Volume 10, Issue 2 (5-2023)
JROS 2023, 10(2): 95-100 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jabalameli M, Yahyazadeh H, Bagherifard A, Askari A, Alsamori S. Kirschner Wire in the Fixation of Knee Osteochondral Lesions. JROS 2023; 10 (2) :95-100
URL: http://jros.iums.ac.ir/article-1-2247-en.html
URL: http://jros.iums.ac.ir/article-1-2247-en.html
Mahmoud Jabalameli1 

 , Houman Yahyazadeh1
, Houman Yahyazadeh1 

 , Abolfazl Bagherifard1
, Abolfazl Bagherifard1 

 , Alireza Askari1
, Alireza Askari1 
 , Shadi Alsamori1
, Shadi Alsamori1 




 , Houman Yahyazadeh1
, Houman Yahyazadeh1 

 , Abolfazl Bagherifard1
, Abolfazl Bagherifard1 

 , Alireza Askari1
, Alireza Askari1 
 , Shadi Alsamori1
, Shadi Alsamori1 


1- Department of Orthopedics, School of Medicine, Bone and Joint Reconstruction Research Center, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 1878 kb]
(146 Downloads)
| Abstract (HTML) (879 Views)
Full-Text: (210 Views)
Introduction
Osteochondral lesions of the knee are common among adolescent populations and can result from primary traumatic osteochondral fracture or secondary to osteochondritis dissecans [1, 2]. Several factors, including lesion size, stability, and symptom severity, influence these lesions’ treatment. Accordingly, managing these lesions includes a range of procedures from fixation to microfracture/marrow stimulation and autograft/allograft implantation [3-6].
Surgical fixation is preferred for treating osteochondral lesions because it perfectly restores the native articular surface [3]. Various fixation methods are available for this purpose. Metal implants, such as headless screws and biodegradable implants, are routinely used for the fixation of osteochondral lesions, both of which have demonstrated acceptable radiographic healing [7, 8]. Bioabsorbable implants are considered a viable alternative to metal implants because they obviate the need for a second procedure for implant removal. However, bioabsorbable screws are more expensive than conventional implants; therefore, they are not available in many orthopedic centers, particularly in developing countries [9]. In addition, both bioabsorbable and non-bioabsorbable screws have been associated with a high reoperation rate of up to 44% in systematic evaluation [10]. Therefore, developing affordable fixation methods that provide the same or superior outcomes to the available methods while being easily removable is of significant value.
Methods
The medical history of patients with osteochondral lesions of the knee managed with surgical fixation between 2015 and 2020 was retrospectively evaluated. The inclusion criteria included surgical treatment in the acute phase of injury, fixation with K-wire, and a minimum one-year follow-up period. The exclusion criteria included patients with a history of fracture, surgery of the ipsilateral knee, or associated knee injuries. Twenty-one patients met the study requirements, of whom 15 were eligible for the final evaluation and inclusion.
Surgical procedure
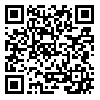
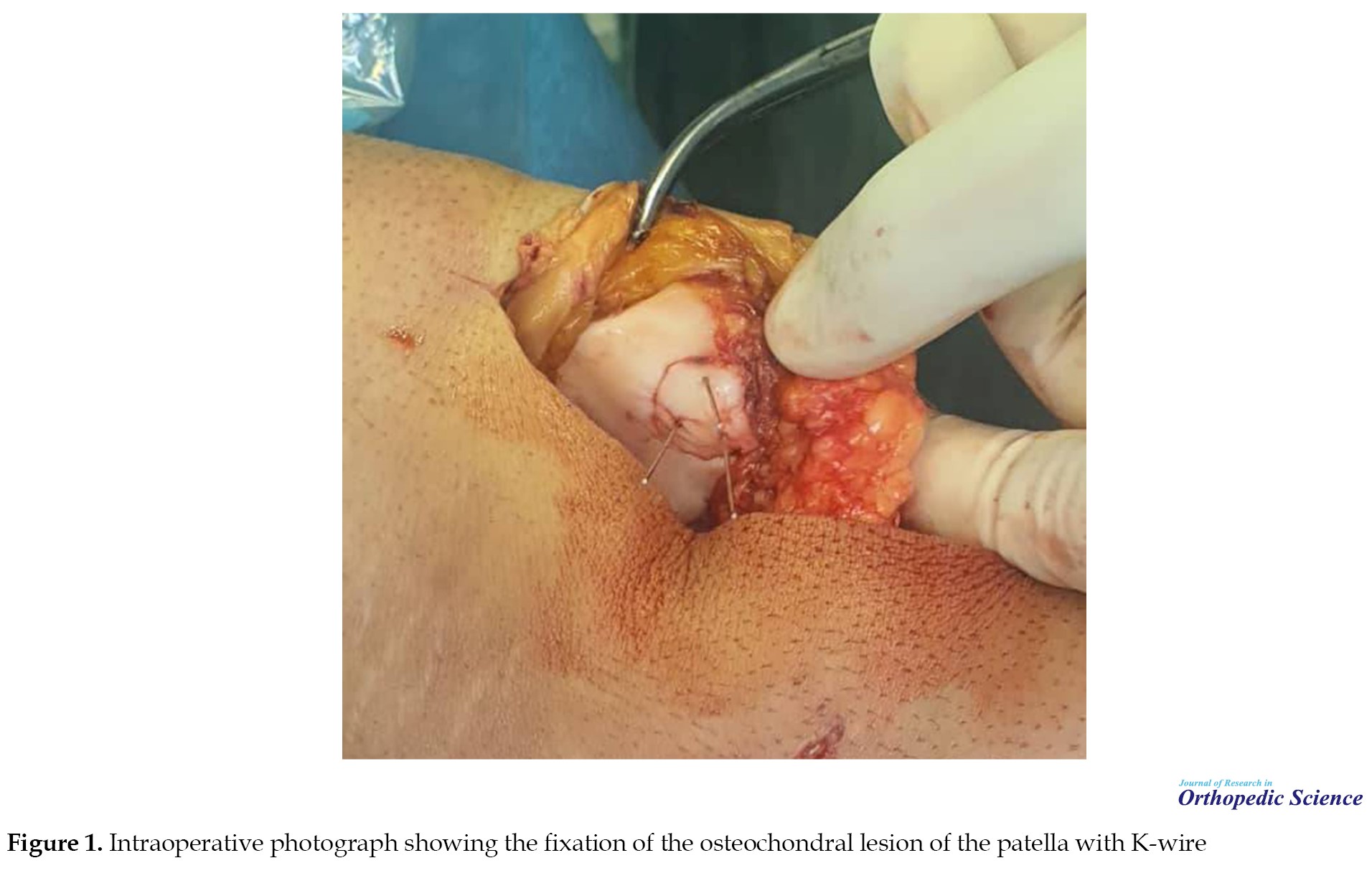
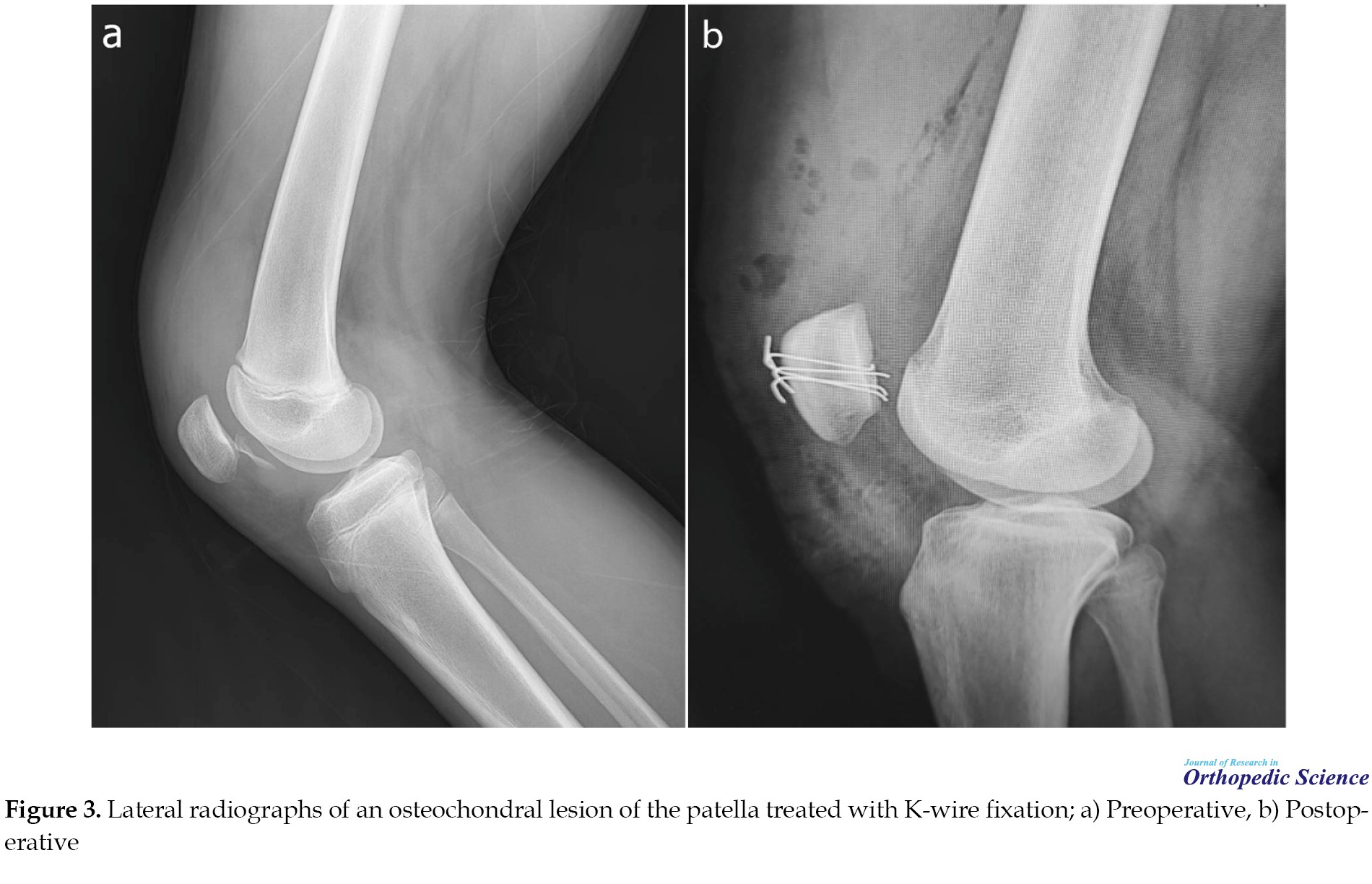
A single senior knee surgeon performed all surgical procedures. Arthroscopic evaluation of the lesion was performed for all cases. If the diagnosis was consistent with that observed on knee radiographs and magnetic resonance imaging (MRI), joint arthrotomy was performed through a midline skin incision. Irrigation and curettage were performed after anteromedial arthrotomy and lesion exploration. After that, the lesion was fixed with an adequate number and size of K-wire (0.5-2 mm in diameter), according to the size of the fragment. Inside the joint, the K-wire was bent on the cartilage surface, and outside the joint, and it was cut and bent near the cortex. The K-wires were tilted at an angle of approximately 45° to facilitate extraction (Figures 1, 2 and 3). Postoperatively, the knee was immobilized in a knee cast for one month. Knee range of motion was subsequently initiated. The wires were removed three months after surgery in the operating room and under sedation. For this purpose, the wires were located with a small incision over the cortex without opening the joint.
Data measurements
Patient demographic information was obtained from medical profiles. Postoperative complications were identified from patients’ medical records. Knee function was assessed using three separate questionnaires: The knee injury and osteoarthritis outcome score (KOOS), the International Knee Documentation Committee (IKDC) score, and the Lysholm knee scoring scale. All the questionnaires were scored on a 0-100 scale, with a higher score representing less disability and better function. Lysholm scores were also categorized into excellent (score of 95-100), good (84-94), fair (65-83), and poor (<65) outcomes.
Results
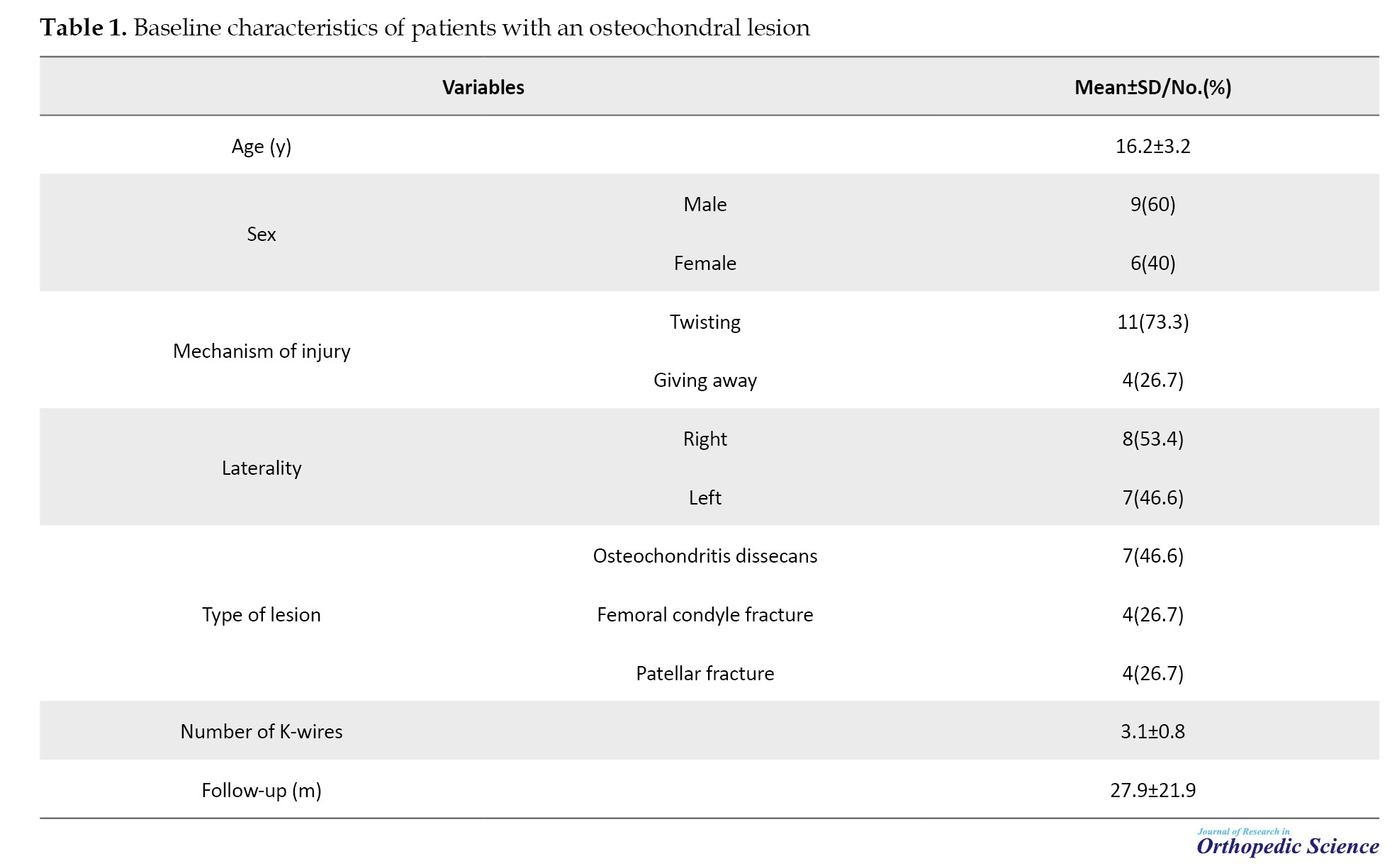
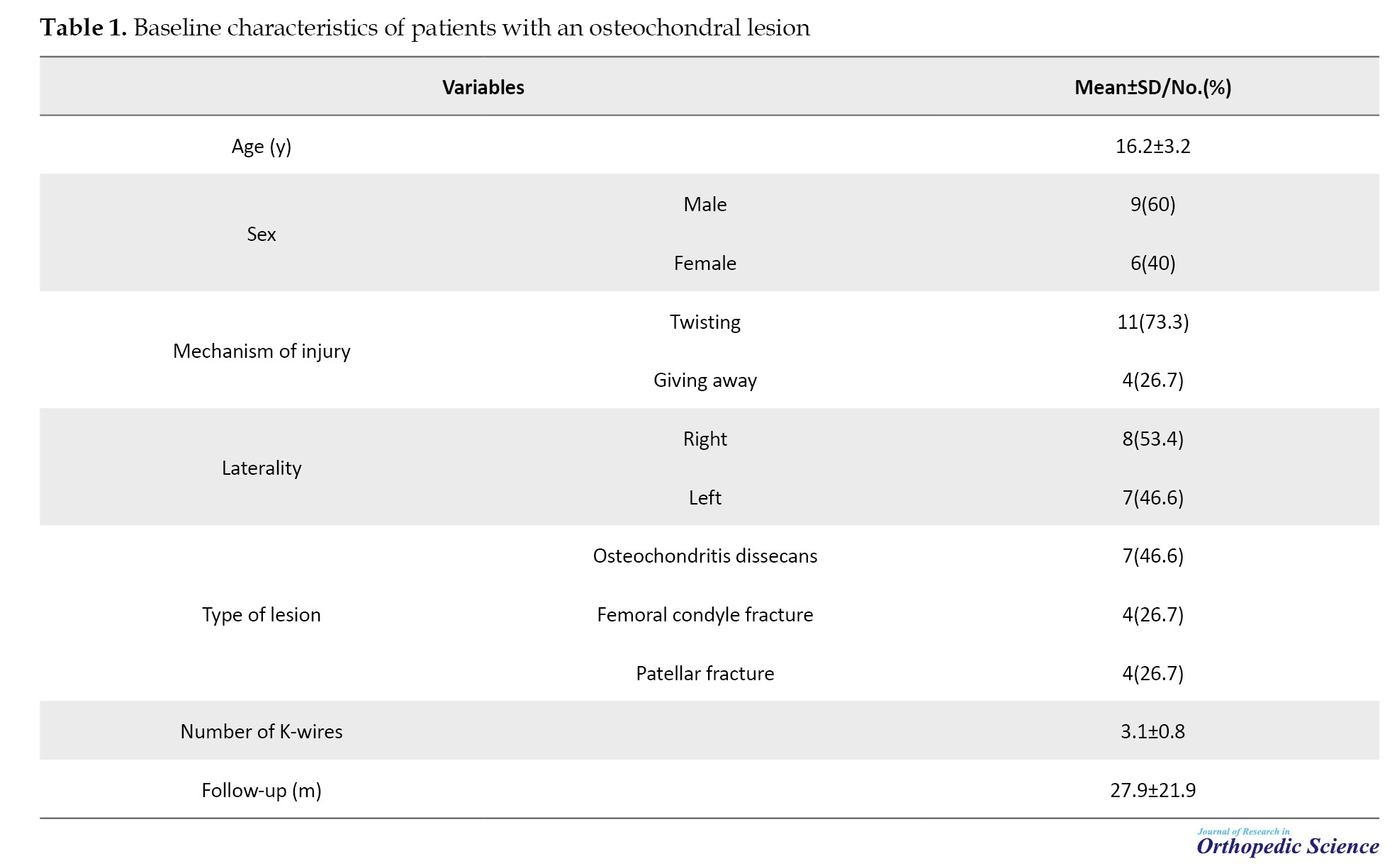
Fifteen patients who underwent K-wire fixation for osteochondral lesions were evaluated in this study. The etiology of the osteochondral lesion was osteochondritis dissecans in seven cases, the femoral condyle fracture in four cases, and the osteochondral lesion of the patella in four cases. The study population included nine males and six females, averaging 16.2±3.2 years (range: 11-23). The mechanism of injury was twisted in 11 patients and removed in four patients. The mean number of used K-wires was 3.1±0.8 (range: 2-5). The patients had a mean follow-up of 27.9±21.9 months (range: 12-81). Table 1 presents a more detailed summary of patients’ baseline characteristics.
The mean KOOS score was 95.7±5.5 (range: 85-100). The mean IKDC score was 95.9±8.3 (range: 71.6-100). The mean Lysholm knee score was 96.7±4.9 (range: 85-100). According to the Lysholm knee scoring scale, knee function was excellent in 11 patients and suitable in four cases. None of the patients had a fair or poor outcome.
Postoperative complications
Non:union: was observed in a patient treated for osteochondritis dissecans. Mosaicplasty was indicated for the patient. However, the patient refused to undergo this procedure. One patient required manipulation under anesthesia. No other postoperative complications were observed.
Discussion
In this study, we assessed the effectiveness of K-wires in knee osteochondral lesion fixation. Our analysis revealed that K-wire fixation provided excellent patient-reported outcomes in most patients and was associated with a limited number of postoperative complications. Therefore, it can be considered a viable alternative for absorbable and non-absorbable fixation devices because it is inexpensive and widely available in most orthopedic centers. Meanwhile, its extraction is much easier than traditional headless screws.
Historically, K-wires have been utilized for the fixation of osteochondral lesions of the knee [11]. Later, metal compression screws, such as Herbert headless screws, were used instead of K-wires. Barrett et al. studied the results of metal screw fixation for the treatment of 22 cases of unstable osteochondritis dissecans. The mean follow-up duration was 8.7 years. Fragment :union: was observed in 18 of 22 patients (82%). The mean postoperative IKDC and KOOS scores were 85 and 87, respectively [7]. Wang et al. investigated the results of Herbert screw fixation in the treatment of eight patients with osteochondritis dissecans. Seven of eight cases had good to excellent results with an average of 30.1 months follow-up [12]. Johnson et al. evaluated the results of osteochondritis dissecans in 35 knees treated with cannulated AO-type screws through an arthroscopic technique. The results were good or excellent in 90% of cases [13]. Several other studies have also reported acceptable outcomes of metal screw fixation in treating osteochondral knee lesions [14-17].
More recently, biodegradable screws have attracted attention for the fixation of osteochondral lesions because they do not require a second procedure for implant removal. Wiktor and Tomaszewski systematically reviewed the role of biodegradable implants in treating osteochondritis dissecans in children and adults. Eleven studies, including 164 OCD osteochondritis dissecans in 158 patients, were included in this review. Complete healing of lesions was observed in 94.86% of cases [18]. Nuelle et al. also reported the effectiveness of bioabsorbable screw fixation for traumatic osteochondral lesions of the patella [19]. However, few promising results have been reported. Millington et al. assessed the results of the treatment of unstable osteochondritis dissecans in 18 knees using bioabsorbable fixation devices, such as nails, pins, darts, and screws. The mean IKDC and Kysholm knee scale scores were 82 and 85, respectively, during 59 months of follow-up. In 12 patients, fragment :union: was observed (67%), while the remaining six patients required loose fragment removal surgery. In addition, two patients required reoperation for nail break-out [8]. Scioscia et al. considered unpredictable and inconsistent degradation of bioabsorbable screws as the reason for screw backout and cartilage damage [20]. Friederichs et al. also stated that the quick degradation of bioabsorbable implants cannot be relied upon [21].
In a systematic review, Leland et al. evaluated the results of internal fixation using various devices to manage unstable osteochondritis dissecans. Thirteen studies involving 158 patients (160 knees) were included in this review. Radiographic :union: was obtained in 67%-100% of patients. Reoperation was a typical scenario, so up to 44% of patients required reoperation, mainly to remove loose body fragments [10]. The different :union: and reoperation rates can be attributed to various confounding factors, including defect size [3].
Compared to the results of metal screws and bioabsorbable implants, the use of K-wire in the present study provided acceptable results in the management of osteochondral lesions of the knee. In this study, we observed only one fragment non-:union: (6.7%). The mean IKDC, KOOS, and Lysholm knee scores were 95.9, 95.7, and 96.7, respectively. Only one patient required reoperation.
Conclusion
K-wire fixation provides favorable patient-reported outcomes for the treatment of knee osteochondral lesions. It is also associated with a high radiographic healing rate and a low rate of postoperative complications and reoperation. Compared to biodegradable implants, it costs much less, and compared to metal screws, it does not require a second surgery for screw removal. Therefore, it can be regarded as a viable option for managing osteochondral lesions of the knee.
This study has some limitations. The principal limitation of this study was its retrospective design and limited sample size. The heterogeneous etiology of osteochondral lesions and the short follow-up period can be regarded as limitations of other studies. Therefore, these results need to be confirmed in future complementary studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1401.1015).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Mahmoud Jabalameli; Supervision: Abolfazl Bagherifard; Data collection and analysis: Shadi Alsamori; Writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
Osteochondral lesions of the knee are common among adolescent populations and can result from primary traumatic osteochondral fracture or secondary to osteochondritis dissecans [1, 2]. Several factors, including lesion size, stability, and symptom severity, influence these lesions’ treatment. Accordingly, managing these lesions includes a range of procedures from fixation to microfracture/marrow stimulation and autograft/allograft implantation [3-6].
Surgical fixation is preferred for treating osteochondral lesions because it perfectly restores the native articular surface [3]. Various fixation methods are available for this purpose. Metal implants, such as headless screws and biodegradable implants, are routinely used for the fixation of osteochondral lesions, both of which have demonstrated acceptable radiographic healing [7, 8]. Bioabsorbable implants are considered a viable alternative to metal implants because they obviate the need for a second procedure for implant removal. However, bioabsorbable screws are more expensive than conventional implants; therefore, they are not available in many orthopedic centers, particularly in developing countries [9]. In addition, both bioabsorbable and non-bioabsorbable screws have been associated with a high reoperation rate of up to 44% in systematic evaluation [10]. Therefore, developing affordable fixation methods that provide the same or superior outcomes to the available methods while being easily removable is of significant value.
Methods
The medical history of patients with osteochondral lesions of the knee managed with surgical fixation between 2015 and 2020 was retrospectively evaluated. The inclusion criteria included surgical treatment in the acute phase of injury, fixation with K-wire, and a minimum one-year follow-up period. The exclusion criteria included patients with a history of fracture, surgery of the ipsilateral knee, or associated knee injuries. Twenty-one patients met the study requirements, of whom 15 were eligible for the final evaluation and inclusion.
Surgical procedure
A single senior knee surgeon performed all surgical procedures. Arthroscopic evaluation of the lesion was performed for all cases. If the diagnosis was consistent with that observed on knee radiographs and magnetic resonance imaging (MRI), joint arthrotomy was performed through a midline skin incision. Irrigation and curettage were performed after anteromedial arthrotomy and lesion exploration. After that, the lesion was fixed with an adequate number and size of K-wire (0.5-2 mm in diameter), according to the size of the fragment. Inside the joint, the K-wire was bent on the cartilage surface, and outside the joint, and it was cut and bent near the cortex. The K-wires were tilted at an angle of approximately 45° to facilitate extraction (Figures 1, 2 and 3). Postoperatively, the knee was immobilized in a knee cast for one month. Knee range of motion was subsequently initiated. The wires were removed three months after surgery in the operating room and under sedation. For this purpose, the wires were located with a small incision over the cortex without opening the joint.
Data measurements
Patient demographic information was obtained from medical profiles. Postoperative complications were identified from patients’ medical records. Knee function was assessed using three separate questionnaires: The knee injury and osteoarthritis outcome score (KOOS), the International Knee Documentation Committee (IKDC) score, and the Lysholm knee scoring scale. All the questionnaires were scored on a 0-100 scale, with a higher score representing less disability and better function. Lysholm scores were also categorized into excellent (score of 95-100), good (84-94), fair (65-83), and poor (<65) outcomes.
Results
Fifteen patients who underwent K-wire fixation for osteochondral lesions were evaluated in this study. The etiology of the osteochondral lesion was osteochondritis dissecans in seven cases, the femoral condyle fracture in four cases, and the osteochondral lesion of the patella in four cases. The study population included nine males and six females, averaging 16.2±3.2 years (range: 11-23). The mechanism of injury was twisted in 11 patients and removed in four patients. The mean number of used K-wires was 3.1±0.8 (range: 2-5). The patients had a mean follow-up of 27.9±21.9 months (range: 12-81). Table 1 presents a more detailed summary of patients’ baseline characteristics.
The mean KOOS score was 95.7±5.5 (range: 85-100). The mean IKDC score was 95.9±8.3 (range: 71.6-100). The mean Lysholm knee score was 96.7±4.9 (range: 85-100). According to the Lysholm knee scoring scale, knee function was excellent in 11 patients and suitable in four cases. None of the patients had a fair or poor outcome.
Postoperative complications
Non:union: was observed in a patient treated for osteochondritis dissecans. Mosaicplasty was indicated for the patient. However, the patient refused to undergo this procedure. One patient required manipulation under anesthesia. No other postoperative complications were observed.
Discussion
In this study, we assessed the effectiveness of K-wires in knee osteochondral lesion fixation. Our analysis revealed that K-wire fixation provided excellent patient-reported outcomes in most patients and was associated with a limited number of postoperative complications. Therefore, it can be considered a viable alternative for absorbable and non-absorbable fixation devices because it is inexpensive and widely available in most orthopedic centers. Meanwhile, its extraction is much easier than traditional headless screws.
Historically, K-wires have been utilized for the fixation of osteochondral lesions of the knee [11]. Later, metal compression screws, such as Herbert headless screws, were used instead of K-wires. Barrett et al. studied the results of metal screw fixation for the treatment of 22 cases of unstable osteochondritis dissecans. The mean follow-up duration was 8.7 years. Fragment :union: was observed in 18 of 22 patients (82%). The mean postoperative IKDC and KOOS scores were 85 and 87, respectively [7]. Wang et al. investigated the results of Herbert screw fixation in the treatment of eight patients with osteochondritis dissecans. Seven of eight cases had good to excellent results with an average of 30.1 months follow-up [12]. Johnson et al. evaluated the results of osteochondritis dissecans in 35 knees treated with cannulated AO-type screws through an arthroscopic technique. The results were good or excellent in 90% of cases [13]. Several other studies have also reported acceptable outcomes of metal screw fixation in treating osteochondral knee lesions [14-17].
More recently, biodegradable screws have attracted attention for the fixation of osteochondral lesions because they do not require a second procedure for implant removal. Wiktor and Tomaszewski systematically reviewed the role of biodegradable implants in treating osteochondritis dissecans in children and adults. Eleven studies, including 164 OCD osteochondritis dissecans in 158 patients, were included in this review. Complete healing of lesions was observed in 94.86% of cases [18]. Nuelle et al. also reported the effectiveness of bioabsorbable screw fixation for traumatic osteochondral lesions of the patella [19]. However, few promising results have been reported. Millington et al. assessed the results of the treatment of unstable osteochondritis dissecans in 18 knees using bioabsorbable fixation devices, such as nails, pins, darts, and screws. The mean IKDC and Kysholm knee scale scores were 82 and 85, respectively, during 59 months of follow-up. In 12 patients, fragment :union: was observed (67%), while the remaining six patients required loose fragment removal surgery. In addition, two patients required reoperation for nail break-out [8]. Scioscia et al. considered unpredictable and inconsistent degradation of bioabsorbable screws as the reason for screw backout and cartilage damage [20]. Friederichs et al. also stated that the quick degradation of bioabsorbable implants cannot be relied upon [21].
In a systematic review, Leland et al. evaluated the results of internal fixation using various devices to manage unstable osteochondritis dissecans. Thirteen studies involving 158 patients (160 knees) were included in this review. Radiographic :union: was obtained in 67%-100% of patients. Reoperation was a typical scenario, so up to 44% of patients required reoperation, mainly to remove loose body fragments [10]. The different :union: and reoperation rates can be attributed to various confounding factors, including defect size [3].
Compared to the results of metal screws and bioabsorbable implants, the use of K-wire in the present study provided acceptable results in the management of osteochondral lesions of the knee. In this study, we observed only one fragment non-:union: (6.7%). The mean IKDC, KOOS, and Lysholm knee scores were 95.9, 95.7, and 96.7, respectively. Only one patient required reoperation.
Conclusion
K-wire fixation provides favorable patient-reported outcomes for the treatment of knee osteochondral lesions. It is also associated with a high radiographic healing rate and a low rate of postoperative complications and reoperation. Compared to biodegradable implants, it costs much less, and compared to metal screws, it does not require a second surgery for screw removal. Therefore, it can be regarded as a viable option for managing osteochondral lesions of the knee.
This study has some limitations. The principal limitation of this study was its retrospective design and limited sample size. The heterogeneous etiology of osteochondral lesions and the short follow-up period can be regarded as limitations of other studies. Therefore, these results need to be confirmed in future complementary studies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1401.1015).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Mahmoud Jabalameli; Supervision: Abolfazl Bagherifard; Data collection and analysis: Shadi Alsamori; Writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
References
- Gorbachova T, Melenevsky Y, Cohen M, Cerniglia BW. Osteochondral lesions of the knee: Differentiating the most common entities at MRI. Radiographics. 2018; 38(5):1478-95. [DOI:10.1148/rg.2018180044] [PMID]
- Bruns J, Werner M, Habermann C. Osteochondritis dissecans: Etiology, pathology, and imaging with a special focus on the knee joint. Cartilage. 2018; 9(4):346-62. [DOI:10.1177/1947603517715736] [PMID] [PMCID]
- Howell M, Liao Q, Gee CW. Surgical management of osteochondral defects of the knee: An educational review. Curr Rev Musculoskelet Med. 2021; 14(1):60-6. [DOI:10.1007/s12178-020-09685-1] [PMID] [PMCID]
- Gracitelli GC, Meric G, Pulido PA, McCauley JC, Bugbee WD. Osteochondral allograft transplantation for knee lesions after failure of cartilage repair surgery. Cartilage. 2015; 6(2):98-105. [DOI:10.1177/1947603514566298] [PMID] [PMCID]
- Angele P, Zellner J, Schröter S, Flechtenmacher J, Fritz J, Niemeyer P. Biological reconstruction of localized full-thickness cartilage defects of the knee: A systematic review of level 1 studies with a minimum follow-up of 5 years. Cartilage. 2022; 13(4):5-18. [DOI:10.1177/19476035221129571] [PMID] [PMCID]
- Moyad TF. Cartilage injuries in the adult knee: Evaluation and management. Cartilage. 2011; 2(3):226-36. [DOI:10.1177/1947603510383973] [PMID] [PMCID]
- Barrett I, King AH, Riester S, van Wijnen A, Levy BA, Stuart MJ, et al. Internal fixation of unstable osteochondritis dissecans in the skeletally mature knee with metal screws. Cartilage. 2016; 7(2):157-62. [DOI:10.1177/1947603515622662] [PMID] [PMCID]
- Millington KL, Shah JP, Dahm DL, Levy BA, Stuart MJ. Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am J Sports Med. 2010; 38(10):2065-70. [DOI:10.1177/0363546510371369] [PMID]
- Debieux P, Franciozi CE, Lenza M, Tamaoki MJ, Magnussen RA, Faloppa F, et al. Bioabsorbable versus metallic interference screws for graft fixation in anterior cruciate ligament reconstruction. Cochrane Database Syst Rev. 2016; 7(7):CD009772. [DOI:10.1002/14651858.CD009772.pub2] [PMID] [PMCID]
- Leland DP, Bernard CD, Camp CL, Nakamura N, Saris DBF, Krych AJ. Does internal fixation for unstable osteochondritis dissecans of the skeletally mature knee work? A systematic review. Arthroscopy. 2019; 35(8):2512-22. [DOI:10.1016/j.arthro.2019.03.020] [PMID]
- Scott DJ Jr, Stevenson CA. Osteochondritis dissecans of the knee in adults. Clin Orthop Relat Res. 1971; 76:82-6. [DOI:10.1097/00003086-197105000-00012] [PMID]
- Wang TI, Huang TF, Hung SC, Jiang ER, Ma HL, Liu CL. Functional outcome of surgical treatment for knee osteochondritis dissecans with Herbert screw. Formosan J Surg. 2011; 44(4):146-50. [DOI:10.1016/j.fjs.2011.08.009]
- Johnson LL, Uitvlugt G, Austin MD, Detrisac DA, Johnson C. Osteochondritis dissecans of the knee: Arthroscopic compression screw fixation. Arthroscopy. 1990; 6(3):179-89. [DOI:10.1016/0749-8063(90)90073-M] [PMID]
- Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M. Arthroscopic fixation of osteochondritis dissecans of the knee: Clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005; 33(10):1499-504. [DOI:10.1177/0363546505274717] [PMID]
- O'Connor MA, Palaniappan M, Khan N, Bruce CE. Osteochondritis dissecans of the knee in children. A comparison of MRI and arthroscopic findings. J Bone Joint Surg Br. 2002; 84(2):258-62. [DOI:10.1302/0301-620X.84B2.0840258] [PMID]
- Perelli S, Molina Romoli AR, Costa-Paz M, Erquicia JI, Gelber PE, Monllau JC. Internal fixation of osteochondritis dissecans of the knee leads to good long-term outcomes and high degree of healing without differences between fixation devices. J Clin Med. 2019; 8(11):1934. [DOI:10.3390/jcm8111934] [PMID] [PMCID]
- Wang X, Teng X, Cong L, Zhou X, Ma Z. Herbert screw internal fixation for treating adult osteochondritis dissecans of the knees. Chinese J Tissue Eng Res. 2021; 25(3):397. [DOI:10.3969/j.issn.2095-4344.2988]
- Wiktor Ł, Tomaszewski R. Evaluation of osteochondritis dissecans treatment with bioabsorbable implants in children and adolescents. J Clin Med. 2022; 11(18):5395. [DOI:10.3390/jcm11185395] [PMID] [PMCID]
- Nuelle CW, Nuelle JAV, Balldin BC. Open reduction internal fixation of a traumatic osteochondral lesion of the patella with bioabsorbable screw fixation. Arthrosc Tech. 2019; 8(11):e1361-5. [DOI:10.1016/j.eats.2019.07.012] [PMID] [PMCID]
- Scioscia TN, Giffin JR, Allen CR, Harner CD. Potential complication of bioabsorbable screw fixation for osteochondritis dissecans of the knee. Arthroscopy. 2001; 17(2):E7. [DOI:10.1053/jars.2001.17995] [PMID]
- Friederichs MG, Greis PE, Burks RT. Pitfalls associated with fixation of osteochondritis dissecans fragments using bioabsorbable screws. Arthroscopy. 2001; 17(5):542-5. [DOI:10.1053/jars.2001.22397] [PMID]
Type of Study: Research Article |
Subject:
Knee surgery
Received: 2022/06/10 | Accepted: 2022/09/15 | Published: 2023/05/1
Received: 2022/06/10 | Accepted: 2022/09/15 | Published: 2023/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |