Volume 9, Issue 3 (8-2022)
JROS 2022, 9(3): 149-156 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gharanizadeh K, Pisoudeh K, Sarikhani M, aminian A, Bahaeddini M. Evaluation of the Accuracy of Cup Positioning in Total Hip Arthroplasty Using the Antero-lateral Approach. JROS 2022; 9 (3) :149-156
URL: http://jros.iums.ac.ir/article-1-2230-en.html
URL: http://jros.iums.ac.ir/article-1-2230-en.html
Kaveh Gharanizadeh1 

 , Karim Pisoudeh1
, Karim Pisoudeh1 

 , Mahmoodreza Sarikhani1
, Mahmoodreza Sarikhani1 

 , Amir Aminian1
, Amir Aminian1 

 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 




 , Karim Pisoudeh1
, Karim Pisoudeh1 

 , Mahmoodreza Sarikhani1
, Mahmoodreza Sarikhani1 

 , Amir Aminian1
, Amir Aminian1 

 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 803 kb]
(173 Downloads)
| Abstract (HTML) (727 Views)
Full-Text: (210 Views)
1. Introduction
Total hip arthroplasty (THA) stands out as one of the most successful procedures in orthopedic surgery [1]. Given its status as the gold standard for addressing advanced osteoarthritis, a global increase in the number of performed THA cases is anticipated [2, 3]. Component positioning plays a crucial role in influencing THA outcomes, with improper cup positioning potentially linked to issues, such as dislocation, increased polyethylene wear, reduced abductor muscle strength, and impingement [4-11].
THA can be performed through various surgical approaches, including anterolateral (AL), direct anterior (DA), and lateral and posterior approaches (PAs) [12]. The AL approach was initially articulated by von Sprengel and Bardenheuer and subsequently, modified on multiple occasions, first by Watson-Jones and later by Harris et al. [13, 14]. This approach is associated with several advantages, such as optimal exposure of the acetabulum, precise implant positioning, leg length correction, and a reduced risk of dislocation [4, 15]. Furthermore, this approach utilizes the intermuscular plane between the tensor fascia lata and gluteus medius, innervated by the superior gluteal nerve [16].
The choice of surgical approach can impact component positioning due to variations in the visibility of critical anatomical landmarks [17]. Numerous studies have investigated the optimal orientation of the acetabular cup in THA. Lewinnek et al. recommended a safe zone for cup orientation with an inclination angle of 40±10° and an anteversion angle of 15±10° [5]. Callanan et al. reported that accurate cup placement, whether by freehand or mechanical guide techniques, depended on factors, like age, surgical approach, and the surgeon’s experience. They noted that cup alignment with the AL approach exhibited decreased accuracy compared to the PA, trending towards higher abduction angles and lower versions [17].
Objectives
In this study, we aimed to investigate the accuracy of cup position by exploring cup anteversion and inclination in patients undergoing THA by an experienced surgeon utilizing the AL approach.
2. Methods
In this cross-sectional study, we included patients undergoing THA at Shafa Yahyaiyan Hospital in Tehran, affiliated with the Iran University of Medical Sciences, from 2018 to 2023. All patients underwent AL-THA in a lateral position by an expert right-hand dominant hip orthopedic surgeon.
The inclusion criteria comprised patients requiring hip replacement due to abnormal hip pathology, including avascular osteonecrosis (AVN) of the femoral head, Crowe I and II developmental dysplasia of the hip (DDH), hip degenerative joint disease (DJD), and a previous history of a femoral neck fracture. Exclusion criteria included patients undergoing revision surgery, those with a history of Perthes disease, types III and IV DDH, and individuals with pathological fractures during childhood.
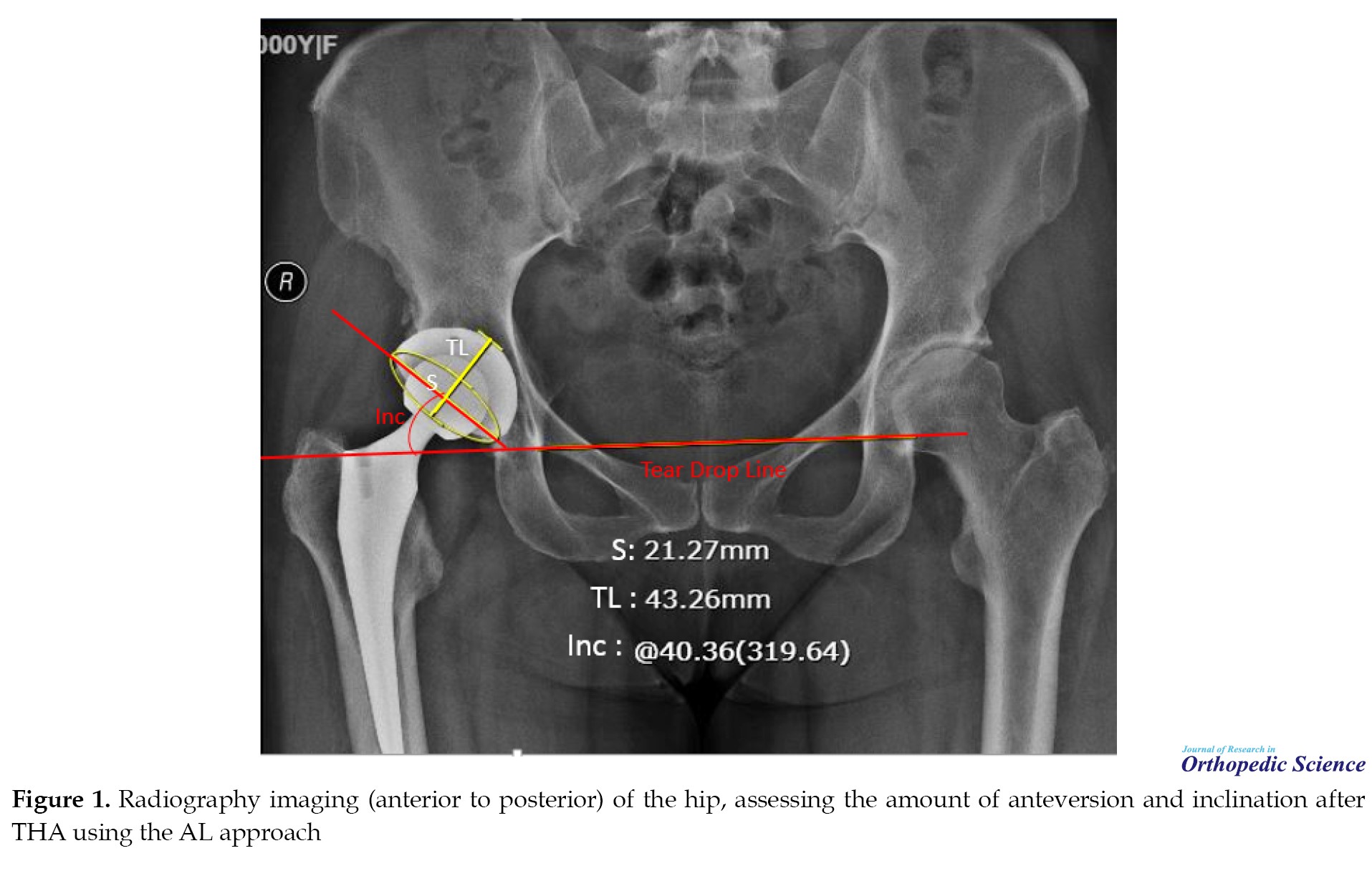
Post-operative radiological evaluations were conducted, with all radiographic performed in an anteroposterior (AP) manner with a 15-degree intra-rotation of the hip, following standard hip radiographic assessment protocols [18, 19]. Anteversion and inclination were assessed using a method previously described by Widmer et al. [20] (Figure 1), determining whether the values fell within the safe zone (inclination angle of 40±10° and an anteversion angle of 15±10°) [5]. A single orthopedic surgeon evaluated the radiographs. Patients’ age and gender were also documented.
Collected data were entered into SPSS software, version 26 for statistical analysis and comparisons. The normality of data was evaluated by the Kolmogorov-Smirnov test. Categorical variables are presented as frequency and percentage (%), while continuous variables are presented with Mean±SD for normally distributed data, and median with first and third quantiles [Q1–Q3] for non-normal data. Statistical analysis involved using the chi-square or Fisher’s exact test for categorical variables (gender and side of operation) and an independent t-test for age. A P<0.05 was considered statistically significant.
3. Results
Among 166 patients, 91 cases were entered into our final analysis based on accurate radiographic imaging and complete data in their files. The patients’ age ranged from 18 to 80 years, with the majority being in the age group of 46 to 65 years. The majority of patients were male (52.7%). The etiology of hip pathology included fracture of the femoral neck in 11(12.1%), AVN in 36(39.6%), DJD in 18(19.8%) and DDH in 26(28.6%) cases. Table 1 presents the characteristics of the patients in our study.

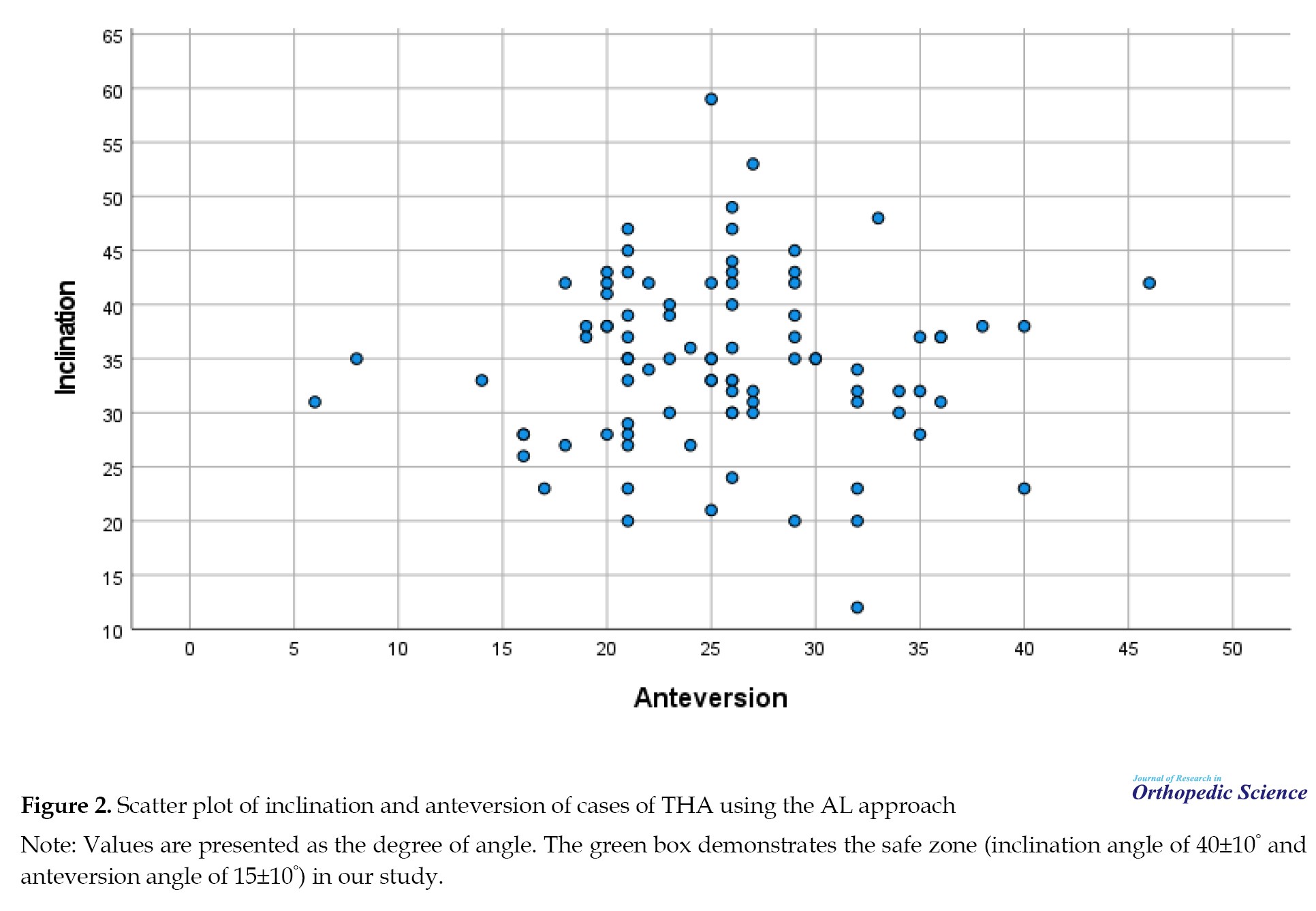
The angle of inclination ranged from 12 to 59°, while the angle of anteversion ranged from 6 to 46°. By considering a safe zone for cup orientation with an inclinationangle of 40±10°, 69 patients (75.8%) were within the safe zone, and by considering an anteversion angle of 15±10°, 46 cases (50.5%) were within the safe zone. Table 2 demonstrates the features of the patients based on their presence in the safe zone.
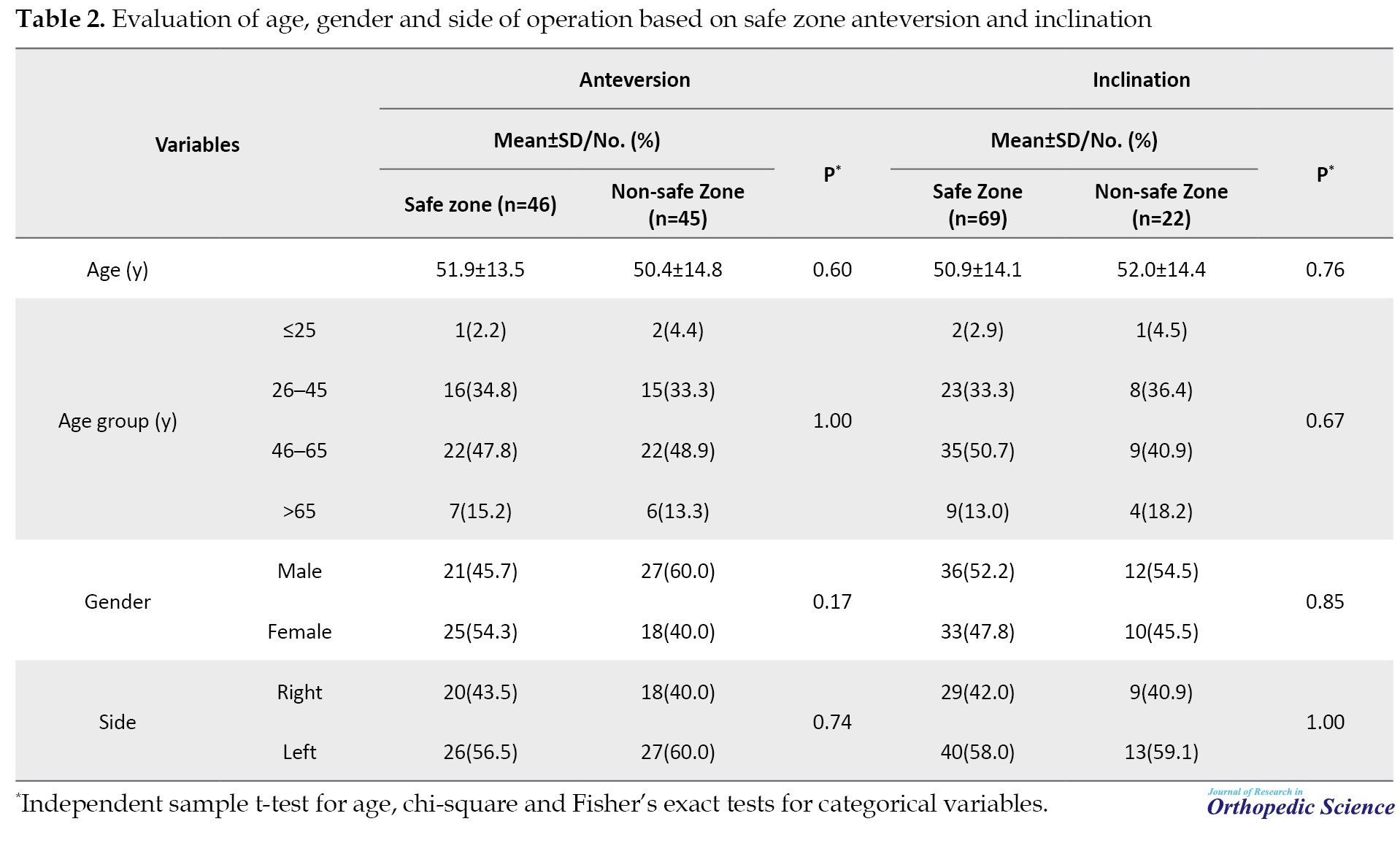
As demonstrated, none of the variables in our study showed a significant association with anteversion and inclination safe zones.
Regarding the inclination angle, out of the 22 cases that were outside the safe zone, 20(22.0%) had angles below 30° and two (2.2%) had angles exceeding 50°. In terms of the anteversion angle, all 45 cases outside the safe zone had angles greater than 25°. The median level of anteversion deviation from the safe zone was 4° [Q1–Q3: 1–9]. Figure 2 demonstrates the scatter plot of the cases in our study based on anteversion and inclination.
4. Discussion
The positioning of components plays a crucial role in the functionality and durability of THA [21]. In this study, we aimed to evaluate the accuracy of component positioning in AL-THA, particularly based on radiographic anteversion and inclination. Our findings indicated that based on the determined safe zone, the majority of patients (75.8%) were within the safe zone of inclination, while approximately half (50.5%) of the patients were within the safe zone of anteversion, indicating that the majority of patients were in the safe zone of cup orientation.
The most concerning factor in our study was that around half of the patients had an anteversion angle outside our safe zone, with a mean deviation of 4° larger than the designated safe zone. Similar findings were also reported in other studies utilizing the anterior approach. Takada et al. [22] noted that the positive error of anteversion was consistently higher than the negative error in the AL, indicating that the majority of cups were implanted with greater anteversion than initially targeted. Maeda et al. [23] also reported a similar trend in radiographic cup anteversion in the AL approach, with values exceeding their target angle by 4.3°, which was similar to our findings. They suggested that the larger anteversion might be attributed to pelvic rotation induced by the retractor placed at the posterior acetabular wall, causing the femoral bone to retract and rotating the ipsilateral pelvis posteriorly during cup preparation. Iwakiri et al. [24] stated that by employing the muscle-sparing modified Watson-Jones AL approach, the deviation from the targeted angle was 3.5±3.1° in inclination and 4.6±4.6° in anteversion. Kawarai et al. [25] also noted the possibility of such rotational instability occurring in the AL approach, similar to the DA approach. This pelvic rotation during surgery could elucidate the prevalence of positive values in the target error of anteversion observed in both groups. Additionally, the angle of inclination ranged from 12 to 59°, while the angle of anteversion ranged from 6 to 46°, suggesting extreme pelvic rotation during surgery in a number of cases. In Takada et al.’s study, the utilization of an operating prop placed on both anterior superior iliac spines to stabilize the pelvis in the lateral position might have played a crucial role in averting excessive pelvic rotation [22]. Overall, careful attention to the potential for ipsilateral posterior pelvic rotation during cup preparation is crucial in the AL approach.
One of the discrepancies in the results of various studies may be attributed to the difference in the assisting device and mechanical guides. These guides are commonly employed without direct consideration of pelvic tilt and position [22]. While various assisting devices, notably computer-assisted navigation systems, are recognized for their potential to achieve precise cup positioning [26-31], their availability remains limited across institutions. A study analyzing registration data in the United States, conducted by Aoude et al. [32], revealed that approximately 97% of THAs were conducted without the use of any computer-assisted system at the time of their report. Concerning the learning curve, de Steiger et al. proposed that a surgeon should conduct 50 or more procedures before the revision rate aligns with that of performing 100 or more procedures [33]. Hence, our study provides valuable insights for surgeons seeking to enhance their proficiency in achieving accurate cup positioning, particularly in settings where advanced assisting devices may not be readily accessible. Furthermore, our results serve as a pertinent reference for understanding the accuracy of cup positioning in the context of the AL approach.
Maintaining the contracted external rotators through the anterior approach limits internal rotation post-THA [34]. In a PA, even with the joint capsule repaired and the tendons of the external rotator muscles sutured, the restriction on internal rotation may not be as effective as the anterior approach [35]. In a retrospective pilot study by Kishimura et al. [36] comparing the modified AL Watson-Jones approach in both supine and lateral positions, they observed that the supine position did not yield higher accuracy in cup positioning compared to the lateral position. Takada et al. also demonstrated no significant difference concerning surgical factors and early outcomes between the AL approach in the supine and lateral position [22].
This study had several limitations. Firstly, it did not follow a prospective randomized trial or a matched case-control study design. Also, the precision of cup positioning likely relied on the experience and skill of the surgeons involved. We refrained from utilizing additional assisting devices, such as mechanical guides, fluoroscopy, and computer-assisted navigation systems. The actual pelvic movement during surgery was not examined in our study. Patients with significant hip deformities were excluded from our study. Investigating the impact of the positioning of such patients during surgery on the accuracy of cup positioning is a topic worthy of exploration in future research. Also, our study solely compared the accuracy of cup positioning based on the designated safe zones. Whether a two-degree difference in inclination would translate to divergent clinical outcomes remains unclear. A more extensive investigation, including long-term follow-ups and a comparison of clinical results, should be conducted in the future.
5. Conclusion
The results indicated that the AL approach, as executed by the experienced surgeon, achieved favorable cup positioning in the majority of patients and is independent of patients’ age and gender. Furthermore, cup anteversion is an important aspect, which should be considered in the AL-THA approach.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.925). Patients’ information was de-identified before data analysis and confidentiality of patients’ information was guaranteed and protected. Based on the retrospective nature of our study, written informed consent was waived by the Ethics Committee of Iran University of Medical Sciences, and their information was obtained from their hospital records. Permission to carry out the study and access patient records was sought from the administrators of Iran University of Medical Sciences, and the study was conducted in accordance with the relevant guidelines and regulations and the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Kaveh Gharanizadeh and Karim Pisoudeh; Methodology: Karim Pisoudeh; Investigation: Mahmoodreza Sarikhani; Data collection: Mahmoodreza Sarikhani, Amir Aminian, and Mohammadreza Bahaeddini; Data analysis: Mahmoodreza Sarikhani; Writing the original draft: Mahmoodreza Sarikhani; Review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Total hip arthroplasty (THA) stands out as one of the most successful procedures in orthopedic surgery [1]. Given its status as the gold standard for addressing advanced osteoarthritis, a global increase in the number of performed THA cases is anticipated [2, 3]. Component positioning plays a crucial role in influencing THA outcomes, with improper cup positioning potentially linked to issues, such as dislocation, increased polyethylene wear, reduced abductor muscle strength, and impingement [4-11].
THA can be performed through various surgical approaches, including anterolateral (AL), direct anterior (DA), and lateral and posterior approaches (PAs) [12]. The AL approach was initially articulated by von Sprengel and Bardenheuer and subsequently, modified on multiple occasions, first by Watson-Jones and later by Harris et al. [13, 14]. This approach is associated with several advantages, such as optimal exposure of the acetabulum, precise implant positioning, leg length correction, and a reduced risk of dislocation [4, 15]. Furthermore, this approach utilizes the intermuscular plane between the tensor fascia lata and gluteus medius, innervated by the superior gluteal nerve [16].
The choice of surgical approach can impact component positioning due to variations in the visibility of critical anatomical landmarks [17]. Numerous studies have investigated the optimal orientation of the acetabular cup in THA. Lewinnek et al. recommended a safe zone for cup orientation with an inclination angle of 40±10° and an anteversion angle of 15±10° [5]. Callanan et al. reported that accurate cup placement, whether by freehand or mechanical guide techniques, depended on factors, like age, surgical approach, and the surgeon’s experience. They noted that cup alignment with the AL approach exhibited decreased accuracy compared to the PA, trending towards higher abduction angles and lower versions [17].
Objectives
In this study, we aimed to investigate the accuracy of cup position by exploring cup anteversion and inclination in patients undergoing THA by an experienced surgeon utilizing the AL approach.
2. Methods
In this cross-sectional study, we included patients undergoing THA at Shafa Yahyaiyan Hospital in Tehran, affiliated with the Iran University of Medical Sciences, from 2018 to 2023. All patients underwent AL-THA in a lateral position by an expert right-hand dominant hip orthopedic surgeon.
The inclusion criteria comprised patients requiring hip replacement due to abnormal hip pathology, including avascular osteonecrosis (AVN) of the femoral head, Crowe I and II developmental dysplasia of the hip (DDH), hip degenerative joint disease (DJD), and a previous history of a femoral neck fracture. Exclusion criteria included patients undergoing revision surgery, those with a history of Perthes disease, types III and IV DDH, and individuals with pathological fractures during childhood.
Post-operative radiological evaluations were conducted, with all radiographic performed in an anteroposterior (AP) manner with a 15-degree intra-rotation of the hip, following standard hip radiographic assessment protocols [18, 19]. Anteversion and inclination were assessed using a method previously described by Widmer et al. [20] (Figure 1), determining whether the values fell within the safe zone (inclination angle of 40±10° and an anteversion angle of 15±10°) [5]. A single orthopedic surgeon evaluated the radiographs. Patients’ age and gender were also documented.
Collected data were entered into SPSS software, version 26 for statistical analysis and comparisons. The normality of data was evaluated by the Kolmogorov-Smirnov test. Categorical variables are presented as frequency and percentage (%), while continuous variables are presented with Mean±SD for normally distributed data, and median with first and third quantiles [Q1–Q3] for non-normal data. Statistical analysis involved using the chi-square or Fisher’s exact test for categorical variables (gender and side of operation) and an independent t-test for age. A P<0.05 was considered statistically significant.
3. Results
Among 166 patients, 91 cases were entered into our final analysis based on accurate radiographic imaging and complete data in their files. The patients’ age ranged from 18 to 80 years, with the majority being in the age group of 46 to 65 years. The majority of patients were male (52.7%). The etiology of hip pathology included fracture of the femoral neck in 11(12.1%), AVN in 36(39.6%), DJD in 18(19.8%) and DDH in 26(28.6%) cases. Table 1 presents the characteristics of the patients in our study.

The angle of inclination ranged from 12 to 59°, while the angle of anteversion ranged from 6 to 46°. By considering a safe zone for cup orientation with an inclinationangle of 40±10°, 69 patients (75.8%) were within the safe zone, and by considering an anteversion angle of 15±10°, 46 cases (50.5%) were within the safe zone. Table 2 demonstrates the features of the patients based on their presence in the safe zone.
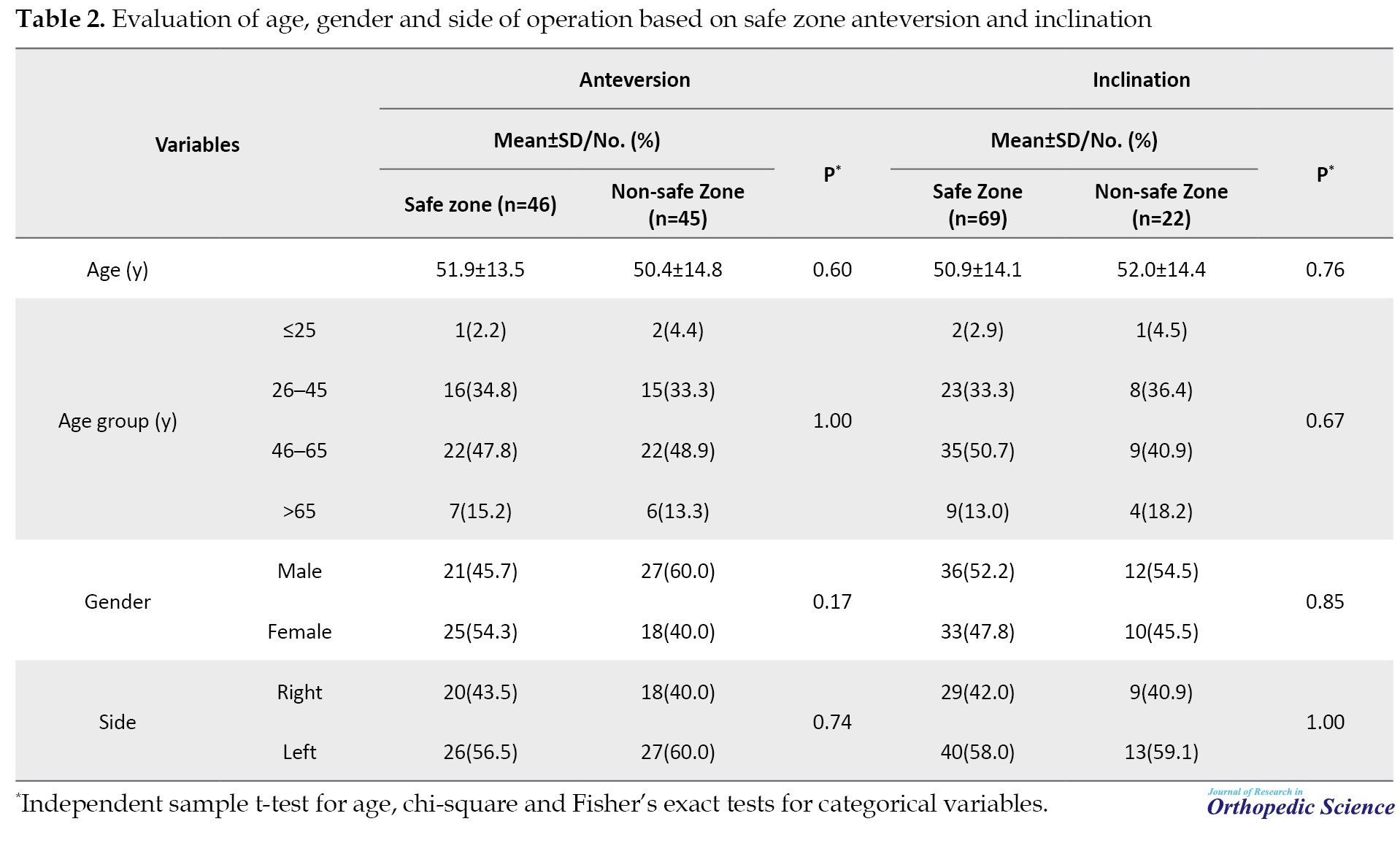
As demonstrated, none of the variables in our study showed a significant association with anteversion and inclination safe zones.
Regarding the inclination angle, out of the 22 cases that were outside the safe zone, 20(22.0%) had angles below 30° and two (2.2%) had angles exceeding 50°. In terms of the anteversion angle, all 45 cases outside the safe zone had angles greater than 25°. The median level of anteversion deviation from the safe zone was 4° [Q1–Q3: 1–9]. Figure 2 demonstrates the scatter plot of the cases in our study based on anteversion and inclination.
4. Discussion
The positioning of components plays a crucial role in the functionality and durability of THA [21]. In this study, we aimed to evaluate the accuracy of component positioning in AL-THA, particularly based on radiographic anteversion and inclination. Our findings indicated that based on the determined safe zone, the majority of patients (75.8%) were within the safe zone of inclination, while approximately half (50.5%) of the patients were within the safe zone of anteversion, indicating that the majority of patients were in the safe zone of cup orientation.
The most concerning factor in our study was that around half of the patients had an anteversion angle outside our safe zone, with a mean deviation of 4° larger than the designated safe zone. Similar findings were also reported in other studies utilizing the anterior approach. Takada et al. [22] noted that the positive error of anteversion was consistently higher than the negative error in the AL, indicating that the majority of cups were implanted with greater anteversion than initially targeted. Maeda et al. [23] also reported a similar trend in radiographic cup anteversion in the AL approach, with values exceeding their target angle by 4.3°, which was similar to our findings. They suggested that the larger anteversion might be attributed to pelvic rotation induced by the retractor placed at the posterior acetabular wall, causing the femoral bone to retract and rotating the ipsilateral pelvis posteriorly during cup preparation. Iwakiri et al. [24] stated that by employing the muscle-sparing modified Watson-Jones AL approach, the deviation from the targeted angle was 3.5±3.1° in inclination and 4.6±4.6° in anteversion. Kawarai et al. [25] also noted the possibility of such rotational instability occurring in the AL approach, similar to the DA approach. This pelvic rotation during surgery could elucidate the prevalence of positive values in the target error of anteversion observed in both groups. Additionally, the angle of inclination ranged from 12 to 59°, while the angle of anteversion ranged from 6 to 46°, suggesting extreme pelvic rotation during surgery in a number of cases. In Takada et al.’s study, the utilization of an operating prop placed on both anterior superior iliac spines to stabilize the pelvis in the lateral position might have played a crucial role in averting excessive pelvic rotation [22]. Overall, careful attention to the potential for ipsilateral posterior pelvic rotation during cup preparation is crucial in the AL approach.
One of the discrepancies in the results of various studies may be attributed to the difference in the assisting device and mechanical guides. These guides are commonly employed without direct consideration of pelvic tilt and position [22]. While various assisting devices, notably computer-assisted navigation systems, are recognized for their potential to achieve precise cup positioning [26-31], their availability remains limited across institutions. A study analyzing registration data in the United States, conducted by Aoude et al. [32], revealed that approximately 97% of THAs were conducted without the use of any computer-assisted system at the time of their report. Concerning the learning curve, de Steiger et al. proposed that a surgeon should conduct 50 or more procedures before the revision rate aligns with that of performing 100 or more procedures [33]. Hence, our study provides valuable insights for surgeons seeking to enhance their proficiency in achieving accurate cup positioning, particularly in settings where advanced assisting devices may not be readily accessible. Furthermore, our results serve as a pertinent reference for understanding the accuracy of cup positioning in the context of the AL approach.
Maintaining the contracted external rotators through the anterior approach limits internal rotation post-THA [34]. In a PA, even with the joint capsule repaired and the tendons of the external rotator muscles sutured, the restriction on internal rotation may not be as effective as the anterior approach [35]. In a retrospective pilot study by Kishimura et al. [36] comparing the modified AL Watson-Jones approach in both supine and lateral positions, they observed that the supine position did not yield higher accuracy in cup positioning compared to the lateral position. Takada et al. also demonstrated no significant difference concerning surgical factors and early outcomes between the AL approach in the supine and lateral position [22].
This study had several limitations. Firstly, it did not follow a prospective randomized trial or a matched case-control study design. Also, the precision of cup positioning likely relied on the experience and skill of the surgeons involved. We refrained from utilizing additional assisting devices, such as mechanical guides, fluoroscopy, and computer-assisted navigation systems. The actual pelvic movement during surgery was not examined in our study. Patients with significant hip deformities were excluded from our study. Investigating the impact of the positioning of such patients during surgery on the accuracy of cup positioning is a topic worthy of exploration in future research. Also, our study solely compared the accuracy of cup positioning based on the designated safe zones. Whether a two-degree difference in inclination would translate to divergent clinical outcomes remains unclear. A more extensive investigation, including long-term follow-ups and a comparison of clinical results, should be conducted in the future.
5. Conclusion
The results indicated that the AL approach, as executed by the experienced surgeon, achieved favorable cup positioning in the majority of patients and is independent of patients’ age and gender. Furthermore, cup anteversion is an important aspect, which should be considered in the AL-THA approach.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1402.925). Patients’ information was de-identified before data analysis and confidentiality of patients’ information was guaranteed and protected. Based on the retrospective nature of our study, written informed consent was waived by the Ethics Committee of Iran University of Medical Sciences, and their information was obtained from their hospital records. Permission to carry out the study and access patient records was sought from the administrators of Iran University of Medical Sciences, and the study was conducted in accordance with the relevant guidelines and regulations and the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Kaveh Gharanizadeh and Karim Pisoudeh; Methodology: Karim Pisoudeh; Investigation: Mahmoodreza Sarikhani; Data collection: Mahmoodreza Sarikhani, Amir Aminian, and Mohammadreza Bahaeddini; Data analysis: Mahmoodreza Sarikhani; Writing the original draft: Mahmoodreza Sarikhani; Review & editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Varacallo M, Chakravarty R, Denehy K, Star A. Joint perception and patient perceived satisfaction after total hip and knee arthroplasty in the American population. J Orthop. 2018; 15(2):495-9. [DOI:10.1016/j.jor.2018.03.018] [PMID] [PMCID]
- Singh JA, Yu S, Chen L, Cleveland JD. Rates of total joint replacement in the United States: Future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019; 46(9):1134-40. [DOI:10.3899/jrheum.170990] [PMID]
- Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018; 100(17):1455-60. [DOI:10.2106/JBJS.17.01617] [PMID]
- Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. J Arthroplasty. 2002; 17(3):282-8. [DOI:10.1054/arth.2002.30286] [PMID]
- Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978; 60(2):217-20. [DOI:10.2106/00004623-197860020-00014] [PMID]
- Kim YH, Choi Y, Kim JS. Influence of patient-, design, and surgery-related factors on rate of dislocation after primary cementless total hip arthroplasty. J Arthroplasty. 2009; 24(8):1258-63. [DOI:10.1016/j.arth.2009.09.005] [PMID]
- Seagrave KG, Troelsen A, Malchau H, Husted H, Gromov K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop. 2017; 88(1):10-7. [DOI:10.1080/17453674.2016.1251255] [PMID] [PMCID]
- Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998; 13(5):530-4. [DOI:10.1016/S0883-5403(98)90052-3] [PMID]
- Leslie IJ, Williams S, Isaac G, Ingham E, Fisher J. High cup angle and microseparation increase the wear of hip surface replacements. Clin Orthop Relat Res. 2009; 467(9):2259-65. [DOI:10.1007/s11999-009-0830-x] [PMID] [PMCID]
- Cassidy KA, Noticewala MS, Macaulay W, Lee JH, Geller JA. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012; 27(10):1863-9. [DOI:10.1016/j.arth.2012.05.001] [PMID]
- Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010; 25(8):1275-81.e1. [DOI:10.1016/j.arth.2009.10.007] [PMID]
- Aggarwal VK, Iorio R, Zuckerman JD, Long WJ. Surgical approaches for primary total hip arthroplasty from charnley to now: The quest for the best approach. JBJS Rev. 2020; 8(1):e0058. [DOI:10.2106/JBJS.RVW.19.00058] [PMID]
- Watson-Jones R. Fractures of the neck of the femur. British Journal of Surgery. 1936; 23(92):787-808. [DOI: 10.1002/bjs.1800239213]
- Harris WH. A new lateral approach to the hip joint. J Bone Joint Surg Am. 1967; 49(5):891-8. [PMID]
- Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002; (405):46-53. [DOI:10.1097/00003086-200212000-00006] [PMID]
- Palan J, Beard DJ, Murray DW, Andrew JG, Nolan J. Which approach for total hip arthroplasty: Anterolateral or posterior? Clin Orthop Relat Res. 2009; 467(2):473-7. [DOI:10.1007/s11999-008-0560-5] [PMID] [PMCID]
- Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley award: Risk factors for cup malpositioning: Quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011; 469(2):319-29. [DOI:10.1007/s11999-010-1487-1] [PMID] [PMCID]
- Lim SJ, Park YS. Plain radiography of the hip: A review of radiographic techniques and image features. Hip Pelvis. 2015; 27(3):125-34. [DOI:10.5371/hp.2015.27.3.125] [PMID] [PMCID]
- Salimi A, Mirghaderi SP, Gholamzadeh MJ, Qahremani R, Hadizadeh A, Shahriarirad R, et al. Evaluation of crossover sign in pelvis models made with a three-dimensional printer. Adv Orthop. 2022; 2022:4665342. [DOI:10.1155/2022/4665342] [PMID] [PMCID]
- Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004; 19(3):387-90. [DOI:10.1016/j.arth.2003.10.016] [PMID]
- Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008; 23(1):51-6. [DOI:10.1016/j.arth.2007.06.008] [PMID]
- Takada R, Jinno T, Miyatake K, Hirao M, Yagishita K, Yoshii T, et al. Supine versus lateral position for accurate positioning of acetabular cup in total hip arthroplasty using the modified Watson-Jones approach: A randomized single-blind controlled trial. Orthop Traumatol Surg Res. 2019; 105(5):915-22. [DOI:10.1016/j.otsr.2019.05.004] [PMID]
- Maeda Y, Sugano N, Nakamura N, Hamawaki M. The accuracy of a mechanical cup alignment guide in total hip arthroplasty (THA) through direct anterior and posterior approaches measured with CT-based navigation. J Arthroplasty. 2015; 30(9):1561-4. [DOI:10.1016/j.arth.2015.04.011] [PMID]
- Iwakiri K, Kobayashi A, Ohta Y, Minoda Y, Takaoka K, Nakamura H. Efficacy of a pelvic lateral positioner with a mechanical cup navigator based on the anatomical pelvic plane in total hip arthroplasty. J Arthroplasty. 2017; 32(12):3659-64. [DOI:10.1016/j.arth.2017.06.033] [PMID]
- Kawarai Y, Iida S, Nakamura J, Shinada Y, Suzuki C, Ohtori S. Does the surgical approach influence the implant alignment in total hip arthroplasty? Comparative study between the direct anterior and the anterolateral approaches in the supine position. Int Orthop. 2017; 41(12):2487-93. [DOI:10.1007/s00264-017-3521-3] [PMID]
- Gurgel HM, Croci AT, Cabrita HA, Vicente JR, Leonhardt MC, Rodrigues JC. Acetabular component positioning in total hip arthroplasty with and without a computer-assisted system: A prospective, randomized and controlled study. J Arthroplasty. 2014; 29(1):167-71. [DOI:10.1016/j.arth.2013.04.017] [PMID]
- Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br. 2007; 89(4):455-60. [DOI:10.1302/0301-620X.89B4.18458] [PMID]
- Lass R, Kubista B, Olischar B, Frantal S, Windhager R, Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: A prospective randomized study. J Arthroplasty. 2014; 29(4):786-91. [DOI:10.1016/j.arth.2013.08.020] [PMID]
- Billaud A, Verdier N, de Bartolo R, Lavoinne N, Chauveaux D, Fabre T. Acetabular component navigation in lateral decubitus based on EOS imaging: A preliminary study of 13 cases. Orthop Traumatol Surg Res. 2015; 101(3):271-5. [DOI:10.1016/j.otsr.2015.01.010] [PMID]
- Verdier N, Billaud A, Masquefa T, Pallaro J, Fabre T, Tournier C. EOS-based cup navigation: Randomised controlled trial in 78 total hip arthroplasties. Orthop Traumatol Surg Res. 2016; 102(4):417-21. [DOI:10.1016/j.otsr.2016.02.006] [PMID]
- Bhimani R, Shahriarirad R, Ranjbar K, Erfani A, Ashkani-Esfahani S. Transportal versus all-inside techniques of anterior cruciate ligament reconstruction: A systematic review. J Orthop Surg Res. 2021; 16(1):734. [DOI:10.1186/s13018-021-02872-x] [PMID] [PMCID]
- Aoude AA, Aldebeyan SA, Nooh A, Weber MH, Tanzer M. Thirty-day complications of conventional and computer-assisted total knee and total hip arthroplasty: Analysis of 103,855 patients in the american college of surgeons national surgical quality improvement program database. J Arthroplasty. 2016; 31(8):1674-9. [DOI:10.1016/j.arth.2016.01.042] [PMID]
- de Steiger RN, Lorimer M, Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res. 2015; 473(12):3860-6. [DOI:10.1007/s11999-015-4565-6] [PMID] [PMCID]
- Akiyama K, Nakata K, Kitada M, Yamamura M, Ohori T, Owaki H, et al. Changes in axial alignment of the ipsilateral hip and knee after total hip arthroplasty. Bone Joint J. 2016; 98-B(3):349-58. [DOI:10.1302/0301-620X.98B3.35468] [PMID]
- Pellicci PM, Potter HG, Foo LF, Boettner F. MRI shows biologic restoration of posterior soft tissue repairs after THA. Clin Orthop Relat Res. 2009; 467(4):940-5. [DOI:10.1007/s11999-008-0503-1] [PMID] [PMCID]
- Kishimura Y, Minoda Y, Mizokawa S, Sugama R, Ohta Y, Nakamura H. Cup alignment in total hip arthroplasty using the muscle-sparing modified Watson-Jones approach-comparison between lateral and supine positions. Int Orthop. 2019; 43(11):2477-83. [DOI:10.1007/s00264-019-04316-y] [PMID]
Type of Study: Research Article |
Subject:
Hip surgery
Received: 2022/04/17 | Accepted: 2022/06/5 | Published: 2022/08/1
Received: 2022/04/17 | Accepted: 2022/06/5 | Published: 2022/08/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |