Volume 10, Issue 2 (5-2023)
JROS 2023, 10(2): 89-94 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chehrassan M, Shakeri M, Nikouei F, Valiollahpour Amiri A, Dadvar A, Ameri E et al . Midterm Outcomes and Complications of Scoliosis Correction in Adolescent Idiopathic Scoliosis: A Tertiary Center Study. JROS 2023; 10 (2) :89-94
URL: http://jros.iums.ac.ir/article-1-2243-en.html
URL: http://jros.iums.ac.ir/article-1-2243-en.html
Mohammadreza Chehrassan1 

 , Mohammadreza Shakeri1
, Mohammadreza Shakeri1 

 , Farshad Nikouei1
, Farshad Nikouei1 

 , Ali Valiollahpour Amiri1
, Ali Valiollahpour Amiri1 

 , Amirali Dadvar1
, Amirali Dadvar1 
 , Ebrahim Ameri1
, Ebrahim Ameri1 

 , Hasan Ghandhari1
, Hasan Ghandhari1 




 , Mohammadreza Shakeri1
, Mohammadreza Shakeri1 

 , Farshad Nikouei1
, Farshad Nikouei1 

 , Ali Valiollahpour Amiri1
, Ali Valiollahpour Amiri1 

 , Amirali Dadvar1
, Amirali Dadvar1 
 , Ebrahim Ameri1
, Ebrahim Ameri1 

 , Hasan Ghandhari1
, Hasan Ghandhari1 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafaihiyayan Hospital, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Adolescent idiopathic scoliosis (AIS), Spinal fusion, Pedicle screw, Surgical complications, Postoperative pain
Full-Text [PDF 454 kb]
(147 Downloads)
| Abstract (HTML) (1128 Views)
Full-Text: (271 Views)
Introduction
Adolescent idiopathic scoliosis (AIS) is the primary cause of spinal deformities in the pediatric population. Extensive research has explored the natural progression of AIS and devising effective treatment methodologies [1-3]. Among these, spinal fusion surgery combined with instrumentation has emerged as the gold standard for managing severe cases of scoliosis [4]. However, this surgical procedure poses a physiological burden on healthy adolescents and requires a delicate balance between achieving correction and potential loss of mobility. While traditional evaluation methods have relied on radiographic parameters to assess the efficacy of spinal fusion, there is a growing emphasis on incorporating patient-reported quality-of-life assessments as primary indicators of treatment success [5, 6].
Advancements in AIS surgery introduced pedicle screw technology, offering improved three-dimensional orthopedic effects with fewer segments involved compared to complete hook techniques [7]. Pedicle screw instrumentation, particularly effective for patients with presurgical Cobb angles of less than 60 degrees, has shown safety and efficacy in correcting frontal and sagittal plane deformities [8]. Despite requiring one more integrated segment, posterior surgery with pedicle screws demonstrated comparable outcomes to anterior surgery, although with decreased surgical risks and shorter hospital stays [9]. This shift in favor of posterior surgery was attributed to reduced complications and surgical injury [10, 11].
Based on the above information and the importance of the patient’s outcome and surgical technique in AIS, we conducted a retrospective cohort analysis of AIS cases treated at our hospital before 2011 to compare the advantages and disadvantages and evaluate the patients’ postoperative complications and outcomes.
Methods
This retrospective cohort study employed a census sampling method, enrolling all patients diagnosed with AIS who underwent corrective surgery at Shafayahaieyan Hospital before 2011. The inclusion criteria included patients diagnosed with AIS by a spine subspecialist who underwent posterior spinal fusion (PSF) or anterior spinal fusion (ASF) surgery. The exclusion criteria included patients with congenital, neuromuscular, or infantile scoliosis, a history of previous spine surgeries, such as discectomy, and the presence of diseases, such as rheumatoid arthritis and diabetes, that may affect surgical outcomes.
Data collection involved reviewing patients’ hospitals and follow-up records. The collected data included demographic information at the time of surgery, including age, sex, occupation, educational level, sports activities, marital status, number of children, type of surgical procedure, presence or absence of back pain, Cobb angle before and after surgery, and during follow-up visits.
Patients were followed for up to five years, and postoperative complications following five years after corrective surgery were also collected, including history of reoperation due to involvement of upper or lower parts, proximal junctional kyphosis/distal junctional kyphosis, reoperation history due to device failure, history of infection, reoperation history due to pain or non:union:, history of prominence of subcutaneous device, history of device removal, and patient satisfaction.
Statistical analysis
Data were entered and analyzed using SPSS software, version 26. The results are presented as frequencies and percentages (%) for qualitative variables and as Mean±SD for quantitative variables. The normality of data distribution was assessed using the Kolmogorov-Smirnov test. The relationships between variables were assessed using chi-square and independent t-test for normally distributed data and nonparametric tests, such as Mann-Whitney and Wilcoxon ranked test for non-normally distributed data. Statistical significance was set at P<0.05.
Results
A total of 95 patients were evaluated in our study. The mean age of patients at the time of scoliosis diagnosis ranged from 10 to 25 years (Mean±SD 13.62±2.69 years), and 13 patients (13.68%) were men. Among these, 20 patients (21.05%) underwent corrective surgery for anterior-posterior scoliosis, and 75(78.95%) underwent corrective surgery for posterior scoliosis. Patients were followed up for an average of 6.63±3.2 years. Table 1 presents the demographical and clinical features of the patients included in our study.
.jpg)
The mean Cobb angle before corrective surgery in patients was 49.99±13.61°, which decreased to 16.79±8.09° postoperatively. The average decrease was 33.20±10.71°. Based on the Wilcoxon signed rank test analysis, this decrease was statistically significant (P<0.001). Furthermore, no relationship was observed between the amount of Cobb angle decrease with the surgery method (P=0.090), patient age (P=0.768), gender (P=0.101), and BMI (P=0.068).
Regarding the patients’ postoperative complications, midterm complications (6.63±3.2 years postoperatively) in the study patients included surgical site infection (SSI) (6 cases, 6.3%), surgical site pain (2 cases, 2.1%), and instrument-related complications (5 cases, 5.2%) (Table 2).
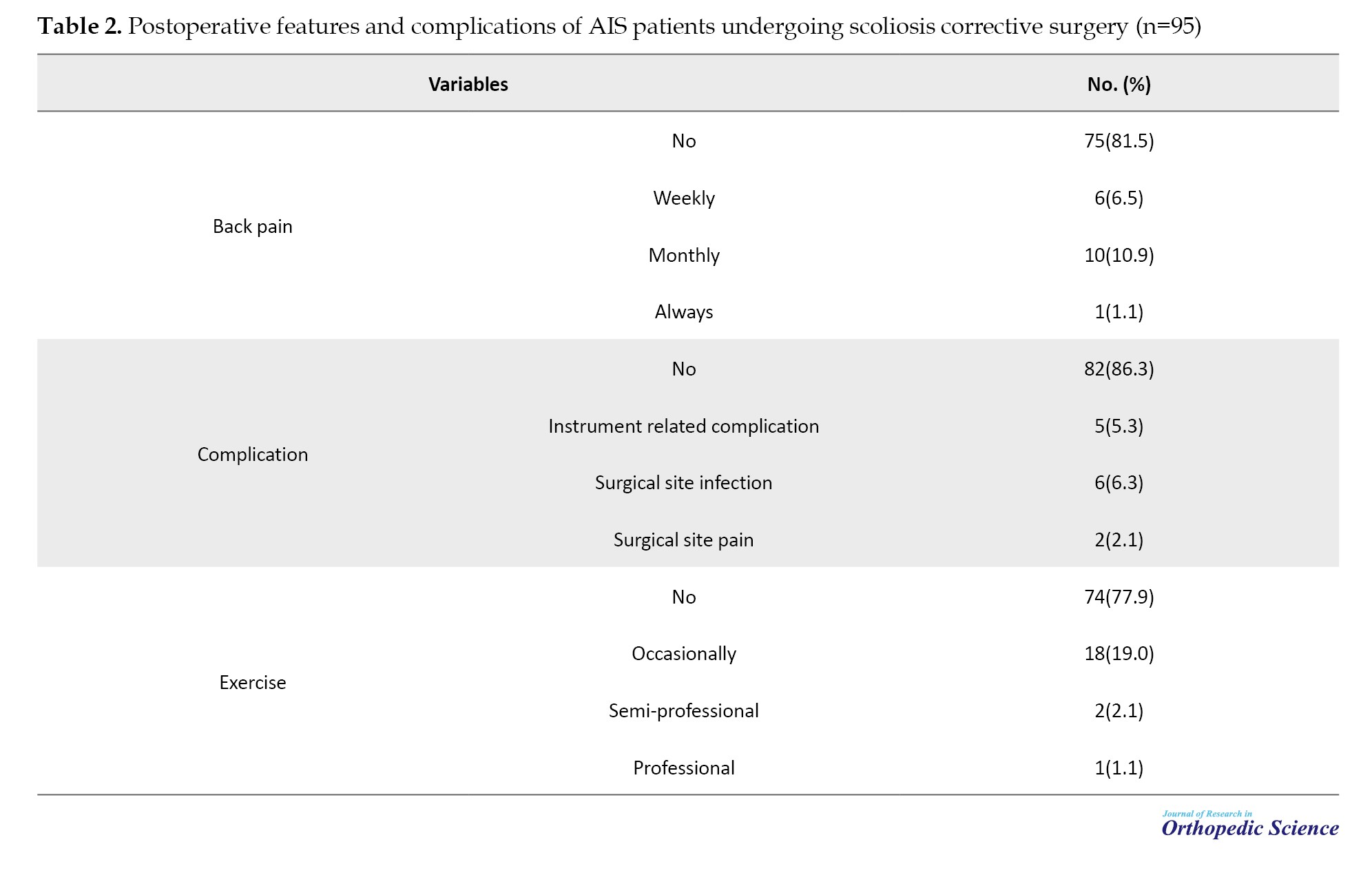
After corrective surgery, one patient (1.05%) reported continuous and daily back pain, six patients (6.31%) reported weekly back pain, 10 patients (10.52%) reported monthly back pain, and the remaining patients (78 out of 95, 82.1%) reported no back pain during the 5-year postoperative period. Furthermore, one patient (1.05%) engaged in professional sports, two patients (2.1%) engaged in semi-professional sports, 17 patients (17.89%) engaged in occasional and recreational sports, and the remaining patients (75 of 95, 78.94%) reported no physical activity (Table 2).
Discussion
This study investigated the frequency of complaints and complications experienced by patients during five years of corrective surgery for scoliosis and the associated factors, including the patient’s age, sex, and type of surgical procedure. In summary, our study underscores the effectiveness of fusion-based surgery for correcting scoliosis in adolescents, as evidenced by reduced Cobb angle and alleviated postoperative issues. Nonetheless, undergoing surgery does not automatically result in heightened physical activity or increased engagement in exercise.
The primary quantitative measure used to assess scoliosis correction was the change in the Cobb angle. Regardless of the surgical technique employed, the postoperative Cobb angle was significantly reduced compared to the initial angle in all patients, indicating the success of surgical intervention in addressing this issue. Despite the higher prevalence of the posterior surgical approach than the anterior-posterior approach, no significant difference was observed in the postoperative Cobb angle correction. This result is consistent with previous studies and underscores the effectiveness of fusion-based surgical approaches in treating scoliosis.
Early SSI following AIS surgery is observed at a rate of 1.6% [12]. The federal directive aimed at eradicating SSIs and the potential withholding of reimbursements for their treatment could prompt shifts in clinical protocols. The results of a study by Marks et al. [12] offer benchmark SSI rates aggregated from various centers, facilitating future comparisons. Analyzing practice disparities among centers may reveal areas warranting enhancement to minimize SSIs in patients with AIS. Encouragingly, 92% of patients maintained their implants and remained pain-free at the last follow-up assessment [12]. In our study, complaints reported by patients postoperatively over five years were primarily related to infection and postoperative pain, albeit infrequently. Commonly reported complaints, such as those related to implant sensations, are rare. The incidence of postoperative complaints related to corrective surgery for scoliosis is low. Sensations associated with implanted devices, including feelings of foreign objects in the body, have occasionally been reported and may require further examination by researchers in future studies.
Back pain is a common complaint in AIS. Danielsson et al. reported that back pain is a prevalent issue affecting three-quarters of adolescents diagnosed with idiopathic scoliosis. However, PSF has also been shown to reduce pain. Factors, such as being overweight, older age, and larger proximal thoracic curve magnitudes are associated with greater preoperative pain. Additionally, patients who perceive themselves as more deformed experience higher levels of pain and may have less postoperative pain relief [13]. As expected, the prevalence of postoperative back pain was minimal, and most patients reported either no pain or occasional monthly discomfort. Given the high prevalence of back pain in the general population worldwide, factors other than surgical intervention may contribute to postoperative discomfort, including pre-existing back pain in patients. The primary therapeutic goal of scoliosis surgery is symptom relief and functional restoration, as evidenced by the study’s results indicating successful surgical outcomes for patients at our center.
Bridwell et al. highlighted that the primary motivation for undergoing AIS surgery is often the anticipation of reducing future pain and disability in adulthood [14]. However, long-term follow-up studies from 5 to 20 years do not convincingly demonstrate these expectations. Furthermore, inconclusive evidence indicates that improved radiographic outcomes translate into enhanced function, self-image, or overall health [15, 16]. Despite adolescents with AIS potentially experiencing significant psychological distress, body image concerns, and other health-related quality-of-life issues, these issues diminish with transition into adulthood [17]. An analysis of postoperative physical activity levels revealed that most patients did not engage in any physical exercise. This result may be attributed to various reasons, including physician recommendations to avoid exercise, patients’ fear of exacerbating symptoms, back pain, inability to perform exercises, and family and caregivers’ recommendations.
Conclusion
In conclusion, this study demonstrates the success of fusion-based scoliosis corrective surgery in adolescents, reducing Cobb angle and mitigating postoperative complaints. However, surgical interventions do not necessarily increase physical activity or exercise engagement.
Our study had several limitations. First, the sample size was small, and the study was conducted at a single center. Additionally, our study’s retrospective nature limits data collection and analysis. Further research is needed to overcome these limitations and obtain more robust results. Specifically, multicenter studies involving larger populations provide comprehensive insights. Moreover, randomized clinical trials offer a more rigorous evaluation of the effects of different treatment methods and variables on patient outcomes.
Ethical Considerations
Compliance with ethical guidelines
The Institutional Review Board of IIran University of Medical Sciences approved the study. The university administrators were asked for permission to conduct the study and access the patient’s records. The study complied with the relevant guidelines and regulations and the Declaration of Helsinki and was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
Adolescent idiopathic scoliosis (AIS) is the primary cause of spinal deformities in the pediatric population. Extensive research has explored the natural progression of AIS and devising effective treatment methodologies [1-3]. Among these, spinal fusion surgery combined with instrumentation has emerged as the gold standard for managing severe cases of scoliosis [4]. However, this surgical procedure poses a physiological burden on healthy adolescents and requires a delicate balance between achieving correction and potential loss of mobility. While traditional evaluation methods have relied on radiographic parameters to assess the efficacy of spinal fusion, there is a growing emphasis on incorporating patient-reported quality-of-life assessments as primary indicators of treatment success [5, 6].
Advancements in AIS surgery introduced pedicle screw technology, offering improved three-dimensional orthopedic effects with fewer segments involved compared to complete hook techniques [7]. Pedicle screw instrumentation, particularly effective for patients with presurgical Cobb angles of less than 60 degrees, has shown safety and efficacy in correcting frontal and sagittal plane deformities [8]. Despite requiring one more integrated segment, posterior surgery with pedicle screws demonstrated comparable outcomes to anterior surgery, although with decreased surgical risks and shorter hospital stays [9]. This shift in favor of posterior surgery was attributed to reduced complications and surgical injury [10, 11].
Based on the above information and the importance of the patient’s outcome and surgical technique in AIS, we conducted a retrospective cohort analysis of AIS cases treated at our hospital before 2011 to compare the advantages and disadvantages and evaluate the patients’ postoperative complications and outcomes.
Methods
This retrospective cohort study employed a census sampling method, enrolling all patients diagnosed with AIS who underwent corrective surgery at Shafayahaieyan Hospital before 2011. The inclusion criteria included patients diagnosed with AIS by a spine subspecialist who underwent posterior spinal fusion (PSF) or anterior spinal fusion (ASF) surgery. The exclusion criteria included patients with congenital, neuromuscular, or infantile scoliosis, a history of previous spine surgeries, such as discectomy, and the presence of diseases, such as rheumatoid arthritis and diabetes, that may affect surgical outcomes.
Data collection involved reviewing patients’ hospitals and follow-up records. The collected data included demographic information at the time of surgery, including age, sex, occupation, educational level, sports activities, marital status, number of children, type of surgical procedure, presence or absence of back pain, Cobb angle before and after surgery, and during follow-up visits.
Patients were followed for up to five years, and postoperative complications following five years after corrective surgery were also collected, including history of reoperation due to involvement of upper or lower parts, proximal junctional kyphosis/distal junctional kyphosis, reoperation history due to device failure, history of infection, reoperation history due to pain or non:union:, history of prominence of subcutaneous device, history of device removal, and patient satisfaction.
Statistical analysis
Data were entered and analyzed using SPSS software, version 26. The results are presented as frequencies and percentages (%) for qualitative variables and as Mean±SD for quantitative variables. The normality of data distribution was assessed using the Kolmogorov-Smirnov test. The relationships between variables were assessed using chi-square and independent t-test for normally distributed data and nonparametric tests, such as Mann-Whitney and Wilcoxon ranked test for non-normally distributed data. Statistical significance was set at P<0.05.
Results
A total of 95 patients were evaluated in our study. The mean age of patients at the time of scoliosis diagnosis ranged from 10 to 25 years (Mean±SD 13.62±2.69 years), and 13 patients (13.68%) were men. Among these, 20 patients (21.05%) underwent corrective surgery for anterior-posterior scoliosis, and 75(78.95%) underwent corrective surgery for posterior scoliosis. Patients were followed up for an average of 6.63±3.2 years. Table 1 presents the demographical and clinical features of the patients included in our study.
.jpg)
The mean Cobb angle before corrective surgery in patients was 49.99±13.61°, which decreased to 16.79±8.09° postoperatively. The average decrease was 33.20±10.71°. Based on the Wilcoxon signed rank test analysis, this decrease was statistically significant (P<0.001). Furthermore, no relationship was observed between the amount of Cobb angle decrease with the surgery method (P=0.090), patient age (P=0.768), gender (P=0.101), and BMI (P=0.068).
Regarding the patients’ postoperative complications, midterm complications (6.63±3.2 years postoperatively) in the study patients included surgical site infection (SSI) (6 cases, 6.3%), surgical site pain (2 cases, 2.1%), and instrument-related complications (5 cases, 5.2%) (Table 2).
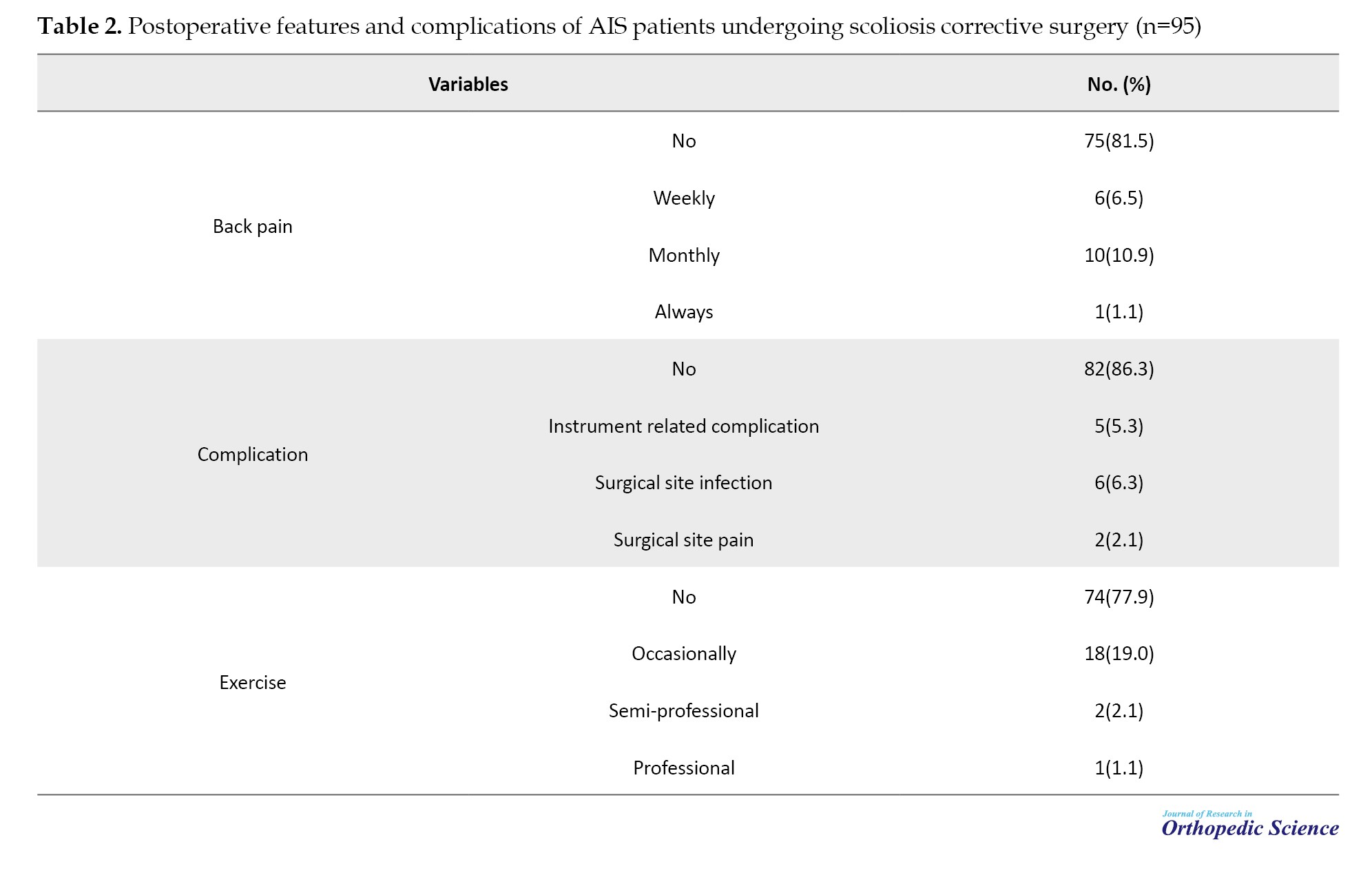
After corrective surgery, one patient (1.05%) reported continuous and daily back pain, six patients (6.31%) reported weekly back pain, 10 patients (10.52%) reported monthly back pain, and the remaining patients (78 out of 95, 82.1%) reported no back pain during the 5-year postoperative period. Furthermore, one patient (1.05%) engaged in professional sports, two patients (2.1%) engaged in semi-professional sports, 17 patients (17.89%) engaged in occasional and recreational sports, and the remaining patients (75 of 95, 78.94%) reported no physical activity (Table 2).
Discussion
This study investigated the frequency of complaints and complications experienced by patients during five years of corrective surgery for scoliosis and the associated factors, including the patient’s age, sex, and type of surgical procedure. In summary, our study underscores the effectiveness of fusion-based surgery for correcting scoliosis in adolescents, as evidenced by reduced Cobb angle and alleviated postoperative issues. Nonetheless, undergoing surgery does not automatically result in heightened physical activity or increased engagement in exercise.
The primary quantitative measure used to assess scoliosis correction was the change in the Cobb angle. Regardless of the surgical technique employed, the postoperative Cobb angle was significantly reduced compared to the initial angle in all patients, indicating the success of surgical intervention in addressing this issue. Despite the higher prevalence of the posterior surgical approach than the anterior-posterior approach, no significant difference was observed in the postoperative Cobb angle correction. This result is consistent with previous studies and underscores the effectiveness of fusion-based surgical approaches in treating scoliosis.
Early SSI following AIS surgery is observed at a rate of 1.6% [12]. The federal directive aimed at eradicating SSIs and the potential withholding of reimbursements for their treatment could prompt shifts in clinical protocols. The results of a study by Marks et al. [12] offer benchmark SSI rates aggregated from various centers, facilitating future comparisons. Analyzing practice disparities among centers may reveal areas warranting enhancement to minimize SSIs in patients with AIS. Encouragingly, 92% of patients maintained their implants and remained pain-free at the last follow-up assessment [12]. In our study, complaints reported by patients postoperatively over five years were primarily related to infection and postoperative pain, albeit infrequently. Commonly reported complaints, such as those related to implant sensations, are rare. The incidence of postoperative complaints related to corrective surgery for scoliosis is low. Sensations associated with implanted devices, including feelings of foreign objects in the body, have occasionally been reported and may require further examination by researchers in future studies.
Back pain is a common complaint in AIS. Danielsson et al. reported that back pain is a prevalent issue affecting three-quarters of adolescents diagnosed with idiopathic scoliosis. However, PSF has also been shown to reduce pain. Factors, such as being overweight, older age, and larger proximal thoracic curve magnitudes are associated with greater preoperative pain. Additionally, patients who perceive themselves as more deformed experience higher levels of pain and may have less postoperative pain relief [13]. As expected, the prevalence of postoperative back pain was minimal, and most patients reported either no pain or occasional monthly discomfort. Given the high prevalence of back pain in the general population worldwide, factors other than surgical intervention may contribute to postoperative discomfort, including pre-existing back pain in patients. The primary therapeutic goal of scoliosis surgery is symptom relief and functional restoration, as evidenced by the study’s results indicating successful surgical outcomes for patients at our center.
Bridwell et al. highlighted that the primary motivation for undergoing AIS surgery is often the anticipation of reducing future pain and disability in adulthood [14]. However, long-term follow-up studies from 5 to 20 years do not convincingly demonstrate these expectations. Furthermore, inconclusive evidence indicates that improved radiographic outcomes translate into enhanced function, self-image, or overall health [15, 16]. Despite adolescents with AIS potentially experiencing significant psychological distress, body image concerns, and other health-related quality-of-life issues, these issues diminish with transition into adulthood [17]. An analysis of postoperative physical activity levels revealed that most patients did not engage in any physical exercise. This result may be attributed to various reasons, including physician recommendations to avoid exercise, patients’ fear of exacerbating symptoms, back pain, inability to perform exercises, and family and caregivers’ recommendations.
Conclusion
In conclusion, this study demonstrates the success of fusion-based scoliosis corrective surgery in adolescents, reducing Cobb angle and mitigating postoperative complaints. However, surgical interventions do not necessarily increase physical activity or exercise engagement.
Our study had several limitations. First, the sample size was small, and the study was conducted at a single center. Additionally, our study’s retrospective nature limits data collection and analysis. Further research is needed to overcome these limitations and obtain more robust results. Specifically, multicenter studies involving larger populations provide comprehensive insights. Moreover, randomized clinical trials offer a more rigorous evaluation of the effects of different treatment methods and variables on patient outcomes.
Ethical Considerations
Compliance with ethical guidelines
The Institutional Review Board of IIran University of Medical Sciences approved the study. The university administrators were asked for permission to conduct the study and access the patient’s records. The study complied with the relevant guidelines and regulations and the Declaration of Helsinki and was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
- McPhail GL, Ehsan Z, Howells SA, Boesch RP, Fenchel MC, Szczesniak R, et al. Obstructive lung disease in children with idiopathic scoliosis. J Pediatr. 2015; 166(4):1018-21. [DOI:10.1016/j.jpeds.2014.12.070] [PMID]
- Vitale MG, Matsumoto H, Bye MR, Gomez JA, Booker WA, Hyman JE, et al. A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in children with congenital scoliosis: An evaluation of patient outcomes after early spinal fusion. Spine. 2008; 33(11):1242-9. [DOI:10.1097/BRS.0b013e3181714536] [PMID]
- Tao F, Wang Z, Li M, Pan F, Shi Z, Zhang Y, et al. A comparison of anterior and posterior instrumentation for restoring and retaining sagittal balance in patients with idiopathic adolescent scoliosis. J Spinal Disord Tech. 2012; 25(6):303-8. [DOI:10.1097/BSD.0b013e3182204c3e] [PMID]
- Helenius I, Remes V, Yrjönen T, Ylikoski M, Schlenzka D, Helenius M, et al. Comparison of long-term functional and radiologic outcomes after Harrington instrumentation and spondylodesis in adolescent idiopathic scoliosis: A review of 78 patients. Spine. 2002; 27(2):176-80. [DOI:10.1097/00007632-200201150-00010] [PMID]
- Andrawis JP, Chenok KE, Bozic KJ. Health policy implications of outcomes measurement in orthopaedics. Clin Orthop Relat Res. 2013; 471(11):3475-81. [DOI:10.1007/s11999-013-3014-7] [PMID] [PMCID]
- Brodke DJ, Saltzman CL, Brodke DS. PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg. 2016; 24(11):744-9. [DOI:10.5435/JAAOS-D-15-00404] [PMID]
- Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994; 18(6):341-6. [DOI:10.1007/BF00187077] [PMID]
- Halm H, Niemeyer T, Link T, Liljenqvist U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J. 2000; 9(3):191-7. [DOI:10.1007/s005860000139] [PMID] [PMCID]
- Hee HT, Yu ZR, Wong HK. Comparison of segmental pedicle screw instrumentation versus anterior instrumentation in adolescent idiopathic thoracolumbar and lumbar scoliosis. Spine. 2007; 32(14):1533-42. [DOI:10.1097/BRS.0b013e318067dc3d] [PMID]
- Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, et al. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: Anterior dual rod versus posterior pedicle fixation surgery: A comparison of two practices. Spine. 2009; 34(18):1942-51. [DOI:10.1097/BRS.0b013e3181a3c777] [PMID]
- Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999; 24(3):225-39. [DOI:10.1097/00007632-199902010-00007] [PMID]
- Marks MC, Newton PO, Bastrom TP, Betz RR, Sponseller PD, Lonner B, et al. Surgical site infection in adolescent idiopathic scoliosis surgery. Spine Deform. 2013; 1(5):352-8. [DOI:10.1016/j.jspd.2013.07.004] [PMID]
- Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: A case-control study-part II. Spine. 2003; 28(18):E373-83. [DOI:10.1097/01.BRS.0000084267.41183.75] [PMID]
- Bridwell KH, Shufflebarger HL, Lenke LG, Lowe TG, Betz RR, Bassett GS. Parents' and patients' preferences and concerns in idiopathic adolescent scoliosis: A cross-sectional preoperative analysis. Spine. 2000; 25(18):2392-9. [DOI:10.1097/00007632-200009150-00020] [PMID]
- Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008; 371(9623):1527-37. [DOI:10.1016/S0140-6736(08)60658-3] [PMID]
- Bridwell KH, Anderson PA, Boden SD, Vaccaro AR, Wang JC. What’s new in spine surgery. JBJS. 2007; 89(7):1654-63. [DOI:10.2106/JBJS.G.00425]
- Tones M, Moss N, Polly DW Jr. A review of quality of life and psychosocial issues in scoliosis. Spine. 2006; 31(26):3027-38. [DOI:10.1097/01.brs.0000249555.87601.fc] [PMID]
Type of Study: Research Article |
Subject:
Spine surgery
Received: 2022/05/12 | Accepted: 2022/05/19 | Published: 2023/05/8
Received: 2022/05/12 | Accepted: 2022/05/19 | Published: 2023/05/8
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |