Volume 10, Issue 1 (2-2023)
JROS 2023, 10(1): 1-6 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Valiolahpour Amiri A, Sadat Kiaei S M, Athari M, Chehrassan M. Managing Unintentional Dural Tear in Spine Surgery: An Algorithmic Approach and Review of the Literature. JROS 2023; 10 (1) :1-6
URL: http://jros.iums.ac.ir/article-1-2235-en.html
URL: http://jros.iums.ac.ir/article-1-2235-en.html
1- Bone and Joint Reconstruction Research Center, Shafa Yahyaeian Orthopedic Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, Imam Hossein Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, Imam Hossein Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Incidental dural tear, Spine surgery, Complication management, Repair techniques, Algorithmic approach, Narrative review
Full-Text [PDF 550 kb]
(471 Downloads)
| Abstract (HTML) (1092 Views)
Full-Text: (437 Views)
Introduction
ncidental dural tear is one of the most critical complications in spine surgery that happens when dura matter tears and cerebrospinal fluid (CSF) leaks. Incidental dural tears occur more frequently in lumbar spine surgery compared to cervical or thoracic spine surgeries. This discrepancy may be attributed to dural manipulation or less careful laminectomy in the lumbar zone compared to other spine areas. Moreover, the higher rate of lumbar surgeries may justify the greater incidence of dural tears in the lumbar spine zone. Recent studies have shown an incidence of 1% for cervical surgeries, 7.6% for primary lumbar surgeries, and 15.9% for revision lumbar surgeries [1]. However, it is important to note that most dural tears are not reported because many patients with dural tears have no morbidities.
Dural tears may be identified either intraoperatively or postoperatively. Moreover, appropriate management of these dural tears depends on various factors, including the location of the lesion along the spinal zones and actual conditions. This complexity underscores the importance of a proper diagnosis and a thorough understanding of different treatment methods. To perform appropriate diagnosis and treatment for each scenario, an algorithmic approach based on recent evidence for managing dural tears may help the surgeon make better decisions and optimize patient outcomes.
During surgery vs after surgery (diagnosis, which one needs to be repaired)
Dural tears can happen during surgery. They are usually identified by CSF leakage or bleeding from epidural veins due to the loss of the expanded dural tamponade effect. However, if this event remains unrecognized during surgery, it can lead to complications such as CSF leak, fistula, wound dehiscence, infection, and rarely meningitis or even subdural hematoma [2-5].
After surgery, symptoms of low CSF pressure can indicate an unrecognized dural tear. The incidence of late-presenting dural tears (LPDT) was estimated to be 0.28% by Cammisa et al., and most cases remained asymptomatic [3]. Khazim et al. reported the incidence of LPDT 0.9% in primary cases and 0.5% in revision cases [6]. In a multicenter cohort study, Durand et al. found that the main risk factors for LPDT were lumbar spine procedures and decompression surgery [7].
Unrecognized dural tears or improper repair of dural tears may lead to complications such as fistulas and pseudomeningoceles. These complications can present with many symptoms and signs [8]. Most pseudomeningoceles are asymptomatic and can be detected on MRI [9]. Fistulas are tracts that communicate intra and extra-dural space. If they reach the skin, the presence of CSF can be determined with β2 transferrin [10].
Hershman et al. reported two cases of LPDT and suggested 24 hours of bed rest for patients. After this period, if the symptoms persist, they recommend using an epidural patch (EPB). If the patient does not improve, a second attempt for an epidural blood patch can be performed, and at last, surgery should be considered [11].
Classifications (size/repairability/zone)
There is currently no agreement about the classification of dural tears. While the tear size can categorize them, there is no consensus on this classification. Ointment et al. divided dural tears into three different groups: Pinhole tears, measuring <1 mm; medium-sized tears, defined as 1 mm to 1 cm; and large tears exceeding 1 cm [12].
In another study, Galarza et al. classified dural tears into three groups with guidelines for treatment [13]. Their classification is based on the amount of CSF leak, arachnoid involvement, and the presence of one clean or more than one border [13].
Furthermore, the location of dural tears can be dorsal, ventral, or along the nerve root [14], each requiring different management approaches.
Site of the lesion (cervical/thoracic/lumbar)
Dural tears can occur during cervical, thoracic, or lumbar procedures. Risk factors and management for each segment differ.
A dural tear in the thoracic spine is typically documented along with lumbar surgery. Limited data exists regarding thoracic surgeries independently. Ossification of the ligamentum flavum (OLF) is a disease that can cause myelopathy and is treated with surgery [15]. Hamouda et al. performed thoracic spine laminectomy in 18 cases. Among these cases, durotomy and CSF leakage were reported in 4 patients (22%) [16]. In another study by Sun et al., the incidence of dural tears and CSF leakage in thoracic OLF patients was 32%, and the main reasons were adhesion and ossification of dura [17].
The incidence of dural tears is lower in the cervical spine compared to the lumbar spine [18]. Risk factors for cervical dural tears have been extensively studied. Patient age, diagnosis of ossification of the posterior longitudinal ligament, anterior approach, OLF, revision surgery, surgeon’s experience, and synovial cyst have been associated with cervical dural tears [19-22].
Dural tears most frequently occur in the lumbar segment of the spine. Age, surgeon’s experience, revision surgery, and the number of decompressed levels have been noted as risk factors for lumbar dural tears [23, 24].
Repair or not
After encountering the dural tear during surgery, the first question is the repair method. For a long time, suturing was the only option for dural tears [3, 4, 25, 26]. However, some studies have utilized dural sealant [13, 27]. Bio adhesives alone may be used for small pinpoint tears, but for larger tears, repair with suture, with or without the addition of bioadhesive, is recommended [12, 27].
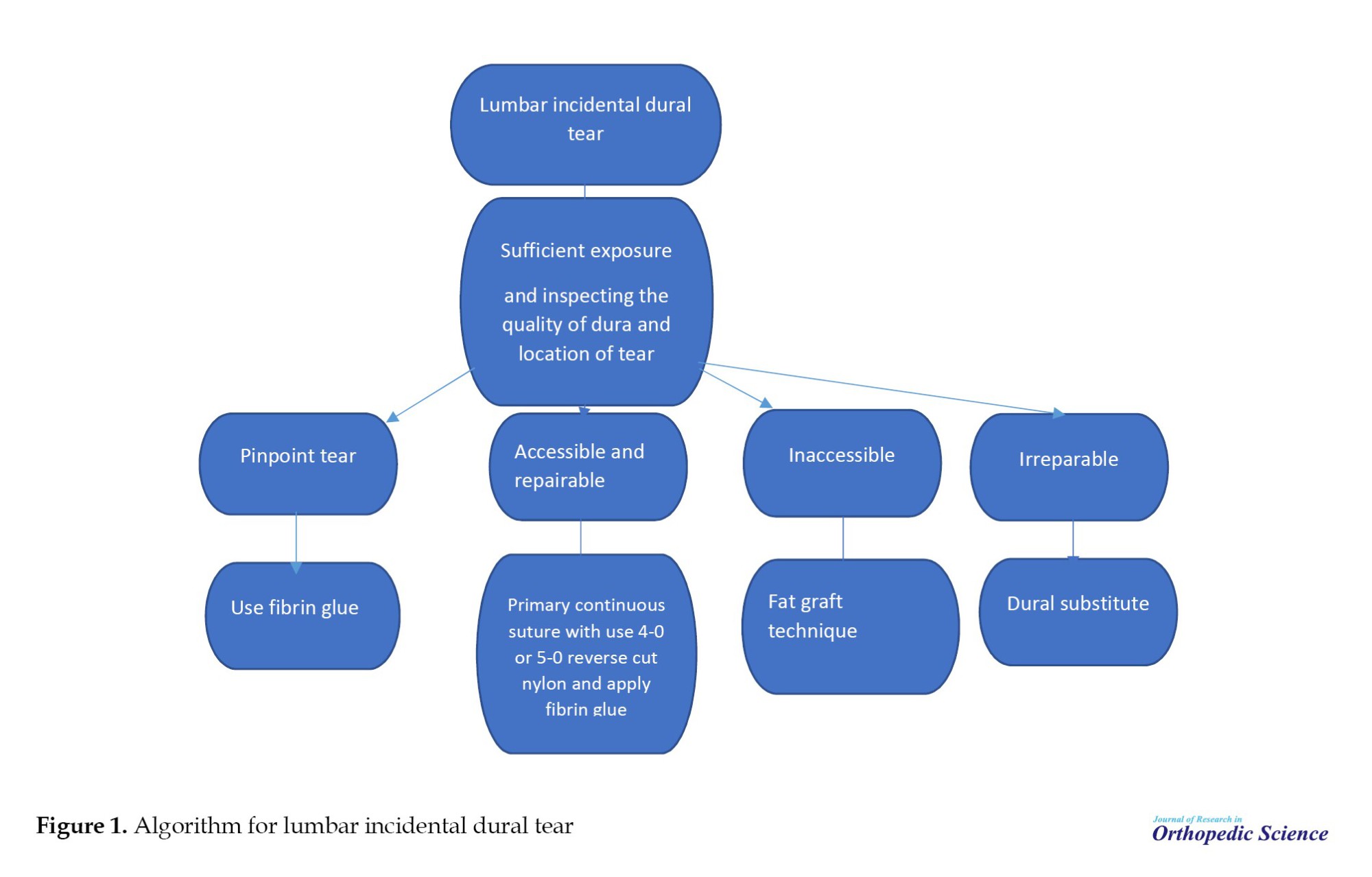
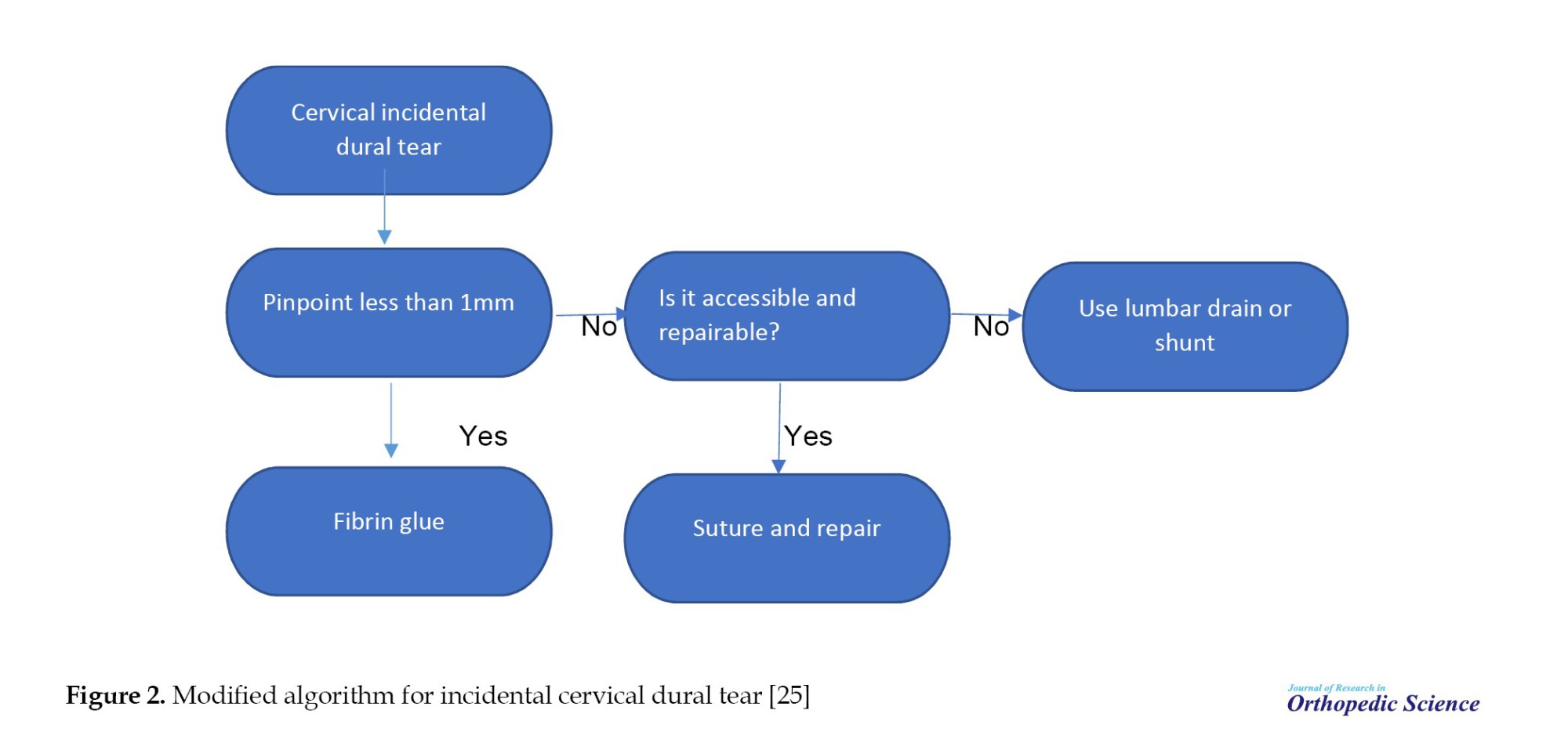
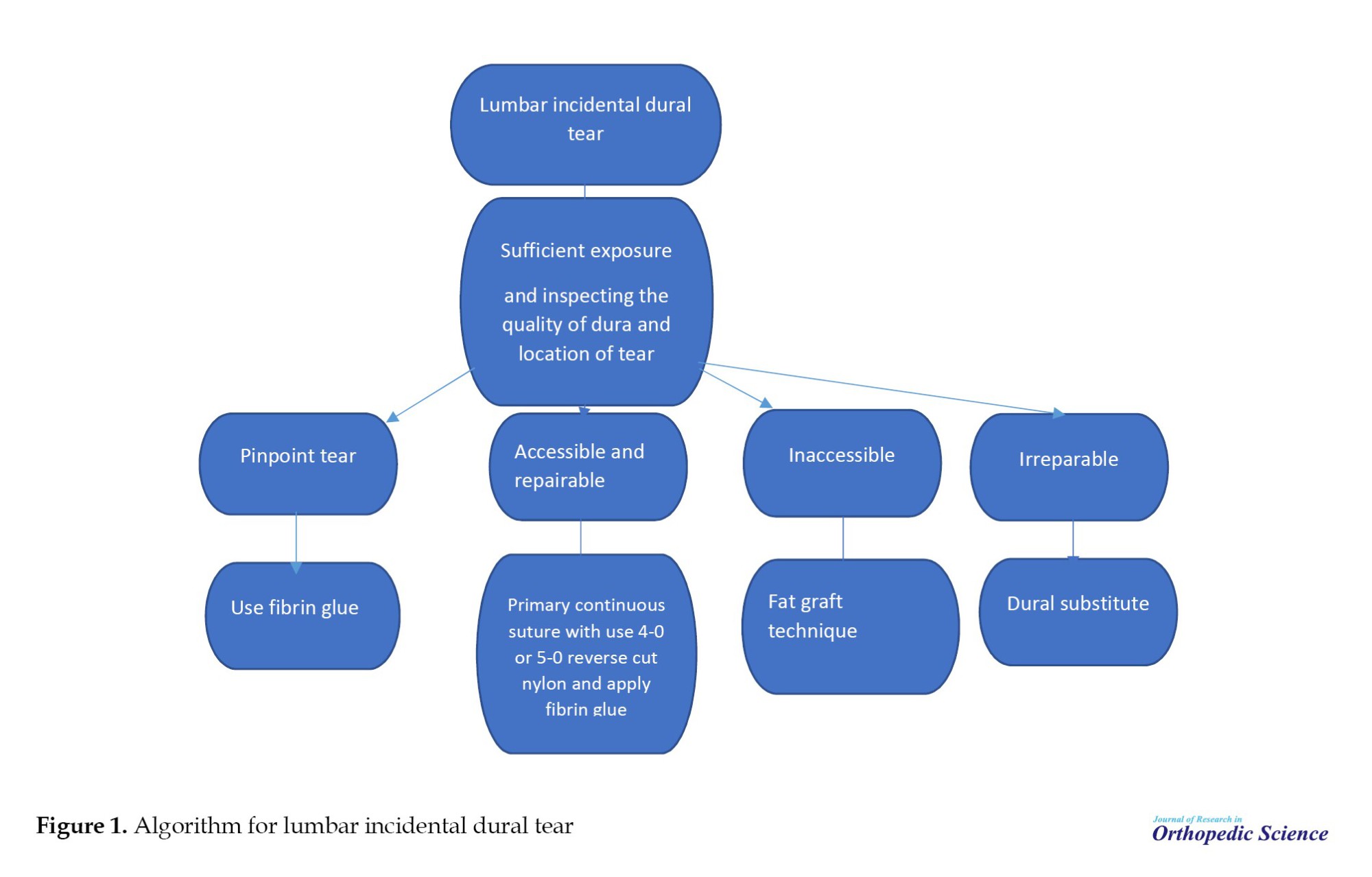
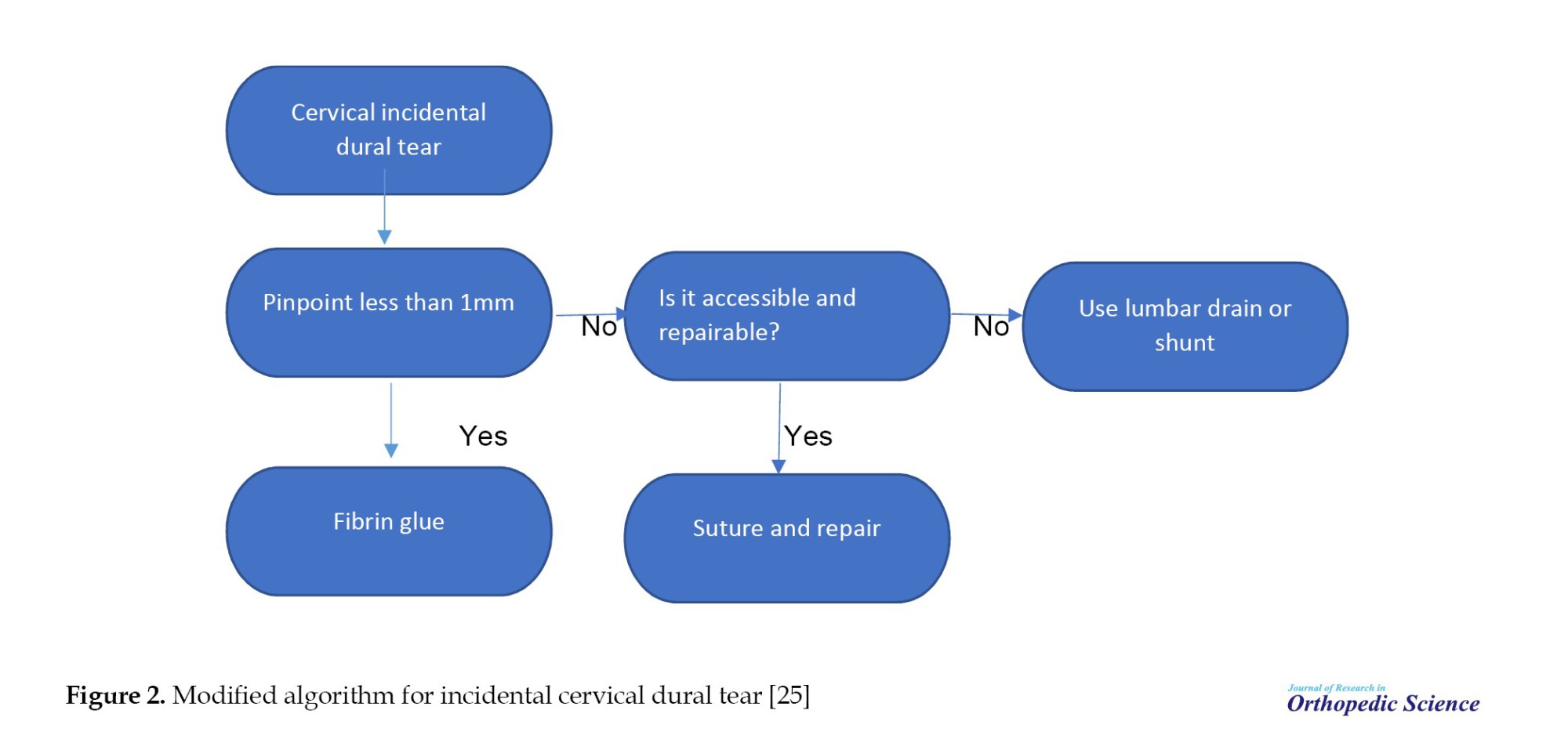
According to current studies, several methods have been employed for managing dural tears. However, there is still no consensus among spine surgeons on this matter. We have developed a new algorithm for managing dural tears based on various studies and our experience. Figures 1 and 2 depict the flowcharts for managing lumbar and cervical dural tears, respectively.
Method of repair (tight suture/non-tight suture/patch/muscle or Fat/glue or other materials)
There is no consensus regarding the material of suture and type of suturing. Some prefer continuous locking [25, 28, 29], while others prefer separate sutures [30]. Materials such as 7-0 Gore-Tex [30], 4-0 or 5-0 silk [25], and 4-0 nylon [1] have all been utilized. To our knowledge, no research compares methods and types of sutures.
After suturing, the Valsalva maneuver is employed to check the repair. If the repair is not watertight, it can be reinforced by a fat plug [31], a muscle patch [30], or a spinal sealant system [32].
Anterior and anterolateral wall tears of the dura cannot be easily sutured. In these cases, a technique described by Mayfield [31] and further developed by Black [14] involves using fat grafts covered with fibrin glue and then further with surgery or Gelfoam.
Drain
The insertion of a drainage tube is controversial following an incidental dural tear during surgery. Tosun et al. believed that lumbar drains proximal to the tear may reduce the hydrostatic pressure [33]. Conversely, Eismont et al. advised against the placement of drains [4]. Cammisa et al. recommended drains based on the type of surgery [3]. According to a questionnaire, Oitment found that most Canadian surgeons disagree with using drains [12].
Antibiotic
Antibiotic prophylaxis following a dural tear has not been addressed in the literature. Whether the prophylactic antibiotics administered before surgery should be continued postoperatively has not been studied extensively. Based on the French literature, Wolff et al. recommend continuing cefazolin for 48 hours postoperatively [34], while Guerin et al. advocated for continuing cefuroxime for 24 hours [35].
Dural tear and vertebral fracture
The incidence of dural tears in lumbar fractures has been reported to be up to 25% in lumbar burst fractures [36]. Luszczyk et al. demonstrated that the risk of dural tear was greater in the lumbar region compared to the thoracic and cervical regions [37]. Neurologic disorders and laminar fractures increase the incidence [38, 39].
Increasing interpedicular distance, the central canal diameter ratio, and the angle of the retropulsion segment can predict dural tears before surgery [40].
Repairing dural tears in vertebral fractures is similar to incidental dural tears, but they are more complex, and watertight closure is far less consistent [37]. Nerve roots may emerge through the tear and can become entrapped in the lamina and surrounding muscles [41].
Conclusion
Addressing incidental dural tears in spine surgery is complex and requires careful consideration of tear location, size, and repairability. The absence of consensus on classification and optimal repair methods underscores the need for standardized approaches and ongoing research. Utilizing an algorithmic approach informed by current literature, surgeons can optimize patient outcomes and mitigate the risks associated with this challenging complication. Continued research and collaboration within the medical community are essential for advancing treatment strategies and improving patient care in this complex clinical scenario.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mohammadreza Chehrassan; Methodology: Mirbahador Athari; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
ncidental dural tear is one of the most critical complications in spine surgery that happens when dura matter tears and cerebrospinal fluid (CSF) leaks. Incidental dural tears occur more frequently in lumbar spine surgery compared to cervical or thoracic spine surgeries. This discrepancy may be attributed to dural manipulation or less careful laminectomy in the lumbar zone compared to other spine areas. Moreover, the higher rate of lumbar surgeries may justify the greater incidence of dural tears in the lumbar spine zone. Recent studies have shown an incidence of 1% for cervical surgeries, 7.6% for primary lumbar surgeries, and 15.9% for revision lumbar surgeries [1]. However, it is important to note that most dural tears are not reported because many patients with dural tears have no morbidities.
Dural tears may be identified either intraoperatively or postoperatively. Moreover, appropriate management of these dural tears depends on various factors, including the location of the lesion along the spinal zones and actual conditions. This complexity underscores the importance of a proper diagnosis and a thorough understanding of different treatment methods. To perform appropriate diagnosis and treatment for each scenario, an algorithmic approach based on recent evidence for managing dural tears may help the surgeon make better decisions and optimize patient outcomes.
During surgery vs after surgery (diagnosis, which one needs to be repaired)
Dural tears can happen during surgery. They are usually identified by CSF leakage or bleeding from epidural veins due to the loss of the expanded dural tamponade effect. However, if this event remains unrecognized during surgery, it can lead to complications such as CSF leak, fistula, wound dehiscence, infection, and rarely meningitis or even subdural hematoma [2-5].
After surgery, symptoms of low CSF pressure can indicate an unrecognized dural tear. The incidence of late-presenting dural tears (LPDT) was estimated to be 0.28% by Cammisa et al., and most cases remained asymptomatic [3]. Khazim et al. reported the incidence of LPDT 0.9% in primary cases and 0.5% in revision cases [6]. In a multicenter cohort study, Durand et al. found that the main risk factors for LPDT were lumbar spine procedures and decompression surgery [7].
Unrecognized dural tears or improper repair of dural tears may lead to complications such as fistulas and pseudomeningoceles. These complications can present with many symptoms and signs [8]. Most pseudomeningoceles are asymptomatic and can be detected on MRI [9]. Fistulas are tracts that communicate intra and extra-dural space. If they reach the skin, the presence of CSF can be determined with β2 transferrin [10].
Hershman et al. reported two cases of LPDT and suggested 24 hours of bed rest for patients. After this period, if the symptoms persist, they recommend using an epidural patch (EPB). If the patient does not improve, a second attempt for an epidural blood patch can be performed, and at last, surgery should be considered [11].
Classifications (size/repairability/zone)
There is currently no agreement about the classification of dural tears. While the tear size can categorize them, there is no consensus on this classification. Ointment et al. divided dural tears into three different groups: Pinhole tears, measuring <1 mm; medium-sized tears, defined as 1 mm to 1 cm; and large tears exceeding 1 cm [12].
In another study, Galarza et al. classified dural tears into three groups with guidelines for treatment [13]. Their classification is based on the amount of CSF leak, arachnoid involvement, and the presence of one clean or more than one border [13].
Furthermore, the location of dural tears can be dorsal, ventral, or along the nerve root [14], each requiring different management approaches.
Site of the lesion (cervical/thoracic/lumbar)
Dural tears can occur during cervical, thoracic, or lumbar procedures. Risk factors and management for each segment differ.
A dural tear in the thoracic spine is typically documented along with lumbar surgery. Limited data exists regarding thoracic surgeries independently. Ossification of the ligamentum flavum (OLF) is a disease that can cause myelopathy and is treated with surgery [15]. Hamouda et al. performed thoracic spine laminectomy in 18 cases. Among these cases, durotomy and CSF leakage were reported in 4 patients (22%) [16]. In another study by Sun et al., the incidence of dural tears and CSF leakage in thoracic OLF patients was 32%, and the main reasons were adhesion and ossification of dura [17].
The incidence of dural tears is lower in the cervical spine compared to the lumbar spine [18]. Risk factors for cervical dural tears have been extensively studied. Patient age, diagnosis of ossification of the posterior longitudinal ligament, anterior approach, OLF, revision surgery, surgeon’s experience, and synovial cyst have been associated with cervical dural tears [19-22].
Dural tears most frequently occur in the lumbar segment of the spine. Age, surgeon’s experience, revision surgery, and the number of decompressed levels have been noted as risk factors for lumbar dural tears [23, 24].
Repair or not
After encountering the dural tear during surgery, the first question is the repair method. For a long time, suturing was the only option for dural tears [3, 4, 25, 26]. However, some studies have utilized dural sealant [13, 27]. Bio adhesives alone may be used for small pinpoint tears, but for larger tears, repair with suture, with or without the addition of bioadhesive, is recommended [12, 27].
According to current studies, several methods have been employed for managing dural tears. However, there is still no consensus among spine surgeons on this matter. We have developed a new algorithm for managing dural tears based on various studies and our experience. Figures 1 and 2 depict the flowcharts for managing lumbar and cervical dural tears, respectively.
Method of repair (tight suture/non-tight suture/patch/muscle or Fat/glue or other materials)
There is no consensus regarding the material of suture and type of suturing. Some prefer continuous locking [25, 28, 29], while others prefer separate sutures [30]. Materials such as 7-0 Gore-Tex [30], 4-0 or 5-0 silk [25], and 4-0 nylon [1] have all been utilized. To our knowledge, no research compares methods and types of sutures.
After suturing, the Valsalva maneuver is employed to check the repair. If the repair is not watertight, it can be reinforced by a fat plug [31], a muscle patch [30], or a spinal sealant system [32].
Anterior and anterolateral wall tears of the dura cannot be easily sutured. In these cases, a technique described by Mayfield [31] and further developed by Black [14] involves using fat grafts covered with fibrin glue and then further with surgery or Gelfoam.
Drain
The insertion of a drainage tube is controversial following an incidental dural tear during surgery. Tosun et al. believed that lumbar drains proximal to the tear may reduce the hydrostatic pressure [33]. Conversely, Eismont et al. advised against the placement of drains [4]. Cammisa et al. recommended drains based on the type of surgery [3]. According to a questionnaire, Oitment found that most Canadian surgeons disagree with using drains [12].
Antibiotic
Antibiotic prophylaxis following a dural tear has not been addressed in the literature. Whether the prophylactic antibiotics administered before surgery should be continued postoperatively has not been studied extensively. Based on the French literature, Wolff et al. recommend continuing cefazolin for 48 hours postoperatively [34], while Guerin et al. advocated for continuing cefuroxime for 24 hours [35].
Dural tear and vertebral fracture
The incidence of dural tears in lumbar fractures has been reported to be up to 25% in lumbar burst fractures [36]. Luszczyk et al. demonstrated that the risk of dural tear was greater in the lumbar region compared to the thoracic and cervical regions [37]. Neurologic disorders and laminar fractures increase the incidence [38, 39].
Increasing interpedicular distance, the central canal diameter ratio, and the angle of the retropulsion segment can predict dural tears before surgery [40].
Repairing dural tears in vertebral fractures is similar to incidental dural tears, but they are more complex, and watertight closure is far less consistent [37]. Nerve roots may emerge through the tear and can become entrapped in the lamina and surrounding muscles [41].
Conclusion
Addressing incidental dural tears in spine surgery is complex and requires careful consideration of tear location, size, and repairability. The absence of consensus on classification and optimal repair methods underscores the need for standardized approaches and ongoing research. Utilizing an algorithmic approach informed by current literature, surgeons can optimize patient outcomes and mitigate the risks associated with this challenging complication. Continued research and collaboration within the medical community are essential for advancing treatment strategies and improving patient care in this complex clinical scenario.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and supervision: Mohammadreza Chehrassan; Methodology: Mirbahador Athari; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Khan MH, Rihn J, Steele G, Davis R, Donaldson III WF, Kang JD, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: A review of 3,183 consecutive degenerative lumbar cases. Spine. 2006; 31(22):2609-13. [DOI:10.1097/01.brs.0000241066.55849.41]
- Sciubba DM, Kretzer RM, Wang PP. Acute intracranial subdural hematoma following a lumbar CSF leak caused by spine surgery. Spine. 2005; 30(24):E730-E2. [DOI:10.1097/01.brs.0000192208.66360.29]
- Cammisa Jr FP, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine. 2000; 25(20):2663-7. [DOI:10.1097/00007632-200010150-00019]
- Eismont FJ, Wiesel SW, Rothman RH. Treatment of dural tears associated with spinal surgery. J Bone Joint Surg Am. 1981;63(7):1132-6. [DOI:10.2106/00004623-198163070-00010]
- Goodkin R, Laska LL. Unintended “incidental” durotomy during surgery of the lumbar spine: Medicolegal implications. Surg Neurol. 1995; 43(1):4-14. [DOI:10.1016/0090-3019(95)80031-B]
- Khazim R, Dannawi Z, Spacey K, Khazim M, Lennon S, Reda A, et al. Incidence and treatment of delayed symptoms of CSF leak following lumbar spinal surgery. Eur Spine J. 2015; 24(9):2069-76. [DOI:10.1007/s00586-015-3830-4]
- Durand WM, DePasse JM, Kuris EO, Yang J, Daniels AH. Late-presenting dural tear: Incidence, risk factors, and associated complications. Spine J. 2018; 18(11):2043-50. [DOI:10.1016/j.spinee.2018.04.004]
- Hawk MW, Kim KD. Review of spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2000; 9(1):1-8. [DOI:10.3171/foc.2000.9.1.5]
- Murayama S, Numaguchi Y, Whitecloud TS, Brent CR. Magnetic resonance imaging of post-surgical pseudomeningocele. Comput Med Imaging Graph. 1989; 13(4):335-9. [DOI:10.1016/0895-6111(89)90211-5]
- Ryali RG, Peacock MK, Simpson DA. Usefulness of β2-transferrin assay in the detection of cerebrospinal fluid leaks following head injury. J Neurosurg. 1992; 77(5):737-9. [DOI:10.3171/jns.1992.77.5.0737]
- Hershman S, Cuellar VG, Bendo JA. Delayed presentation of incidental durotomy. Bull Hosp Jt Dis. 2013;71(3):231-4. [PMID]
- Oitment C, Aref M, Almenawar S, Reddy K. Spinal dural repair: A Canadian questionnaire. Glob Spine J. 2018; 8(4):359-64. [DOI:10.1177/2192568217724132]
- Galarza M, Gazzeri R, Alfaro R, De la Rosa P, Arraez C, Piqueras C. Evaluation and management of small dural tears in primary lumbar spinal decompression and discectomy surgery. J Clin Neurosci. 2018; 50:177-82. [DOI:10.1016/j.jocn.2018.01.008]
- Black P. Cerebrospinal fluid leaks following spinal or posterior fossa surgery: Use of fat grafts for prevention and repair. Neurosurg Focus. 2000; 9(1):1-4. [DOI:10.3171/foc.2000.9.1.4]
- Yonenobu K, Ebara S, Fujiwara K, Yamashita K, Ono K, Yamamoto T, et al. Thoracic myelopathy secondary to ossification of the spinal ligament. J Neurosurg. 1987; 66(4):511-8. [DOI:10.3171/jns.1987.66.4.0511]
- Hamouda KB, Jemel H, Haouet S, Khaldi M. Thoracic myelopathy caused by ossification of the ligamentum flavum: A report of 18 cases. Spine. 2003; 99(2):157-61. [DOI:10.3171/spi.2003.99.2.0157]
- Sun X, Sun C, Liu X, Liu Z, Qi Q, Guo Z, et al. The frequency and treatment of dural tears and cerebrospinal fluid leakage in 266 patients with thoracic myelopathy caused by ossification of the ligamentum flavum. Spine. 2012; 37(12):E702-7. [DOI:10.1097/BRS.0b013e31824586a8]
- Yoshihara H, Yoneoka D. Incidental dural tear in spine surgery: Analysis of a nationwide database. Eur Spine. 2014; 23(2):389-94. [DOI:10.1007/s00586-013-3091-z]
- Hannallah D, Lee J, Khan M, Donaldson WF, Kang JD. Cerebrospinal fluid leaks following cervical spine surgery. J Bone Joint Surg. 2008; 90(5):1101-5. [DOI:10.2106/JBJS.F.01114]
- Williams BJ, Sansur CA, Smith JS, Berven SH, Broadstone PA, Choma TJ, et al. Incidence of unintended durotomy in spine surgery based on 108 478 cases. Neurosurg. 2011; 68(1):117-24. [DOI:10.1227/NEU.0b013e3181fcf14e]
- Baker GA, Cizik AM, Bransford RJ, Bellabarba C, Konodi MA, Chapman JR, et al. Risk factors for unintended durotomy during spine surgery: A multivariate analysis. Spine. 2012; 12(2):121-6. [DOI:10.1016/j.spinee.2012.01.012]
- Epstein NE. The frequency and etiology of intraoperative dural tears in 110 predominantly geriatric patients undergoing multilevel laminectomy with noninstrumented fusions. Clin Spine Surg. 2007; 20(5):380-6. [DOI:10.1097/BSD.0b013e31802dabd2]
- Smorgick Y, Baker KC, Herkowitz H, Montgomery D, Badve SA, Bachison C, et al. Predisposing factors for dural tear in patients undergoing lumbar spine surgery. Spine. 2015; 22(5):483-6. [DOI:10.3171/2015.1.SPINE13864]
- Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. Spine. 2006; 5(3):224-7. [DOI:10.3171/spi.2006.5.3.224]
- Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine. Management and results after a two-year-minimum follow-up of eighty-eight patients. J Bone Joint Surg. 1998; 80(12):1728-32. [DOI:10.2106/00004623-199812000-00002]
- Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest: A retrospective review of 20 cases. Spine. 1999; 24(19):2062. [DOI:10.1097/00007632-199910010-00017]
- Kamenova M, Leu S, Mariani L, Schaeren S, Soleman J. Management of incidental dural tear during lumbar spine surgery. To suture or not to suture? World Neurosurg. 2016; 87:455-62. [DOI:10.1016/j.wneu.2015.11.045]
- Espiritu MT, Rhyne A, Darden BV. Dural tears in spine surgery. J Am Acad Orthop Surg. 2010; 18(9):537-45. [DOI:10.5435/00124635-201009000-00005]
- Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: A review. Clin Orthop Relat Res. 2001; 389:238-47. [DOI:10.1097/00003086-200108000-00033]
- Epstein NE. A review article on the diagnosis and treatment of cerebrospinal fluid fistulas and dural tears occurring during spinal surgery. Surg Neurol Int. 2013; 4(Suppl 5):S301. [DOI:10.4103/2152-7806.111427] [PMID]
- Mayfield FH, Kurokawa K. Watertight closure of spinal dura mater. J Neurosurg. 1975; 43(5):639-40. [DOI:10.3171/jns.1975.43.5.0639]
- Wright NM, Park J, Tew JM, Kim KD, Shaffrey ME, Cheng J, et al. Spinal sealant system provides better intraoperative watertight closure than standard of care during spinal surgery: A prospective, multicenter, randomized controlled study. Spine. 2015; 40(8):505-13. [DOI:10.1097/BRS.0000000000000810]
- Tosun B, Ilbay K, Kim MSM, Selek O. Management of persistent cerebrospinal fluid leakage following thoraco-lumbar surgery. Asian Spine J. 2012; 6(3):157. [DOI:10.4184/asj.2012.6.3.157]
- Wolff S, Kheirredine W, Riouallon G. Surgical dural tears: prevalence and updated management protocol based on 1359 lumbar vertebra interventions. Orthop Traumatol. 2012; 98(8):879-86. [DOI:10.1016/j.otsr.2012.06.016]
- Guerin P, El Fegoun AB, Obeid I, Gille O, Lelong L, Luc S, et al. Incidental durotomy during spine surgery: Incidence, management and complications. A retrospective review. Injury. 2012; 43(4):397-401. [DOI:10.1016/j.injury.2010.12.014]
- Aydnl U, Karaeminogullar O, Tiskaya K, Öztürk Ç. Dural tears in lumbar burst fractures with greenstick lamina fractures. Spine. 2001; 26(18):E410-5. [DOI:10.1097/00007632-200109150-00012]
- Luszczyk MJ, Blaisdell GY, Wiater BP, Bellabarba C, Chapman JR, Agel JA, et al. Traumatic dural tears: What do we know and are they a problem? Spine J. 2014; 14(1):49-56. [DOI:10.1016/j.spinee.2013.03.049]
- Cammisa F, Eismont F, Green B. Dural laceration occurring with burst fractures and associated laminar. J Bone Joint Surg Am. 1989; 71:1044-52. [DOI:10.2106/00004623-198971070-00011]
- Kahamba J, Rath S, Antoniadis G, Schneider O, Neff U, Richter H. Laminar and arch fractures with dural tear and nerve root entrapment in patients operated upon for thoracic and lumbar spine injuries. Acta Neurochir. 1998; 140(2):114-9. [DOI:10.1007/s007010050071]
- Lee I, Kim H, Lee J, Kim S-J, Jeong Y, Kim D, et al. Dural tears in spinal burst fractures: predictable MR imaging findings. Am J Neuroradiol. 2009; 30(1):142-6. [DOI:10.3174/ajnr.A1273]
- Kareem H, Raza MH, Kontojannis V, Nimer A, Tsang K. Case series of posterior instrumentation for repair of burst lumbar vertebral body fractures with entrapped neural elements. J Spine Surg. 2018; 4(2):374. [DOI:10.21037/jss.2018.06.03]
Type of Study: Review Paper |
Subject:
Spine surgery
Received: 2024/04/6 | Accepted: 2024/04/6 | Published: 2023/03/10
Received: 2024/04/6 | Accepted: 2024/04/6 | Published: 2023/03/10
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |