Volume 10, Issue 1 (2-2023)
JROS 2023, 10(1): 49-52 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najd Mazher F, Hasan A I, Ganbari A, Torab R. Tenosynovial Chondromatosis in Finger, Mimicking Neoplastic Lesion. JROS 2023; 10 (1) :49-52
URL: http://jros.iums.ac.ir/article-1-2234-en.html
URL: http://jros.iums.ac.ir/article-1-2234-en.html
1- Department of Orthopedic Surgery, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, School of Medicine, Bone and Joint Reconstruction Center, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, School of Medicine, Bone and Joint Reconstruction Center, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Tenosynovial chondromatosis, Soft tissue neoplasm, Proximal interphalangeal (PIP) joint, Osteochondromatosis, Finger, Hand, Bone
Full-Text [PDF 914 kb]
(203 Downloads)
| Abstract (HTML) (834 Views)
Full-Text: (180 Views)
Introduction
Primary synovial chondromatosis is characterized by the histological presence of hyaline cartilage nodules within the sub-synovial lining. It can occur within joints, known as articular synovial chondromatosis, or within tendon sheaths, referred to as tenosynovial chondromatosis (TC) [1]. Although intra-articular and extra-articular forms of synovial chondromatosis share similar histological features, they differ in surgical management and recurrence rates [2].
TC is a rare condition with a tendency for high recurrence and more commonly affects the flexor tendon sheaths than the extensor sheaths [3, 4].
This study presents a case of TC involving the finger tendon sheath in a 31-year-old man. He experienced pain upon pressure and restricted movement. Additionally, x-ray imaging revealed periosteal reaction and bone erosion.
Case Presentation
A 31-year-old male patient was admitted to the hand clinic with the complaint of painless and progressive swelling at the proximal interphalangeal (PIP) joint of the right index finger over the past 18 months. The patient denied any history of trauma or excessive use of the right hand. Physical examination of the finger showed a 1×1 cm irregularly shaped mass on the palm side of the index finger, near the PIP joint. The mass was firm in texture with well-defined borders. It was mildly painful under pressure. The interphalangeal joint of the right index finger exhibited a decreased range of motion, measuring 65 degrees. The patient’s blood biochemistry results were unremarkable.
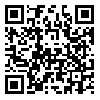
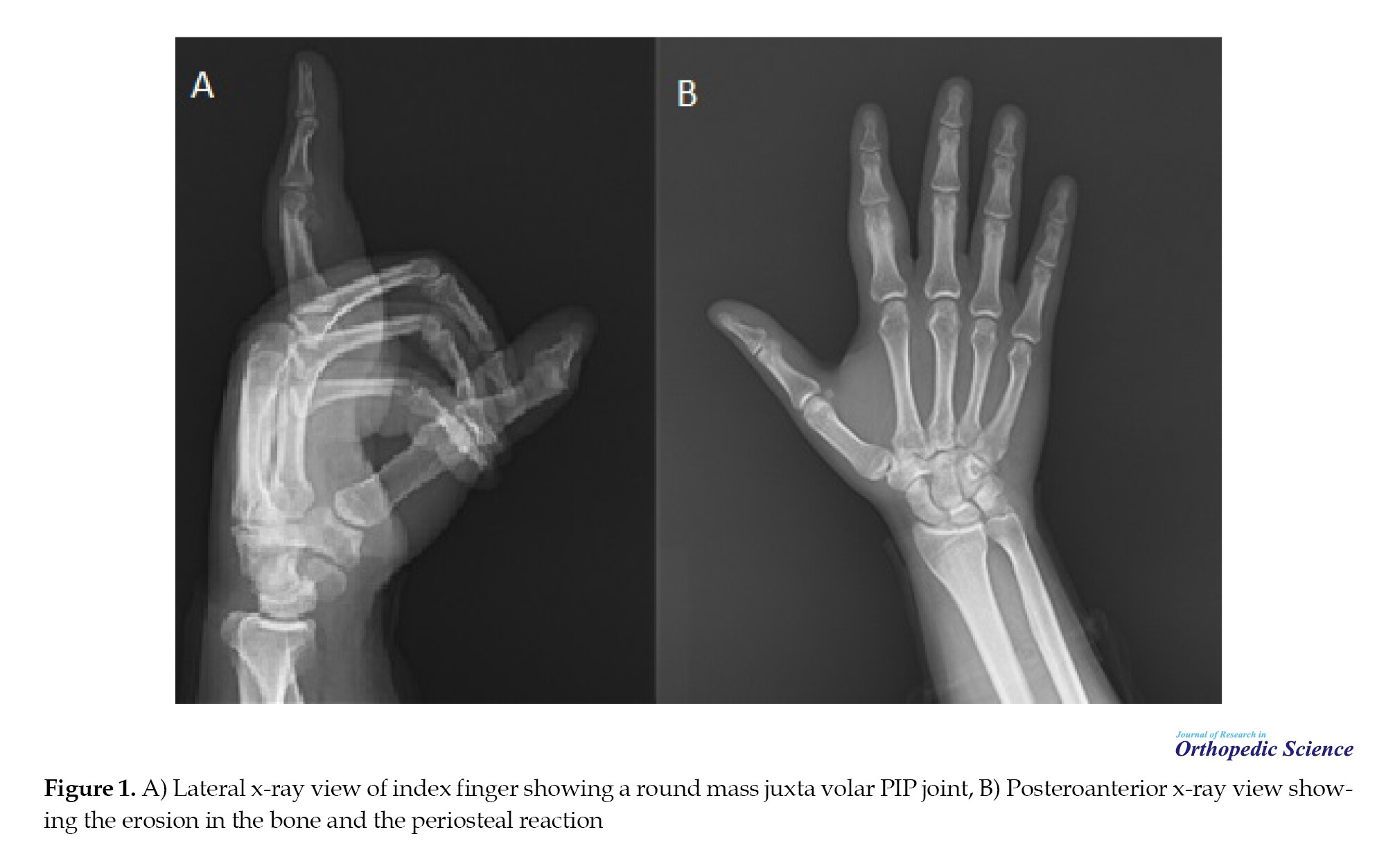
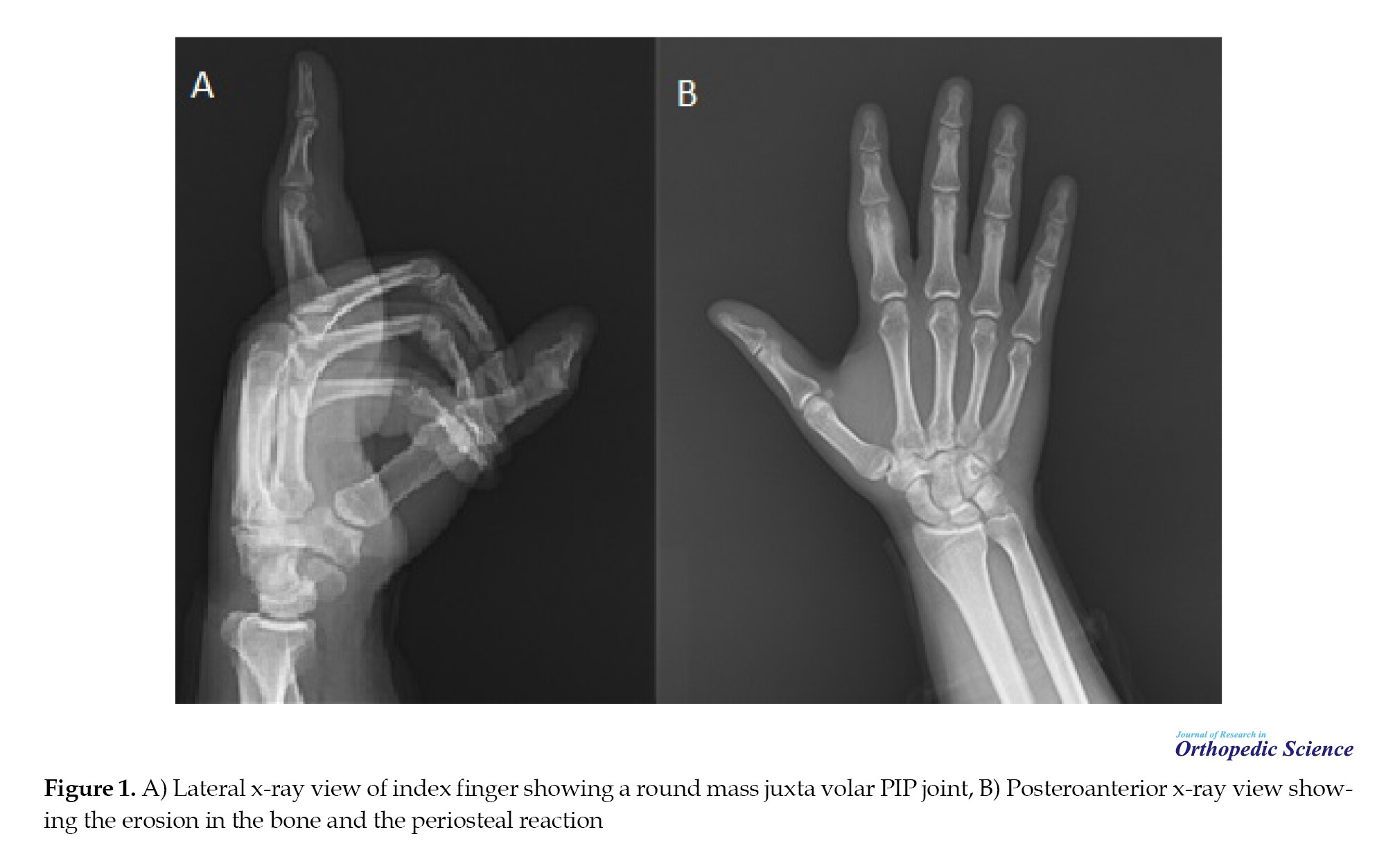
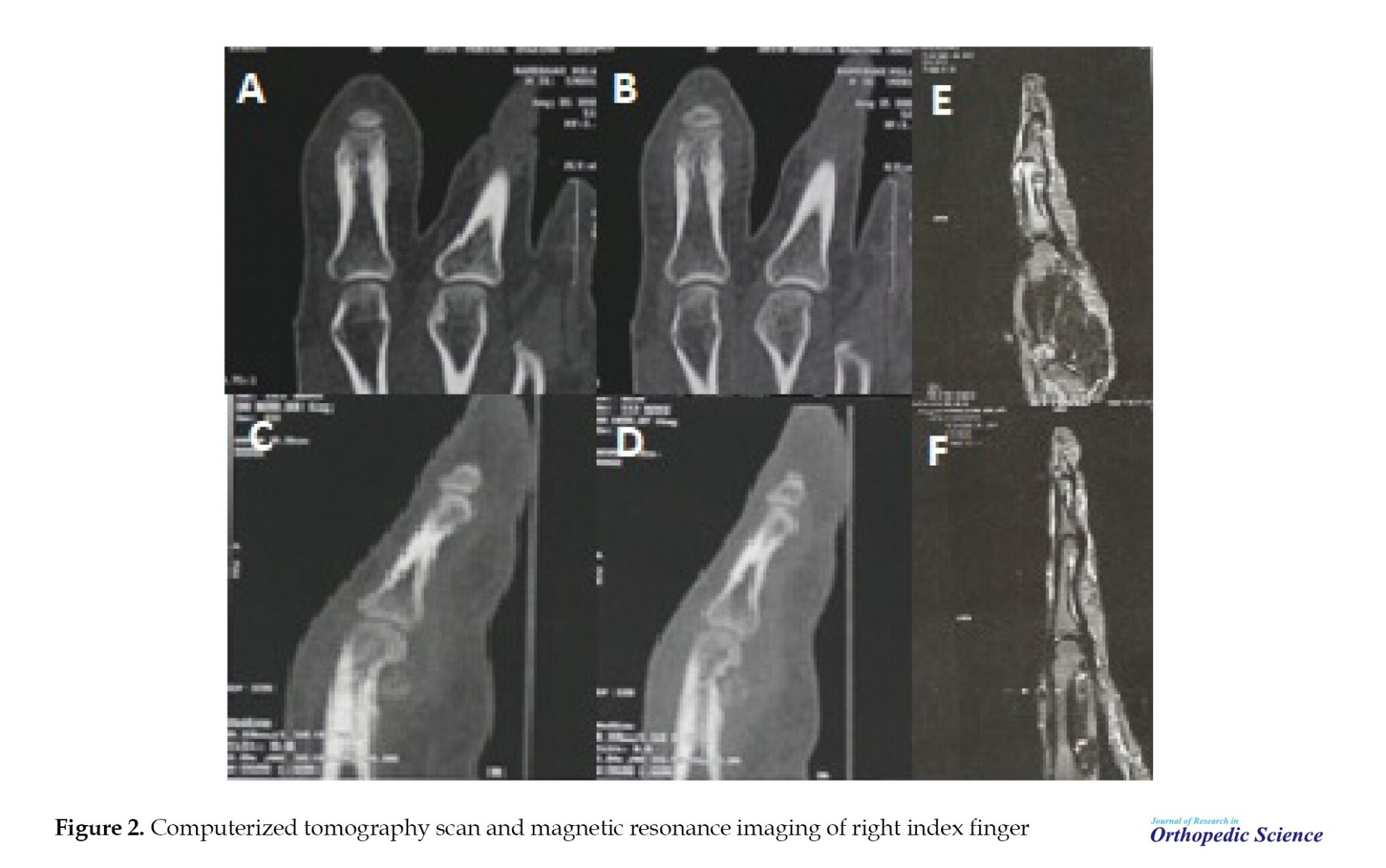
A thorough imaging evaluation, including x-ray and CT scan, revealed a well-defined, heterogeneous ossification that measures about 0.8 mm anteriorly to the palmar face of the distal part of the proximal phalanx adjacent to the joint without reaching the cartilage of the PIP joint. The tumor exhibited saucerization, remodeling the phalanx shape with a compressed intact cortex. Also, it caused thickening and a single layer of periosteal reaction surrounding the middle and distal parts of the proximal phalanx of the second digit (Figures 1 and 2).
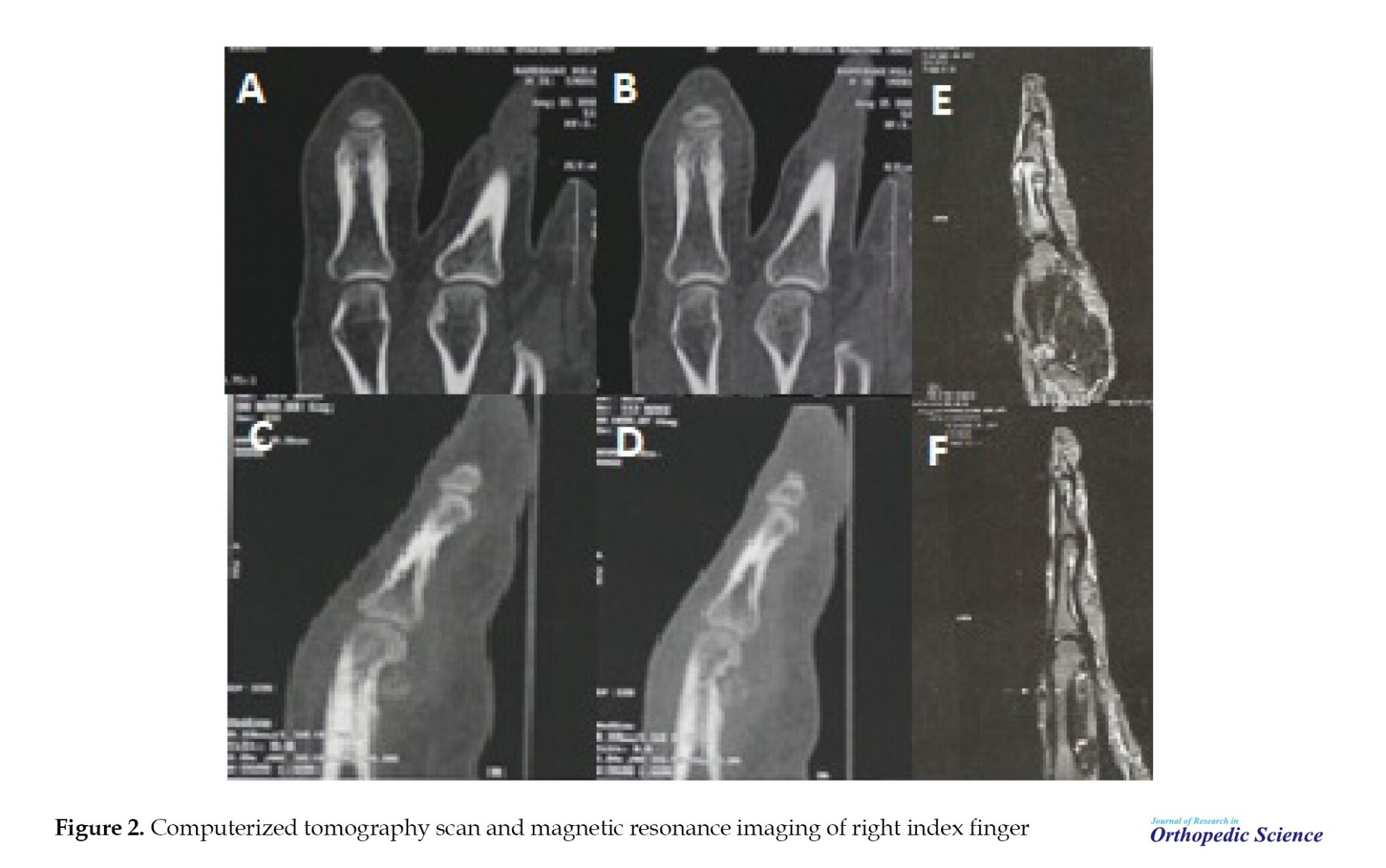
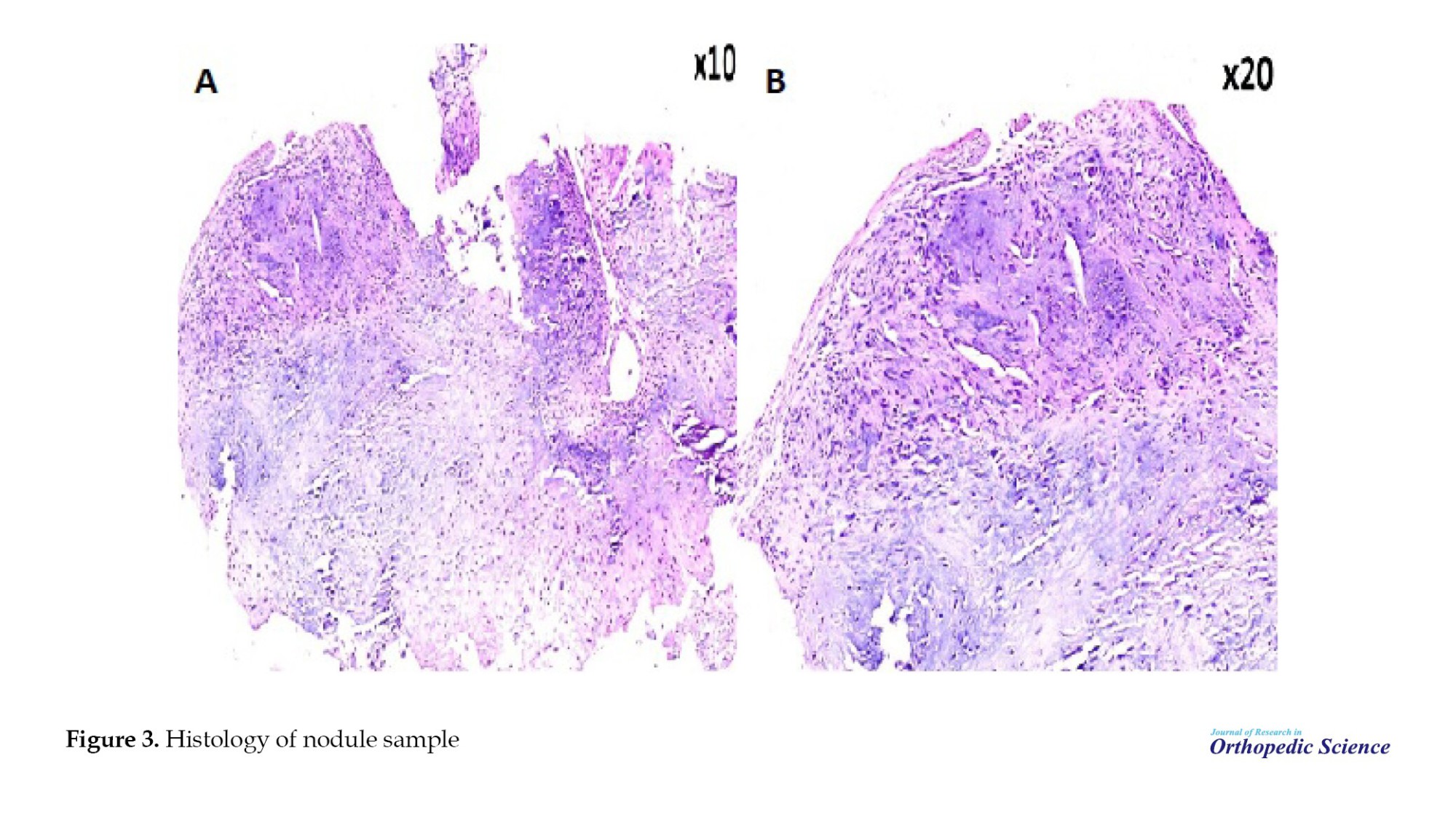
Surgical resection of the nodules was performed under general anesthesia. After preparing and draping the area, a tourniquet was applied at 280 mm Hg pressure. A Z-shaped Brunner zigzag incision was made on the palm side of the proximal phalanx of the right index finger to access the tendon sheath. Firm, smooth white nodules were identified beneath the flexor tendon. Histopathological analysis of these nodules showed elevated chondrocyte cellularity and a fibrous capsule, confirming the diagnosis of CT (Figure 3).
Six months postoperatively, the patient was symptom-free. There were no signs of recurrence at a subsequent follow-up, and the associated symptoms had significantly improved following the excision.
Discussion
Synovial chondromatosis is believed to result from metaplasia [5]. Extra-articular TC tends to affect the flexor surfaces of the fingers more often [5, 6]. In Murphey’s study, bone erosion was noted in 9 cases (43%), although no bone invasion or periosteal reaction was visible on radiographs. However, one case had a periosteal reaction in their foot CT scan [7]. In this case, there is a periosteal reaction and remodeling of the shape of the phalanx. Contrary to this, Fetsch et al. analyzed 37 cases and found that 50% of bone erosions were observed without any periosteal reaction [4].
According to Chen et al, aggressive behaviors evident in imaging, such as cortical erosion or periosteal reaction, may indicate chondrosarcoma with malignancy [2]. Although erosion and periosteal reaction were observed in our study, no evidence of histopathological malignancy was reported.
A conclusive diagnosis of chondrosarcoma is established through histological examination [8]. Fetsch identified several features that can help differentiate synovial-based chondrosarcoma from synovial chondromatosis, such as notable cytoarchitectural variation within tumors, pronounced myxoid alterations, high cellularity with crowding, spindle formation, marked nuclear atypia, and necrosis—all of which were absent in our study.
Cases of malignant transformation from synovial chondromatosis to chondrosarcoma have been documented, with one study showing an incidence rate of 2.5% (4 out of 155 cases) [9], primarily involving the hip joint and one case affecting the elbow joint. In this case, no recurrence of lesions was observed throughout the follow-up period.
According to this case report, we recommend a more comprehensive study with a larger sample size of TC cases to understand better the clinical presentation, radiological features, and recurrence patterns. This could improve diagnostic accuracy, optimal surgical strategies, and postoperative management protocols to mitigate recurrence rates and ensure better patient outcomes.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision: Farid Najd Mazhar; Data Collection: Ahmad Hassan; Writing: Alireza Ghanbari and Reza Torab.
Conflict of interest
The authors declared no conflict of interest.
References
Primary synovial chondromatosis is characterized by the histological presence of hyaline cartilage nodules within the sub-synovial lining. It can occur within joints, known as articular synovial chondromatosis, or within tendon sheaths, referred to as tenosynovial chondromatosis (TC) [1]. Although intra-articular and extra-articular forms of synovial chondromatosis share similar histological features, they differ in surgical management and recurrence rates [2].
TC is a rare condition with a tendency for high recurrence and more commonly affects the flexor tendon sheaths than the extensor sheaths [3, 4].
This study presents a case of TC involving the finger tendon sheath in a 31-year-old man. He experienced pain upon pressure and restricted movement. Additionally, x-ray imaging revealed periosteal reaction and bone erosion.
Case Presentation
A 31-year-old male patient was admitted to the hand clinic with the complaint of painless and progressive swelling at the proximal interphalangeal (PIP) joint of the right index finger over the past 18 months. The patient denied any history of trauma or excessive use of the right hand. Physical examination of the finger showed a 1×1 cm irregularly shaped mass on the palm side of the index finger, near the PIP joint. The mass was firm in texture with well-defined borders. It was mildly painful under pressure. The interphalangeal joint of the right index finger exhibited a decreased range of motion, measuring 65 degrees. The patient’s blood biochemistry results were unremarkable.
A thorough imaging evaluation, including x-ray and CT scan, revealed a well-defined, heterogeneous ossification that measures about 0.8 mm anteriorly to the palmar face of the distal part of the proximal phalanx adjacent to the joint without reaching the cartilage of the PIP joint. The tumor exhibited saucerization, remodeling the phalanx shape with a compressed intact cortex. Also, it caused thickening and a single layer of periosteal reaction surrounding the middle and distal parts of the proximal phalanx of the second digit (Figures 1 and 2).
Surgical resection of the nodules was performed under general anesthesia. After preparing and draping the area, a tourniquet was applied at 280 mm Hg pressure. A Z-shaped Brunner zigzag incision was made on the palm side of the proximal phalanx of the right index finger to access the tendon sheath. Firm, smooth white nodules were identified beneath the flexor tendon. Histopathological analysis of these nodules showed elevated chondrocyte cellularity and a fibrous capsule, confirming the diagnosis of CT (Figure 3).
Six months postoperatively, the patient was symptom-free. There were no signs of recurrence at a subsequent follow-up, and the associated symptoms had significantly improved following the excision.
Discussion
Synovial chondromatosis is believed to result from metaplasia [5]. Extra-articular TC tends to affect the flexor surfaces of the fingers more often [5, 6]. In Murphey’s study, bone erosion was noted in 9 cases (43%), although no bone invasion or periosteal reaction was visible on radiographs. However, one case had a periosteal reaction in their foot CT scan [7]. In this case, there is a periosteal reaction and remodeling of the shape of the phalanx. Contrary to this, Fetsch et al. analyzed 37 cases and found that 50% of bone erosions were observed without any periosteal reaction [4].
According to Chen et al, aggressive behaviors evident in imaging, such as cortical erosion or periosteal reaction, may indicate chondrosarcoma with malignancy [2]. Although erosion and periosteal reaction were observed in our study, no evidence of histopathological malignancy was reported.
A conclusive diagnosis of chondrosarcoma is established through histological examination [8]. Fetsch identified several features that can help differentiate synovial-based chondrosarcoma from synovial chondromatosis, such as notable cytoarchitectural variation within tumors, pronounced myxoid alterations, high cellularity with crowding, spindle formation, marked nuclear atypia, and necrosis—all of which were absent in our study.
Cases of malignant transformation from synovial chondromatosis to chondrosarcoma have been documented, with one study showing an incidence rate of 2.5% (4 out of 155 cases) [9], primarily involving the hip joint and one case affecting the elbow joint. In this case, no recurrence of lesions was observed throughout the follow-up period.
According to this case report, we recommend a more comprehensive study with a larger sample size of TC cases to understand better the clinical presentation, radiological features, and recurrence patterns. This could improve diagnostic accuracy, optimal surgical strategies, and postoperative management protocols to mitigate recurrence rates and ensure better patient outcomes.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Supervision: Farid Najd Mazhar; Data Collection: Ahmad Hassan; Writing: Alireza Ghanbari and Reza Torab.
Conflict of interest
The authors declared no conflict of interest.
References
- Qi-Huang S, Jacho FAL, David L, Weingarten E. Extra-articular tenosynovial chondromatosis of the right fifth digit in a 59-year-old man: A case report and literature review. J Radiol Case Rep. 2021; 15(8):8-17. [DOI:10.3941/jrcr.v15i8.4212] [PMID]
- Chen YX, Lu YX, Zhuang ZE, Li ZY. Extra-articular tenosynovial chondromatosis of the left ring finger in a 23-year-old man: A case report and literature review. Exp Ther Med. 2015; 10(4):1581-3. [DOI:10.3892/etm.2015.2687] [PMID] [PMCID]
- Walker EA, Murphey MD, Fetsch JF. Imaging characteristics of tenosynovial and bursal chondromatosis. Skeletal Radiol. 2011; 40(3):317-25. [DOI:10.1007/s00256-010-1012-3] [PMID]
- Fetsch JF, Vinh TN, Remotti F, Walker EA, Murphey MD, Sweet DE. Tenosynovial (extraarticular) chondromatosis: an analysis of 37 cases of an underrecognized clinicopathologic entity with a strong predilection for the hands and feet and a high local recurrence rate. Am J Surg Pathol. 2003; 27(9):1260-8. [DOI:10.1097/00000478-200309000-00010] [PMID]
- Wong SH, Salama S, Thoma A. Synovial chondromatosis of the hand: Three case reports and literature review. Can J Plast Surg. 2003; 11(1):47-52. [DOI:10.1177/229255030301100109] [PMID] [PMCID]
- Roulot E, Le Viet D. Primary synovial osteochondromatosis of the hand and wrist. Report of a series of 21 cases and literature review. Rev Rhum Engl Ed. 1999; 66(5):256-66. [PMID]
- Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics. 2007; 27(5):1465-88. [DOI:10.1148/rg.275075116] [PMID]
- Milgram JW. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg. 1977; 59(6):792-801. [DOI:10.2106/00004623-197759060-00013]
- McCarthy C, Anderson WJ, Vlychou M, Inagaki Y, Whitwell D, Gibbons CL, et al. Primary synovial chondromatosis: A reassessment of malignant potential in 155 cases. Skeletal Radiol. 2016; 45(6):755-62. [DOI:10.1007/s00256-016-2353-3] [PMID]
Type of Study: Case Report |
Subject:
Hand surgery / Elbow
Received: 2022/06/12 | Accepted: 2022/12/23 | Published: 2023/02/1
Received: 2022/06/12 | Accepted: 2022/12/23 | Published: 2023/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |