluation revealed concentric reduction and :union: in all patients. The mean DASH score and VAS score were 8 and 1.4, respectively. They concluded that the percutaneous technique provides a stable PIP joint and results in excellent clinical and radiographic outcomes. Similarly, in the present study, the percutaneous technique yielded acceptable clinical and radiographic outcomes. However, the mean VAS score for pain was higher in our study.
Haseth et al. reported the outcomes of closed reduction and percutaneous pinning (Trans-articular K-Wire) in the treatment of nine patients with acute dorsal PIP joint fracture-dislocations [11]. At a mean follow-up of 6.5 months, all patients exhibited painless but fusiform and swollen PIP joints. The mean ROM of the PIP joint ranged from 4º extension to 106º flexion. The mean extension lag and flexion contracture were 10º and 15º, respectively. Radiographically, all patients had a concentric PIP joint with the :union:. Additionally, two patients showed radiographic evidence of PIP joint degenerative changes that were asymptomatic. They concluded that close reduction and percutaneous pinning, as a minimally invasive technique, provide satisfactory outcomes in the short to mid-term. The mean flexion contracture and extension lag were 6.7º and 6.3º, respectively, in the present study, which was remarkably lower than those reported by Haseth et al. However, all patients in our study exhibited radiographic evidence of joint degeneration that was asymptomatic.
Gianakos et al. systematically reviewed the outcomes of different surgical methods in the treatment of acute PIP joint fracture-dislocations [16]. They found that open reduction and internal fixation had the highest revision rate (19.7%), while closed reduction and percutaneous pinning, as well as volar plate arthroplasty, exhibited the lowest complication rates, alongside good clinical and functional outcomes. However, they also noted that the overall outcomes of PIP joint dorsal fracture-dislocations remarkably depend on the severity of the injury.
We believe that closed reduction and percutaneous pinning represent a valuable minimally invasive method in the treatment of PIP joint dorsal fracture-dislocation. However, the present study was not without limitations. These included its respective design, a small study population, and the absence of a control group of patients treated by other methods. Therefore, future prospective studies involving larger patient populations and adequate control groups are required to further explore the value of the present technique in the treatment of PIP joint fracture-dislocation.
5. Conclusion
Closed reduction and percutaneous pinning is a simple, accessible, and minimally invasive method for managing the PIP joint dorsal fracture-dislocations. Clinical and radiographic outcomes range from good to excellent, providing a stable and concentric joint, at least in mid-term follow-up, with a low rate of postoperative complications. Therefore, this technique can be considered a valuable surgical option in the treatment of PIP joint dorsal fracture-dislocations.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the ethical board of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1401.71).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
References
- Glickel SZ, Barron OA. Proximal interphalangeal joint fracture dislocations. Hand Clin. 2000; 16(3):333-44.[DOI:10.1016/S0749-0712(21)00575-8] [PMID]
- Elfar J, Mann T. Fracture-dislocations of the proximal interphalangeal joint. J Am Acad Orthop Surg. 2013; 21(2):88-98. [DOI:10.5435/JAAOS-21-02-88] [PMID] [PMCID]
- Mazhar FN. Proximal interphalangeal joint fracture dislocation. Shafa Ortho J. 2013; 1(2):29-33. [Link]
- Moura SP, Meulendijks MZ, Veeramani A, Szapary H, Gomez-Eslava B, Hoftiezer YAJ, et al. Epidemiology and fracture patterns of traumatic phalangeal fractures. Plast Reconstr Surg Glob Open. 2022; 10(8):e4455. [DOI:10.1097/GOX.0000000000004455] [PMID] [PMCID]
- Tan RES, Cheah AEJ. Injuries around the proximal interphalangeal joint. Clin Plast Surg. 2019; 46(3):437-49. [DOI:10.1016/j.cps.2019.03.005] [PMID]
- Mazhar FN, Motaghi P. Closed reduction and percutaneous pinning for treatment of proximal interphalangeal joint pilon fractures. Hand. 2023; 18(1):40-7. [DOI:10.1177/1558944721990774] [PMID] [PMCID]
- Kamnerdnakta S, Huetteman HE, Chung KC. Complications of proximal interphalangeal joint injuries: Prevention and treatment. Hand Clin. 2018; 34(2):267-88. [DOI:10.1016/j.hcl.2017.12.014] [PMID] [PMCID]
- Demino C, Yates M, Fowler JR. Surgical management of proximal interphalangeal joint fracture-dislocations: A review of outcomes. Hand. 2021; 16(4):453-60. [DOI:10.1177/1558944719873152] [PMID] [PMCID]
- Najd Mazhar F, Bahaeddini MR, Jafari D, Mirzaei A. Evaluation of the clinical and radiological outcome of hemi-hamate arthroplasty in the reconstruction of proximal interphalangeal Joint fracture-dislocations. Med J Islam Repub Iran. 2019; 33:152. [PMID]
- Najd Mazhar F, Jafari D, Taraz H, Mirzaei A. Treatment of dorsal fracture-dislocations of the proximal interphalangeal joint using the shotgun approach. J Hand Surg Eur Vol. 2018; 43(5):499-505. [DOI:10.1177/1753193418766274] [PMID]
- de Haseth KB, Neuhaus V, Mudgal CS. Dorsal fracture-dislocations of the proximal interphalangeal joint: evaluation of closed reduction and percutaneous Kirschner wire pinning. Hand. 2015; 10(1):88-93. [DOI:10.1007/s11552-014-9660-8] [PMID] [PMCID]
- Ebrahimzadeh MH, Moradi A, Vahedi E, Kachooei AR, Birjandinejad A. Validity and reliability of the Persian version of shortened disabilities of the arm, shoulder and hand questionnaire (quick-DASH).Int J Prev Med. 2015; 6:59. [DOI:10.4103/2008-7802.160336] [PMID] [PMCID]
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957; 16(4):494-502.[DOI:10.1136/ard.16.4.494] [PMID] [PMCID]
- Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: A 16-year follow up. J Hand Surg Br. 2001; 26(6):537-40. [DOI:10.1054/jhsb.2001.0698] [PMID]
- Vitale MA, White NJ, Strauch RJ. A percutaneous technique to treat unstable dorsal fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2011; 36(9):1453-9. [DOI:10.1016/j.jhsa.2011.06.022] [PMID]
- Gianakos A, Yingling J, Athens CM, Barra AE, Capo JT. Treatment for acute proximal interphalangeal joint fractures and fracture-dislocations: A systematic review of the literature. J Hand Microsurg. 2020; 12(Suppl 1):S9-15.[DOI:10.1055/s-0040-1713323] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2022/03/18 | Accepted: 2022/06/12 | Published: 2022/11/1
Received: 2022/03/18 | Accepted: 2022/06/12 | Published: 2022/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |