Volume 10, Issue 1 (2-2023)
JROS 2023, 10(1): 35-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Pahlevan Sabagh A, Behjat M, Niroomand M, Sobhani A, Amiri S, Soleimani N. Cosmetic Outcomes of Horizontal Mattress Suture in Open Carpal Tunnel Release Surgery. JROS 2023; 10 (1) :35-42
URL: http://jros.iums.ac.ir/article-1-2249-en.html
URL: http://jros.iums.ac.ir/article-1-2249-en.html
Alireza Pahlevan Sabagh1 

 , Morteza Behjat1
, Morteza Behjat1 

 , Mohammad Niroomand1
, Mohammad Niroomand1 

 , Amir Sobhani1
, Amir Sobhani1 

 , Shayan Amiri1
, Shayan Amiri1 

 , Naseh Soleimani1
, Naseh Soleimani1 




 , Morteza Behjat1
, Morteza Behjat1 

 , Mohammad Niroomand1
, Mohammad Niroomand1 

 , Amir Sobhani1
, Amir Sobhani1 

 , Shayan Amiri1
, Shayan Amiri1 

 , Naseh Soleimani1
, Naseh Soleimani1 


1- Department of Orthopedics, School of Medicine, Bone and Joint Reconstruction Research Center, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 549 kb]
(374 Downloads)
| Abstract (HTML) (948 Views)
Full-Text: (356 Views)
Introduction
Carpal tunnel syndrome (CTS) causes various clinical symptoms, including paresthesia, pain, and hypoesthesia [1]. The diagnosis of this disorder is based on taking a history and performing clinical examinations that include electromyography and nerve conduction studies [2, 3]. Its average annual incidence is estimated at 378 per 100000 people, with an average of 10% of women and 1% of men affecting this disorder [4]. Depending on the severity of the median nerve’s involvement, this treatment includes conservative therapy and surgery [5]. Median nerve release surgery is the primary treatment for most patients, especially those with moderate or severe nerve involvement, thenar muscle atrophy, and mild symptoms that have not responded to conservative therapy [6]. Surgery treatment involves incision through the transverse ligament, which improves the symptoms by increasing the carpal tunnel volume and reducing the nerve pressure. This is currently performed by open and endoscopic release [7].
After open carpal tunnel release (OCTR) surgery, the patients often face various problems such as scar sensitivity, pain, burning, tingling, hypertrophic scars, and wrist flexion contractures [8]. Scar sensitivity in carpal tunnel surgeries has been reported between 19% and 61%, and the cause is still not fully understood [9]. The horizontal mattress suture technique has been used in some studies to repair rotator cuff tendon tears [10, 11], meniscal tears [12, 13], and Achilles tendon repair [14]. Also, in a study to repair skin defects caused by Mohs surgeries, the horizontal mattress suture had better aesthetic results than single interrupted sutures and left smoother and flatter scars [15].
Considering the complications of scars in CTS patients after median nerve release surgery, in this study, we investigate the aesthetic results and the thickness and height of the scar and its pigmentation between two suturing techniques, the single interrupted method, and the horizontal mattress method.
Methods
Study design
The current study is a randomized controlled trial. It compared cosmetic outcomes between single interrupted and horizontal mattress sutures among CTS patients undergoing open median nerve release surgery in Rasool-Akram, Kasra, and Moheb-Kosar hospitals, Tehran, Iran, from September 2020 to October 2021. The Ethics Committee of the Iran University of Medical Sciences approved the study, informed and written consent was obtained, and the study was accomplished in the Department of Orthopedic Surgery at Iran University of Medical Sciences.
The patients who met the inclusion criteria were randomly divided into two groups one by one: After the nerve release surgery, in the first group, the skin of the incision was sutured using a single interrupted method, and in the second group, the skin of the surgical site was sutured using the horizontal mattress technique. Patients were followed up 6 months after surgery in the clinic by evaluating the scar of the wound site and its color and measuring its height and width. A caliper was used with an accuracy of 0.01 mm to measure the width and height of the scar. The measurement was done in such a way that for each scar, from both sides of the healthy skin, it moved towards the scar using a sensitive tool, and wherever the tool stopped (the difference between the level of the scar and the healthy skin) was considered a measurement point. For each scar, two points were determined, then the distance between these two points was estimated, and their average was considered as the height or width of the scar. The researcher who estimated the scar size was unaware of the type of suture. Scar pigmentation was evaluated qualitatively by an external observer unaware of the type of suture, based on clinical examinations using an eye scale. It was divided into three levels: Hyperpigmented, hypopigmented, and normal.
Technique of surgery
All patients who had indications for open surgery and met the inclusion criteria underwent surgery. Open CTS release surgery was performed by a hand surgeon (Dr Pahlevan Sabagh). After sterilization with alcohol and povidone-iodine, injection of a local anesthetic block was performed by a combination of 2% lidocaine and 1/100000 epinephrine after inflating the tourniquet. A longitudinal skin incision was made along the radial side of the ring finger and in such a way as not to cut the crease of the wrist flexor. The approximate length of the cut was 2 cm. Using scalpel 15, the distal and proximal cuts of the transverse carpal ligament were made, and the median nerve was released. The tourniquet was deflated, and local bleeding areas were checked. Then, the skin was sutured with three sutures using one of the single interrupted method or the horizontal mattress method, followed by a sterile pressure dressing that was applied for two days. The skin sutures were removed after 10 days.
Skin closure technique
After releasing the median nerve, the patients were randomly divided into two groups.
In group A (single interrupted technique), the superficial skin was approximated by single interrupted sutures, all of which have a single knot, applying 3-0 nonabsorbable polypropylene (Prolene, Ethicon, USA) with a tapered suture needle.
Also, in group B (horizontal mattress technique), the skin was approximated by a suture bite followed by an adjacent reverse bite helping wound eversion that uses 3-0 nonabsorbable polypropylene (Prolene, Ethicon, USA) with a cutting needle.
The inclusion criteria were as follows: Patients aged 18-80 years, a definitive diagnosis of CTS based on clinical findings and electrodiagnostic examination that is based on the diagnosis of an orthopedic specialist, patients with a follow-up of at least 6 months, and patients who have had at least 6 months of surgery.
The exclusion criteria were as follows: A positive history of open median nerve release surgery or a history of previous hand surgery, skin lesions or diseases; patients taking anticoagulants; complications at the surgical site, such as wound dehiscence, hematoma, infection, etc.; chronic diseases such as kidney and liver failure diseases, a history of hypertrophic scars, lack of cooperation or willingness to participate in the study; a history of severe peripheral vascular diseases that interfere with wound healing; and diabetic patients who had a history of heart attack or stroke, history of retinopathy or nephropathy, or diabetic foot ulcer.
Statistical analysis
After collecting information, all the data were analyzed using SPSS software, version 21. Descriptive results were presented as Mean±SD or number (percentage). The Shapiro-Wilk test was used to evaluate the normality of the data. The t-test was used to compare the quantitative variables in the two groups with the assumption of a normal distribution, and non-parametric Mann-Whitney tests were used if the distribution of the variables was not normal. The chi-square test was used to compare qualitative variables. A P<0.05 was considered significant.
The appropriate sample size of this study with an effect size estimation of 0.96 for the difference in making a more severe scar based on the study of BR Moody et al. [15], with an acceptable alpha error size of 5%, a confidence interval of 95%, and a study power of 80%, using SPSS software, the number of 24 patients were considered for each group. To increase the power of the study, the number of 30 patients in each group was evaluated.
Results
Demographic data
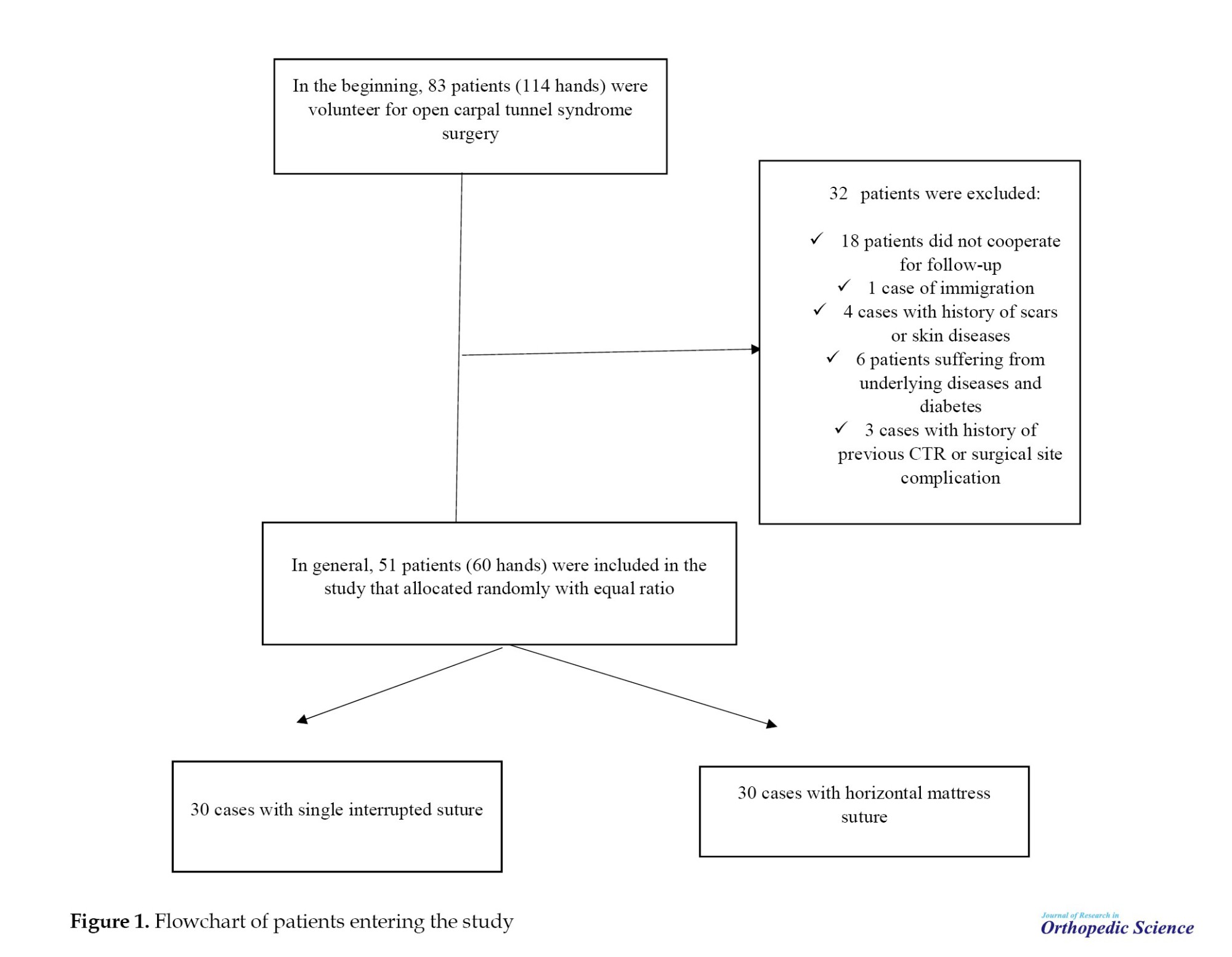
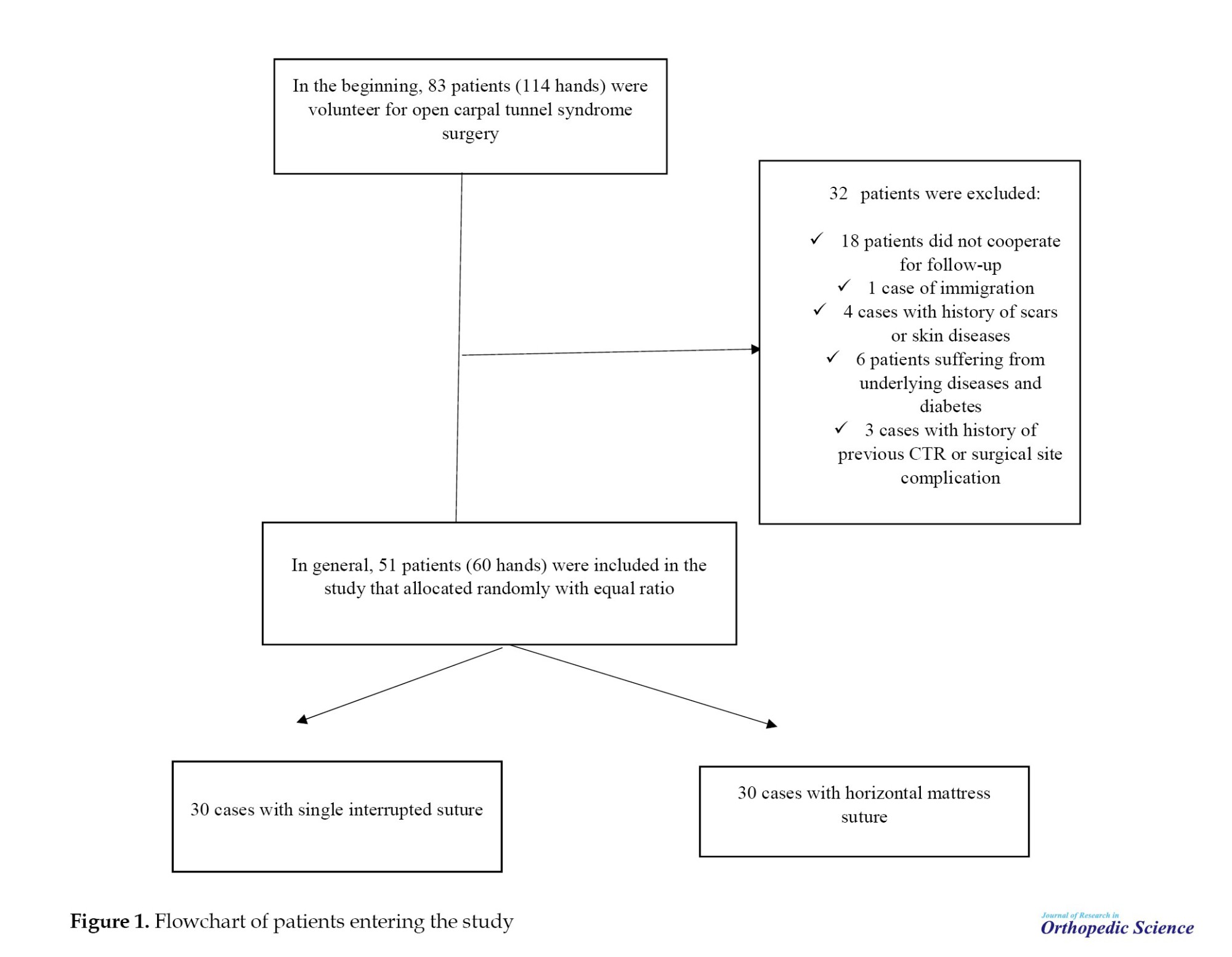
In this study, 83 patients, or 114 hands (31 bilateral patients and 52 unilateral patients), met the inclusion criteria as candidates for nerve-opening surgery. While 32 patients did not cooperate during the follow-up period and were excluded from the study.
Finally, 51 patients, or 60 hands, were included in the study. Among 9 patients, both left and right hands underwent median nerve release surgery. Between these groups, in 5 patients, one hand was closed with a single interrupted suture technique, and the opposite was closed with a horizontal mattress suture technique. However, in 4 patients, both hands were closed with the same method.
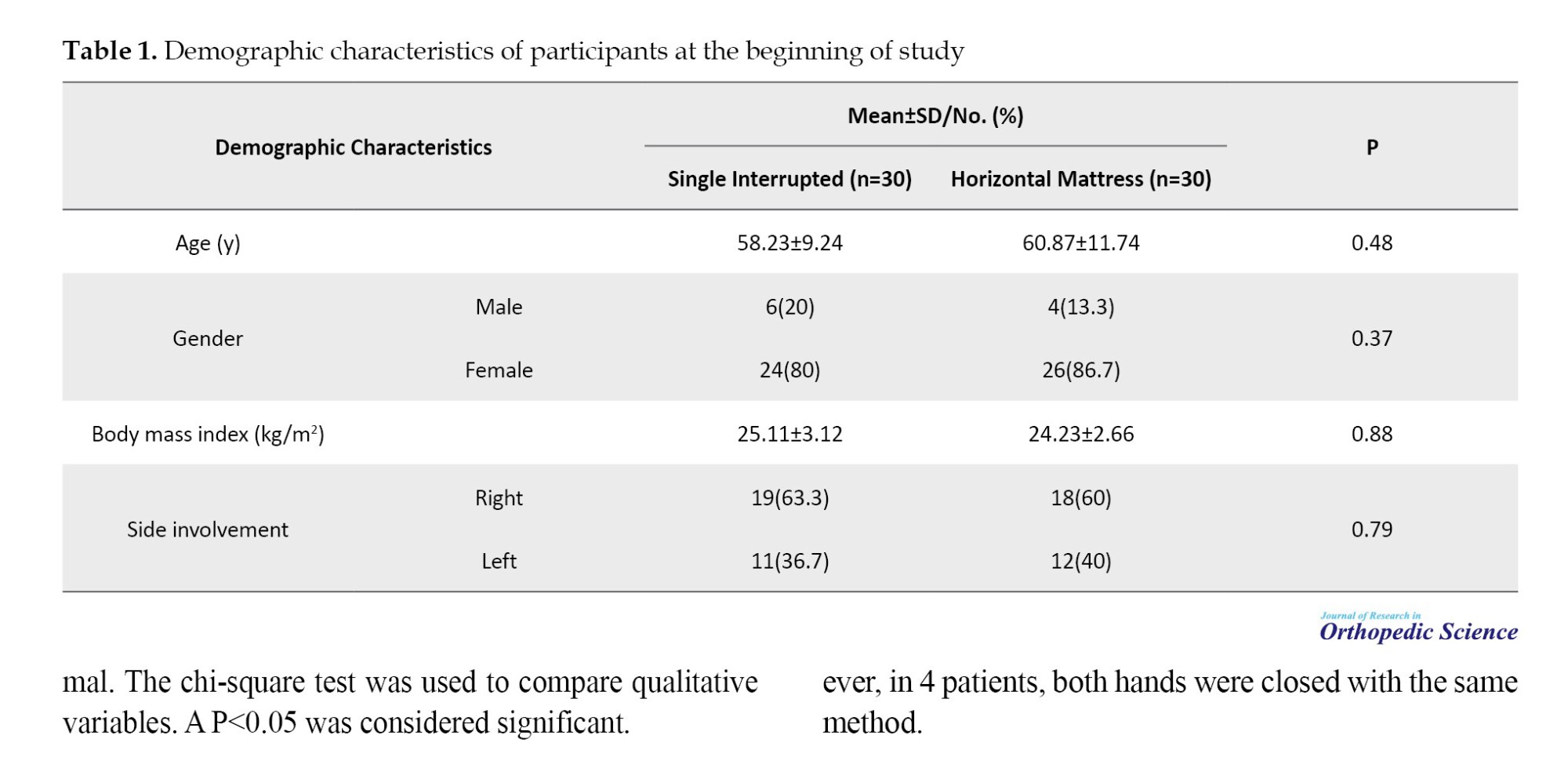
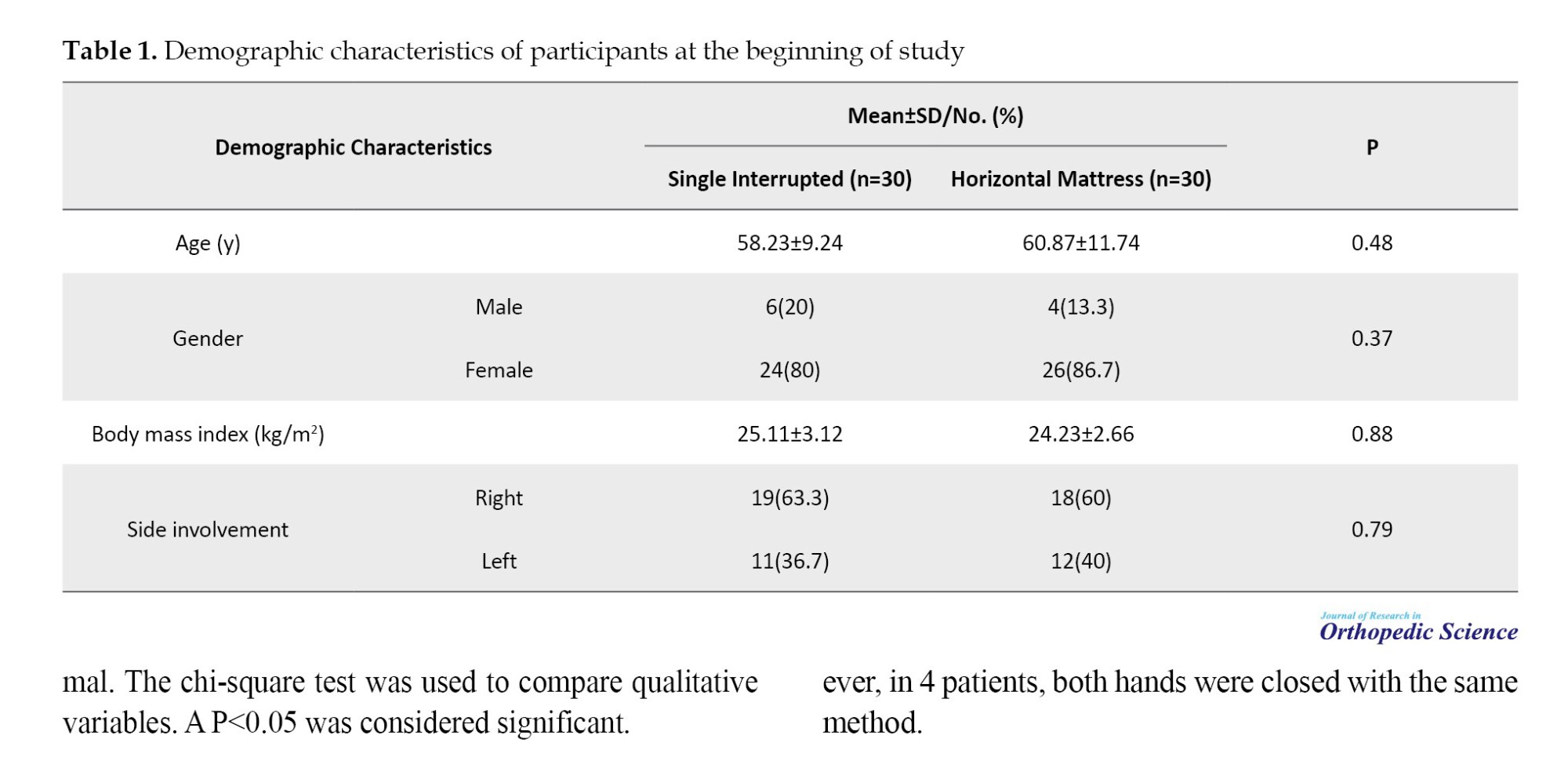
In the study population, 43 cases (84.3%) were women and 8 (15.7%) were men. The overall mean age of the patients was 59.75±11.54 years (37 to 83 years). The mean body mass index of the patients was 24.86±2.96 kg/m2. The right-hand nerve was generally involved in 61.6% of the cases. The age and gender distribution of patients in both groups at the beginning of the study were similar. No significant difference was reported for the distribution of demographic variables in the two groups at the start of the study (P>0.05) (Table 1).
Comparing scar findings
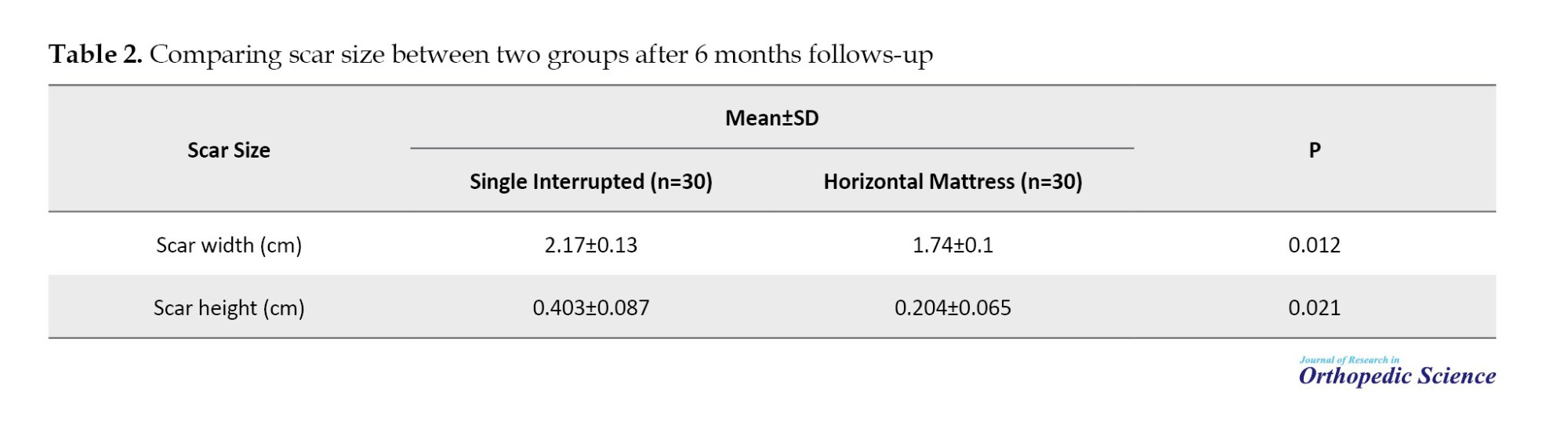
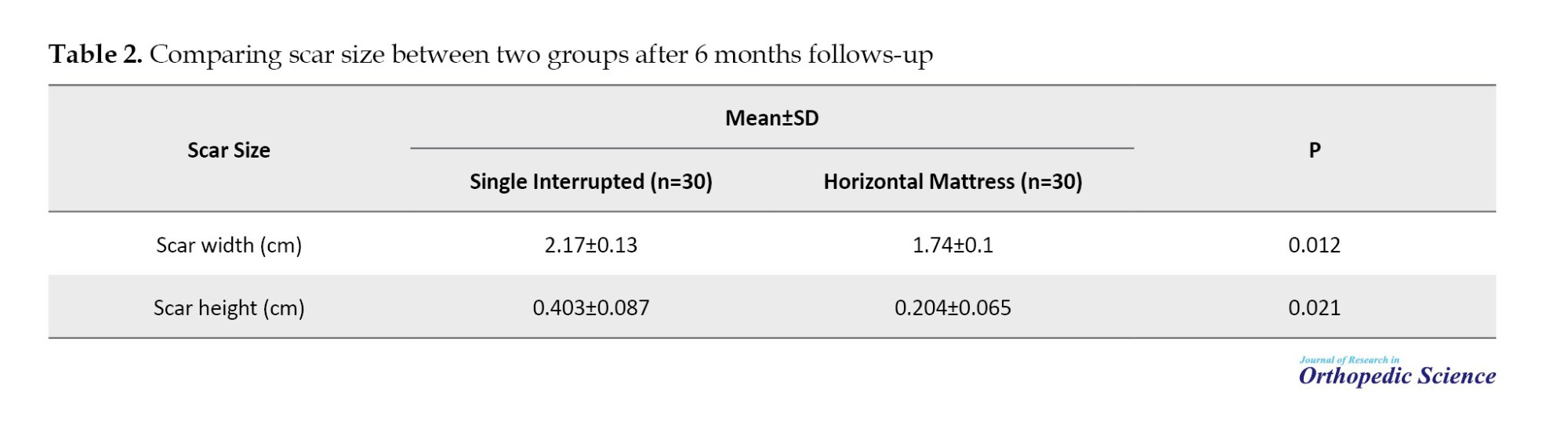
After 6 months of surgery, the mean scar width for patients in the horizontal mattress group (1.74±0.1 cm) was significantly lower than that of the single interrupted suture group (2.17±0.13 cm) (P=0.012). Also, the measured scar height 6 months after surgery in the horizontal mattress group (0.204±0.065 cm) was significantly lower than the single interrupted suture group (0.403±0.087 cm) (P=0.021) (Table 2).
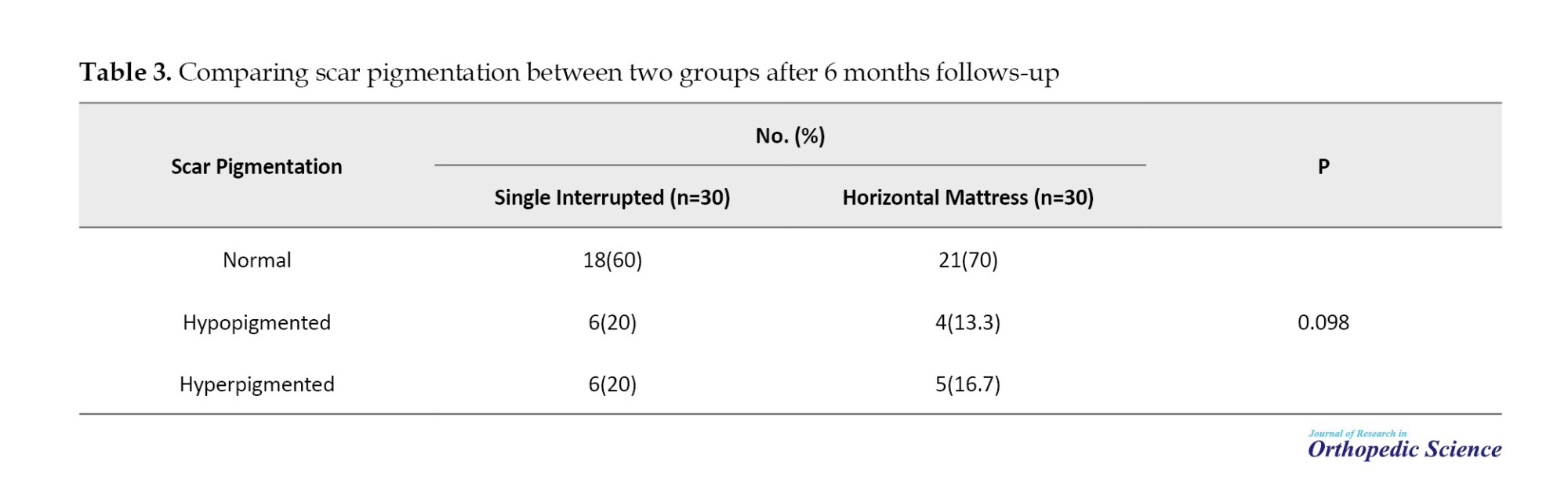
Comparing scar pigmentation
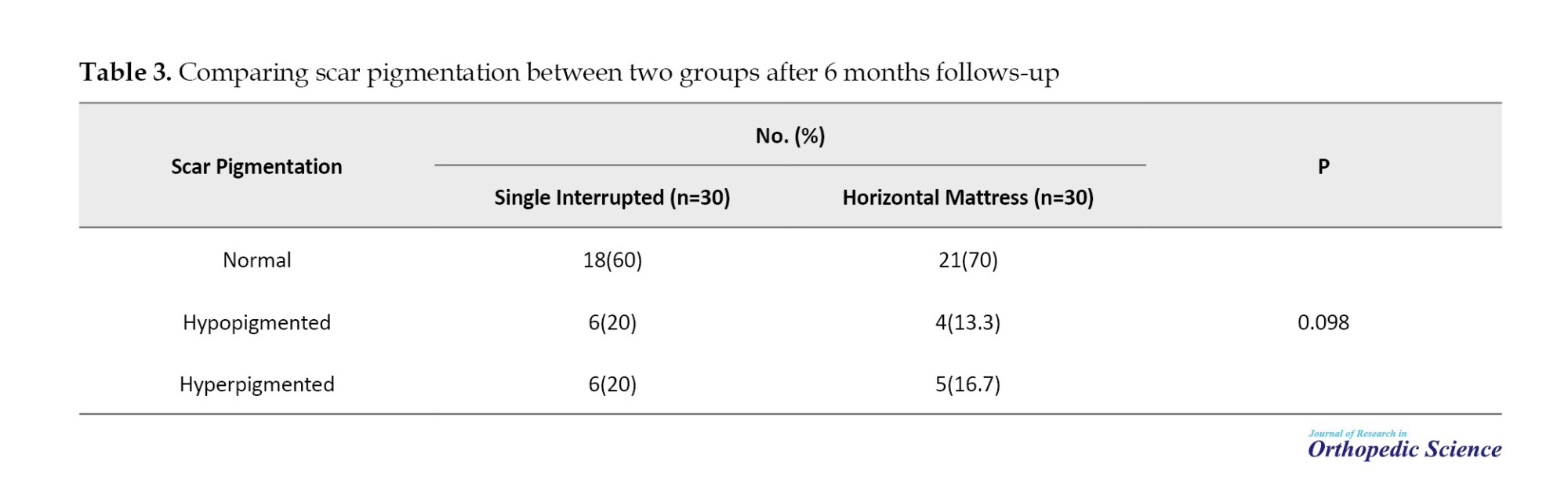
Based on the results of this comparison, although the frequency of people with hyperpigmentation scars in the horizontal mattress suture group was slightly lower than in the single interrupted suture group, this difference was not statistically significant (P=0.098) (Table 3).
Discussion
The present study compared the cosmetic results of scars between single interrupted suture and horizontal mattress techniques in carpal tunnel release surgery patients. Finally, it was determined that the height and width of the scar among the horizontal mattress group was significantly lower than the single interrupted suture group and showed better aesthetic outcomes 6 weeks postoperatively.
According to this study’s results, most patients were women. Similarly, in the Bolster et al. study, the female sex had a higher frequency. The overall mean age of the patients was 59.75 years (ranging from 37 to 83 years). Also, in the study of Bolster et al., the mean age was 55, and the age range was from 24 to 81 years, which is similar to the present study. In most patients, the nerve of the right hand was involved and underwent surgery; the percentage of right-side involvement in the study of Bolster et al. was approximately 61% [16]. No significant difference was observed in the distribution of demographic variables between the two groups at the beginning of the study, and the two groups had a completely homogeneous distribution.
After 6 months of surgery, the mean scar width and height for patients whose wound was closed with the horizontal mattress technique after open surgery were significantly less than the group of patients whose wounds were closed with the single interrupted suture. The visual evaluation of the scar demonstrated that the horizontal mattress method had a better cosmetic outcome. Still, there was no significant difference in the degree of hyperpigmentation between the two groups. Bolster et al. (2013) evaluated and compared the aesthetic effects of two types of single interrupted and Donati stitches (vertical mattress stitches) for skin closure in open carpal tunnel surgery. In this study, both sutures were associated with the formation of appropriate scars and a high level of patient satisfaction, and no difference was observed between the two groups. Based on the qualitative classification of patients’ scars, the percentage of good or excellent groups in appearance was 94% and 97% in single interrupted and Donati sutures, respectively [16]. In the present study, the horizontal mattress sutures showed less scar height and width than the single interrupted suture group. One of the reasons for this difference is the comparison of surgical site scars using a qualitative method, not quantitative and precise criteria in the Bolster study.
Moody et al. compared the scars of two techniques of sutures, horizontal mattress and single interrupted running, in 47 patients who underwent Mohs facial surgery. They showed that the type of horizontal mattress suture had significantly better cosmetic results and a smoother and flatter scar than the single interrupted suture [15]. Although these results were not performed on the wrist’s skin, they confirmed our study’s results. In their study, the upper or lower half of the incision was closed with a horizontal mattress suture and the other half with a single interrupted running suture. In contrast, in our study, in some bilateral cases, one wound was closed with a single interrupted suture, and the wound on the opposite side was closed with a horizontal mattress suture.
Meng et al. (2017) investigated the strength of horizontal mattress and vertical mattress sutures among in vitro skin flaps. Under laboratory conditions, skin flaps were pulled with increasing tensile force, and wound dehiscence was measured. Finally, it was declared that the horizontal mattress sutures displayed significantly less dehiscence under different stretching conditions, reducing the tension on the skin and subcutaneous tissue [17]. This finding was in line with the present study because a smaller scar size was produced in the horizontal mattress groups, which was caused by less tension and pressure on the skin.
The wound scar is usually related to the suture technique and material. To compare the type of thread and material used in terms of absorbable or nonabsorbable, many studies have been conducted for skin closure, including the studies of Erel et al. and Kharwadkar et al. that they had declared nonabsorbable sutures had more wound scar satisfaction and less inflammation than absorbable suture type [18, 19]. Also, Menovsky et al. compared the closure of open carpal tunnel surgical wounds using nylon, polyglactin 910, and stainless-steel sutures. They showed that the scar measures and pain were statistically more observed with Vicryl suture 6 weeks after surgery [20].
Wu et al. compared wound closure techniques using horizontal mattress with nylon and interrupted deep dermal with Monocryl among patients with CTS surgery. They demonstrated that the Monocryl (intradermal) group was significantly more satisfied with scars than the nylon (horizontal mattress) group in the 2-week postoperative follow-up, while no difference was observed between these two groups in the 6-week follow-up [21]. Also, Rochlin et al. observed that Monocryl sutures revealed a lower rate of wound-related complications, including infection and dehiscence, than nylon sutures [22]. In the current study, nylon sutures and the horizontal mattress method had better clinical results than single interrupted sutures in a 6-week postoperative visit, and no comparison was made between nylon sutures and Monocryl sutures that showed less wound and scar-related reactions in Monocryl sutures can justify the different clinical results between these studies.
Liu et al. (2021) examined the outcomes of modified buried vertical mattress suture (MBVMS) versus buried intradermal suture (BIS) in 20 patients’ chest wounds, of which half were randomly closed with MBVMS and the other half closed with the BIS method. They demonstrated that the mean height and width of the postoperative scar were lower with the MBVMS method. This study showed that the aesthetic results at the end of the follow-up period were significantly better with the MBVMS method than the BIS method [23]. Although this study’s method and technique differed from ours, it generally confirms that vertical and horizontal suture techniques can have better results than the single interrupted suture technique.
Conclusion
In general, this study demonstrated that applying a horizontal mattress suture can have better results than a single interrupted suture, so the scar formation after surgery and the scar size in this method were significantly lower than single interrupted sutures in patients undergoing median nerve release. This study declared that using the horizontal mattress method in patients undergoing median nerve release can be considered a technique with fewer complications and greater effectiveness after surgery. Comparing different types of stitches with varying thread types can be a good idea for further studies.
Coincidence with COVID-19 and a significant decrease in the number of patients, decreasing the power of the study was our main challenge, and this issue even affected the desire of patients to come back for follow-up visits. In the current study, there was only one postoperative visit for surveillance of wound and scar measurements. However, 6 months for scar assessment is not enough, and longer periods of clinic follow-up, like 1 year or 2 years, are necessary for the precise prediction of aesthetic complaints of patients from their scars and the challenging features of the horizontal mattress technique. Also, better evaluation of wound complications like infection and dehiscence is achieved in short-term visits, making them essential for the next studies. Bilateral patients, each side closed with one type of suture, are very suitable for accurately comparing these two sutures with minimal confounding factors. Still, the number of these cases in our study was small, which made it impossible to analyze them accurately. This problem was one of the restrictions of our research, and it can be considered in future studies. The most important strength of the present study was its design in the form of a randomized controlled clinical trial in patients undergoing Median nerve release surgery, as well as the accurate quantitative measurement of scar indicators due to the prospective nature of the study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.FMD.REC.1399.466). Also, written informed consent was obtained.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and methodology: Alireza Pahlevansabagh; Supervision and funding acquisition: Amir Sobhani; Software, validation and formal analysis: Mohammad Niroomand; Investigation and resources: Naseh Soleimani; Data curation, project administration, and writing the original draft: Morteza Behjat; Review, editing and visualization: Shayan Amiri.
Conflict of interest
The authors declared no conflict of interest.
References
Carpal tunnel syndrome (CTS) causes various clinical symptoms, including paresthesia, pain, and hypoesthesia [1]. The diagnosis of this disorder is based on taking a history and performing clinical examinations that include electromyography and nerve conduction studies [2, 3]. Its average annual incidence is estimated at 378 per 100000 people, with an average of 10% of women and 1% of men affecting this disorder [4]. Depending on the severity of the median nerve’s involvement, this treatment includes conservative therapy and surgery [5]. Median nerve release surgery is the primary treatment for most patients, especially those with moderate or severe nerve involvement, thenar muscle atrophy, and mild symptoms that have not responded to conservative therapy [6]. Surgery treatment involves incision through the transverse ligament, which improves the symptoms by increasing the carpal tunnel volume and reducing the nerve pressure. This is currently performed by open and endoscopic release [7].
After open carpal tunnel release (OCTR) surgery, the patients often face various problems such as scar sensitivity, pain, burning, tingling, hypertrophic scars, and wrist flexion contractures [8]. Scar sensitivity in carpal tunnel surgeries has been reported between 19% and 61%, and the cause is still not fully understood [9]. The horizontal mattress suture technique has been used in some studies to repair rotator cuff tendon tears [10, 11], meniscal tears [12, 13], and Achilles tendon repair [14]. Also, in a study to repair skin defects caused by Mohs surgeries, the horizontal mattress suture had better aesthetic results than single interrupted sutures and left smoother and flatter scars [15].
Considering the complications of scars in CTS patients after median nerve release surgery, in this study, we investigate the aesthetic results and the thickness and height of the scar and its pigmentation between two suturing techniques, the single interrupted method, and the horizontal mattress method.
Methods
Study design
The current study is a randomized controlled trial. It compared cosmetic outcomes between single interrupted and horizontal mattress sutures among CTS patients undergoing open median nerve release surgery in Rasool-Akram, Kasra, and Moheb-Kosar hospitals, Tehran, Iran, from September 2020 to October 2021. The Ethics Committee of the Iran University of Medical Sciences approved the study, informed and written consent was obtained, and the study was accomplished in the Department of Orthopedic Surgery at Iran University of Medical Sciences.
The patients who met the inclusion criteria were randomly divided into two groups one by one: After the nerve release surgery, in the first group, the skin of the incision was sutured using a single interrupted method, and in the second group, the skin of the surgical site was sutured using the horizontal mattress technique. Patients were followed up 6 months after surgery in the clinic by evaluating the scar of the wound site and its color and measuring its height and width. A caliper was used with an accuracy of 0.01 mm to measure the width and height of the scar. The measurement was done in such a way that for each scar, from both sides of the healthy skin, it moved towards the scar using a sensitive tool, and wherever the tool stopped (the difference between the level of the scar and the healthy skin) was considered a measurement point. For each scar, two points were determined, then the distance between these two points was estimated, and their average was considered as the height or width of the scar. The researcher who estimated the scar size was unaware of the type of suture. Scar pigmentation was evaluated qualitatively by an external observer unaware of the type of suture, based on clinical examinations using an eye scale. It was divided into three levels: Hyperpigmented, hypopigmented, and normal.
Technique of surgery
All patients who had indications for open surgery and met the inclusion criteria underwent surgery. Open CTS release surgery was performed by a hand surgeon (Dr Pahlevan Sabagh). After sterilization with alcohol and povidone-iodine, injection of a local anesthetic block was performed by a combination of 2% lidocaine and 1/100000 epinephrine after inflating the tourniquet. A longitudinal skin incision was made along the radial side of the ring finger and in such a way as not to cut the crease of the wrist flexor. The approximate length of the cut was 2 cm. Using scalpel 15, the distal and proximal cuts of the transverse carpal ligament were made, and the median nerve was released. The tourniquet was deflated, and local bleeding areas were checked. Then, the skin was sutured with three sutures using one of the single interrupted method or the horizontal mattress method, followed by a sterile pressure dressing that was applied for two days. The skin sutures were removed after 10 days.
Skin closure technique
After releasing the median nerve, the patients were randomly divided into two groups.
In group A (single interrupted technique), the superficial skin was approximated by single interrupted sutures, all of which have a single knot, applying 3-0 nonabsorbable polypropylene (Prolene, Ethicon, USA) with a tapered suture needle.
Also, in group B (horizontal mattress technique), the skin was approximated by a suture bite followed by an adjacent reverse bite helping wound eversion that uses 3-0 nonabsorbable polypropylene (Prolene, Ethicon, USA) with a cutting needle.
The inclusion criteria were as follows: Patients aged 18-80 years, a definitive diagnosis of CTS based on clinical findings and electrodiagnostic examination that is based on the diagnosis of an orthopedic specialist, patients with a follow-up of at least 6 months, and patients who have had at least 6 months of surgery.
The exclusion criteria were as follows: A positive history of open median nerve release surgery or a history of previous hand surgery, skin lesions or diseases; patients taking anticoagulants; complications at the surgical site, such as wound dehiscence, hematoma, infection, etc.; chronic diseases such as kidney and liver failure diseases, a history of hypertrophic scars, lack of cooperation or willingness to participate in the study; a history of severe peripheral vascular diseases that interfere with wound healing; and diabetic patients who had a history of heart attack or stroke, history of retinopathy or nephropathy, or diabetic foot ulcer.
Statistical analysis
After collecting information, all the data were analyzed using SPSS software, version 21. Descriptive results were presented as Mean±SD or number (percentage). The Shapiro-Wilk test was used to evaluate the normality of the data. The t-test was used to compare the quantitative variables in the two groups with the assumption of a normal distribution, and non-parametric Mann-Whitney tests were used if the distribution of the variables was not normal. The chi-square test was used to compare qualitative variables. A P<0.05 was considered significant.
The appropriate sample size of this study with an effect size estimation of 0.96 for the difference in making a more severe scar based on the study of BR Moody et al. [15], with an acceptable alpha error size of 5%, a confidence interval of 95%, and a study power of 80%, using SPSS software, the number of 24 patients were considered for each group. To increase the power of the study, the number of 30 patients in each group was evaluated.
Results
Demographic data
In this study, 83 patients, or 114 hands (31 bilateral patients and 52 unilateral patients), met the inclusion criteria as candidates for nerve-opening surgery. While 32 patients did not cooperate during the follow-up period and were excluded from the study.
Finally, 51 patients, or 60 hands, were included in the study. Among 9 patients, both left and right hands underwent median nerve release surgery. Between these groups, in 5 patients, one hand was closed with a single interrupted suture technique, and the opposite was closed with a horizontal mattress suture technique. However, in 4 patients, both hands were closed with the same method.
In the study population, 43 cases (84.3%) were women and 8 (15.7%) were men. The overall mean age of the patients was 59.75±11.54 years (37 to 83 years). The mean body mass index of the patients was 24.86±2.96 kg/m2. The right-hand nerve was generally involved in 61.6% of the cases. The age and gender distribution of patients in both groups at the beginning of the study were similar. No significant difference was reported for the distribution of demographic variables in the two groups at the start of the study (P>0.05) (Table 1).
Comparing scar findings
After 6 months of surgery, the mean scar width for patients in the horizontal mattress group (1.74±0.1 cm) was significantly lower than that of the single interrupted suture group (2.17±0.13 cm) (P=0.012). Also, the measured scar height 6 months after surgery in the horizontal mattress group (0.204±0.065 cm) was significantly lower than the single interrupted suture group (0.403±0.087 cm) (P=0.021) (Table 2).
Comparing scar pigmentation
Based on the results of this comparison, although the frequency of people with hyperpigmentation scars in the horizontal mattress suture group was slightly lower than in the single interrupted suture group, this difference was not statistically significant (P=0.098) (Table 3).
Discussion
The present study compared the cosmetic results of scars between single interrupted suture and horizontal mattress techniques in carpal tunnel release surgery patients. Finally, it was determined that the height and width of the scar among the horizontal mattress group was significantly lower than the single interrupted suture group and showed better aesthetic outcomes 6 weeks postoperatively.
According to this study’s results, most patients were women. Similarly, in the Bolster et al. study, the female sex had a higher frequency. The overall mean age of the patients was 59.75 years (ranging from 37 to 83 years). Also, in the study of Bolster et al., the mean age was 55, and the age range was from 24 to 81 years, which is similar to the present study. In most patients, the nerve of the right hand was involved and underwent surgery; the percentage of right-side involvement in the study of Bolster et al. was approximately 61% [16]. No significant difference was observed in the distribution of demographic variables between the two groups at the beginning of the study, and the two groups had a completely homogeneous distribution.
After 6 months of surgery, the mean scar width and height for patients whose wound was closed with the horizontal mattress technique after open surgery were significantly less than the group of patients whose wounds were closed with the single interrupted suture. The visual evaluation of the scar demonstrated that the horizontal mattress method had a better cosmetic outcome. Still, there was no significant difference in the degree of hyperpigmentation between the two groups. Bolster et al. (2013) evaluated and compared the aesthetic effects of two types of single interrupted and Donati stitches (vertical mattress stitches) for skin closure in open carpal tunnel surgery. In this study, both sutures were associated with the formation of appropriate scars and a high level of patient satisfaction, and no difference was observed between the two groups. Based on the qualitative classification of patients’ scars, the percentage of good or excellent groups in appearance was 94% and 97% in single interrupted and Donati sutures, respectively [16]. In the present study, the horizontal mattress sutures showed less scar height and width than the single interrupted suture group. One of the reasons for this difference is the comparison of surgical site scars using a qualitative method, not quantitative and precise criteria in the Bolster study.
Moody et al. compared the scars of two techniques of sutures, horizontal mattress and single interrupted running, in 47 patients who underwent Mohs facial surgery. They showed that the type of horizontal mattress suture had significantly better cosmetic results and a smoother and flatter scar than the single interrupted suture [15]. Although these results were not performed on the wrist’s skin, they confirmed our study’s results. In their study, the upper or lower half of the incision was closed with a horizontal mattress suture and the other half with a single interrupted running suture. In contrast, in our study, in some bilateral cases, one wound was closed with a single interrupted suture, and the wound on the opposite side was closed with a horizontal mattress suture.
Meng et al. (2017) investigated the strength of horizontal mattress and vertical mattress sutures among in vitro skin flaps. Under laboratory conditions, skin flaps were pulled with increasing tensile force, and wound dehiscence was measured. Finally, it was declared that the horizontal mattress sutures displayed significantly less dehiscence under different stretching conditions, reducing the tension on the skin and subcutaneous tissue [17]. This finding was in line with the present study because a smaller scar size was produced in the horizontal mattress groups, which was caused by less tension and pressure on the skin.
The wound scar is usually related to the suture technique and material. To compare the type of thread and material used in terms of absorbable or nonabsorbable, many studies have been conducted for skin closure, including the studies of Erel et al. and Kharwadkar et al. that they had declared nonabsorbable sutures had more wound scar satisfaction and less inflammation than absorbable suture type [18, 19]. Also, Menovsky et al. compared the closure of open carpal tunnel surgical wounds using nylon, polyglactin 910, and stainless-steel sutures. They showed that the scar measures and pain were statistically more observed with Vicryl suture 6 weeks after surgery [20].
Wu et al. compared wound closure techniques using horizontal mattress with nylon and interrupted deep dermal with Monocryl among patients with CTS surgery. They demonstrated that the Monocryl (intradermal) group was significantly more satisfied with scars than the nylon (horizontal mattress) group in the 2-week postoperative follow-up, while no difference was observed between these two groups in the 6-week follow-up [21]. Also, Rochlin et al. observed that Monocryl sutures revealed a lower rate of wound-related complications, including infection and dehiscence, than nylon sutures [22]. In the current study, nylon sutures and the horizontal mattress method had better clinical results than single interrupted sutures in a 6-week postoperative visit, and no comparison was made between nylon sutures and Monocryl sutures that showed less wound and scar-related reactions in Monocryl sutures can justify the different clinical results between these studies.
Liu et al. (2021) examined the outcomes of modified buried vertical mattress suture (MBVMS) versus buried intradermal suture (BIS) in 20 patients’ chest wounds, of which half were randomly closed with MBVMS and the other half closed with the BIS method. They demonstrated that the mean height and width of the postoperative scar were lower with the MBVMS method. This study showed that the aesthetic results at the end of the follow-up period were significantly better with the MBVMS method than the BIS method [23]. Although this study’s method and technique differed from ours, it generally confirms that vertical and horizontal suture techniques can have better results than the single interrupted suture technique.
Conclusion
In general, this study demonstrated that applying a horizontal mattress suture can have better results than a single interrupted suture, so the scar formation after surgery and the scar size in this method were significantly lower than single interrupted sutures in patients undergoing median nerve release. This study declared that using the horizontal mattress method in patients undergoing median nerve release can be considered a technique with fewer complications and greater effectiveness after surgery. Comparing different types of stitches with varying thread types can be a good idea for further studies.
Coincidence with COVID-19 and a significant decrease in the number of patients, decreasing the power of the study was our main challenge, and this issue even affected the desire of patients to come back for follow-up visits. In the current study, there was only one postoperative visit for surveillance of wound and scar measurements. However, 6 months for scar assessment is not enough, and longer periods of clinic follow-up, like 1 year or 2 years, are necessary for the precise prediction of aesthetic complaints of patients from their scars and the challenging features of the horizontal mattress technique. Also, better evaluation of wound complications like infection and dehiscence is achieved in short-term visits, making them essential for the next studies. Bilateral patients, each side closed with one type of suture, are very suitable for accurately comparing these two sutures with minimal confounding factors. Still, the number of these cases in our study was small, which made it impossible to analyze them accurately. This problem was one of the restrictions of our research, and it can be considered in future studies. The most important strength of the present study was its design in the form of a randomized controlled clinical trial in patients undergoing Median nerve release surgery, as well as the accurate quantitative measurement of scar indicators due to the prospective nature of the study.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences (Code: IR.IUMS.FMD.REC.1399.466). Also, written informed consent was obtained.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization and methodology: Alireza Pahlevansabagh; Supervision and funding acquisition: Amir Sobhani; Software, validation and formal analysis: Mohammad Niroomand; Investigation and resources: Naseh Soleimani; Data curation, project administration, and writing the original draft: Morteza Behjat; Review, editing and visualization: Shayan Amiri.
Conflict of interest
The authors declared no conflict of interest.
References
- Gerritsen AA, Uitdehaag BM, van Geldere D, Scholten RJ, de Vet HC, Bouter LM. Systematic review of randomized clinical trials of surgical treatment for carpal tunnel syndrome. Br J Surg. 2001; 88(10):1285-95. [DOI:10.1046/j.0007-1323.2001.01858.x]
- Genova A, Dix O, Saefan A, Thakur M, Hassan A. Carpal tunnel syndrome: A review of literature. Cureus. 2020; 12(3):e7333. [DOI:10.7759/cureus.7333]
- Pourmemari MH, Heliövaara M, Viikari-Juntura E, Shiri R. Carpal tunnel release: Lifetime prevalence, annual incidence, and risk factors. Muscle Nerve. 2018; 58(4):497-502. [DOI:10.1002/mus.26145]
- Mondelli M, Giannini F, Giacchi M. Carpal tunnel syndrome incidence in a general population. Neurology. 2002; 58(2):289-94. [DOI:10.1212/WNL.58.2.289]
- Aslani HR, Alizadeh K, Eajazi A, Karimi A, Karimi MH, Zaferani Z, et al. Comparison of carpal tunnel release with three different techniques. Clin Neurol Neurosurg. 2012; 114(7):965-8. [DOI:10.1016/j.clineuro.2012.02.017]
- Benson LS, Bare AA, Nagle DJ, Harder VS, Williams CS, Visotsky JL. Complications of endoscopic and open carpal tunnel release. Arthroscopy. 2006; 22(9):919-24. [DOI:10.1016/j.arthro.2006.05.008]
- Okutsu I, Ninomiya S, Yoshida A, Hamanaka I, Kitajima I. Measurement of carpal canal and median nerve pressure in patients with carpal tunnel syndrome. Tech Hand Up Extrem Surg. 2004; 8(2):124-8. [DOI:10.1097/01.bth.0000127362.60294.92]
- Faucher GK, Daruwalla JH, Seiler JG, 3rd. Complications of surgical releasebreak of carpal tunnel syndrome: A systematic review. J Surg Orthop Adv. 2017; 26(1):18-24. [DOI:10.3113/JSOA.2017.0018] [PMID]
- Kluge W, Simpson RG, Nicol AC. Late complications after open carpal tunnel decompression. J Hand Surg Br. 1996; 21(2):205-7. [DOI:10.1016/S0266-7681(96)80098-2]
- Kim KC, Rhee KJ, Shin HD, Kim DK. Mattress suture-bridge technique for bursal-side partial-thickness rotator cuff tears. Arch Orthop Trauma Surg. 2010; 130(3):407-11. [DOI:10.1007/s00402-009-0996-4]
- Lorbach O, Trennheuser C, Kieb M, Efe T, Kohn D, Anagnostakos K. Reconstruction of 25 and 50 % subscapularis tears: A single anchor with a double-mattress suture is sufficient for the reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016; 24(12):3855-62. [DOI:10.1007/s00167-015-3767-5]
- Bhatia S, Civitarese DM, Turnbull TL, LaPrade CM, Nitri M, Wijdicks CA, et al. A Novel repair method for radial tears of the medial meniscus: Biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med. 2016; 44(3):639-45. [DOI:10.1177/0363546515615565]
- Rosso C, Müller S, Buckland DM, Schwenk T, Zimmermann S, de Wild M, et al. All-inside meniscal repair devices compared with their matched inside-out vertical mattress suture repair: Introducing 10,000 and 100,000 loading cycles. Am J Sports Med. 2014; 42(9):2226-33. [DOI:10.1177/0363546514538394]
- Guzzini M, Lanzetti RM, Proietti L, Mazza D, Fabbri M, Monaco E, et al. Interlocking horizontal mattress suture versus Kakiuchi technique in repair of Achilles tendon rupture: A biomechanical study. J Orthop Traumatol. 2017; 18(3):251-7. [DOI:10.1007/s10195-017-0455-x]
- Moody BR, McCarthy JE, Linder J, Hruza GJ. Enhanced cosmetic outcome with running horizontal mattress sutures. Dermatol Surg. 2005; 31(10):1313-6. [DOI:10.1097/00042728-200510000-00009]
- Bolster M, Schipper C, Van Sterkenburg S, Ruettermann M, Reijnen M. Single interrupted sutures compared with Donati sutures after open carpal tunnel release: A prospective randomised trial. J Plast Surg Hand Surg. 2013; 47(4):289-91. [DOI:10.3109/2000656X.2012.762006]
- Meng F, Andrea S, Cheng S, Wang Q, Huo R. Modified subcutaneous buried horizontal mattress suture compared with vertical buried mattress suture. Ann Plast Surg. 2017; 79(2):197-202. [DOI:10.1097/SAP.0000000000001043]
- Erel E, Pleasance PI, Ahmed O, Hart NB. Absorbable versus non-absorbable suture in carpal tunnel decompression. J Hand Surg Br. 2001; 26(2):157-8. [DOI:10.1054/jhsb.2000.0545]
- Kharwadkar N, Naique S, Molitor PJ. Prospective randomized trial comparing absorbable and nonabsorbable sutures in open carpal tunnel release. J Hand Surg Br. 2005; 30(1):92-5. [DOI:10.1016/J.JHSB.2004.10.009]
- Menovsky T, Bartels RH, van Lindert EL, Grotenhuis JA. Skin closure in carpal tunnel surgery: A prospective comparative study between nylon, polyglactin 910 and stainless steel sutures. Hand Surg. 2004; 9(1):35-8. [DOI:10.1142/S0218810404002017]
- Wu E, Allen R, Bayne C, Szabo R. Prospective randomized controlled trial comparing the effect of Monocryl versus nylon sutures on patient- and observer-assessed outcomes following carpal tunnel surgery. J Hand Surg. 2023; 48(10):1014-21. [DOI:10.1177/17531934231178383]
- Rochlin DH, Sheckter CC, Curtin CM. Which stitch? Replacing anecdote with evidence in minor hand surgery. Plast Reconstr Surg Glob Open. 2019; 7(4):e2189. [DOI:10.1097/GOX.0000000000002189]
- Liu Z, Tang Z, Hao X, Liu X, He L, Yu X, et al. Modified buried vertical mattress suture versus buried intradermal suture: A prospective split-scar study. Dermatol Surg. 2021; 47(3):e75-80. [DOI:10.1097/DSS.0000000000002642]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2022/11/13 | Accepted: 2023/01/25 | Published: 2023/02/1
Received: 2022/11/13 | Accepted: 2023/01/25 | Published: 2023/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |