Volume 10, Issue 2 (5-2023)
JROS 2023, 10(2): 67-74 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bahaeddini M R, Mohammadianpour F, Dehghani Nazhvani H R, Ahmadi R, Elahifar O. Comparison of Dynamic Hip Screw and Proximal Femoral Nail Anti-rotation in the Treatment of A2-type Intertrochanteric Fractures: A Randomized Clinical Trials. JROS 2023; 10 (2) :67-74
URL: http://jros.iums.ac.ir/article-1-2255-en.html
URL: http://jros.iums.ac.ir/article-1-2255-en.html
Mohammad Reza Bahaeddini1 

 , Fereidoon Mohammadianpour1
, Fereidoon Mohammadianpour1 
 , Hamid Reza Dehghani Nazhvani1
, Hamid Reza Dehghani Nazhvani1 

 , Reza Ahmadi2
, Reza Ahmadi2 

 , Omid Elahifar1
, Omid Elahifar1 




 , Fereidoon Mohammadianpour1
, Fereidoon Mohammadianpour1 
 , Hamid Reza Dehghani Nazhvani1
, Hamid Reza Dehghani Nazhvani1 

 , Reza Ahmadi2
, Reza Ahmadi2 

 , Omid Elahifar1
, Omid Elahifar1 


1- Department of Orthopedics, School of Medicine, Firoozgar General Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafa Yahyaeian Orthopedics Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafa Yahyaeian Orthopedics Hospital, Iran University of Medical Sciences, Tehran, Iran.
Keywords: Hip fractures, Intertrochanteric fractures, Fracture fixation, Internal Fracture fixation, Intramedullary adverse effects
Full-Text [PDF 469 kb]
(102 Downloads)
| Abstract (HTML) (666 Views)
Full-Text: (155 Views)
Introduction
Intertrochanteric fracture (IF) is a common injury in individuals aged >60 years. It is characterized by a fracture line extending through the greater and lesser trochanters between the femoral neck and the lesser trochanter. This injury poses a significant healthcare challenge with implications that extend beyond immediate trauma [1, 2].
Intra-abdominal injury (IAI) is a potentially life-threatening condition with a mortality rate of approximately 17%, more than twice that of femoral neck fracture [3].
Although IF is primarily associated with severe trauma, such as car accidents in younger individuals, it can also occur due to minor trauma, especially among the elderly population, particularly those with underlying medical conditions, such as osteoporosis [3, 4].
Studies show that approximately 200,000 cases of IF occur annually in the United States, with a mortality rate ranging from 10% to 30% per year [5, 6]. Furthermore, the risk of surgical site infection after surgical treatment of IF is estimated to be between 1.7% and 17%, depending on factors, such as the surgical approach, wound proximity to the perineum, and duration of the operation [7, 8, 9].
Despite the substantial economic burden of $2.63 billion annually [10], it is necessary to comprehensively evaluate treatment modalities due to their impact on patient quality of life.
While various treatment options exist, including conservative and surgical approaches for the management of IF, surgery with different implants, commonly with dynamic hip screw (DHS), is the usual treatment to immobilize the fracture [11, 12].
Conservative management is not commonly used due to its association with a higher likelihood of complications, such as bedsores, joint contractures, urinary tract, and lung infections, as well as an increased probability of mortality (up to 34.6%) [13].
Surgery is the preferred treatment for managing IF [13]due to its ability to significantly reduce hospitalization duration, facilitate a quicker return to the patient’s preoperative level of functioning, and mitigate complications associated with IF. Although DHS is a simple approach to implement and provides satisfactory results, it may be correlated with certain risks and complications, such as an increased likelihood of varus coxa due to subsurface operation and fixation failure, particularly in cases of unstable fractures and reverse oblique IF. In contrast, proximal femoral nail anti-rotation (PFNA) offers several advantages over DHS [12].
In contrast, PFNA is a less invasive implant designed in 2004 to reduce implant-related complications. Its spiral blade penetrates the femoral head more easily, causing less bone tissue loss during penetration than other screw-based tools. Additionally, it prevents protrusion on the opposite side of the bone, which is a significant issue in other techniques [13-16]. Although PFNA is the preferred treatment for osteoporotic patients owing to its advantages over other treatments, it is more challenging and expensive to implement than DHS [10, 17].
The current literature does not adequately explore the comparative effectiveness of these methods, particularly in treating A2-type IF. Our study aimed to fill this gap by providing valuable insights into the effectiveness and complications of DHS and PFNA in the surgical treatment of A2-type IF. We conducted a randomized clinical trial to compare the efficacy and complications of these two approaches.
Methods
This randomized clinical trial was conducted from July 2022 to August 2023 at the Orthopedic Center of Firouzgar Hospital and Shafayahyaeian Hospital, Tehran Province, Iran, affiliated with Iran University of Medical Sciences.
Patient selection
The inclusion criteria included patients older than 18 years with A2-type IF who provided informed consent. The exclusion criteria included patients with IF other than the A2-type, open fractures, old IF, pathological fractures, systemic hematological or immune system diseases, IF-caused mortality, accompanying musculoskeletal diseases, severe psychiatric disorders, or cognitive impairments, and patients who were unwilling to participate or failed to complete the informed consent.
Randomization and interventions
An expert epidemiologist used computerized random allocation software, version 1.0 to perform randomization. Patients with A2-type IF were randomly assigned to the DHS or PFNA groups in a 1:1 ratio.
Both DHS and PFNA surgical interventions followed established protocols. Both groups underwent surgical interventions following established scientific standards, ensuring no patient was deprived of standard treatment. The primary objective of this study was to compare the outcomes and complications associated with the two surgical methods.
Data collection and follow-up
The researcher, Fereidoon Mohammadianpour recorded patient information twice: Once during admission for surgery and again during the follow-up period. The collected data included demographic information (age and sex) and postoperative clinical and radiographic outcomes. This included the duration of the operation, bleeding during the operation, duration of callus formation, non:union: rate, and duration of hospitalization. The collected information was stored, analyzed, and maintained confidentially and anonymously, following the principles of Helsinki ethics.
Patients were followed up immediately after the operation and at five subsequent intervals (two weeks, six weeks, three months, and six months post-operation). The follow-ups were conducted by specialist doctors in the orthopedic clinic who assessed patients for the operation outcomes and complications using clinical and radiographic assessments. This study involved welding and non:union: treatments, enabling a thorough comparison of treatment outcomes between the two groups at various time intervals.
Statistical analysis
This study meticulously examined the age and sex distributions between the DHS and PFNA groups. Subsequent multivariate analyses were conducted to enhance control over potential confounding factors.
Statistical analyses were performed to compare demographic and clinical variables, ensuring robustness in assessing outcomes associated with DHS and PFNA interventions. After data collection, patient information was processed and analyzed using SPSS software, version 26. Descriptive statistics and central indices were used to calculate the mean and median values for the DHS and PFNA groups. This provided a comprehensive overview of the central tendencies of the collected data. The normality of the distribution of variables in the two groups was assessed using the Kolmogorov-Smirnov test to determine the appropriateness of parametric statistical tests. To compare quantitative variables between the DHS and PFNA groups, we utilized the t-test, which assumed a normal distribution of variables. In cases where standard distribution assumptions were unmet, we applied the non-parametric Mann-Whitney test to ensure robust statistical comparisons. We analyzed qualitative variables using Fisher’s statistical test and the chi-square test. These tests examined the two surgical intervention groups’ relationships and differences in categorical variables. The significance of the rate in the two groups was reported using the risk ratio (RR) with a 95% confidence interval. This measure provides insight into the relative risk associated with each surgical method, contributing to a nuanced interpretation of the results. P<0.05 was used as a statistical significance threshold, following standard scientific research practices. This ensured the robustness of the interpretation of results.
Results
Characteristics
A total of 234 patients were enrolled between July 2022 and August 2023, with an age range of 26 to 97 years and a mean age of 73.22±16.07. Ninety-three patients were lost to follow-up, leaving 76 PFNA-treated and 65 DHS-treated patients who completed the 6-month follow-up. The mean age of the PFNA group was 76.14, while the DHS group had a mean age of 71.52 (Table 1).
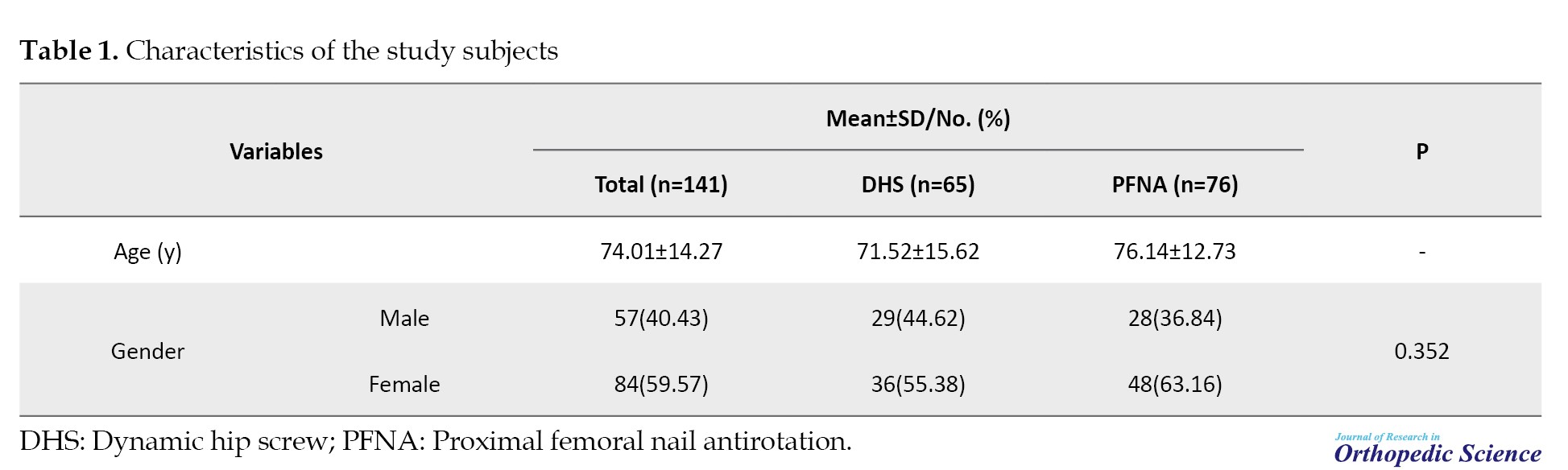
Of the 76 patients in the PFNA group, 48 (63.16%) were women, and 28 (36.84%) were men. Among the 65 subjects in the DHS group, 36(55.38%) were women, and 29(44.64%) were men. No statistically significant differences were observed between the two groups regarding demographic characteristics, including age and sex.
Table 2 summarizes the observed results, including the Mean±SD of bleeding volume during the operation per deciliter, duration of the operation per hour, and duration of hospitalization per day.
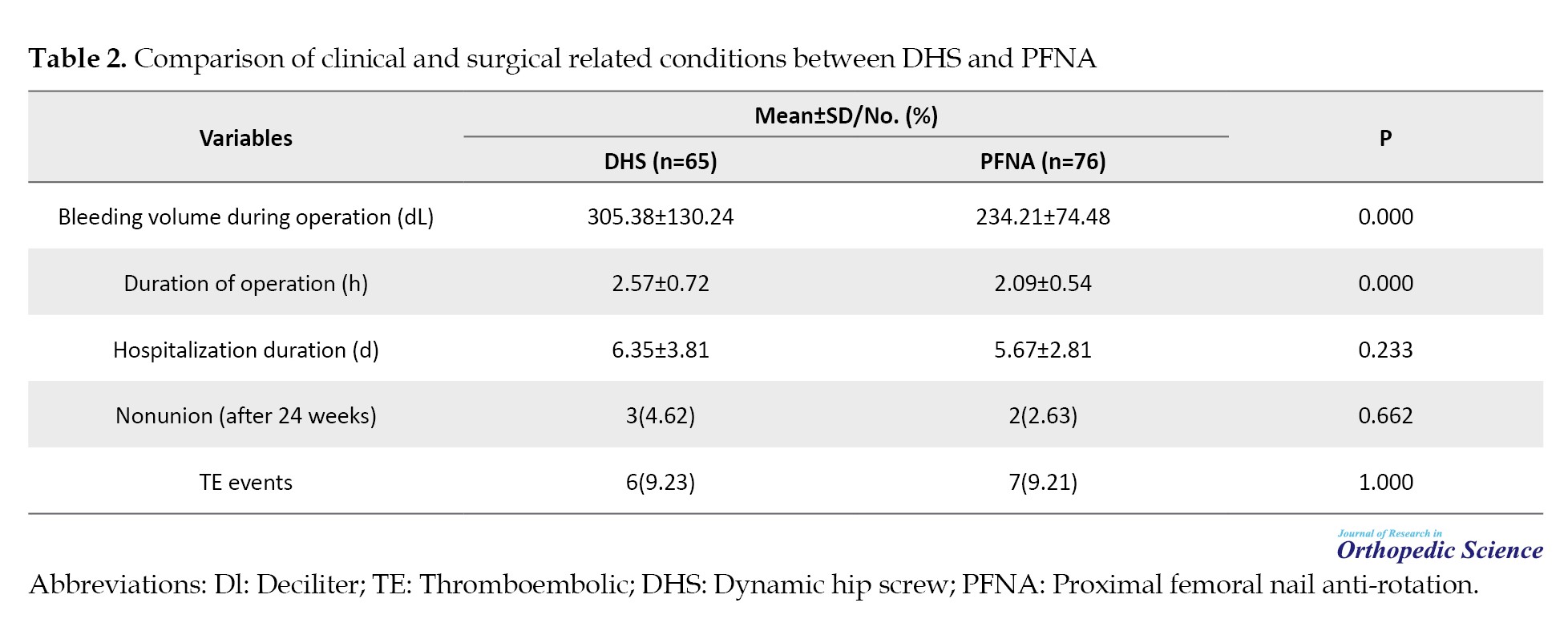
It also includes complications after the surgery, such as the percentages of non:union: after 24 weeks and thromboembolic events.
The Mean±SD of bleeding volume during the operation was 305.38±130.24 and 234.21±74.48 in the DHS- and PFNA-treated groups, respectively. The mean duration of operation was 2.57±0.72 and 2.09±0.54 in the DHS- and PFNA-treated groups, respectively. The DHS-treated group had a statistically significant higher mean bleeding volume during operation (305.38±130.24 vs 234.21±74.48, P<0.001) and mean duration of operation (2.57±0.72 vs 2.09±0.54, P=<0.001) compared to the PFNA-treated group.
However, no statistically significant difference was observed between the two groups regarding the mean duration of hospitalization, percentage of non:union: after 24 weeks, and percentage of thromboembolic events (P>0.05).
Discussion
Fracture management in orthopedic surgery, particularly IF, poses a substantial challenge with implications for healthcare systems and individuals. This study compared the DHS and PFNA approaches to treat IF to provide valuable insights.
Our investigation revealed significant advantages of the PFNA approach for A2-type IF. Specifically, PFNA resulted in significantly lower perioperative bleeding volume and operative duration than DHS (P=0.000). No significant differences were observed regarding hospitalization duration and postsurgical complications, including non:union: and thromboembolic events. However, PFNA significantly decreased intraoperative hemorrhage and operative duration (P=0.000).
It is essential to note that these findings are consistent with a recent systematic review and meta-analysis comparing intramedullary nails and DHS [18]. The study found that DHS was associated with a statistically significant increase in operative time and blood loss during surgery compared with intramedullary nails, which is consistent with our results. However, no significant differences were observed between the two approaches regarding mortality, associated complications, or fixation failure rates [18].
A recent systematic review compared the DHS approach with intramedullary nails in treating IF. A review found that the DHS approach was associated with significantly increased blood loss and a longer duration of operation [19].
According to a meta-analysis, a longer operative time logically results in a higher probability of increased blood loss during surgery. Intramedullary nails have been recommended to treat unstable IF due to lower blood loss during surgery [20]. It has been hypothesized that DHS may be associated with a higher likelihood of infection and blood loss owing to longer operation time [21].
Consistent with our results on the lack of significant difference between the DHS and PFNA approaches for postsurgical complications, a study that followed approximately 6000 individuals for more than 7 years after surgical treatment of IF by DHS or intramedullary nail approach revealed that the associated complication rates were the same at 16%. No significant differences were observed between the two approaches. However, a systematic review found no significant difference between the two approaches, DHS and intramedullary nails, regarding implant-related postoperative complications, including non:union: and implant breakage [22].
Studies have shown that both DHS and intramedullary nails effectively treat IF. However, the final decision on whether to use a DHS or intramedullary nail approach may be influenced by underlying medical conditions, comorbidities, such as osteoporosis or advanced age, and other factors [22].
The study indicated that PFNA may be preferred for A2-type IF in older patients with comorbid conditions despite its higher cost [17]. This is due to the significant reduction in operative duration and blood loss during surgery, making PFNA a potentially safer choice when minimizing these factors.
Although both the PFNA and DHS approaches have similar outcomes, such as duration of hospitalization and associated complications, including the risk of non:union: and thromboembolic events following surgical interventions, our results show that the PFNA approach has a significantly shorter operative duration and less blood loss during the operation. Therefore, PFNA could be considered a safer and potentially the first option for treating IF, specifically A2-type IF, in situations where minimal operative duration and blood loss are necessary, despite the higher cost compared to screw-based approaches, such as DHS. In other words, PFNA may be the best choice for A2-type IF in older patients with multiple underlying comorbid conditions and cardiovascular diseases, making them sensitive to intravascular volume and blood pressure alterations, which can be life-threatening.
Similar to other studies, our study has limitations that warrant consideration. The trial was conducted at a single center, potentially introducing institutional biases and limiting the external validity of the results to diverse healthcare settings. The follow-up period was limited to six months post-operation, which may not capture long-term complications or delayed adverse events associated with either DHS or PFNA. Limiting the focus to the A2-type of IF may restrict the generalizability of the results to a broader range of IF. As with other surgical trials, the assigned treatment is not blinded to surgeons and patients, which may affect subjective measures. Moreover, the study primarily relied on clinical and radiographic outcomes obtained by an expert physician without comprehensive patient-reported outcomes that could provide valuable insights into the quality of life, pain, and functional recovery. Additionally, the patient’s cardiovascular and coagulation profiles, which could have impacted thromboembolic events, were not obtained.
We propose several recommendations to improve the robustness and precision of the comparative analysis of the efficacy and adverse outcomes associated with DHS and PFNA approaches. To increase the generalizability of results, overcome the limitations of single-center studies, and ensure applicability across various demographics, multicenter trials involving diverse populations are imperative. Additionally, extending the duration of follow-up studies is essential for capturing prolonged complications and delayed adverse events associated with both DHS and PFNA treatments.
Furthermore, an assessment involving extended patient-reported outcome measures is indispensable to provide holistic insight into the impacts on quality of life, pain, and functional recovery. In addition, exploring patient preferences and satisfaction levels regarding both DHS and PFNA approaches is crucial.
Furthermore, a comprehensive cost-effectiveness analysis that includes all expenses associated with DHS and PFNA procedures, such as surgical costs, hospitalization, and potential complications is necessary. The assessment should consider the benefits of reduced operating duration and blood loss against the higher costs of PFNA. It is essential to gain a nuanced understanding of the economic considerations associated with each approach. Additionally, underlying medical conditions should be considered when discerning treatment outcomes and informing the decision-making process between DHS and PFNA. The investigation should determine whether specific patient profiles benefit more from one approach than from another.
When examining patient histories, it is crucial to focus on cardiovascular and coagulation disorders to identify specific risk factors that contribute to postsurgical thromboembolic events. Refining research methodologies and considering these factors can improve the scientific rigor of the study and advance evidence-based clinical practices in orthopedic interventions.
Conclusion
In conclusion, our comparative study of the DHS and PFNA approaches for A2-type IF indicates that PFNA has notable advantages. These include significantly lower preoperative bleeding volume and shorter operative duration. However, no significant difference is observed in the duration of hospitalization or postsurgical complications, such as the risk of non:union: and thromboembolic events, between PNFA and DHS.
Our study suggests that PFNA may be a preferred option for the surgical treatment of A2-type fractures in individuals with multiple comorbidities, especially cardiovascular comorbidities, due to its safety benefits in scenarios prioritizing minimized operative duration and blood loss despite comparable postsurgical complications. It is crucial to note that this recommendation is based solely on objective data and not subjective evaluations.
While acknowledging the study’s limitations, such as its single-center design and limited follow-up period, we recommend future research. These should include multicenter trials with extended follow-up, comprehensive patient-reported outcomes, and cost-effectiveness analyses. Such refinements will contribute to evidence-based orthopedic interventions, enabling more informed decision-making in treating IF.
Ethical Considerations
Compliance with ethical guidelines
This study adhered to the principles outlined in the Declaration of Helsinki. The Institutional Ethics Board of Iran University of Medical Sciences, Tehran, Iran approved the study (Code: IR.IUMS.FMD.REC.1401.220. Informed consent was obtained from all the participants at the start of the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Mohammad Reza Bahaeddini, Omid Elahifar, Fereidoon Mohammadianpour, and HamidReza Dehghani Nazhvani; Data analysis: Reza Ahmadi; Writing: Omid Elahifar.
Conflict of interest
The authors declared no conflict of interest.
References
Intertrochanteric fracture (IF) is a common injury in individuals aged >60 years. It is characterized by a fracture line extending through the greater and lesser trochanters between the femoral neck and the lesser trochanter. This injury poses a significant healthcare challenge with implications that extend beyond immediate trauma [1, 2].
Intra-abdominal injury (IAI) is a potentially life-threatening condition with a mortality rate of approximately 17%, more than twice that of femoral neck fracture [3].
Although IF is primarily associated with severe trauma, such as car accidents in younger individuals, it can also occur due to minor trauma, especially among the elderly population, particularly those with underlying medical conditions, such as osteoporosis [3, 4].
Studies show that approximately 200,000 cases of IF occur annually in the United States, with a mortality rate ranging from 10% to 30% per year [5, 6]. Furthermore, the risk of surgical site infection after surgical treatment of IF is estimated to be between 1.7% and 17%, depending on factors, such as the surgical approach, wound proximity to the perineum, and duration of the operation [7, 8, 9].
Despite the substantial economic burden of $2.63 billion annually [10], it is necessary to comprehensively evaluate treatment modalities due to their impact on patient quality of life.
While various treatment options exist, including conservative and surgical approaches for the management of IF, surgery with different implants, commonly with dynamic hip screw (DHS), is the usual treatment to immobilize the fracture [11, 12].
Conservative management is not commonly used due to its association with a higher likelihood of complications, such as bedsores, joint contractures, urinary tract, and lung infections, as well as an increased probability of mortality (up to 34.6%) [13].
Surgery is the preferred treatment for managing IF [13]due to its ability to significantly reduce hospitalization duration, facilitate a quicker return to the patient’s preoperative level of functioning, and mitigate complications associated with IF. Although DHS is a simple approach to implement and provides satisfactory results, it may be correlated with certain risks and complications, such as an increased likelihood of varus coxa due to subsurface operation and fixation failure, particularly in cases of unstable fractures and reverse oblique IF. In contrast, proximal femoral nail anti-rotation (PFNA) offers several advantages over DHS [12].
In contrast, PFNA is a less invasive implant designed in 2004 to reduce implant-related complications. Its spiral blade penetrates the femoral head more easily, causing less bone tissue loss during penetration than other screw-based tools. Additionally, it prevents protrusion on the opposite side of the bone, which is a significant issue in other techniques [13-16]. Although PFNA is the preferred treatment for osteoporotic patients owing to its advantages over other treatments, it is more challenging and expensive to implement than DHS [10, 17].
The current literature does not adequately explore the comparative effectiveness of these methods, particularly in treating A2-type IF. Our study aimed to fill this gap by providing valuable insights into the effectiveness and complications of DHS and PFNA in the surgical treatment of A2-type IF. We conducted a randomized clinical trial to compare the efficacy and complications of these two approaches.
Methods
This randomized clinical trial was conducted from July 2022 to August 2023 at the Orthopedic Center of Firouzgar Hospital and Shafayahyaeian Hospital, Tehran Province, Iran, affiliated with Iran University of Medical Sciences.
Patient selection
The inclusion criteria included patients older than 18 years with A2-type IF who provided informed consent. The exclusion criteria included patients with IF other than the A2-type, open fractures, old IF, pathological fractures, systemic hematological or immune system diseases, IF-caused mortality, accompanying musculoskeletal diseases, severe psychiatric disorders, or cognitive impairments, and patients who were unwilling to participate or failed to complete the informed consent.
Randomization and interventions
An expert epidemiologist used computerized random allocation software, version 1.0 to perform randomization. Patients with A2-type IF were randomly assigned to the DHS or PFNA groups in a 1:1 ratio.
Both DHS and PFNA surgical interventions followed established protocols. Both groups underwent surgical interventions following established scientific standards, ensuring no patient was deprived of standard treatment. The primary objective of this study was to compare the outcomes and complications associated with the two surgical methods.
Data collection and follow-up
The researcher, Fereidoon Mohammadianpour recorded patient information twice: Once during admission for surgery and again during the follow-up period. The collected data included demographic information (age and sex) and postoperative clinical and radiographic outcomes. This included the duration of the operation, bleeding during the operation, duration of callus formation, non:union: rate, and duration of hospitalization. The collected information was stored, analyzed, and maintained confidentially and anonymously, following the principles of Helsinki ethics.
Patients were followed up immediately after the operation and at five subsequent intervals (two weeks, six weeks, three months, and six months post-operation). The follow-ups were conducted by specialist doctors in the orthopedic clinic who assessed patients for the operation outcomes and complications using clinical and radiographic assessments. This study involved welding and non:union: treatments, enabling a thorough comparison of treatment outcomes between the two groups at various time intervals.
Statistical analysis
This study meticulously examined the age and sex distributions between the DHS and PFNA groups. Subsequent multivariate analyses were conducted to enhance control over potential confounding factors.
Statistical analyses were performed to compare demographic and clinical variables, ensuring robustness in assessing outcomes associated with DHS and PFNA interventions. After data collection, patient information was processed and analyzed using SPSS software, version 26. Descriptive statistics and central indices were used to calculate the mean and median values for the DHS and PFNA groups. This provided a comprehensive overview of the central tendencies of the collected data. The normality of the distribution of variables in the two groups was assessed using the Kolmogorov-Smirnov test to determine the appropriateness of parametric statistical tests. To compare quantitative variables between the DHS and PFNA groups, we utilized the t-test, which assumed a normal distribution of variables. In cases where standard distribution assumptions were unmet, we applied the non-parametric Mann-Whitney test to ensure robust statistical comparisons. We analyzed qualitative variables using Fisher’s statistical test and the chi-square test. These tests examined the two surgical intervention groups’ relationships and differences in categorical variables. The significance of the rate in the two groups was reported using the risk ratio (RR) with a 95% confidence interval. This measure provides insight into the relative risk associated with each surgical method, contributing to a nuanced interpretation of the results. P<0.05 was used as a statistical significance threshold, following standard scientific research practices. This ensured the robustness of the interpretation of results.
Results
Characteristics
A total of 234 patients were enrolled between July 2022 and August 2023, with an age range of 26 to 97 years and a mean age of 73.22±16.07. Ninety-three patients were lost to follow-up, leaving 76 PFNA-treated and 65 DHS-treated patients who completed the 6-month follow-up. The mean age of the PFNA group was 76.14, while the DHS group had a mean age of 71.52 (Table 1).
Of the 76 patients in the PFNA group, 48 (63.16%) were women, and 28 (36.84%) were men. Among the 65 subjects in the DHS group, 36(55.38%) were women, and 29(44.64%) were men. No statistically significant differences were observed between the two groups regarding demographic characteristics, including age and sex.
Table 2 summarizes the observed results, including the Mean±SD of bleeding volume during the operation per deciliter, duration of the operation per hour, and duration of hospitalization per day.
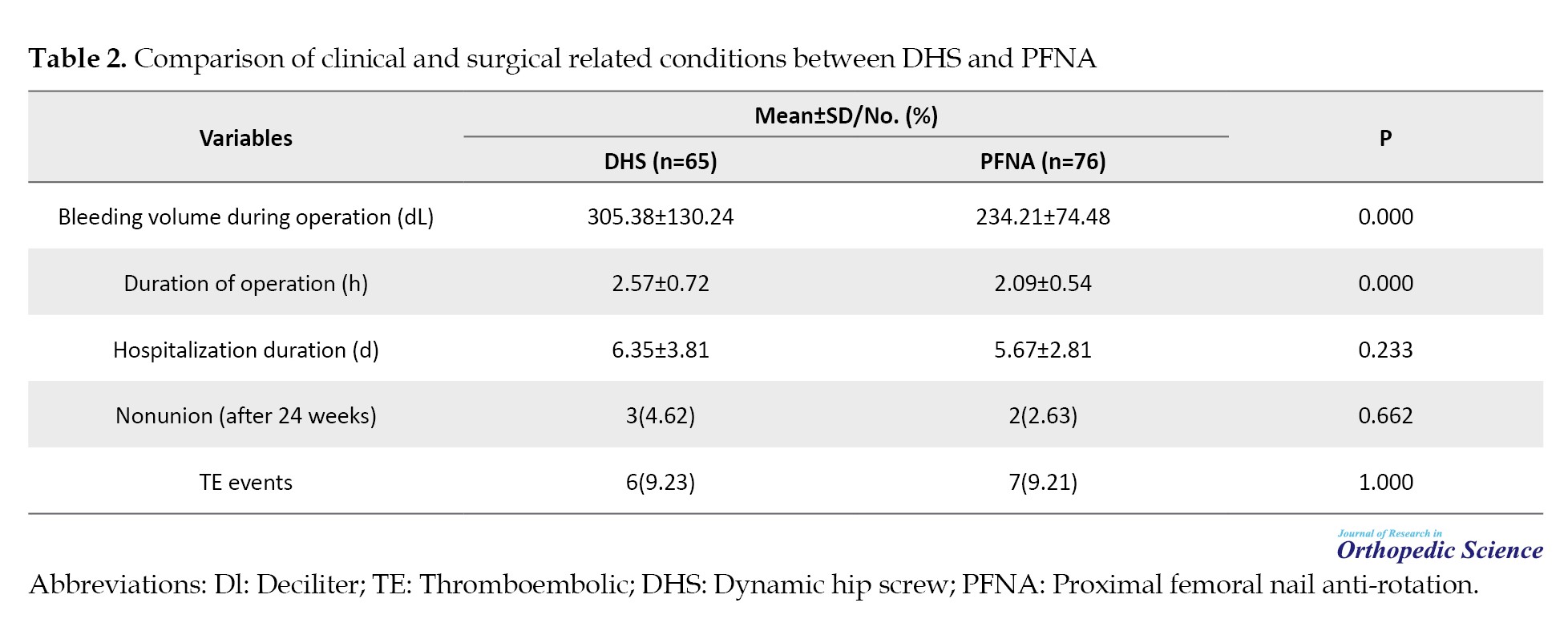
It also includes complications after the surgery, such as the percentages of non:union: after 24 weeks and thromboembolic events.
The Mean±SD of bleeding volume during the operation was 305.38±130.24 and 234.21±74.48 in the DHS- and PFNA-treated groups, respectively. The mean duration of operation was 2.57±0.72 and 2.09±0.54 in the DHS- and PFNA-treated groups, respectively. The DHS-treated group had a statistically significant higher mean bleeding volume during operation (305.38±130.24 vs 234.21±74.48, P<0.001) and mean duration of operation (2.57±0.72 vs 2.09±0.54, P=<0.001) compared to the PFNA-treated group.
However, no statistically significant difference was observed between the two groups regarding the mean duration of hospitalization, percentage of non:union: after 24 weeks, and percentage of thromboembolic events (P>0.05).
Discussion
Fracture management in orthopedic surgery, particularly IF, poses a substantial challenge with implications for healthcare systems and individuals. This study compared the DHS and PFNA approaches to treat IF to provide valuable insights.
Our investigation revealed significant advantages of the PFNA approach for A2-type IF. Specifically, PFNA resulted in significantly lower perioperative bleeding volume and operative duration than DHS (P=0.000). No significant differences were observed regarding hospitalization duration and postsurgical complications, including non:union: and thromboembolic events. However, PFNA significantly decreased intraoperative hemorrhage and operative duration (P=0.000).
It is essential to note that these findings are consistent with a recent systematic review and meta-analysis comparing intramedullary nails and DHS [18]. The study found that DHS was associated with a statistically significant increase in operative time and blood loss during surgery compared with intramedullary nails, which is consistent with our results. However, no significant differences were observed between the two approaches regarding mortality, associated complications, or fixation failure rates [18].
A recent systematic review compared the DHS approach with intramedullary nails in treating IF. A review found that the DHS approach was associated with significantly increased blood loss and a longer duration of operation [19].
According to a meta-analysis, a longer operative time logically results in a higher probability of increased blood loss during surgery. Intramedullary nails have been recommended to treat unstable IF due to lower blood loss during surgery [20]. It has been hypothesized that DHS may be associated with a higher likelihood of infection and blood loss owing to longer operation time [21].
Consistent with our results on the lack of significant difference between the DHS and PFNA approaches for postsurgical complications, a study that followed approximately 6000 individuals for more than 7 years after surgical treatment of IF by DHS or intramedullary nail approach revealed that the associated complication rates were the same at 16%. No significant differences were observed between the two approaches. However, a systematic review found no significant difference between the two approaches, DHS and intramedullary nails, regarding implant-related postoperative complications, including non:union: and implant breakage [22].
Studies have shown that both DHS and intramedullary nails effectively treat IF. However, the final decision on whether to use a DHS or intramedullary nail approach may be influenced by underlying medical conditions, comorbidities, such as osteoporosis or advanced age, and other factors [22].
The study indicated that PFNA may be preferred for A2-type IF in older patients with comorbid conditions despite its higher cost [17]. This is due to the significant reduction in operative duration and blood loss during surgery, making PFNA a potentially safer choice when minimizing these factors.
Although both the PFNA and DHS approaches have similar outcomes, such as duration of hospitalization and associated complications, including the risk of non:union: and thromboembolic events following surgical interventions, our results show that the PFNA approach has a significantly shorter operative duration and less blood loss during the operation. Therefore, PFNA could be considered a safer and potentially the first option for treating IF, specifically A2-type IF, in situations where minimal operative duration and blood loss are necessary, despite the higher cost compared to screw-based approaches, such as DHS. In other words, PFNA may be the best choice for A2-type IF in older patients with multiple underlying comorbid conditions and cardiovascular diseases, making them sensitive to intravascular volume and blood pressure alterations, which can be life-threatening.
Similar to other studies, our study has limitations that warrant consideration. The trial was conducted at a single center, potentially introducing institutional biases and limiting the external validity of the results to diverse healthcare settings. The follow-up period was limited to six months post-operation, which may not capture long-term complications or delayed adverse events associated with either DHS or PFNA. Limiting the focus to the A2-type of IF may restrict the generalizability of the results to a broader range of IF. As with other surgical trials, the assigned treatment is not blinded to surgeons and patients, which may affect subjective measures. Moreover, the study primarily relied on clinical and radiographic outcomes obtained by an expert physician without comprehensive patient-reported outcomes that could provide valuable insights into the quality of life, pain, and functional recovery. Additionally, the patient’s cardiovascular and coagulation profiles, which could have impacted thromboembolic events, were not obtained.
We propose several recommendations to improve the robustness and precision of the comparative analysis of the efficacy and adverse outcomes associated with DHS and PFNA approaches. To increase the generalizability of results, overcome the limitations of single-center studies, and ensure applicability across various demographics, multicenter trials involving diverse populations are imperative. Additionally, extending the duration of follow-up studies is essential for capturing prolonged complications and delayed adverse events associated with both DHS and PFNA treatments.
Furthermore, an assessment involving extended patient-reported outcome measures is indispensable to provide holistic insight into the impacts on quality of life, pain, and functional recovery. In addition, exploring patient preferences and satisfaction levels regarding both DHS and PFNA approaches is crucial.
Furthermore, a comprehensive cost-effectiveness analysis that includes all expenses associated with DHS and PFNA procedures, such as surgical costs, hospitalization, and potential complications is necessary. The assessment should consider the benefits of reduced operating duration and blood loss against the higher costs of PFNA. It is essential to gain a nuanced understanding of the economic considerations associated with each approach. Additionally, underlying medical conditions should be considered when discerning treatment outcomes and informing the decision-making process between DHS and PFNA. The investigation should determine whether specific patient profiles benefit more from one approach than from another.
When examining patient histories, it is crucial to focus on cardiovascular and coagulation disorders to identify specific risk factors that contribute to postsurgical thromboembolic events. Refining research methodologies and considering these factors can improve the scientific rigor of the study and advance evidence-based clinical practices in orthopedic interventions.
Conclusion
In conclusion, our comparative study of the DHS and PFNA approaches for A2-type IF indicates that PFNA has notable advantages. These include significantly lower preoperative bleeding volume and shorter operative duration. However, no significant difference is observed in the duration of hospitalization or postsurgical complications, such as the risk of non:union: and thromboembolic events, between PNFA and DHS.
Our study suggests that PFNA may be a preferred option for the surgical treatment of A2-type fractures in individuals with multiple comorbidities, especially cardiovascular comorbidities, due to its safety benefits in scenarios prioritizing minimized operative duration and blood loss despite comparable postsurgical complications. It is crucial to note that this recommendation is based solely on objective data and not subjective evaluations.
While acknowledging the study’s limitations, such as its single-center design and limited follow-up period, we recommend future research. These should include multicenter trials with extended follow-up, comprehensive patient-reported outcomes, and cost-effectiveness analyses. Such refinements will contribute to evidence-based orthopedic interventions, enabling more informed decision-making in treating IF.
Ethical Considerations
Compliance with ethical guidelines
This study adhered to the principles outlined in the Declaration of Helsinki. The Institutional Ethics Board of Iran University of Medical Sciences, Tehran, Iran approved the study (Code: IR.IUMS.FMD.REC.1401.220. Informed consent was obtained from all the participants at the start of the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: Mohammad Reza Bahaeddini, Omid Elahifar, Fereidoon Mohammadianpour, and HamidReza Dehghani Nazhvani; Data analysis: Reza Ahmadi; Writing: Omid Elahifar.
Conflict of interest
The authors declared no conflict of interest.
References
- Clawson DK. Intertrochanteric fracture of the hip. Am J Surg. 1957; 93(4):580-7. [DOI:10.1016/0002-9610(57)90513-5] [PMID]
- Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture: A medicare claims database analysis. JB JS Open Access. 2019; 4(1):e0045. [DOI:10.2106/JBJS.OA.18.00045] [PMID] [PMCID]
- Zhao F, Wang X, Dou Y, Wang H, Zhang Y. Analysis of risk factors for perioperative mortality in elderly patients with intertrochanteric fracture. Eur J Orthop Surg Traumatol. 2019; 29(1):59-63. [DOI:10.1007/s00590-018-2285-9] [PMID]
- Hsueh KK, Fang CK, Chen CM, Su YP, Wu HF, Chiu FY. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: An evaluation of 937 patients. Int Orthop. 2010; 34(8):1273-6. [DOI:10.1007/s00264-009-0866-2] [PMID] [PMCID]
- Tang P, Hu F, Shen J, Zhang L, Zhang L. Proximal femoral nail antirotation versus hemiarthroplasty: A study for the treatment of intertrochanteric fractures. Injury. 2012; 43(6):876-81. [DOI:10.1016/j.injury.2011.11.008] [PMID]
- Ma KL, Wang X, Luan FJ, Xu HT, Fang Y, Min J, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: A meta-analysis. Orthop Traumatol Surg Res. 2014; 100(8):859-66. [DOI:10.1016/j.otsr.2014.07.023] [PMID]
- Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991; 73(2):330-4. [DOI:10.1302/0301-620X.73B2.2005167] [PMID]
- Zhang B, Chiu KY, Wang M. Hip arthroplasty for failed internal fixation of intertrochanteric fractures. J Arthroplasty. 2004; 19(3):329-33. [DOI:10.1016/j.arth.2003.10.010] [PMID]
- Zhao K, Zhang J, Li J, Meng H, Wang Z, Zhu Y, et al. Incidence and risk factors of surgical site infection after intertrochanteric fracture surgery: A prospective cohort study. Int Wound J. 2020; 17(6):1871-80. [DOI:10.1111/iwj.13477] [PMID] [PMCID]
- Li H, Wang Q, Dai GG, Peng HP. PFNA vs DHS helical blade for elderly patients with osteoporotic femoral intertrochanteric fractures. Eur Rev Med Pharmacol Sci. 2018; 22(1 Suppl):1-7. [Link]
- Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: Rationale, evidence, and recommendations. Bone Joint J. 2017; 99-B(1):128-33. [DOI:10.1302/0301-620X.99B1.BJJ-2016-0134.R1] [PMID]
- Avakian Z, Shiraev T, Lam L, Hope N. Dynamic hip screws versus proximal femoral nails for intertrochanteric fractures. ANZ J Surg. 2012; 82(1-2):56-9. [DOI:10.1111/j.1445-2197.2011.05929.x] [PMID]
- Xu R, Ru J, Ji F, Liu J, Ji Y, Wu Z, et al. Comparison of efficacy, complications and TGF-β2 expression between DHS and PFNA in elderly patients with osteoporotic femoral intertrochanteric fracture. Exp Ther Med. 2018; 16(1):394-99. [DOI:10.3892/etm.2018.6177] [PMID] [PMCID]
- Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010; 38(4):1266-75. [DOI:10.1177/147323001003800408] [PMID]
- Shen L, Zhang Y, Shen Y, Cui Z. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: A meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res. 2013; 99(4):377-83. [DOI:10.1016/j.otsr.2012.12.019] [PMID]
- Zou J, Xu Y, Yang H. A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int Med Res. 2009; 37(4):1057-64. [DOI:10.1177/147323000903700410] [PMID]
- Wang B, Liu Q, Liu Y, Jiang R. Comparison of proximal femoral nail antirotation and dynamic hip screw internal fixation on serum markers in elderly patients with intertrochanteric fractures. J Coll Physicians Surg Pak. 2019; 29(7):644-8. [DOI:10.29271/jcpsp.2019.07.644] [PMID]
- Raj S, Grover S, Bola H, Pradhan A, Fazal MA, Patel A. Dynamic hip screws versus cephalocondylic intramedullary nails for unstable extracapsular hip fractures in 2021: A systematic review and meta-analysis of randomised trials. Journal of Orthopaedics. 2023 [Unpublished]. [DOI:10.21203/rs.3.rs-1994351/v1]
- Hao Z, Wang X, Zhang X. Comparing surgical interventions for intertrochanteric hip fracture by blood loss and operation time: A network meta-analysis. J Orthop Surg Res. 2018; 13(1):157. [DOI:10.1186/s13018-018-0852-8] [PMID] [PMCID]
- Li AB, Zhang WJ, Wang J, Guo WJ, Wang XH, Zhao YM. Intramedullary and extramedullary fixations for the treatment of unstable femoral intertrochanteric fractures: A meta-analysis of prospective randomized controlled trials. Int Orthop. 2017; 41(2):403-13. [DOI:10.1007/s00264-016-3308-y] [PMID]
- Schipper I, Steyerberg E, Castelein RM, Van der Heijden F, Den Hoed P, Kerver A, et al. Treatment of unstable trochanteric fractures: Randomised comparison of the gamma nail and the proximal femoral nail. J Bone Joint Surg Br Volume. 2004; 86(1):86-94. [DOI:10.1302/0301-620X.86B1.14455]
- Zhang WQ, Sun J, Liu CY, Zhao HY, Sun YF. Comparing the intramedullary nail and extramedullary fixation in treatment of unstable intertrochanteric fractures. Sci Rep. 2018; 8(1):2321. [DOI:10.1038/s41598-018-20717-2] [PMID] [PMCID]
Type of Study: Research Article |
Subject:
Trauma
Received: 2022/08/31 | Accepted: 2022/11/9 | Published: 2023/05/1
Received: 2022/08/31 | Accepted: 2022/11/9 | Published: 2023/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |