Volume 10, Issue 1 (2-2023)
JROS 2023, 10(1): 7-14 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zabihiyeganeh M, Rezaee A, Aminiana A, Bahaeddini M, Sarikhani M, Mirzaei A. Assessment of Refracture Rates and Associated Risk Factors Among Patients With Osteoporotic Fractures: A Cross-sectional Study. JROS 2023; 10 (1) :7-14
URL: http://jros.iums.ac.ir/article-1-2231-en.html
URL: http://jros.iums.ac.ir/article-1-2231-en.html
Mozhdeh Zabihiyeganeh1 

 , Aryan Rezaee1
, Aryan Rezaee1 

 , Amir Aminiana1
, Amir Aminiana1 

 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 
 , Mahmoodreza Sarikhani1
, Mahmoodreza Sarikhani1 

 , Alireza Mirzaei1
, Alireza Mirzaei1 




 , Aryan Rezaee1
, Aryan Rezaee1 

 , Amir Aminiana1
, Amir Aminiana1 

 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 
 , Mahmoodreza Sarikhani1
, Mahmoodreza Sarikhani1 

 , Alireza Mirzaei1
, Alireza Mirzaei1 


1- Department of Orthopedics, School of Medicine, Bone and Joint Reconstruction Research Center, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 551 kb]
(312 Downloads)
| Abstract (HTML) (890 Views)
Full-Text: (225 Views)
Introduction
Osteoporosis is a skeletal disorder marked by a decline in bone mass and quality, leading to diminished bone strength and an elevated risk of fractures. The consequences of osteoporotic fractures are noteworthy, encompassing considerable physical and psychological effects [1, 2]. The condition of osteoporosis typically lacks noticeable symptoms, and its initial clinical indication often emerges in the form of a low-impact (fragility) fracture. This fragility contributes significantly to both morbidity and mortality, presenting a substantial public health challenge [3]. The adverse outcomes, measured in terms of disability-adjusted life years, surpass those associated with numerous other chronic health conditions [4]. According to the Bone Health & Osteoporosis Foundation (BHOF), approximately 10.2 million Americans had osteoporosis in 2010, with statistics indicating that 1 in 2 women and 1 in 5 men will experience an osteoporotic-related fracture at some point in their lives [5]. Notably, a prior low-impact fracture, regardless of location, elevates the risk of subsequent fractures by about two-fold in both women and men [6, 7]. This condition poses a significant burden on individuals, as well as on a societal and global scale, affecting mortality and morbidity at national and international levels [8-10].
Refracture following an osteoporotic fracture refers to the occurrence of bone fracture in an individual who has previously experienced an osteoporotic fracture. Individuals with osteoporosis or bone fragility are generally at risk of recurrent fractures due to decreased bone density and structural weakness. These fractures usually occur in weaker areas of the bone, such as the spine, hip, and wrist [11, 12].
Diagnostic imaging such as an x-ray, CT scan, or MRI can help diagnose a fracture following an osteoporotic fracture. These images assist the physician in determining whether a new fracture has occurred and, if so, its severity [13, 14].
The management of refracture following an osteoporotic fracture relies on preventing bone weakening, minimizing the risk of recurring fractures, and expediting fracture recovery. The treatment approach may encompass osteoporosis management, vitamin D supplementation and a nutritious diet, rehabilitation, physiotherapy interventions, and the utilization of assistive devices [15].
Fracture liaison service (FLS) provides models for coordinating secondary fracture prevention services that cover various activities. The primary objective of FLS is to identify people at risk of a secondary fracture, conduct comprehensive assessments, and ensure that appropriate treatment is initiated through increased coordination and communication [16-18].
Guidelines from the American Society for Bone and Mineral Research (ASBMR) [19] and the European Alliance of Associations for Rheumatology (EULAR)/European Federation of National Associations of Orthopaedics and Traumatology (EFORT) [20] recommend the establishment of FLS services to prevent secondary bone fractures. Notably, FLS has played a crucial role in enhancing bone mineral density (BMD) testing rates and the initiation of treatment post major fragility fractures, mainly when FLS adopts a comprehensive and coordinated approach to patient care, as evidenced by a meta-analysis conducted in 2012, covering publications from 1996 to 2011 [21].
Despite these advancements, there are still gaps in treatment, and pharmacological prevention has remained suboptimal [21]. In 2013, the International Osteoporosis Foundation (IOF) began promoting FLS programs that are consistently implemented globally, although results show considerable variability in the existing literature.
Objectives
Recognizing that preventing recurrent fractures resulting from osteoporosis is crucial for averting a decline in physical activity and enhancing the quality of life (QoL) in individuals with osteoporosis, it becomes imperative to pay attention to the factors influencing the occurrence of these fractures. In this prospective cohort study, our objective was to assess the prevalence of recurrent fractures due to osteoporosis among patients attending the FLS Clinic at Shafa Yahyaeian Orthopedic Hospital, Tehran, Iran. Additionally, we examined the relationship between patient factors and the occurrence of recurrent fractures, aiming to enhance prevention and screening measures for these patients.
Methods
In this observational prospective cohort study, we included patients with osteoporosis-related fractures who were diagnosed, treated, and followed up at the FLS Clinic of Shafa Yahyaeian Orthopedic Hospital in Tehran, affiliated with Iran University of Medical Sciences, from 2021 to 2023. The sampling method was census-based, including all patients with a history of osteoporotic fractures and fulfilling the eligibility criteria.
The inclusion criteria were the occurrence of osteoporosis fractures in sensitive areas of the body. Patients with incomplete records or follow-up and those without consent were excluded from the study.
Demographic and clinical information was collected through a checklist that included age, gender, body mass index (BMI), history of rheumatic diseases or diabetes type 2, use of anti-coagulant, history of antidepressant or steroid medication, serum parathyroid (PTH) levels, serum vitamin D3 levels, BMD indices, and menopausal age.
Refracture was documented through an x-ray examination, and in cases with suspicion of fracture based on the patient’s history and clinical examination, a CT scan was requested.
The collected data were entered into SPSS software version 27 for statistical analysis and comparison. The independent t-test, chi-squared test, Mann-Whitney test, Fisher exact test, Pearson correlation, and Spearman test were used for statistical analysis. Regression analysis was employed to assess the risk factors. P<0.05 was considered statistically significant.
Results
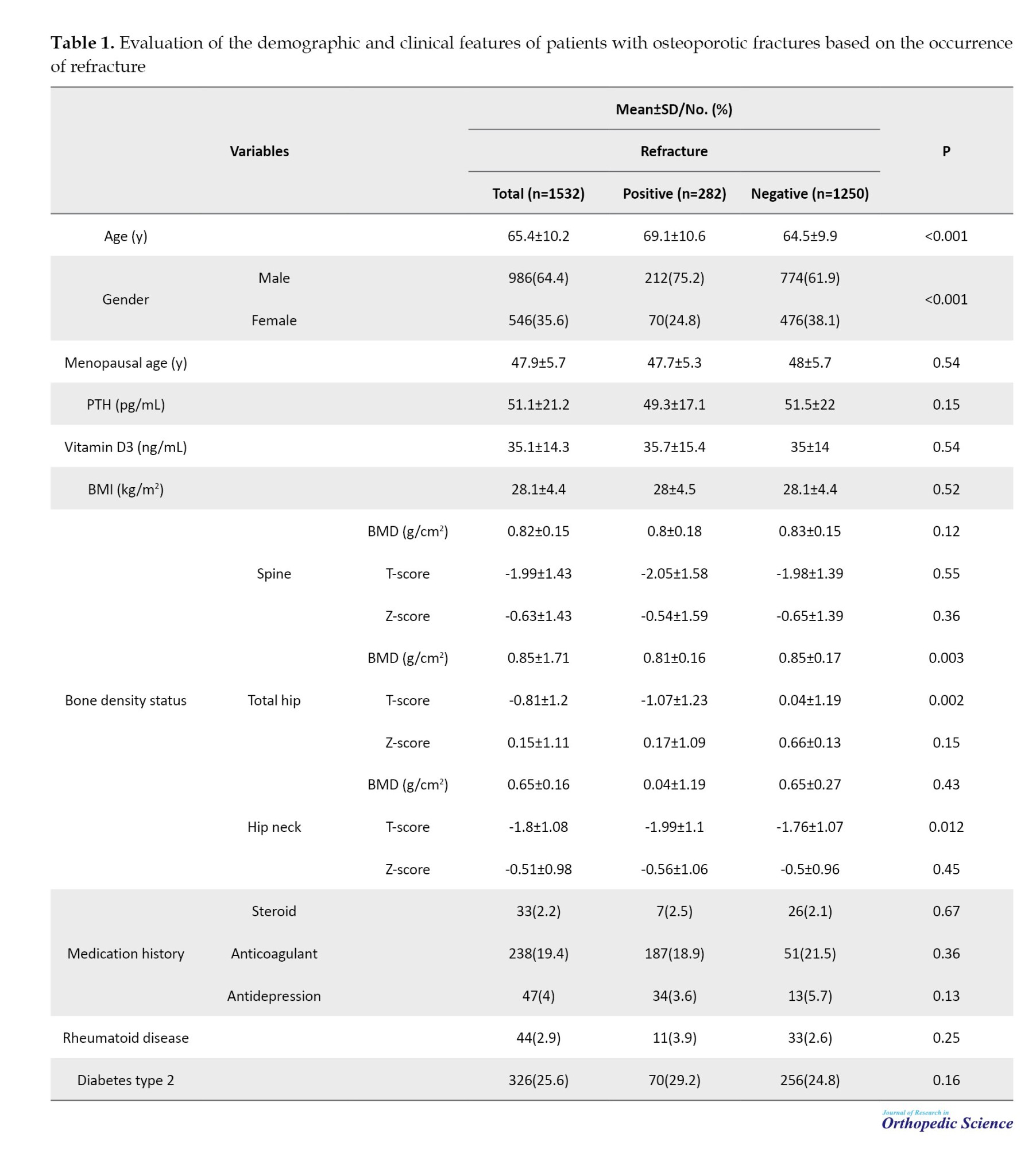
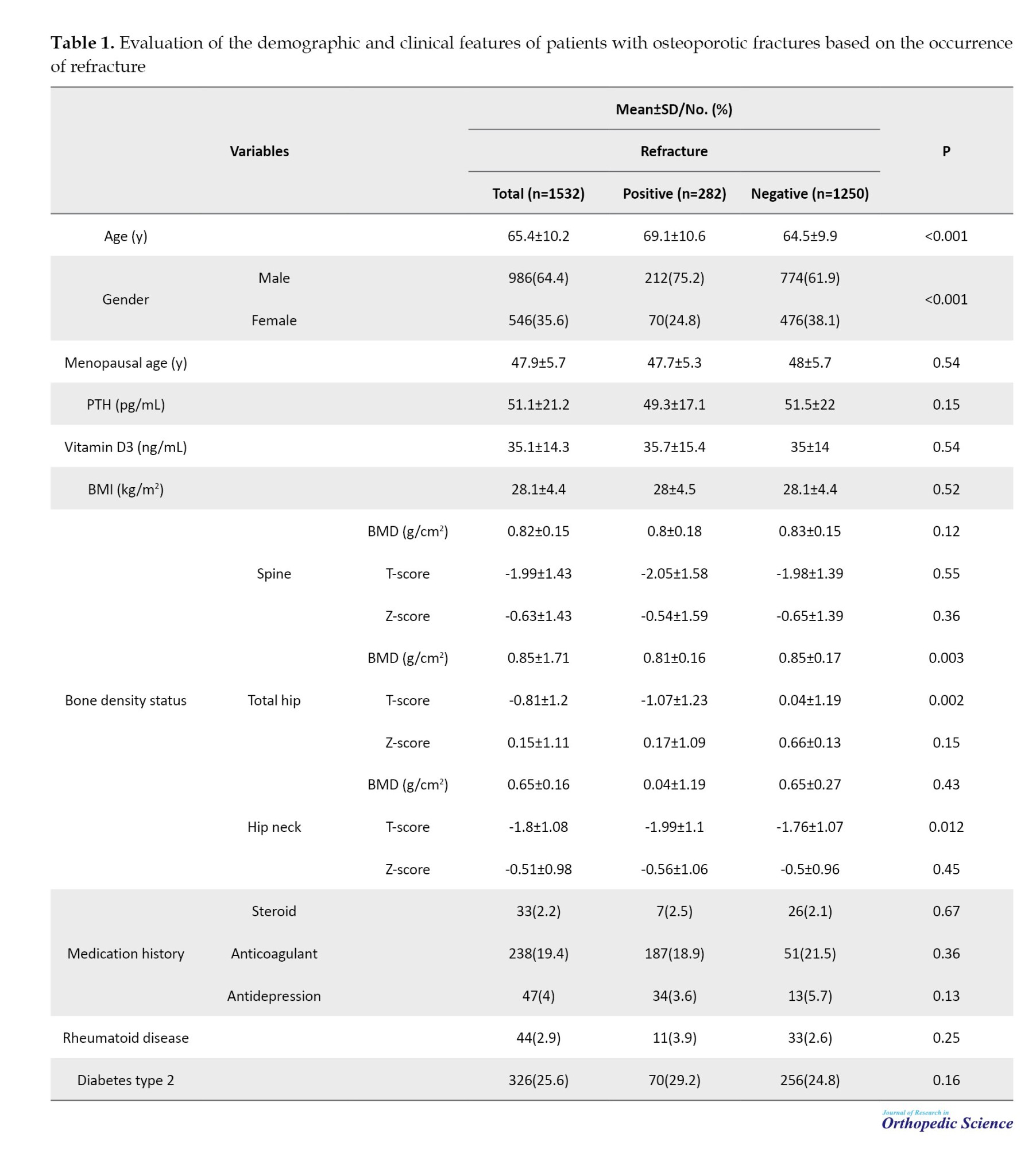
We identified and included 1532 patients with osteoporosis and a history of osteoporotic fractures from 2021 to 2023. Among the patients, 282(18.4%) developed refractures. The features of the patients are reported in Table 1. As demonstrated, only age, gender, hip (total), BMD mean and T-score, and hip (neck) T-score had a significant association with refracture.
We further evaluated our data based on regression analysis. Based on our results, only older age (P=0.005; OR=1.033) and female gender (P=0.010; OR=0.437) had a significant correlation with refracture (R2=0.040).
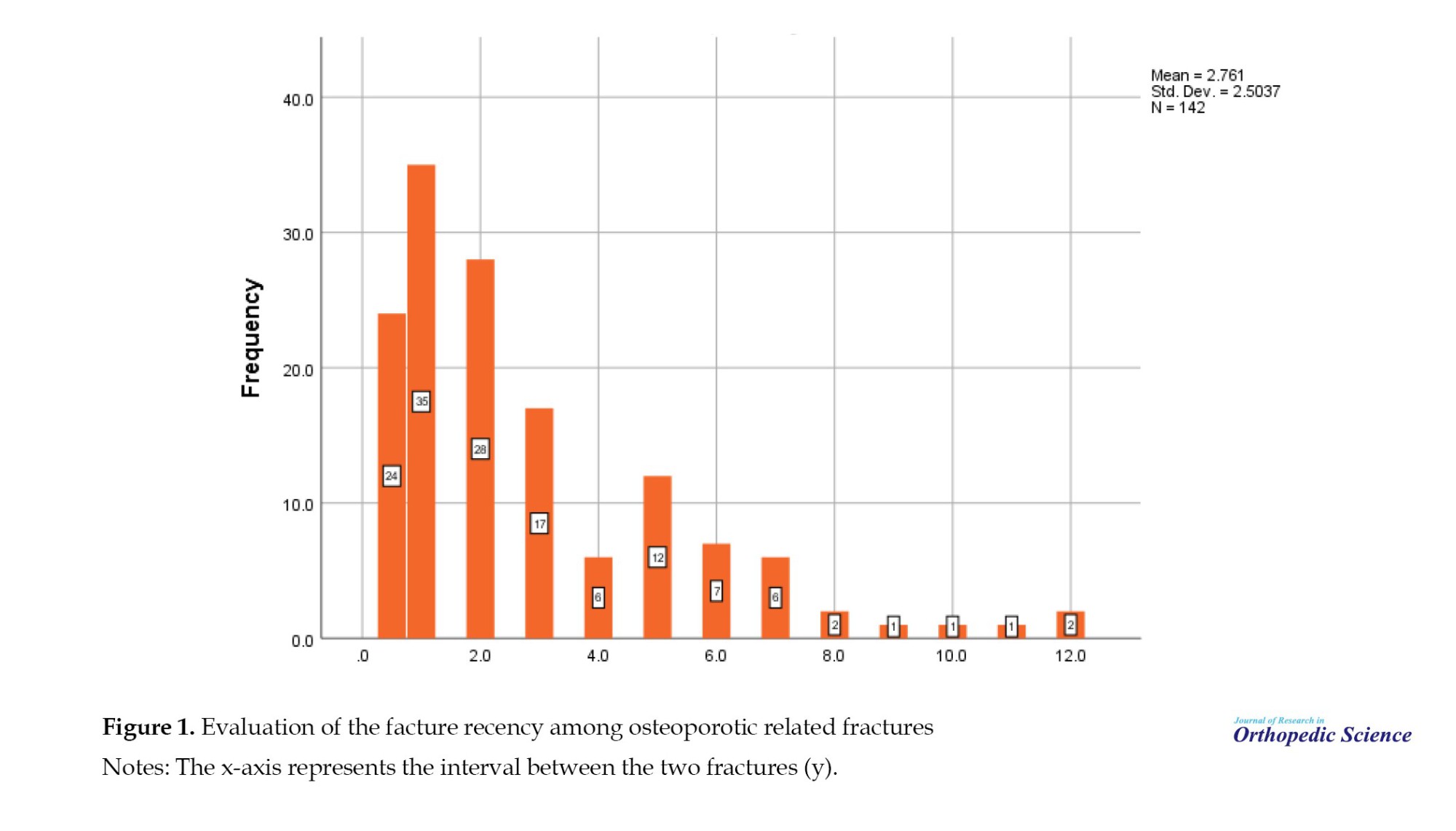
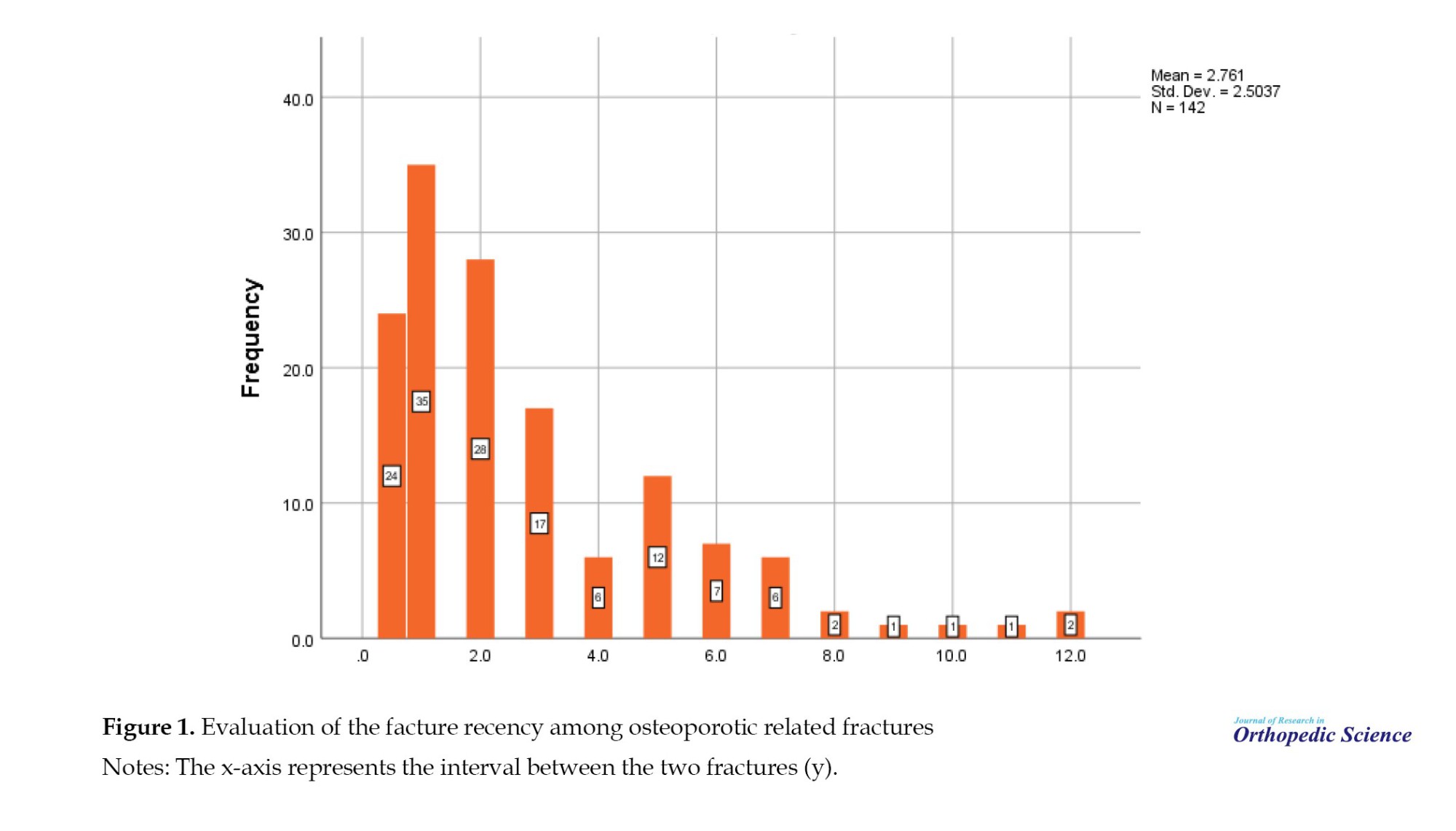
In evaluating fracture recency, the mean interval between the last two fractures was 2.8±2.5 (range: 0.5-12) years. Additionally, the mean number of previous fractures in patients with recurrent fractures in the study was 1.23±0.9. Fracture recency was mainly observed after the recent fracture, especially in the first year (41.5%) (Figure 1).
Discussion
Bone fractures represent a significant global health concern, with fractures associated with osteoporosis presenting a particularly intricate challenge in healthcare. Osteoporosis, a chronic bone disease, compromises bone integrity, elevating the susceptibility to recurrent fractures and refractures [22-24]. This study aims to discern factors influencing the heightened risk of recurrent fractures by examining the prevalence of refractures in individuals with osteoporotic fractures. The objective is to offer recommendations for prevention, diagnosis, and suitable interventions to enhance the QoL for affected individuals. A systematic literature review and meta-analysis by Wu et al. demonstrated that FLS implementation worldwide has significantly elevated rates of clinical management and treatment among individuals who have suffered fragility fractures. Consequently, there has been a notable decrease in refracture and mortality rates associated with these interventions [25]. Our study, conducted at the FLS clinic, not only aimed to assess the prevalence of refracture but also sought to enhance awareness in the field of bone health and reduce the vulnerability of individuals to refractures resulting from osteoporosis.
In our study, out of 1532 patients, 282 experienced recurrent fractures, resulting in a prevalence rate of 18.4%. A study by Shim et al. [15] in South Korea also reported a prevalence of 17.91% for recurrent fractures, closely aligning with the prevalence in our study. In a study in the US, Balasubramanian et al. [26] reported the occurrence of recurrent fractures among women over 65 years in the first and second years of their study to be 10% and 18%, respectively. Ganda et al. [27] also reported a prevalence of 20.9% over an mean follow-up duration of approximately five years.
Our prevalence was also lower than some studies, such as a study by Ma et al. [28] with a prevalence of 28.5% after two years, and also a study in New South Wales, Australia, which revealed that 35% of individuals with incident osteoporotic fractures experienced another fracture within six years [28-29].
In the evaluation of demographic features, approximately 64.5% of the study population were females, establishing a female-to-male ratio of 1.8:1, indicating a higher prevalence of females in osteoporotic fractures. Furthermore, in the context of recurrent fractures, this ratio increased to 75.2% for females, revealing a substantial association between recurrent fractures and gender, particularly favoring females. Examining the mean age, the group with recurrent fractures exhibited a significantly higher age (69 compared to 64.5 years). Regression analysis also demonstrated that higher age and female gender were independent risk factors for refracture in osteoporosis-related fractures. Ma et al. [28]also identified female gender and older age as significant risk factors influencing the occurrence and prevalence of recurrent fractures, which was 28.5% after two years.
The challenge of osteoporosis is particularly significant for elderly individuals or those with conditions that lead to diminished bone density. Physiological factors such as age, gender, hormonal status, and biological factors like fracture history, lifestyle, and nutrition play pivotal roles in recurrent fractures attributable to osteoporosis [29-32].
The analysis of fracture recency in patients with recurrent fractures reveals that the highest frequency of patients in terms of the interval between the last two fractures was less than one year, followed by two and three years, respectively. Thus, the probability of recurrent fractures significantly peaks in the initial years following the previous fracture, progressively diminishing over time.
Conclusion
Noteworthy, refracture occurs in 18.4% of cases, with women and older individuals having a higher likelihood of experiencing it. Recurrence of fractures is most common during the first year. Therefore, it is crucial to conduct timely investigations and implement targeted preventive measures to reduce the incidence of refracture. In any FLS clinic, early investigation, medical treatment, and non-pharmacological interventions for osteoporosis play a vital role in reducing the risk of refracture.
One of the limitations of this study is the scarcity of similar studies with a large sample size within the country for accurate statistical comparison and interpretation of differences.
Due to the significance of this topic, it is advisable to carry out studies with larger samples and over an extended period (using either prospective cohort or randomized controlled trials) to gain more insight into laboratory parameters and demographic variables (such as education level, employment status, income, dietary habits, and physical activity) as well as clinical and risk factors that impact the treatment outcomes. This would allow for a more precise evaluation of confounding variables.
Ethical Considerations
Compliance with ethical guidelines
The patient’s information was recorded confidentially in the present study, and no charges were applied to the patients at any study stage. Additionally, all patients (or their legal representatives) provided written informed consent. The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.106) and conducted in compliance with the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mozhdeh Zabihiyeganeh; Methodology: Alireza Mirzaei; Data collection: Aryan Rezaei; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Osteoporosis is a skeletal disorder marked by a decline in bone mass and quality, leading to diminished bone strength and an elevated risk of fractures. The consequences of osteoporotic fractures are noteworthy, encompassing considerable physical and psychological effects [1, 2]. The condition of osteoporosis typically lacks noticeable symptoms, and its initial clinical indication often emerges in the form of a low-impact (fragility) fracture. This fragility contributes significantly to both morbidity and mortality, presenting a substantial public health challenge [3]. The adverse outcomes, measured in terms of disability-adjusted life years, surpass those associated with numerous other chronic health conditions [4]. According to the Bone Health & Osteoporosis Foundation (BHOF), approximately 10.2 million Americans had osteoporosis in 2010, with statistics indicating that 1 in 2 women and 1 in 5 men will experience an osteoporotic-related fracture at some point in their lives [5]. Notably, a prior low-impact fracture, regardless of location, elevates the risk of subsequent fractures by about two-fold in both women and men [6, 7]. This condition poses a significant burden on individuals, as well as on a societal and global scale, affecting mortality and morbidity at national and international levels [8-10].
Refracture following an osteoporotic fracture refers to the occurrence of bone fracture in an individual who has previously experienced an osteoporotic fracture. Individuals with osteoporosis or bone fragility are generally at risk of recurrent fractures due to decreased bone density and structural weakness. These fractures usually occur in weaker areas of the bone, such as the spine, hip, and wrist [11, 12].
Diagnostic imaging such as an x-ray, CT scan, or MRI can help diagnose a fracture following an osteoporotic fracture. These images assist the physician in determining whether a new fracture has occurred and, if so, its severity [13, 14].
The management of refracture following an osteoporotic fracture relies on preventing bone weakening, minimizing the risk of recurring fractures, and expediting fracture recovery. The treatment approach may encompass osteoporosis management, vitamin D supplementation and a nutritious diet, rehabilitation, physiotherapy interventions, and the utilization of assistive devices [15].
Fracture liaison service (FLS) provides models for coordinating secondary fracture prevention services that cover various activities. The primary objective of FLS is to identify people at risk of a secondary fracture, conduct comprehensive assessments, and ensure that appropriate treatment is initiated through increased coordination and communication [16-18].
Guidelines from the American Society for Bone and Mineral Research (ASBMR) [19] and the European Alliance of Associations for Rheumatology (EULAR)/European Federation of National Associations of Orthopaedics and Traumatology (EFORT) [20] recommend the establishment of FLS services to prevent secondary bone fractures. Notably, FLS has played a crucial role in enhancing bone mineral density (BMD) testing rates and the initiation of treatment post major fragility fractures, mainly when FLS adopts a comprehensive and coordinated approach to patient care, as evidenced by a meta-analysis conducted in 2012, covering publications from 1996 to 2011 [21].
Despite these advancements, there are still gaps in treatment, and pharmacological prevention has remained suboptimal [21]. In 2013, the International Osteoporosis Foundation (IOF) began promoting FLS programs that are consistently implemented globally, although results show considerable variability in the existing literature.
Objectives
Recognizing that preventing recurrent fractures resulting from osteoporosis is crucial for averting a decline in physical activity and enhancing the quality of life (QoL) in individuals with osteoporosis, it becomes imperative to pay attention to the factors influencing the occurrence of these fractures. In this prospective cohort study, our objective was to assess the prevalence of recurrent fractures due to osteoporosis among patients attending the FLS Clinic at Shafa Yahyaeian Orthopedic Hospital, Tehran, Iran. Additionally, we examined the relationship between patient factors and the occurrence of recurrent fractures, aiming to enhance prevention and screening measures for these patients.
Methods
In this observational prospective cohort study, we included patients with osteoporosis-related fractures who were diagnosed, treated, and followed up at the FLS Clinic of Shafa Yahyaeian Orthopedic Hospital in Tehran, affiliated with Iran University of Medical Sciences, from 2021 to 2023. The sampling method was census-based, including all patients with a history of osteoporotic fractures and fulfilling the eligibility criteria.
The inclusion criteria were the occurrence of osteoporosis fractures in sensitive areas of the body. Patients with incomplete records or follow-up and those without consent were excluded from the study.
Demographic and clinical information was collected through a checklist that included age, gender, body mass index (BMI), history of rheumatic diseases or diabetes type 2, use of anti-coagulant, history of antidepressant or steroid medication, serum parathyroid (PTH) levels, serum vitamin D3 levels, BMD indices, and menopausal age.
Refracture was documented through an x-ray examination, and in cases with suspicion of fracture based on the patient’s history and clinical examination, a CT scan was requested.
The collected data were entered into SPSS software version 27 for statistical analysis and comparison. The independent t-test, chi-squared test, Mann-Whitney test, Fisher exact test, Pearson correlation, and Spearman test were used for statistical analysis. Regression analysis was employed to assess the risk factors. P<0.05 was considered statistically significant.
Results
We identified and included 1532 patients with osteoporosis and a history of osteoporotic fractures from 2021 to 2023. Among the patients, 282(18.4%) developed refractures. The features of the patients are reported in Table 1. As demonstrated, only age, gender, hip (total), BMD mean and T-score, and hip (neck) T-score had a significant association with refracture.
We further evaluated our data based on regression analysis. Based on our results, only older age (P=0.005; OR=1.033) and female gender (P=0.010; OR=0.437) had a significant correlation with refracture (R2=0.040).
In evaluating fracture recency, the mean interval between the last two fractures was 2.8±2.5 (range: 0.5-12) years. Additionally, the mean number of previous fractures in patients with recurrent fractures in the study was 1.23±0.9. Fracture recency was mainly observed after the recent fracture, especially in the first year (41.5%) (Figure 1).
Discussion
Bone fractures represent a significant global health concern, with fractures associated with osteoporosis presenting a particularly intricate challenge in healthcare. Osteoporosis, a chronic bone disease, compromises bone integrity, elevating the susceptibility to recurrent fractures and refractures [22-24]. This study aims to discern factors influencing the heightened risk of recurrent fractures by examining the prevalence of refractures in individuals with osteoporotic fractures. The objective is to offer recommendations for prevention, diagnosis, and suitable interventions to enhance the QoL for affected individuals. A systematic literature review and meta-analysis by Wu et al. demonstrated that FLS implementation worldwide has significantly elevated rates of clinical management and treatment among individuals who have suffered fragility fractures. Consequently, there has been a notable decrease in refracture and mortality rates associated with these interventions [25]. Our study, conducted at the FLS clinic, not only aimed to assess the prevalence of refracture but also sought to enhance awareness in the field of bone health and reduce the vulnerability of individuals to refractures resulting from osteoporosis.
In our study, out of 1532 patients, 282 experienced recurrent fractures, resulting in a prevalence rate of 18.4%. A study by Shim et al. [15] in South Korea also reported a prevalence of 17.91% for recurrent fractures, closely aligning with the prevalence in our study. In a study in the US, Balasubramanian et al. [26] reported the occurrence of recurrent fractures among women over 65 years in the first and second years of their study to be 10% and 18%, respectively. Ganda et al. [27] also reported a prevalence of 20.9% over an mean follow-up duration of approximately five years.
Our prevalence was also lower than some studies, such as a study by Ma et al. [28] with a prevalence of 28.5% after two years, and also a study in New South Wales, Australia, which revealed that 35% of individuals with incident osteoporotic fractures experienced another fracture within six years [28-29].
In the evaluation of demographic features, approximately 64.5% of the study population were females, establishing a female-to-male ratio of 1.8:1, indicating a higher prevalence of females in osteoporotic fractures. Furthermore, in the context of recurrent fractures, this ratio increased to 75.2% for females, revealing a substantial association between recurrent fractures and gender, particularly favoring females. Examining the mean age, the group with recurrent fractures exhibited a significantly higher age (69 compared to 64.5 years). Regression analysis also demonstrated that higher age and female gender were independent risk factors for refracture in osteoporosis-related fractures. Ma et al. [28]also identified female gender and older age as significant risk factors influencing the occurrence and prevalence of recurrent fractures, which was 28.5% after two years.
The challenge of osteoporosis is particularly significant for elderly individuals or those with conditions that lead to diminished bone density. Physiological factors such as age, gender, hormonal status, and biological factors like fracture history, lifestyle, and nutrition play pivotal roles in recurrent fractures attributable to osteoporosis [29-32].
The analysis of fracture recency in patients with recurrent fractures reveals that the highest frequency of patients in terms of the interval between the last two fractures was less than one year, followed by two and three years, respectively. Thus, the probability of recurrent fractures significantly peaks in the initial years following the previous fracture, progressively diminishing over time.
Conclusion
Noteworthy, refracture occurs in 18.4% of cases, with women and older individuals having a higher likelihood of experiencing it. Recurrence of fractures is most common during the first year. Therefore, it is crucial to conduct timely investigations and implement targeted preventive measures to reduce the incidence of refracture. In any FLS clinic, early investigation, medical treatment, and non-pharmacological interventions for osteoporosis play a vital role in reducing the risk of refracture.
One of the limitations of this study is the scarcity of similar studies with a large sample size within the country for accurate statistical comparison and interpretation of differences.
Due to the significance of this topic, it is advisable to carry out studies with larger samples and over an extended period (using either prospective cohort or randomized controlled trials) to gain more insight into laboratory parameters and demographic variables (such as education level, employment status, income, dietary habits, and physical activity) as well as clinical and risk factors that impact the treatment outcomes. This would allow for a more precise evaluation of confounding variables.
Ethical Considerations
Compliance with ethical guidelines
The patient’s information was recorded confidentially in the present study, and no charges were applied to the patients at any study stage. Additionally, all patients (or their legal representatives) provided written informed consent. The study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.REC.1401.106) and conducted in compliance with the Declaration of Helsinki.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mozhdeh Zabihiyeganeh; Methodology: Alireza Mirzaei; Data collection: Aryan Rezaei; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Papaioannou A, Kennedy CC, Ioannidis G, Sawka A, Hopman WM, Pickard L, et al. The impact of incident fractures on health-related quality of life: 5 years of data from the Canadian multicentre osteoporosis study. Osteoporos Int. 2009; 20:703-14. [DOI:10.1007/s00198-008-0743-7]
- Johari HG, Erfani MA, Erfani A, Shahriarirad R, Karami MM. Profunda brachii pseudoaneurysm following supracondylar fracture of humerus repair in an 8-year-old boy: A case report and review of literature. Case Rep Orthop. 2021; 2021(1):1768529. [DOI:10.1155/2021/1768529]
- Curtis JR, Cai Q, Wade SW, Stolshek BS, Adams JL, Balasubramanian A, et al. Osteoporosis medication adherence: Physician perceptions vs. patients’ utilization. Bone. 2013; 55(1):1-6. [DOI:10.1016/j.bone.2013.03.003]
- Johnell O, Kanis J. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17:1726-33. [DOI:10.1007/s00198-006-0172-4]
- Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014; 29(11):2520-6. [DOI:10.1002/jbmr.2269]
- Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR. Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: The dubbo osteoporosis epidemiology study. J Bone Miner Res. 2015; 30(4):637-46. [DOI:10.1002/jbmr.2393]
- Kanis J, Johnell O, De Laet C, Johansson H, Odén A, Delmas P, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004; 35(2):375-82. [DOI:10.1016/j.bone.2004.03.024]
- Department of Health, Western Australia. Osteoporosis Model of Care. Perth: Health Networks Branch, Department of Health, Western Australia; 2011.
- Watts J, Abimanyi-Ochom J, Sanders KM. Osteoporosis costing all Australian: A new burden of disease analysis-2012 to 2022. Geelong: Deakin University; 2013. [Link]
- Mithal A, Bansal B, Kyer CS, Ebeling P. The Asia-pacific regional audit-epidemiology, costs, and burden of osteoporosis in India 2013: A report of international osteoporosis foundation. Indian J Endocrinol Metabol. 2014; 18(4):449. [DOI:10.4103/2230-8210.137485]
- Hadji P, Schweikert B, Kloppmann E, Gille P, Joeres L, Toth E, et al. Osteoporotic fractures and subsequent fractures: Imminent fracture risk from an analysis of German real-world claims data. Arch Gynecol Obstet. 2021; 304:703-12. [DOI:10.1007/s00404-021-06123-6]
- Ji C, Rong Y, Wang J, Yu S, Yin G, Fan J, et al. Risk factors for refracture following primary osteoporotic vertebral compression fractures. Pain Physician. 2021; 24(3):E335-40. [DOI:10.36076/ppj.2021/24/E335]
- Simpson AH, Murray IR. Osteoporotic fracture models. Current osteoporosis reports. Curr Osteoporos Rep. 2015; 13:9-15. [DOI:10.1007/s11914-014-0246-8]
- Hashemi SA, Ranjbar MR, Tahami M, Shahriarirad R, Erfani A. Comparison of accuracy in expert clinical examination versus magnetic resonance imaging and arthroscopic exam in diagnosis of meniscal tear. Adv Orthop. 2020; 2020(1):1895852. [DOI:10.1155/2020/1895852]
- Shim YB, Park JA, Nam JH, Hong SH, Kim JW, Jeong J, et al. Incidence and risk factors of subsequent osteoporotic fracture: A nationwide cohort study in South Korea. Arch Osteoporos. 2020; 15:180. [DOI:10.1007/s11657-020-00852-y]
- Akesson K, Marsh D, Mitchell P, McLellan A, Stenmark J, Pierroz D, et al. Capture the fracture: A best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013; 24:2135-52. [DOI:10.1007/s00198-013-2348-z]
- Miller AN, Lake AF, Emory CL. Establishing a fracture liaison service: An orthopaedic approach. J Bone Joint Surg. 2015; 97(8):675-81. [DOI:10.2106/JBJS.N.00957]
- Walters S, Khan T, Ong T, Sahota O. Fracture liaison services: Improving outcomes for patients with osteoporosis. Clin Interv Aging. 2017; 2017:117-27. [DOI:10.2147/CIA.S85551]
- Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney Jr RE, McLellan A, et al. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. 2012; 27(10):2039-46. [DOI:10.1002/jbmr.1698]
- Lems WF, Dreinhöfer K, Bischoff-Ferrari H, Blauth M, Czerwinski E, da Silva JA, et al. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis. 2017; 76(5):802-10. [DOI:10.1136/annrheumdis-2016-210289]
- Ganda K, Puech M, Chen J, Speerin R, Bleasel J, Center J, et al. Models of care for the secondary prevention of osteoporotic fractures: A systematic review and meta-analysis. Osteoporos Int. 2013; 24:393-406. [DOI:10.1007/s00198-012-2090-y]
- Robey PG. The biochemistry of bone. Endocrinol Metab Clin N Am. 1989; 18(4):859-902. [DOI:10.1016/S0889-8529(18)30347-5]
- Bhimani R, Shahriarirad R, Ranjbar K, Erfani A, Ashkani-Esfahani S. Transportal versus all-inside techniques of anterior cruciate ligament reconstruction: A systematic review. J Orthop Surg Res. 2021; 16(1):734. [DOI:10.1186/s13018-021-02872-x]
- Hashemi SA, Azad A, Erfani A, Shahriarirad R, Azarpira N. Promising results of captopril in improving knee arthrofibrosis and cartilage status: An animal model study. J Exp Orthop. 2022; 9(1):72. [DOI:10.1186/s40634-022-00516-5]
- Wu CH, Tu ST, Chang YF, Chan DC, Chien JT, Lin CH, et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: A systematic literature review and meta-analysis. Bone. 2018; 111:92-100. [DOI:10.1016/j.bone.2018.03.018]
- Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle S, Grauer A, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019; 30:79-92. [DOI:10.1007/s00198-018-4732-1]
- Ganda K, Schaffer A, Seibel MJ. Predictors of refracture amongst patients managed within a secondary fracture prevention program: A 7-year prospective study. Osteoporos Int. 2015; 26(2):543-51. [DOI:10.1007/s00198-014-2880-5]
- Ma X, Xia H, Wang J, Zhu X, Huang F, Lu L, et al. Refracture and correlated risk factors in patients with osteoporotic vertebral fractures. J Bone Miner Metab. 2019; 37:729. [DOI:10.1007/s00774-019-00999-w]
- Ganda K, Schaffer A, Pearson S, Seibel MJ. Compliance and persistence to oral bisphosphonate therapy following initiation within a secondary fracture prevention program: A randomised controlled trial of specialist vs. non-specialist management. Osteoporos Int. 2014; 25:1345-55. [DOI:10.1007/s00198-013-2610-4]
- Sambrook P, Kelly P, Eisman J. Bone mass and ageing. Baillières Clin Rheumatol. 1993; 7(3):445-57. [DOI:10.1016/S0950-3579(05)80072-X]
- Hansen L, Petersen KD, Eriksen SA, Langdahl BL, Eiken PA, Brixen K, et al. Subsequent fracture rates in a nationwide population-based cohort study with a 10-year perspective. Osteoporos Int. 2015; 26:513-9. [DOI:10.1007/s00198-014-2875-2]
- Riss P, Asari R, Scheuba C, Niederle B. Current trends in surgery for renal hyperparathyroidism (RHPT)-An international survey. Langenbecks Arch Surg. 2013; 398(1):121-30. [DOI:10.1007/s00423-012-1025-6]
Type of Study: Research Article |
Subject:
Rheumatology
Received: 2022/09/18 | Accepted: 2023/01/3 | Published: 2023/02/1
Received: 2022/09/18 | Accepted: 2023/01/3 | Published: 2023/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






