Volume 10, Issue 4 (11-2023)
JROS 2023, 10(4): 237-244 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hajialiloo Sami S, Kargar Shooroki K, Rikhtehgar M, Emtiazi N, Torab R. Local Recurrence Long Bones Hemangiomas in Ulna. JROS 2023; 10 (4) :237-244
URL: http://jros.iums.ac.ir/article-1-2240-en.html
URL: http://jros.iums.ac.ir/article-1-2240-en.html
1- Bone and Joint Reconstruction Research Center, Shafayahyaian Hospital, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 3065 kb]
(197 Downloads)
| Abstract (HTML) (783 Views)
Full-Text: (198 Views)
Introduction
Primary intraosseous hemangiomas (IHs), also recognized as hemangiomas of the bone, are non-malignant neoplasms composed of small and large vessels that develop within the bone [1]. Bone hemangiomas are infrequent intra-bony growths originating from mesenchymal cells, accounting for approximately 0.5% to 1% of all intraosseous tumors and 1% of all primary bone tumors. These IHs manifest as four distinct variants: Capillary, cavernous, mixed, and scirrhous [2]. Osseous hemangioma constitutes 1% of all primary skeletal neoplasms, predominantly located in the vertebra or skull (approximately 75%) and the clavicle, scapula, ribs, and pelvic bones (15%-20%) [3, 4].
Typically, solitary, osseous hemangiomas may also manifest as multiple lesions, characterized by thin-walled vessels or sinuses filled with blood dispersed amidst longitudinally oriented bony trabeculae, with potential secondary accumulation of lipid materials [5]. Although the lesion is often asymptomatic, it can lead to symptoms, such as hematoma formation, epidural invasion, vertebral body expansion, and pathological fractures [6]. This neoplasm, which predominantly affects the vertebrae and craniofacial bones, rarely involves the long tubular bones of the four extremities [7]. We report the case of a 35-year-old woman with an IH of the right proximal ulna. X-ray and magnetic resonance imaging showed a well-defined osteolytic lesion. The patient had a history of curettage surgery for a bone hemangioma.
Case Presentation
A 35-year-old woman was referred to our hospital complaining of right forearm pain persisting for two months. Despite conservative treatment involving the administration of analgesics and non-steroidal anti-inflammatory drugs, the pain persisted.
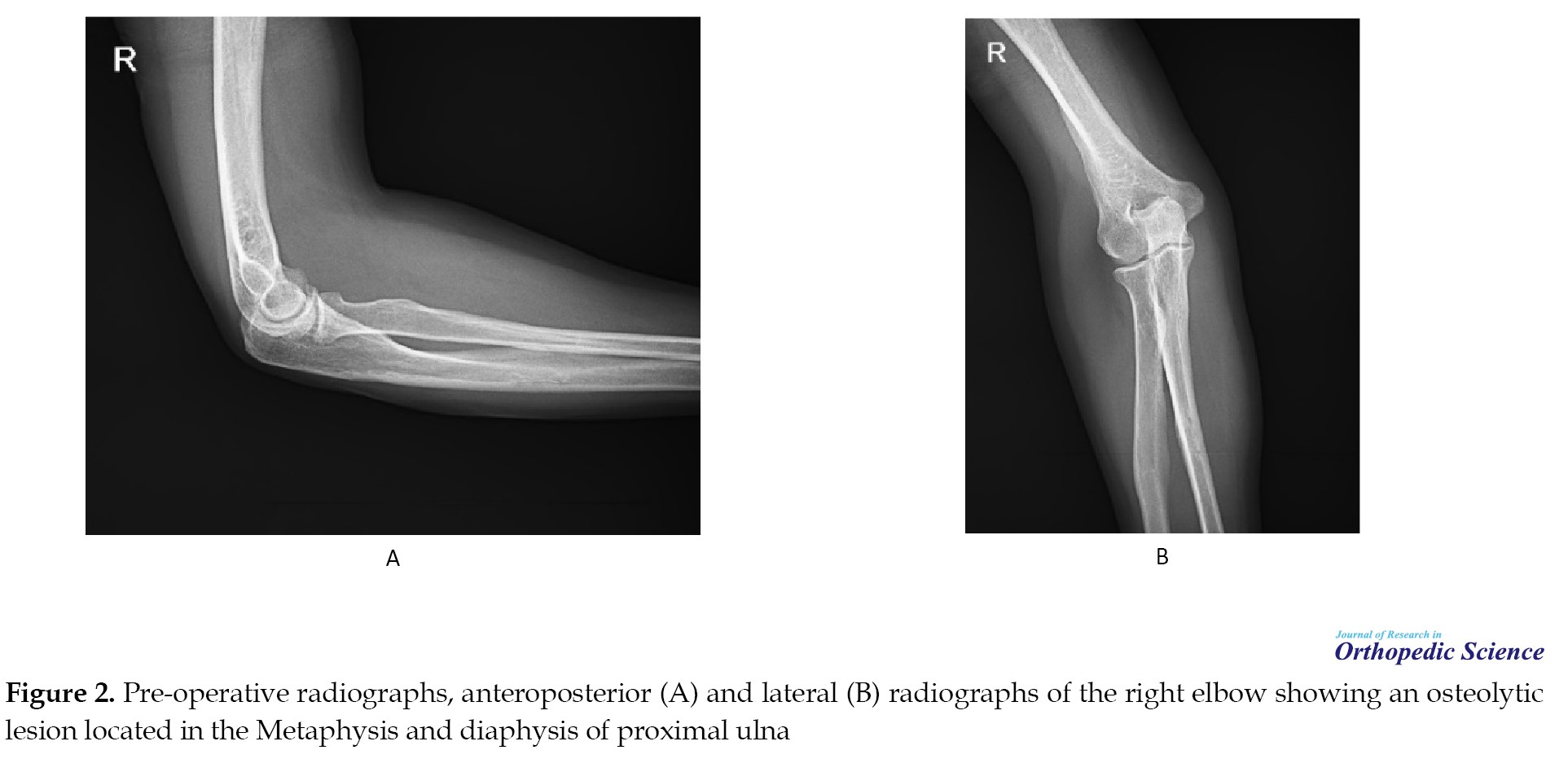
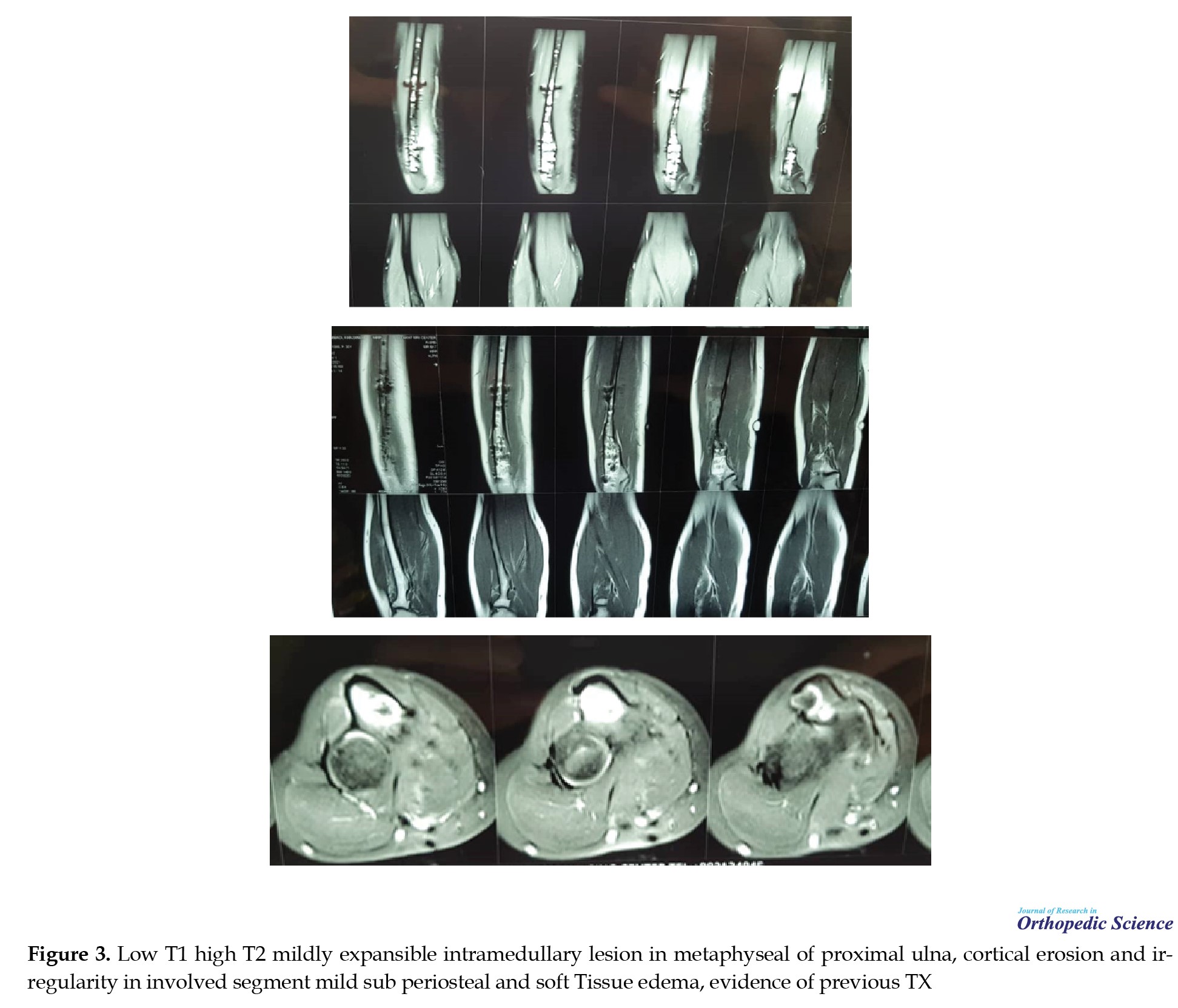
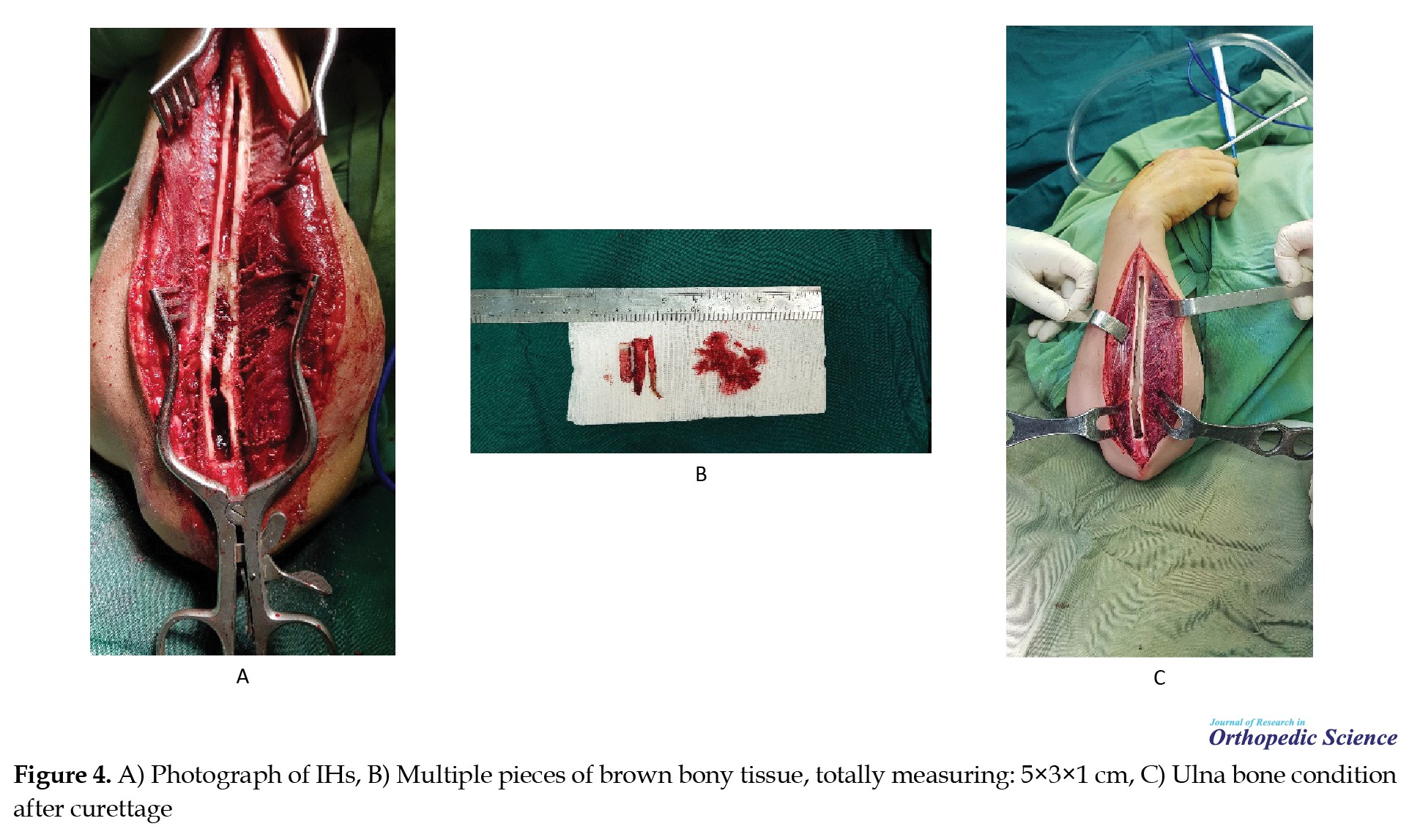
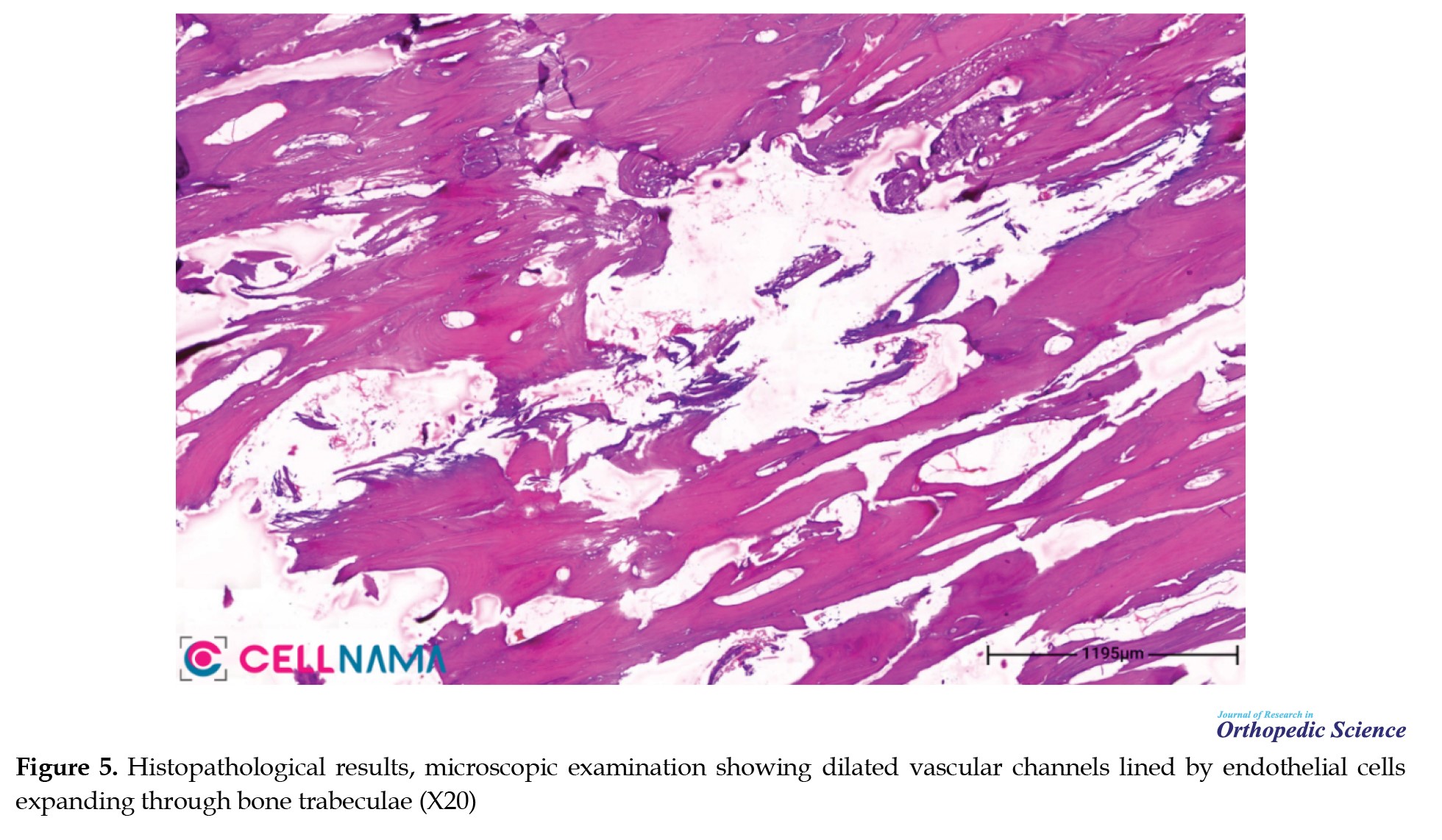
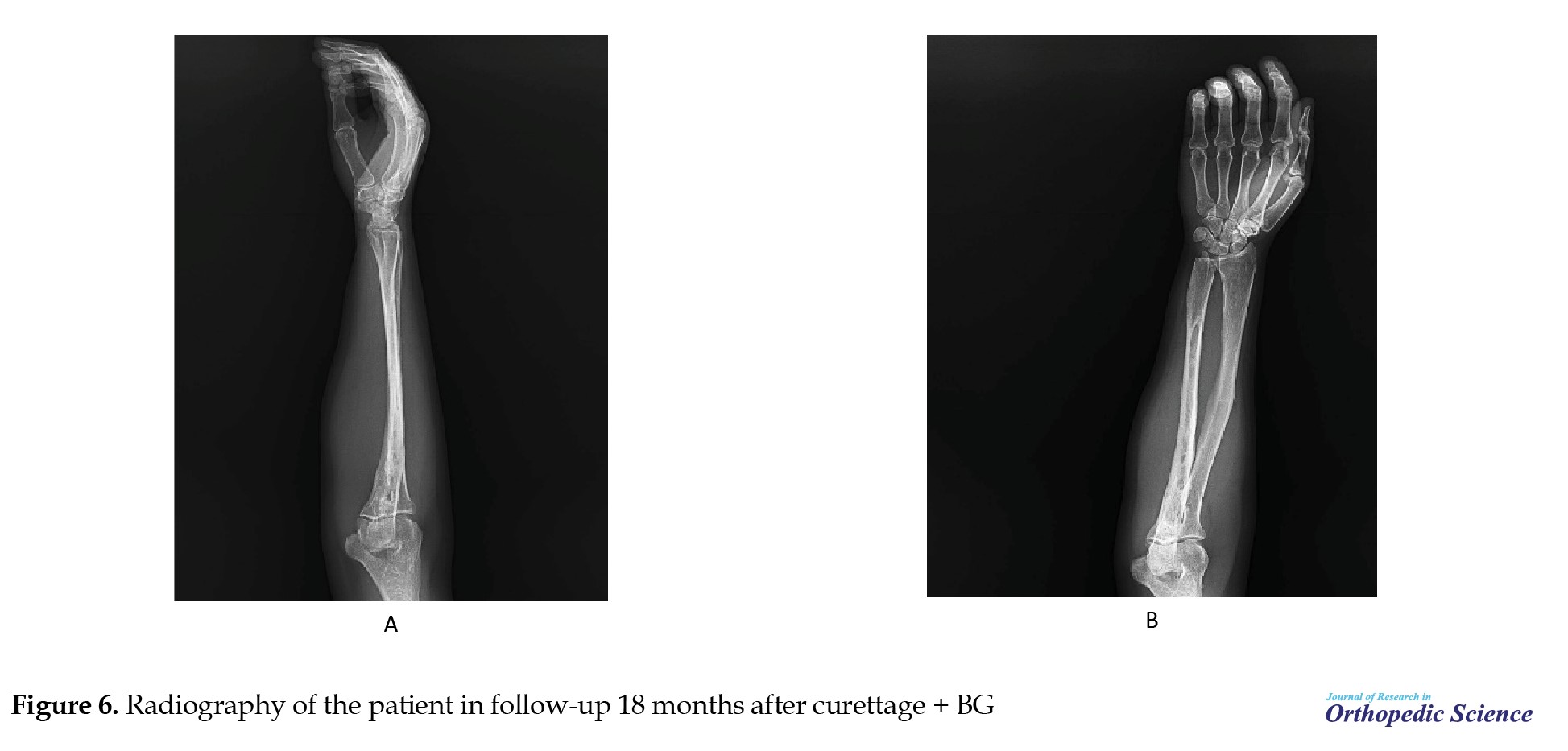
Although no history of trauma was reported, our patient had a history of bone hemangioma twice in the right ulna. Thus, ten years ago, at the age of 25, she was first diagnosed with bone hemangioma, and curettage surgery was used for treatment. However after 3 years, at the age of 28, the patient again suffered from IH in the same area and underwent cortage. And now the patient came to our center complaining of pain in the right forearm. Furthermore, the patient had no history of other special diseases and had not taken any special medicine (Figure 1). Physical examination revealed a range of motion in the elbow joint with no abnormalities, and laboratory tests revealed no significant results. Radiographs indicated a well-defined osteolytic lesion surrounded by a sclerotic border located in the metaphysis and diaphysis of the proximal ulna (Figure 2). Magnetic resonance imaging (MRI) revealed a lesion with low T1 signal intensity and high T2 signal intensity, depicting a mildly expansile intramedullary lesion in the metadiaphysis of the proximal ulna. Cortical erosion and irregularities are observed in the affected segments. Additionally, mild subperiosteal and soft tissue edema was observed. Moreover, evidence indicating previous treatment is also documented in the imaging results (Figure 3). The patient underwent extended curettage and bone grafting (BG) of the lytic lesion, along with a margin of the surrounding normal bone, as a preventive measure against pathological fractures. The surgical approach was based on the previous incision. A relatively dense fibrous tissue was observed within the marrow cavity. The defect was filled with impaction BG (Figure 4). Histopathological analysis of the excised tissues revealed a cavernous hemangioma (Figure 5). In the 18-month follow-up after curettage and BG, the patient did not have any pain symptoms, and the patient’s radiograph also showed evidence of trabrcular formation and bony remodeling in the proximal ulna, which showed corresponding to treatment response (Figure 6).
Discussion
In 1845, Toynbee reported the first vascular tumor of the bone, likely a hemangioma of the parietal bone. Roughton described benign and malignant “blood tumours” in long bones in 1890, but none seem to be hemangiomas. In 1917, Hitzrot reported the first detailed description of a solitary hemangioma in the bone of an extremity [5]. Bone hemangioma are relatively uncommon and can affect any bone regardless of age. The vertebrae and skull collectively represent over 75% of documented cases, with long tubular bones being the least frequently affected. They are characterized by increased normal or abnormal blood vessels [8].
The prevalent histological categories include capillary hemangioma, characterized by diminutive vessels and capillaries interspersed with connective tissue stroma, and cavernous hemangioma, characterized by expansive thin-walled vessels and sinuses enveloped by endothelium and filled with blood, along with fragile connective tissue stroma. Additionally, angiosarcomatous tissue has been detected in bones [9]. Solitary hemangiomas commonly affect the long bones, specifically the metadiaphysis or diaphysis, encompassing intracortical and surface-based presentations. In cases of multifocal hemangiomatosis, epiphysis may be involved in long bones [10].
Adult females are predominantly impacted by this condition, which significantly hinders their daily functioning and may lead to serious complications, such as pathological fractures. These rare, slow-developing neoplasms demonstrate a higher prevalence in women, characterized by a 1:2 male-to-female ratio [11]. Unlike vertebral or calvarial hemangiomas, typically asymptomatic, hemangiomas in the extremities often manifest with symptoms in most patients, such as local swelling or a soft-tissue mass, occurring in 77% of cases [12]. In this study, a 35-year-old woman with a history of two bone hemangioma curettages visited our hospital and was diagnosed with and treated for bone hemangioma for the third time. The presence of a lump and pain in the patient’s right forearm were the initial symptoms at the time of the visit.
IH is a relatively uncommon occurrence that predominantly involves the vertebral body and skull. Identifying IH in these specific bones is easy owing to its characteristic visual features. Conversely, definitively diagnosing IH through imaging becomes intricate when the lesion manifests in atypical sites, such as a long bone [12]. The differential diagnosis for a long bone hemangioma in a juxta-articular location consists of a giant cell tumor, aneurysmal bone cyst, and plasmacytoma [12]. Vertebral hemangiomas show a corduroy appearance on plain radiography with thickened vertical trabecula. The computed tomography (CT) images display a “polka dot” pattern, indicating vertically oriented bony trabeculae with areas of soft tissues, vessels, and lipid. Hemangiomas exhibit high signal intensity on T1WI and T2WI of MRI due to edema, adipocytes, and blood vessels. Radiographic features of this tumor are distinct between the spine and skull, aiding easy identification. However, atypical imaging can complicate diagnosing hemangiomas in the long tubular bones. Peripheral long bone hemangiomas are infrequent, causing diagnostic difficulties and insignificant radiological and laboratory examinations [13]. In this study, radiographic and MRI methods were used as diagnostic methods.
The treatment of IHs is controversial, encompassing techniques ranging from biopsy to segmental resection. Surgical intervention is typically unnecessary for small, asymptomatic, and long-bone IHs. Conversely, curettage and BG are commonly used to treat large, symptomatic lesions or pathological fractures. Nevertheless, radical en bloc resection should be advocated to prevent recurrence and massive bleeding.
Sumer Shikhare et al. documented a case study involving a 19-year-old male patient who presented with a solitary IH located in the proximal ulna. This medical condition was identified and assessed using advanced imaging modalities such as radiographic, CT scan, and MRI. Subsequently, the patient underwent a complex medical intervention in the form of an open surgical procedure, encompassing elements of open biopsy for tissue sampling and curative resection, followed by applying BG techniques to restore structural integrity and functionality to the affected skeletal site [14]. Kai Yao et al. presented a case study on multifocal IH in a 49-year-old female, demonstrating involvement in rare locations, such as bilateral ribs, lumbar vertebrae, ilium, pubis, and proximal femur. The patient opted for radiotherapy as the primary intervention for symptomatic lumbar spine. This study highlights the significant role of radiotherapy in managing symptomatic vertebral hemangiomas in patients with neurological impairments [11]. Joseph Laurian and colleagues described a 43-year-old woman with a zygomatic bone mass with slow growth and pain symptomatology. Surgery with custom-made implant reconstruction was successful. Custom biomaterials offer new options for maxillofacial surgeries. The patient had no postoperative symptoms or balanced zygomatic bone. This method is reliable for zygomatic bone reconstructions [15]. In this case, the approach of choice was curettage and BG, yielding favorable outcomes.
Christina L Goldstein et al. conducted a multicenter study to quantify the local recurrence and mortality rates following surgical intervention for symptomatic spine hemangiomas. They identified a local recurrence rate of 3% (n=2) among the 68 participants included in their investigation, with a mean age of 51 years, who underwent surgical treatment for spinal hemangiomas between 1996 and 2012 [16]. Sung-Min Park documented a case involving a recurrent of IH. They reported a 12-year-old girl with a history of curettage of an intraosseous cavernous hemangioma in the maxilla three years ago [17]. The ulna is a rare location for solitary IH; however, we describe a rare case of recurrent long-bone hemangioma that was effectively treated in the ulna. To our knowledge, this is the first report of recurrent IH of the ulna.
Conclusion
IHs are relatively uncommon and predominantly involve the vertebral body and the skull. Peripheral long-bone hemangiomas are rare, leading to diagnostic difficulties and unnecessary examinations. The differential diagnosis for a long bone hemangioma in the proximal ulna consists of a giant cell tumor, aneurysmal bone cyst, and plasmacytoma. IH causes discomfort in the ulna region. It should be considered in the differential diagnosis of a painful, radiographically benign osseous tumor around the elbow, particularly in women over the age of 30.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
Primary intraosseous hemangiomas (IHs), also recognized as hemangiomas of the bone, are non-malignant neoplasms composed of small and large vessels that develop within the bone [1]. Bone hemangiomas are infrequent intra-bony growths originating from mesenchymal cells, accounting for approximately 0.5% to 1% of all intraosseous tumors and 1% of all primary bone tumors. These IHs manifest as four distinct variants: Capillary, cavernous, mixed, and scirrhous [2]. Osseous hemangioma constitutes 1% of all primary skeletal neoplasms, predominantly located in the vertebra or skull (approximately 75%) and the clavicle, scapula, ribs, and pelvic bones (15%-20%) [3, 4].
Typically, solitary, osseous hemangiomas may also manifest as multiple lesions, characterized by thin-walled vessels or sinuses filled with blood dispersed amidst longitudinally oriented bony trabeculae, with potential secondary accumulation of lipid materials [5]. Although the lesion is often asymptomatic, it can lead to symptoms, such as hematoma formation, epidural invasion, vertebral body expansion, and pathological fractures [6]. This neoplasm, which predominantly affects the vertebrae and craniofacial bones, rarely involves the long tubular bones of the four extremities [7]. We report the case of a 35-year-old woman with an IH of the right proximal ulna. X-ray and magnetic resonance imaging showed a well-defined osteolytic lesion. The patient had a history of curettage surgery for a bone hemangioma.
Case Presentation
A 35-year-old woman was referred to our hospital complaining of right forearm pain persisting for two months. Despite conservative treatment involving the administration of analgesics and non-steroidal anti-inflammatory drugs, the pain persisted.
Although no history of trauma was reported, our patient had a history of bone hemangioma twice in the right ulna. Thus, ten years ago, at the age of 25, she was first diagnosed with bone hemangioma, and curettage surgery was used for treatment. However after 3 years, at the age of 28, the patient again suffered from IH in the same area and underwent cortage. And now the patient came to our center complaining of pain in the right forearm. Furthermore, the patient had no history of other special diseases and had not taken any special medicine (Figure 1). Physical examination revealed a range of motion in the elbow joint with no abnormalities, and laboratory tests revealed no significant results. Radiographs indicated a well-defined osteolytic lesion surrounded by a sclerotic border located in the metaphysis and diaphysis of the proximal ulna (Figure 2). Magnetic resonance imaging (MRI) revealed a lesion with low T1 signal intensity and high T2 signal intensity, depicting a mildly expansile intramedullary lesion in the metadiaphysis of the proximal ulna. Cortical erosion and irregularities are observed in the affected segments. Additionally, mild subperiosteal and soft tissue edema was observed. Moreover, evidence indicating previous treatment is also documented in the imaging results (Figure 3). The patient underwent extended curettage and bone grafting (BG) of the lytic lesion, along with a margin of the surrounding normal bone, as a preventive measure against pathological fractures. The surgical approach was based on the previous incision. A relatively dense fibrous tissue was observed within the marrow cavity. The defect was filled with impaction BG (Figure 4). Histopathological analysis of the excised tissues revealed a cavernous hemangioma (Figure 5). In the 18-month follow-up after curettage and BG, the patient did not have any pain symptoms, and the patient’s radiograph also showed evidence of trabrcular formation and bony remodeling in the proximal ulna, which showed corresponding to treatment response (Figure 6).
Discussion
In 1845, Toynbee reported the first vascular tumor of the bone, likely a hemangioma of the parietal bone. Roughton described benign and malignant “blood tumours” in long bones in 1890, but none seem to be hemangiomas. In 1917, Hitzrot reported the first detailed description of a solitary hemangioma in the bone of an extremity [5]. Bone hemangioma are relatively uncommon and can affect any bone regardless of age. The vertebrae and skull collectively represent over 75% of documented cases, with long tubular bones being the least frequently affected. They are characterized by increased normal or abnormal blood vessels [8].
The prevalent histological categories include capillary hemangioma, characterized by diminutive vessels and capillaries interspersed with connective tissue stroma, and cavernous hemangioma, characterized by expansive thin-walled vessels and sinuses enveloped by endothelium and filled with blood, along with fragile connective tissue stroma. Additionally, angiosarcomatous tissue has been detected in bones [9]. Solitary hemangiomas commonly affect the long bones, specifically the metadiaphysis or diaphysis, encompassing intracortical and surface-based presentations. In cases of multifocal hemangiomatosis, epiphysis may be involved in long bones [10].
Adult females are predominantly impacted by this condition, which significantly hinders their daily functioning and may lead to serious complications, such as pathological fractures. These rare, slow-developing neoplasms demonstrate a higher prevalence in women, characterized by a 1:2 male-to-female ratio [11]. Unlike vertebral or calvarial hemangiomas, typically asymptomatic, hemangiomas in the extremities often manifest with symptoms in most patients, such as local swelling or a soft-tissue mass, occurring in 77% of cases [12]. In this study, a 35-year-old woman with a history of two bone hemangioma curettages visited our hospital and was diagnosed with and treated for bone hemangioma for the third time. The presence of a lump and pain in the patient’s right forearm were the initial symptoms at the time of the visit.
IH is a relatively uncommon occurrence that predominantly involves the vertebral body and skull. Identifying IH in these specific bones is easy owing to its characteristic visual features. Conversely, definitively diagnosing IH through imaging becomes intricate when the lesion manifests in atypical sites, such as a long bone [12]. The differential diagnosis for a long bone hemangioma in a juxta-articular location consists of a giant cell tumor, aneurysmal bone cyst, and plasmacytoma [12]. Vertebral hemangiomas show a corduroy appearance on plain radiography with thickened vertical trabecula. The computed tomography (CT) images display a “polka dot” pattern, indicating vertically oriented bony trabeculae with areas of soft tissues, vessels, and lipid. Hemangiomas exhibit high signal intensity on T1WI and T2WI of MRI due to edema, adipocytes, and blood vessels. Radiographic features of this tumor are distinct between the spine and skull, aiding easy identification. However, atypical imaging can complicate diagnosing hemangiomas in the long tubular bones. Peripheral long bone hemangiomas are infrequent, causing diagnostic difficulties and insignificant radiological and laboratory examinations [13]. In this study, radiographic and MRI methods were used as diagnostic methods.
The treatment of IHs is controversial, encompassing techniques ranging from biopsy to segmental resection. Surgical intervention is typically unnecessary for small, asymptomatic, and long-bone IHs. Conversely, curettage and BG are commonly used to treat large, symptomatic lesions or pathological fractures. Nevertheless, radical en bloc resection should be advocated to prevent recurrence and massive bleeding.
Sumer Shikhare et al. documented a case study involving a 19-year-old male patient who presented with a solitary IH located in the proximal ulna. This medical condition was identified and assessed using advanced imaging modalities such as radiographic, CT scan, and MRI. Subsequently, the patient underwent a complex medical intervention in the form of an open surgical procedure, encompassing elements of open biopsy for tissue sampling and curative resection, followed by applying BG techniques to restore structural integrity and functionality to the affected skeletal site [14]. Kai Yao et al. presented a case study on multifocal IH in a 49-year-old female, demonstrating involvement in rare locations, such as bilateral ribs, lumbar vertebrae, ilium, pubis, and proximal femur. The patient opted for radiotherapy as the primary intervention for symptomatic lumbar spine. This study highlights the significant role of radiotherapy in managing symptomatic vertebral hemangiomas in patients with neurological impairments [11]. Joseph Laurian and colleagues described a 43-year-old woman with a zygomatic bone mass with slow growth and pain symptomatology. Surgery with custom-made implant reconstruction was successful. Custom biomaterials offer new options for maxillofacial surgeries. The patient had no postoperative symptoms or balanced zygomatic bone. This method is reliable for zygomatic bone reconstructions [15]. In this case, the approach of choice was curettage and BG, yielding favorable outcomes.
Christina L Goldstein et al. conducted a multicenter study to quantify the local recurrence and mortality rates following surgical intervention for symptomatic spine hemangiomas. They identified a local recurrence rate of 3% (n=2) among the 68 participants included in their investigation, with a mean age of 51 years, who underwent surgical treatment for spinal hemangiomas between 1996 and 2012 [16]. Sung-Min Park documented a case involving a recurrent of IH. They reported a 12-year-old girl with a history of curettage of an intraosseous cavernous hemangioma in the maxilla three years ago [17]. The ulna is a rare location for solitary IH; however, we describe a rare case of recurrent long-bone hemangioma that was effectively treated in the ulna. To our knowledge, this is the first report of recurrent IH of the ulna.
Conclusion
IHs are relatively uncommon and predominantly involve the vertebral body and the skull. Peripheral long-bone hemangiomas are rare, leading to diagnostic difficulties and unnecessary examinations. The differential diagnosis for a long bone hemangioma in the proximal ulna consists of a giant cell tumor, aneurysmal bone cyst, and plasmacytoma. IH causes discomfort in the ulna region. It should be considered in the differential diagnosis of a painful, radiographically benign osseous tumor around the elbow, particularly in women over the age of 30.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
- Choi JH, Ro JY. The 2020 WHO classification of tumors of soft tissue: Selected changes and new entities. Adv Anat Pathol. 2021; 28(1):44-58. [DOI:10.1097/PAP.0000000000000284] [PMID]
- Li Z, Tang J, Ye Z. Solitary haemangioma of the shaft of long bones: resection and reconstruction with autologous bone graft. Acta Orthop Belg. 2013; 79(2):230-4. [PMID]
- Hung CT, Jou IM, Huang MT. Intraosseous capillary haemangioma of a metacarpal bone. J Hand Surg Eur Vol. 2012; 37(1):76-7. [DOI:10.1177/1753193411423880] [PMID]
- Maclean FM, Schatz J, McCarthy SW, Scolyer RA, Stalley P, Bonar SF. Epithelioid and spindle cell haemangioma of bone. Skeletal Radiol. 2007; 36(Suppl 1):S50-7. [DOI:10.1007/s00256-006-0135-z] [PMID]
- Kaleem Z, Kyriakos M, Totty WG. Solitary skeletal hemangioma of the extremities. Skeletal Radiol. 2000; 29(9):502-13. [DOI:10.1007/s002560000251] [PMID]
- Hwang PM. Vertebral abnormality in a patient with suspected malignancy. Proc. 2002; 15(3):325-6. [DOI:10.1080/08998280.2002.11927858] [PMID] [PMCID]
- Vilanova JC, Barceló J, Smirniotopoulos JG, Pérez-Andrés R, Villalón M, Miró J, et al. Hemangioma from head to toe: MR imaging with pathologic correlation. Radiographics. 2004; 24(2):367-85. [DOI:10.1148/rg.242035079] [PMID]
- Li W, Zou F, Dai M, Zhang B, Nie T. A rare case of pure primary hemangioma of the scapula: A case report. Oncol Lett. 2015; 10(4):2265-8. [DOI:10.3892/ol.2015.3596] [PMID] [PMCID]
- Oosthuizen SF, Barnetson J. Hemangioma of bone. Radiology. 1951; 56(2):256-9. [DOI:10.1148/56.2.256] [PMID]
- Yamamoto T, Kurosaka M, Mizuno K. Juxta-articular hemangioma of long bone. Skeletal Radiol. 2000; 29(9):535-7. [DOI:10.1007/s002560000256] [PMID]
- Yao K, Tang F, Min L, Zhou Y, Tu C. Multifocal intraosseous hemangioma: A case report. Medicine. 2019; 98(2):e14001. [DOI:10.1097/MD.0000000000014001] [PMID] [PMCID]
- Rajani AM, Shah UA, Mittal ARS, Punamiya M. Management of a rare case of cavernous medullary intraosseous hemangioma in proximal tibia of a 38-year-old female. J Orthop Case Rep. 2022; 12(5):96-100. [DOI:10.13107/jocr.2022.v12.i05.2834] [PMID] [PMCID]
- Cao L, Wen JX, Han SM, Wu HZ, Peng ZG, Yu BH, et al. Imaging features of hemangioma in long tubular bones. BMC Musculoskelet Disord. 2021; 22(1):27. [DOI:10.1186/s12891-020-03882-2] [PMID] [PMCID]
- Shikhare S, Sittampalam K, Peh W, Shimpi T. Proximal ulna: A rare location for solitary intraosseous hemangioma. Oman Med J. 2018; 33(3):260-3. [DOI:10.5001/omj.2018.48] [PMID] [PMCID]
- Laurian LJ, Decaudaveine S, Caillot A, Walter P, Benichou L. Case report of a zygomatic bone hemangioma surgery with reconstruction by a custom-made implant. J Stomatol Oral Maxillofac Surg. 2022; 123(6):660-2. [DOI:10.1016/j.jormas.2022.06.019] [PMID]
- Goldstein CL, Varga PP, Gokaslan ZL, Boriani S, Luzzati A, Rhines L, et al. Spinal hemangiomas: Results of surgical management for local recurrence and mortality in a multicenter study. Spine. 2015; 40(9):656-64. [DOI:10.1097/BRS.0000000000000840] [PMID]
- Park SM, Lee JH. Recurrence of intraosseous cavernous hemangioma in the maxilla: A case report. Oral Maxillofac Surg Cases. 2020; 6(2):100147. [DOI:10.1016/j.omsc.2020.100147]
Type of Study: Case Report |
Subject:
Hand surgery / Elbow
Received: 2022/04/28 | Accepted: 2023/01/7 | Published: 2023/11/1
Received: 2022/04/28 | Accepted: 2023/01/7 | Published: 2023/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |