Volume 10, Issue 4 (11-2023)
JROS 2023, 10(4): 201-216 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghanbari A, Yahyazadeh H, Bagherifard A, Khosravi K, Azimi A, Ahmadi R, et al . Total Joint Arthroplasty in Patients With Parkinson’s Disease: A Review of Recent Literature. JROS 2023; 10 (4) :201-216
URL: http://jros.iums.ac.ir/article-1-2260-en.html
URL: http://jros.iums.ac.ir/article-1-2260-en.html
Alireza Ghanbari1 

 , Hooman Yahyazadeh2
, Hooman Yahyazadeh2 

 , Abolfazl Bagherifard3
, Abolfazl Bagherifard3 

 , Karo Khosravi3
, Karo Khosravi3 
 , Amir Azimi3
, Amir Azimi3 
 , Reza Ahmadi3
, Reza Ahmadi3 

 , Tahereh Farkhondeh4
, Tahereh Farkhondeh4 

 , Babak Roshanravan5
, Babak Roshanravan5 

 , Saeed Samarghandian6
, Saeed Samarghandian6 




 , Hooman Yahyazadeh2
, Hooman Yahyazadeh2 

 , Abolfazl Bagherifard3
, Abolfazl Bagherifard3 

 , Karo Khosravi3
, Karo Khosravi3 
 , Amir Azimi3
, Amir Azimi3 
 , Reza Ahmadi3
, Reza Ahmadi3 

 , Tahereh Farkhondeh4
, Tahereh Farkhondeh4 

 , Babak Roshanravan5
, Babak Roshanravan5 

 , Saeed Samarghandian6
, Saeed Samarghandian6 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Student Research Committee, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, Faculty of Medicine, Farhikhtegan Hospital, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran.
3- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Toxicology and Pharmacology, School of Pharmacy, Birjand University of Medical Sciences, Birjand, Iran.
5- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Imam Reza Hospital, Birjand University of Medical Sciences, Birjand, Iran.
6- Department of Medical Physiology, School of Medicine, Neyshabur University of Medical Sciences, Neyshabur, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, Faculty of Medicine, Farhikhtegan Hospital, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran.
3- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
4- Department of Toxicology and Pharmacology, School of Pharmacy, Birjand University of Medical Sciences, Birjand, Iran.
5- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Imam Reza Hospital, Birjand University of Medical Sciences, Birjand, Iran.
6- Department of Medical Physiology, School of Medicine, Neyshabur University of Medical Sciences, Neyshabur, Iran.
Full-Text [PDF 694 kb]
(334 Downloads)
| Abstract (HTML) (808 Views)
Full-Text: (441 Views)
Introduction
Total joint replacement of the lower extremities, or total joint arthroplasty (TJA), is a commonly performed and successful procedure in patients with end-stage arthritis. TJA replaces the degenerative joint with synthetic components to reconstruct the worn joint surface, relieve pain, and improve patient mobility [1]. With the development of surgical techniques and implant designs, the number of total knee or hip arthroplasties (TKA and THA) performed worldwide is significantly increasing [2]. The American Joint Replacement Registry (AJRR) revealed 2 244 587 hip and knee arthroplasties (primary or revision) were performed between 2012 and 2020. The annual report for 2020-2021 has shown approximately 2.4 million hip and knee surgeries conducted during this period. They also represented an 18.3% increase in the procedures conducted compared with the previous year [3]. Therefore, the number of replacement procedures in young and elderly age groups continues to increase, and surgeons expect favorable results from adequately selected patients.
Apart from factors related to surgical techniques, patient-related circumstances also significantly influence the overall outcomes and surgery-associated complications of TJA surgeries [4, 5]. Preexisting neurological conditions have been a challenge for arthroplasty surgeons for a long time, and they have avoided performing joint replacements in patients with neurological conditions. This could be due to potentially higher associated complications in these patients, such as contractures, paresis, altered muscular tone, and muscular imbalance [6, 7]. However, these procedures have been conducted in patients considered unsuitable for arthroplasty in the past [6, 8, 9]. In recent years, TKA and THA have become significantly more common in patients with neurological disorders, and the available evidence has expanded considerably. These surgeries may be helpful in well-chosen individuals to relieve pain and increase functional capacity. However, TJA has been reported to have higher complication rates and lower implant survival rates [6, 7, 10].
Parkinson’s disease (PD) is a neurodegenerative disorder often observed in older individuals. The loss of dopamine and dysfunction of the basal ganglia causes this. PD is associated with a higher risk of falling, gait imbalance, and osteoarthritis (OA) [11, 12]. Therefore, patients with PD may require surgical replacement of the hips or knees. However, studies of TJA in these patients are sparse and limited. Orthopedic surgeons are frequently asked to evaluate the suitability of PD patients for TJA. This study aims to review the recent literature regarding TKA and THA procedures in patients with PD. The results of this study can help surgeons in the challenging setting of TJA in neurologically damaged individuals and increase their understanding of possible complications and outcomes.
TKA
TKA, or total knee replacement, is a practical and cost-efficient surgical option for end-stage knee degeneration. It aims to relieve patients’ pain, restore function, and improve their quality of life (QoL) [13-15]. TKA includes resectioning the knee’s damaged articular surfaces and resurfacing with prosthetic components (metal and polyethylene) [16, 17]. The longevity of knee prostheses is affected by several factors, but a median of 15-20 years lifespan is expected [16]. TKA has been developed over the past decades since the 1970s, when it was first conducted at a hospital for special surgery [18]. Significant advancements in TKA procedures and implant design have resulted in approximately 85%-90% of patients being satisfied with their knee replacement outcomes [19].
TKA designs have demonstrated excellent clinical outcomes and survival rates in patients with knee OA and rheumatoid arthritis (RA) [20]. Although the primary diagnosis commonly associated with TKA is knee OA (KOA), other possible underlying conditions are inflammatory arthritis, fracture, and malignancy [21, 22]. With the increasing prevalence of knee arthritis due to aging populations, the popularity and global demand for TKA is also increasing [23]. By 2030, it is estimated that there will be an 85% increase in the number of TKAs, amounting to approximately 1.26 million procedures, only in the US [24].
In recent years, the number of TKA cases has increased in elderly patients owing to their longer life expectancy. This means more people with underlying diseases are now candidates for TKA [25]. Although TKA can expand the envelope of the function of damaged knees safely and predictably, surgeons are encouraged to ensure that other noninvasive modalities are discussed with the patient. Unresponsive pain to pharmaceutical therapy in OA patients is the most commonly reported indication for TKA in the literature, and knee replacement should only be considered after exhaustion of available nonsurgical and conservative treatments [17, 26].
Total hip arthroplasty (THA)
THA is one of the most significant successes in modern medicine. Hip replacement was first attempted by Professor Themistocles Glück in Germany in 1891. Subsequently, an interposition arthroplasty was performed. This technique involves placing different tissues between the articulating hip surfaces of the damaged hip [27]. Smith-Petersen invented mold arthroplasty in 1925 using glass; however, it proved insufficient to endure the forces that passed through the hip joint. Subsequently, he collaborated with Philip Wiles to develop the first THA using stainless steel, which was affixed to the bone using bolts and screws [28, 29]. Charnley is the father of modern THA. In principle, his low-friction arthroplasty procedure was similar to modern THA, in which the acetabulum and femoral head are removed and substituted with prosthetic implants [30, 31].
Due to the considerable benefits of THA, the utilization of this technique has been increasing, making it one of the most commonly conducted surgeries in this field. It is usually utilized in the advanced stages of OA-associated joint failure. It is one of the most effective orthopedic surgeries to relieve pain and improve QoL in these patients [32, 33]. Other indications include femoral fractures, RA, avascular necrosis, traumatic damage, bone tumors, and their extent [34, 35]. The long-term survival of THA is affected by various factors, most notably the implant design, surgical technique, patient characteristics (such as good preoperative physical function and balanced muscular strength), and surgeon capability [36]. Recent implant modifications, including larger femoral heads, porous metals, and alternative bearings, have been introduced to reduce early and late TJA failure [37]. Therefore, owing to evolving implant design and surgical techniques, even children and patients with complex conditions previously managed by salvage procedures can benefit from total hip replacement [10]. According to the British National Joint Registry, 97.5% of patients reported improved hip pain and function with low surgical complications [38]. Similar to TKA, THA should also be considered after noninvasive therapeutic modalities, such as physical therapy and pain-reducing drugs, have failed.
TJA in neurological disorders
Besides factors related to implant design and surgical techniques, patient-related factors also significantly influence overall outcomes and surgery-associated complications in TJA surgery [4, 5]. Neurological conditions affecting the hip or knee have been a serious challenge for surgeons performing joint replacement since the day these techniques were utilized. A recent study demonstrated that individuals with a pre-existing neurological diagnosis had higher mortality rates, dislocations, and adverse outcomes after hip replacement surgery than controls [39]. This could be due to the increased risk of associated complications, such as contractures, altered muscular tone, and muscular imbalance (ranging from flaccidity to spasticity) [6, 7], as well as altered anatomy and problems in post-surgery rehabilitation. Abnormal muscle tone can also cause early replacement surgery failure due to dislocation and loosening [10]. Zhang and coworkers documented a relatively high prevalence (9%) of prosthesis dislocation after THA in those with neuromuscular conditions [40]. This rate was reported to be higher (up to 13%) in some other investigations [41]. Patients who undergo TJA are also more susceptible to complications, such as falls and fractures, as well as a prolonged hospital stay [42, 43]. Consequently, surgeons avoid performing TJA in patients with severe neurological diseases due to the perceived complexity and concerns over potential complications, most importantly dislocation and loosening [7 44]. For instance, the results of a study highlighted that less than 25% of surgeons conducted more than one THA on cerebral palsy (CP) patients within 9 years [45].
Improved medical management of neurological conditions has led to a longer life expectancy in these patients, who are now more likely to develop OA symptoms. Novel techniques and a better understanding of prosthetic joint biomechanics have broadened TJA indications, extending to populations with neurological conditions [10, 45, 46]. Recent investigations have shown that contrary to conventional perceptions, TJA may be associated with favorable outcomes in neurologically disabled patients. A systematic review of 45 studies with 36 251 THA cases indicated that this procedure is helpful in patients with neurological disorders, decreased pain, and improved function. However, a high complication rate has also been noted, with dislocation being the most reported complication (approximately 10.6%) [7]. Ryu et al. investigated dual mobility THA’s clinical performance and survivorship in elderly patients with neuromuscular conditions (CP, polio, hemiplegia, and PD). They reported that THA may be a practical treatment for femoral neck fractures in these patients. They observed no difference in the dislocation rate between patients with and without neuromuscular conditions treated with THA [4]. Another study demonstrated that TKA can reduce patients’ symptoms and improve functional outcomes, but the complication rate was higher in patients with neurological disorders [6]. It is essential to mention that TJA procedures, especially for those with neurological deficits, should be conducted by specialists with adequate surgery experience [7].
Altogether, there are limited and conflicting results regarding the effectiveness and efficiency of TJA in patients with neurological disorders. Well-designed systematic reviews and general data would assist orthopedic surgeons in surgical planning for patients with neurological conditions considering TJA. In this review, we summarize recent literature regarding the effectiveness and complications of THA/TKA in patients with PD.
Methods
The latest updates from several English databases and search engines (Google Scholar, ScienceDirect, PubMed, Web of Science, and Scopus) were evaluated since January 2018 to identify potentially related articles. English keywords, as well as Boolean operators “AND” and “OR” in addition to advanced search options, were applied as: (Total knee arthroplasty OR total knee replacement AND Parkinson’s disease OR PD) and (total hip arthroplasty OR total hip replacement AND Parkinson’s disease OR PD). Articles without English full text, review articles, case reports, and investigations related to other surgeries or neurological conditions were excluded. After eliminating duplicates and irrelevant papers, careful screening of titles and abstracts was conducted. The full-text versions of the remaining publications were read. Any disagreements between the authors were discussed and resolved.
Results
TJA in patients with PD
PD is a degenerative condition caused by loss of dopamine and dysfunction within the basal ganglia. It is the two most common progressive neurodegenerative disorders among older individuals (after Alzheimer’s disease), and its prevalence is projected to double by 2030 (8.7-9.3 million) [47, 48]. PD is characterized by the presence of both motor (tremors and stiffness) and non-motor (psychiatric symptoms) symptoms [11, 12]. In PD, gait changes occur, starting with reduced step length and increased double-limb support. In advanced cases, reduced postural control and an elevated risk of falling are observed [49]. Patients with PD are at a high risk of falling, with an estimated 60.5% of patients experiencing at least one episode and 39% experiencing recurrent falls. This increased frequency of falls leads to a higher risk of fractures [50]. These patients also have lower bone density, probably due to poor nutritional status and reduced physical activity [51, 52]. Medical advancements have prolonged life expectancy, and people are now more likely to show severe osteopenia and OA symptoms. These conditions increase the risk of falling and fractures and necessitate TJA [53]. However, studies on joint replacement in patients with PD are limited.
Although PD was historically assumed to be a contraindication for TJA [54, 55], an increasing number of joint replacement surgeries are now being performed in these patients [43, 56]. For example, the incidence of THA in patients with PD increased from 946 to 1655 in the US between 2000 and 2014 [42]. However, the outcomes of TJA in PD patients are not entirely known. While some studies reported high postoperative mortality rates and associated complications, such as fractures, dislocations, and a higher need for revision surgeries [57] in PD patients undergoing TJA, more recent investigations suggest better outcomes and no difference in post-TJA complication rates compared to the population [58]. Wang et al. reported that PD patients showed significantly higher rates of postoperative wound infection (surgical site, superficial and periprosthetic) following TJA procedures [59]. However, this may also be because patients with PD have longer hospital stays, which increases the risk of hospital-acquired infections.
Managing orthopedic issues in patients with PD can be challenging due to several factors. These patients have tight muscles, poor bone quality, tremors, and instability, all of which may worsen the outcomes of TJA [54, 59]. Additionally, PD patients are more prone to falling due to their instability, which can lead to postoperative dislocation and fracture [50, 60]. Since orthopedic surgeons are frequently requested to evaluate patients’ suitability for surgical hip or knee replacement, it is crucial to determine the clinical outcomes of TJA in patients with PD [2, 56].
Total hip arthroplasty (THA) in PD patients
Hip fractures are the most common skeletal injuries experienced by patients with PD [54, 61, 62]. A recent study revealed that people with PD have twice the risk of hip fracture than those without this condition [63]. These patients are at higher risk of fractures due to postural instability, reduced bone density, and vitamin D deficiency [64, 65]. Additionally, short- and long-term outcomes of hip fracture, such as post-fracture mortality rate, in patients with PD are worse than those in healthy individuals [66, 67]. Patients with PD also have a higher incidence of degenerative joint disorders and OA due to abnormal stresses around the hip joint. Therefore, these patients may experience severe hip pain and mobility limitations, which may require THA [68, 69].
PD has long been linked with intra- and post-operative challenges in patients after THA. However, now more people with PD are undergoing this procedure due to recent advances in arthroplasty techniques. Although THA improves functional status in PD patients, outcomes are still poorer than those in non-PD patients [57, 70], with higher rates of complications, such as fractures and dislocation [71, 72]. However, patient’s hip dislocation rate after THA is controversial [73]. Some studies reported increased dislocation due to muscle rigidity and gait instability [57, 54], while others demonstrated no difference in dislocation rates following THA in patients with PD and populations [76]. The dislocation rate after THA has been reported to range from 0% to 37% in patients with PD [74, 75]. A study evaluated the potential risk factors for early dislocation after THA and reported that PD was significantly associated with short-term dislocation (OR=1.63) [76]. Several strategies have been developed for dislocation management after THA, such as constrained liner, large femoral head, and dual-mobility implants [77-79]. Dual-mobility cups are used in THA cases with a high instability risk, such as patients with neurological deficits. A previous study showed that cementless implants with dual-mobility bearing surfaces could be associated with acceptable long-term outcomes in patients with PD undergoing primary or revision THA. The follow-up time ranged from 4 to 14 years, and Lazennec et al. observed no dislocations at a mean follow-up of 8.3 years. They reported that although all patients experienced an improvement in their pain, disability increased in most patients (68%) at the latest follow-up, which could be due to disease progression in the long term [80]. Another study revealed that dual-mobility hip arthroplasty had good functional results (efficacy and stability) in PD patients with proximal femoral fractures. Cemented components were used in 9 patients, and cementless components were utilized in another 4. They did not report any prosthesis dislocation among patients [75]. Therefore, THA with dual-mobility implants can provide satisfactory outcomes for patients with PD with a low rate of mechanical complications [79]. It seems that the traditional unwillingness to consider THA in patients with PD may be too conservative because the higher long-term mortality rate may be due to the progressive neurological nature of the disease and not surgery, and those with PD report almost the same outcomes as controls [80, 81].
The choice of optimal implant design, surgical technique, and immediate initiation of rehabilitation can improve outcomes (reduce pain and improve function) in patients undergoing THA [75]. Both the direct anterior approach (DAA) and the posterolateral approach (PLA) are safe and effective for femoral and acetabular reconstruction [82]. However, patients with concomitant PD undergoing PLA have a higher risk of postoperative dislocation due to decreased muscle strength. PLA surgery in these patients may cause hip instability and a higher incidence of dislocation [83]. Berliner et al. also indicated that older age, osteoporosis, and PD are significantly associated with an increased risk of early postoperative periprosthetic femoral fractures following DAA in THA [84]. In another study, Yang et al. investigated the efficacy of DAA versus PLA for THA in 209 patients with PD. They demonstrated that the DAA approach resulted in lower dislocation rate and faster recovery of the hip function. However, DAA was associated with more bleeding and prolonged surgery than PLA, possibly due to the special positions and instruments required for lateral femoral prosthesis installation. They found that elderly patients with PD were more prone to hip dislocation after THA due to limb tremors and muscle tonicity. However, neither the DAA nor PLA group showed any significant difference in hip prosthesis dislocation after surgery [85]. Higgins et al. also showed that DAA was superior to PLA in reducing pain and functional recovery time and the risk of postoperative dislocation in patients with PD [86].
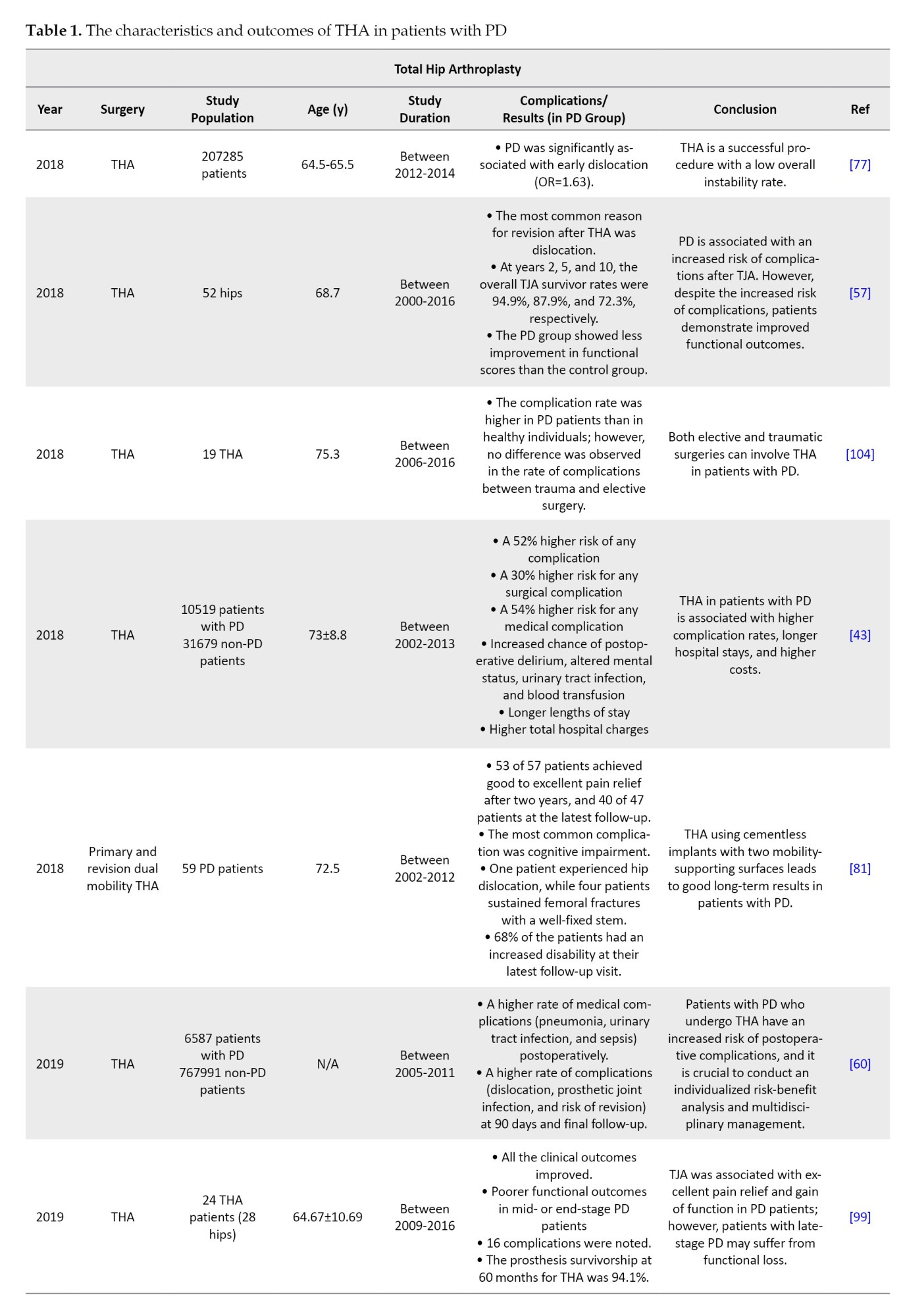
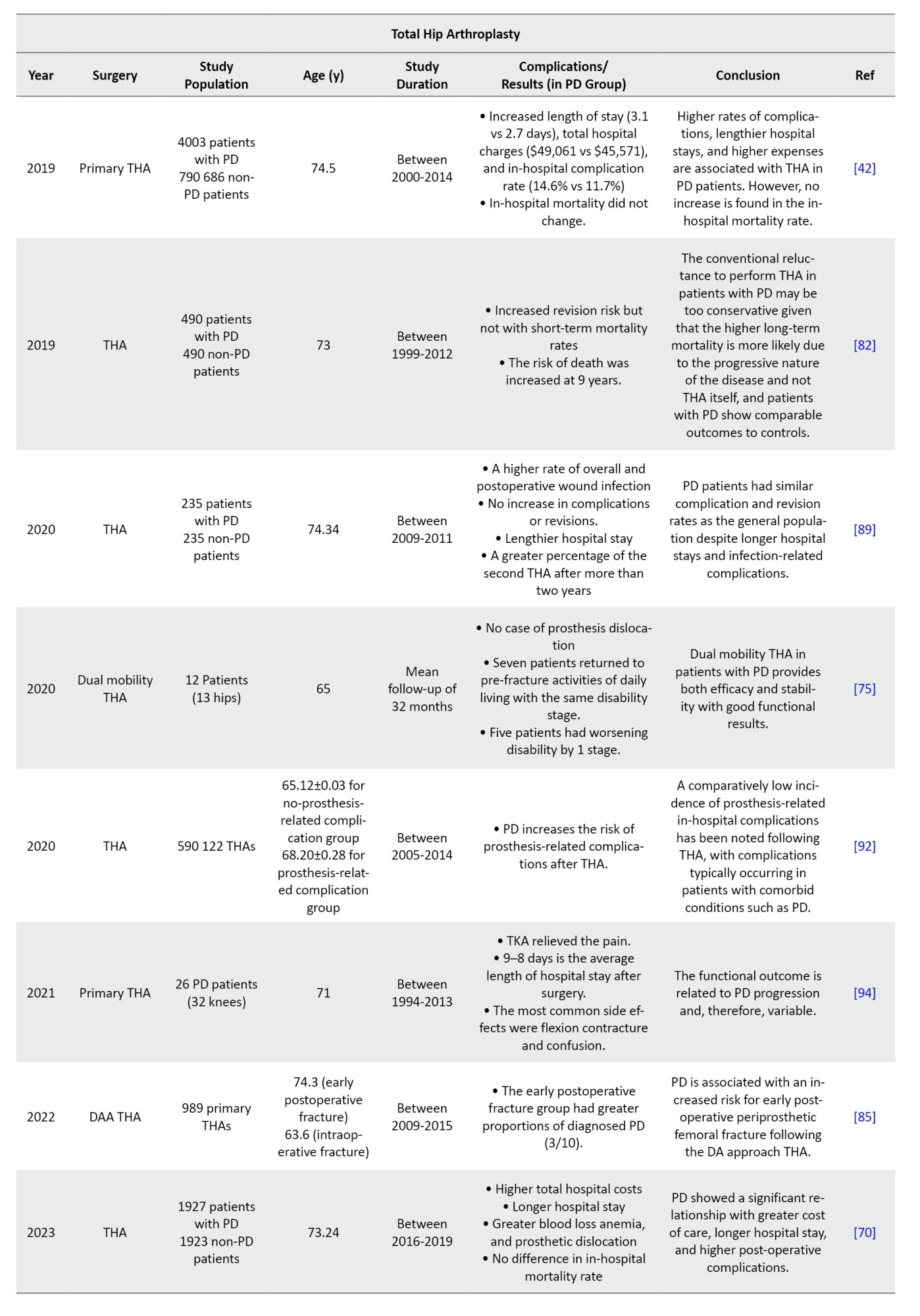
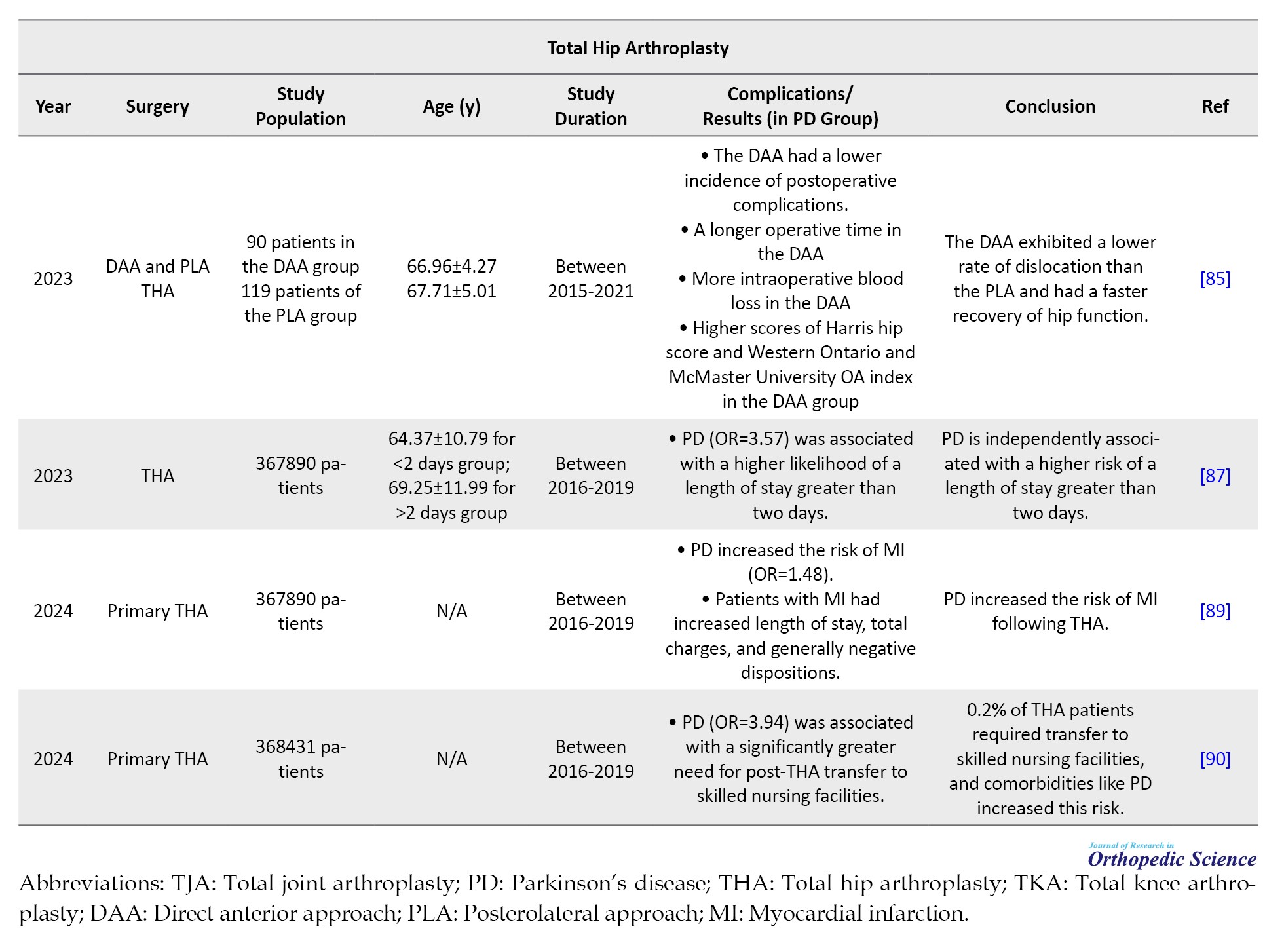
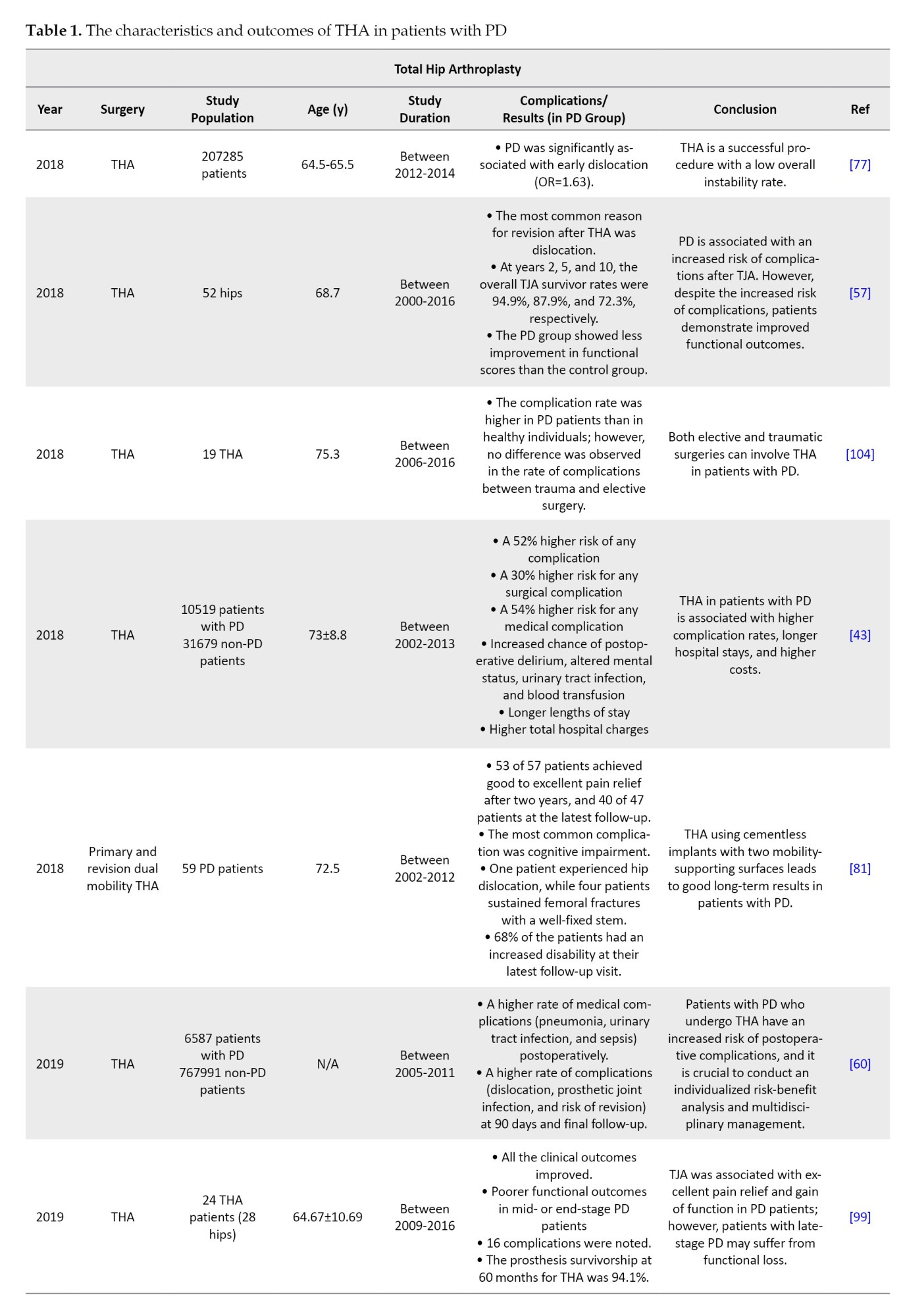
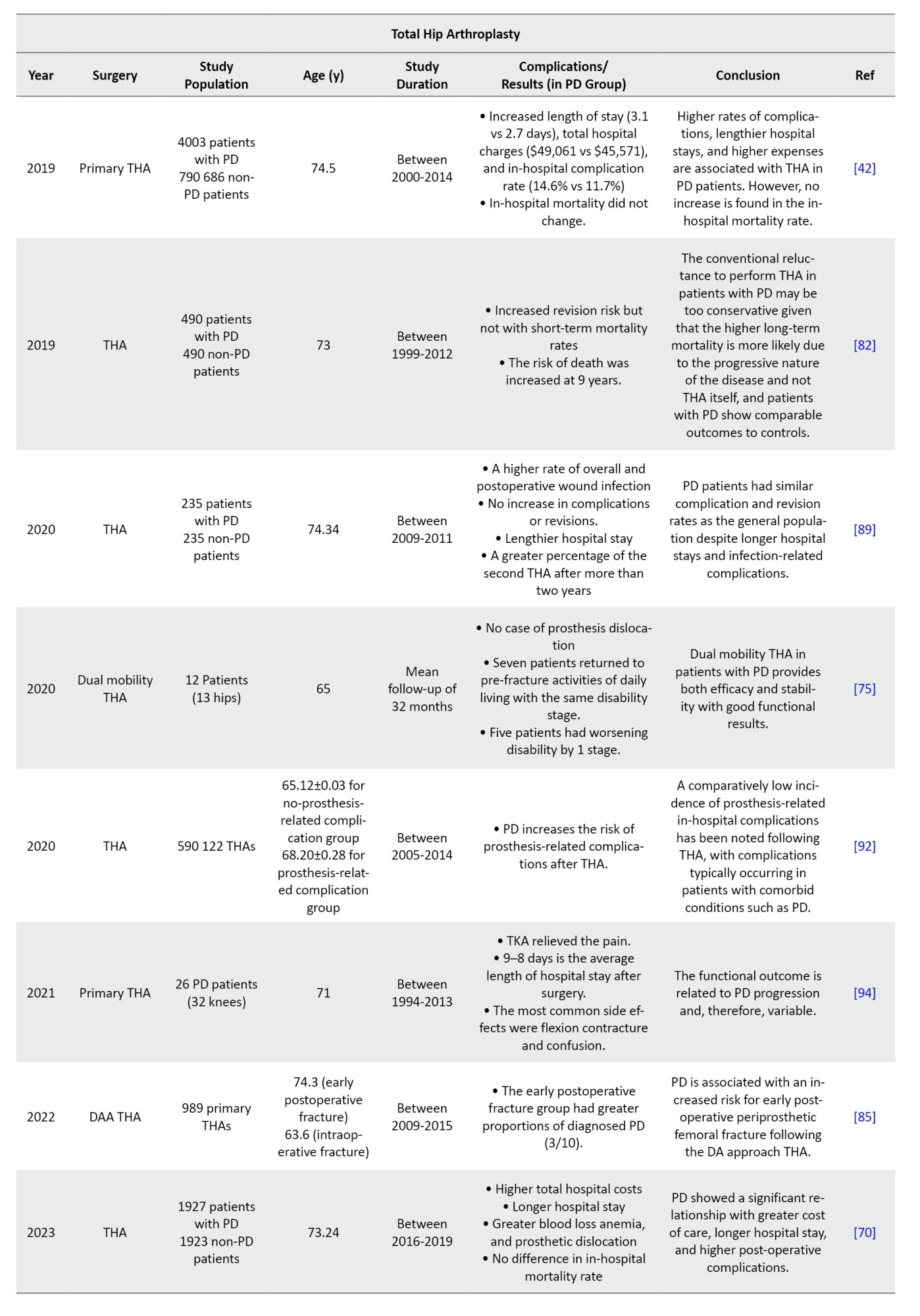
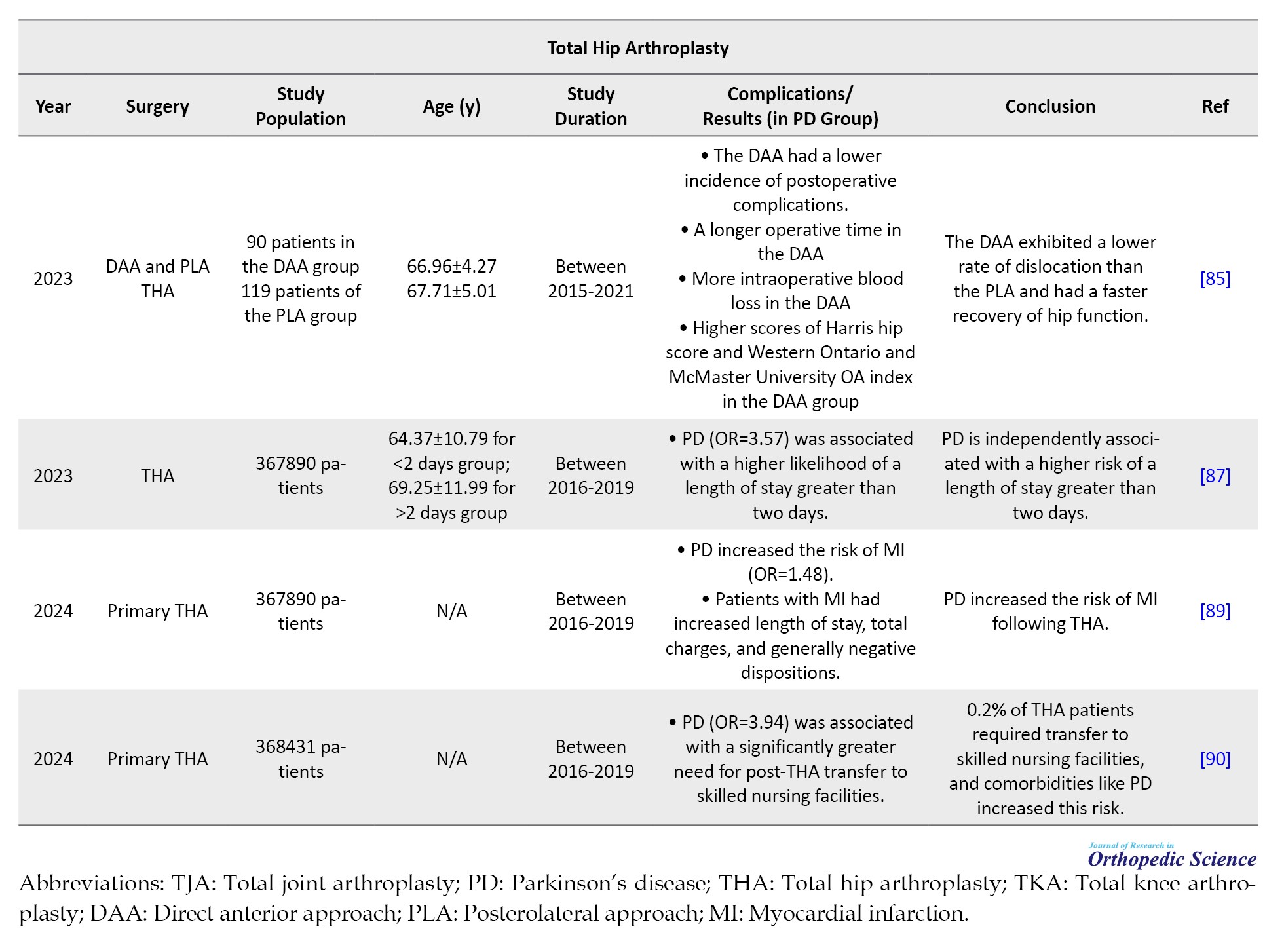
Comorbidities, such as PD, are associated with a longer patient stay after THA [87]. Shah et al. reported that Parkinson’s did not increase the risk of revision surgeries following THA. However, longer hospital stays and infection-related complications have been observed among patients [88]. Another study reported that PD increases the risk of myocardial infarction (MI) after THA and MI patients had longer stays and higher costs than non-MI patients [89]. Viswanathan et al. analyzed the National Inpatient Sample (NIS) database between 2016 and 2019. They found that 0.2% of patients who underwent primary THA required transfer to a skilled nursing facility (SNF). The study also identified PD as one of the comorbidities with the highest likelihood of patients being transferred to SNF (OR=3.94; P<0.001) [90]. In conclusion, most investigations documented poorer outcomes and increased complication rates in patients with PD after THA compared to the general population. Yang et al. suggested that the occurrence of prosthesis-related complications after THA is more frequent in patients with PD or dementia (P<0.0001). The authors also reported that dislocation was the most common complication [91]. Newman et al. demonstrated that PD can increase the risk of perioperative surgical and medical complications after THA (30% and 54%, respectively). They reported that delirium and UTI were more common in patients with PD [43]. Almost all investigations reported short-term mortality rates comparable to those of normal populations. Goel et al. revealed that patients suffering from PD who undergo THA require more expensive care, have to stay longer in hospitals, and have higher chances of experiencing post-surgery complications, such as prosthetic dislocation. However, mortality rates were similar between the two groups [70]. In a matched cohort analysis by Kleiner et al., patients with PD undergoing THA experienced higher complication rates (14.6% vs 11.7%) and longer hospital stays (3.1 vs 2.7 days), but no increase in in-hospital mortality [42]. Wojtowicz et al. reported that although THA did not increase the risk of short-term (90 days and one year) mortality in patients with PD, a higher revision risk and long-term mortality rate were documented after nine years [81]. Two previous investigations reported that patients with PD undergoing THA had a higher mortality rate than those without this neurodegenerative disorder [81, 85]. Considering that PD is a progressive disease affecting patients’ QoL and life expectancy, it is challenging to speculate what proportion of this increased mortality rate could be attributed to PD progression itself rather than the THA operation. Table 1 summarizes the characteristics and outcomes of THA in patients with PD.
Total knee arthroplasty (TKA) in PD patients
Better medical treatment of patients with PD is expected to increase life expectancy, which will increase the number of patients undergoing TKA [92]. Patients with PD often have knee OA. The knee joint poses difficulties for PD patients in the advanced stages of the disease, causing pain, stiffness, and instability that may require TKA [93]. However, associated orthopedic conditions, such as a high risk of falls and fractures, rigidity, and poor bone quality in PD patients, can make THA challenging for arthroplasty surgeons [53, 72]. Additionally, PD symptoms, such as tremors, shuffling gait, and instability, can increase post-surgical complications and decrease TKA functional outcomes. Moreover, although knee arthroplasty can improve mechanical problems of the knee, reduce pain, and improve function, it cannot prevent the progression of PD [94].
Recent studies show that arthroplasty procedures can provide considerable pain relief, but data on their outcomes and complications in the PD population still needs to be improved [95, 96]. TKA is a successful treatment for reducing pain in weight-bearing joints. However, TKA’s efficacy with severe PD remains a concern. Several studies have evaluated functional outcomes following TKA in the PD population, each with contradicting results. Although TKA can provide favorable outcomes for patients with PD, those in the advanced stages may experience worsening motor features. Some studies demonstrated poor functional improvement after joint replacement surgery in PD patients [72, 97]. Noor et al. determined the significance of TKA in patients with PD. They found that TKA improved PD patients’ range of motion (ROM) and stability. Surgery also reduces pain and stiffness and improves physical and mental well-being. However, motor functional outcomes remain poor [98]. Rong et al. found that patients with PD who underwent THA or TKA (24 THA and 18 TKA patients) experienced significant improvements in pain and function. The prosthesis survivorship rates for THA and TKA were reported to be 94.1% and 87.5%, respectively (after 60 months). However, those in the mid- or end-stage of the disease have poor functional outcomes [99]. Baek et al. also demonstrated that TKA in patients with PD was associated with weak functional outcomes and increased mortality rates during follow-up. The mortality rates in the Parkinson’s and control groups were significantly different (31% and 6.9%, respectively). Additionally, they showed that the functional results of TKA in patients were closely associated with the progression of PD [100]. In another study, Montiel Terrón et al. [93] retrospectively examined 26 patients with PD and OA who underwent TKA. The mean follow-up was 3.5 years (2–9 years). They found that TKA reduced pain and improved ROM in patients with PD, which aligns with previous investigations [57, 96, 101]. They also demonstrated that the rate of motor symptom progression diminishes with advancing PD. While patients in the early stages had a higher chance of functional outcome deterioration, patients with more progressive PD tended to remain stable after five years. They had a better outcome after surgery [93]. Therefore, it can be concluded that the functional outcomes of PD patients after TKA are correlated with the severity and progression of PD, and doctors should help delay PD progression to optimize TJA outcomes [25, 71, 99].
Most studies have revealed that patients with PD who undergo TKA experience more complications, longer hospital stays, and higher costs than the normal population [26, 102, 103]. Sharma et al. reported that lower extremity TJA (THA and TKA) in patients with PD is associated with higher perioperative complication rates than in those without this neurodegenerative disorder; however, no significant difference was observed in complication rates between elective and trauma surgery settings. They reported a very low local complication rate, with only one local complication in each group (elective and traumatic surgery) [104]. Another study also demonstrated that PD is associated with an increased risk of complications following TJA (52 hips and 71 knees), mostly periprosthetic infection, fracture, and dislocation [57]. The incidence of periprosthetic joint infection has been documented in the literature to be 0.92% and 0.88% after TKA and THA, respectively [105]. Additionally, it has been reported that the dislocation rate following THA ranges from 1% to 3%, while the periprosthetic fracture rate is 0.6% [106, 107]. However, these complications have been reported to be higher with PD payments. Rondon et al. reported that 23.6% of PD patients required revision surgery in an average follow-up of 5.3 years. The survivorship of knee implants at years 5 and 10 was 89.8% and 66.2%, respectively, and hip implant survivorship was 85.3% and 78.7%, respectively. TJA improved functional outcomes in PD patients but not individuals without PD [57]. In a retrospective study of patients who underwent TKA with and without PD, Cheppalli et al. reported an advanced risk of periprosthetic mechanical problems and an increased cost of care patients with PD [108]. Marchand et al. also demonstrated that PD patients undergoing primary TKA have more medical (4.21 vs 1.24%; OR=3.50) and implant-related (5.09 vs 3.15%; OR=1.64) complications, higher readmission rates, and costs compared with controls [109]. Another study indicated that PD increased hospitalization time (6.5%), charge (3.05%), and perioperative complications after TKA. Since most of these complications can be controlled, multi-specialty patient optimization is required [25]. Altogether, these results suggest that patients with PD can benefit from perioperative consultation with a neurological specialist to reduce complications and improve outcomes after TJA.
While the literature reports high complication rates in PD patients undergoing TKA, some investigations demonstrated no significant increase in the studied populations’ complications. Wong et al. compared the outcomes of TKA in those with PD and those without PD. They suggested that PD is not a contraindication for TKA; however, PD patients show outcomes equivalent to those of the general population. No mortalities occurred during the follow-up period. They reported that PD patients exhibited functional outcomes and complications comparable to controls [96]. Kleiner et al. found that patients with PD who underwent TKA experienced slightly longer hospitalizations and higher costs. However, no increase was found in complications or mortality rates, suggesting that patients with PD can be safely considered for TKA [102]. Another study reported that TKA is a successful surgical option for KOA in patients with PD, with comparable results to the population despite the severity and progression of PD. They reported that preoperative function was low in patients with high PD severity, while postoperative function was comparable to that in the severe PD group [101]. Surgery is a suggested treatment for end-stage knee OA with satisfactory results, which may improve patients’ QoL. Studies have reported that TKA can improve the knee function in patients with PD. However, the positive impact of the procedure was less than that in non-PD patients [57]. In 2022, Zong et al. found that TKA did not improve QoL outcomes in patients with KOA and PD, except for a subtle reduction in pain-related disability. Although the two groups had similar preoperative QoL outcomes, those with PD had worse QoL on all three measures (EuroQol five-dimension [EQ-5D], pain and disability questionnaire [PDQ], and patient health questionnaire-9 [PHQ-9]) at the last follow-up [110]. Another study published in 2021 reported that although individuals with PD have diminished knee function and poorer QoL after TKA, they still experience significant functional improvements and high satisfaction compared to their preoperative situation. The complication and mortality rates were higher in PD patients than in the control group (26.3% vs 10.5% and 15.8% vs 5.3%, respectively) [111].
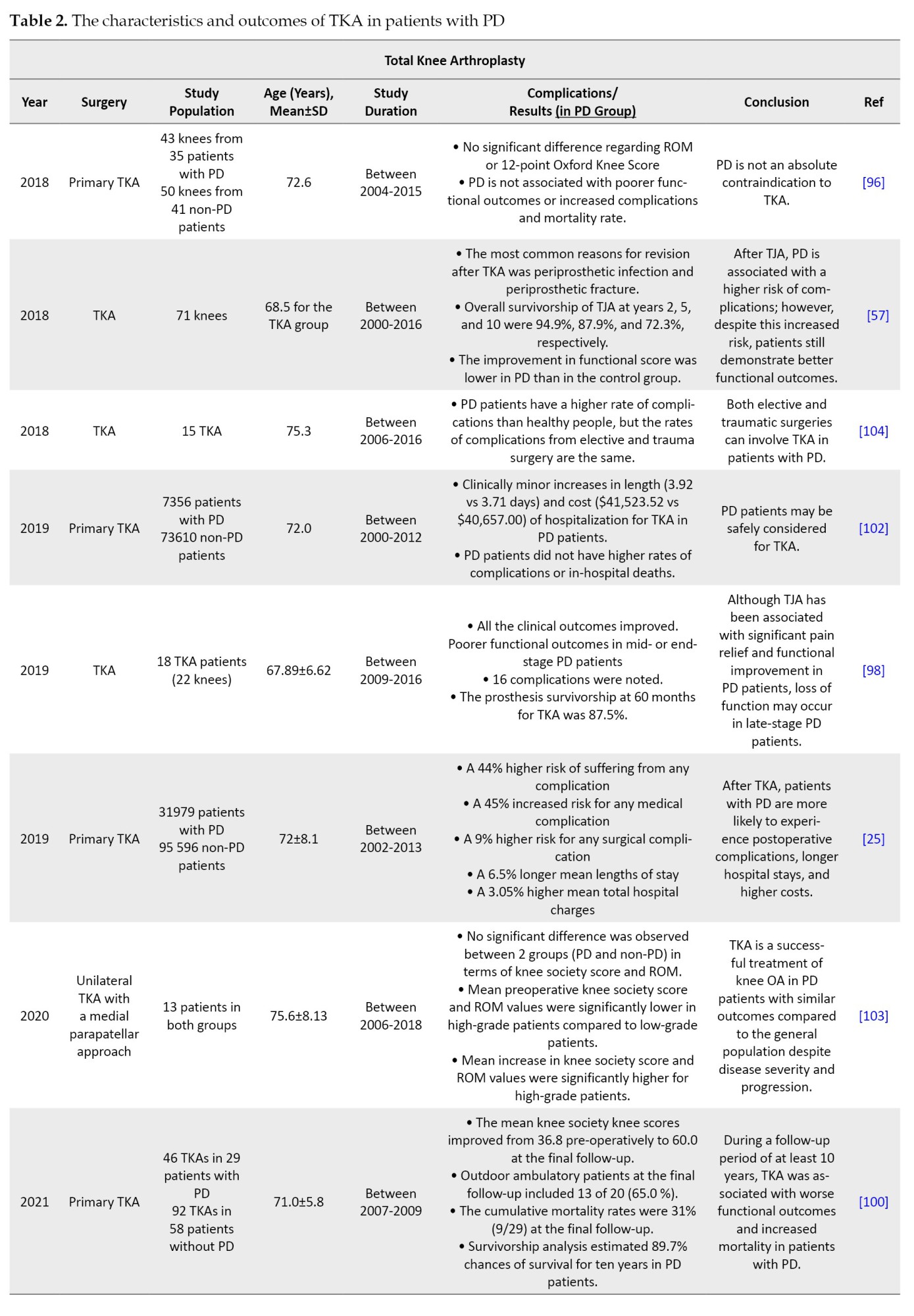
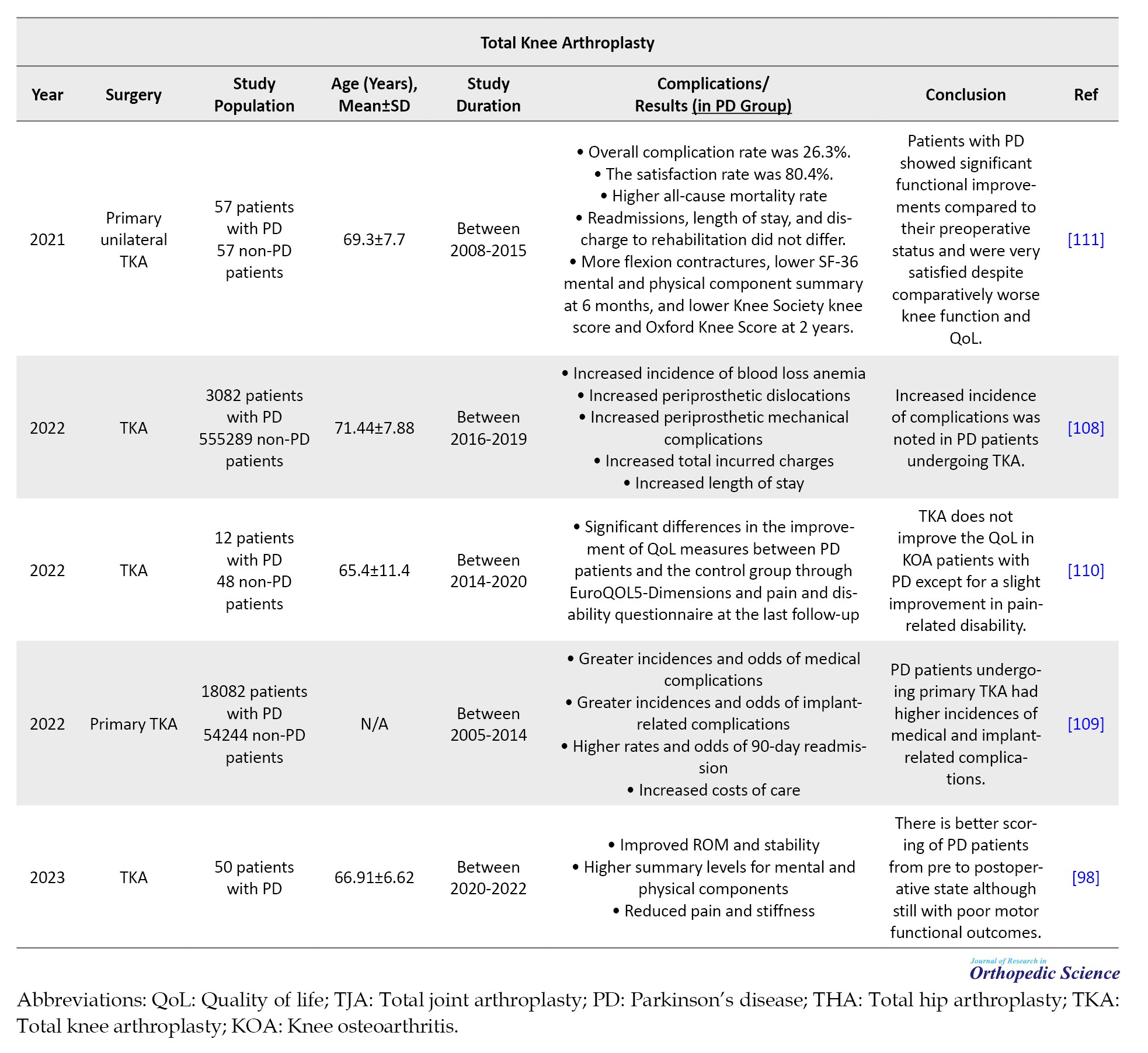
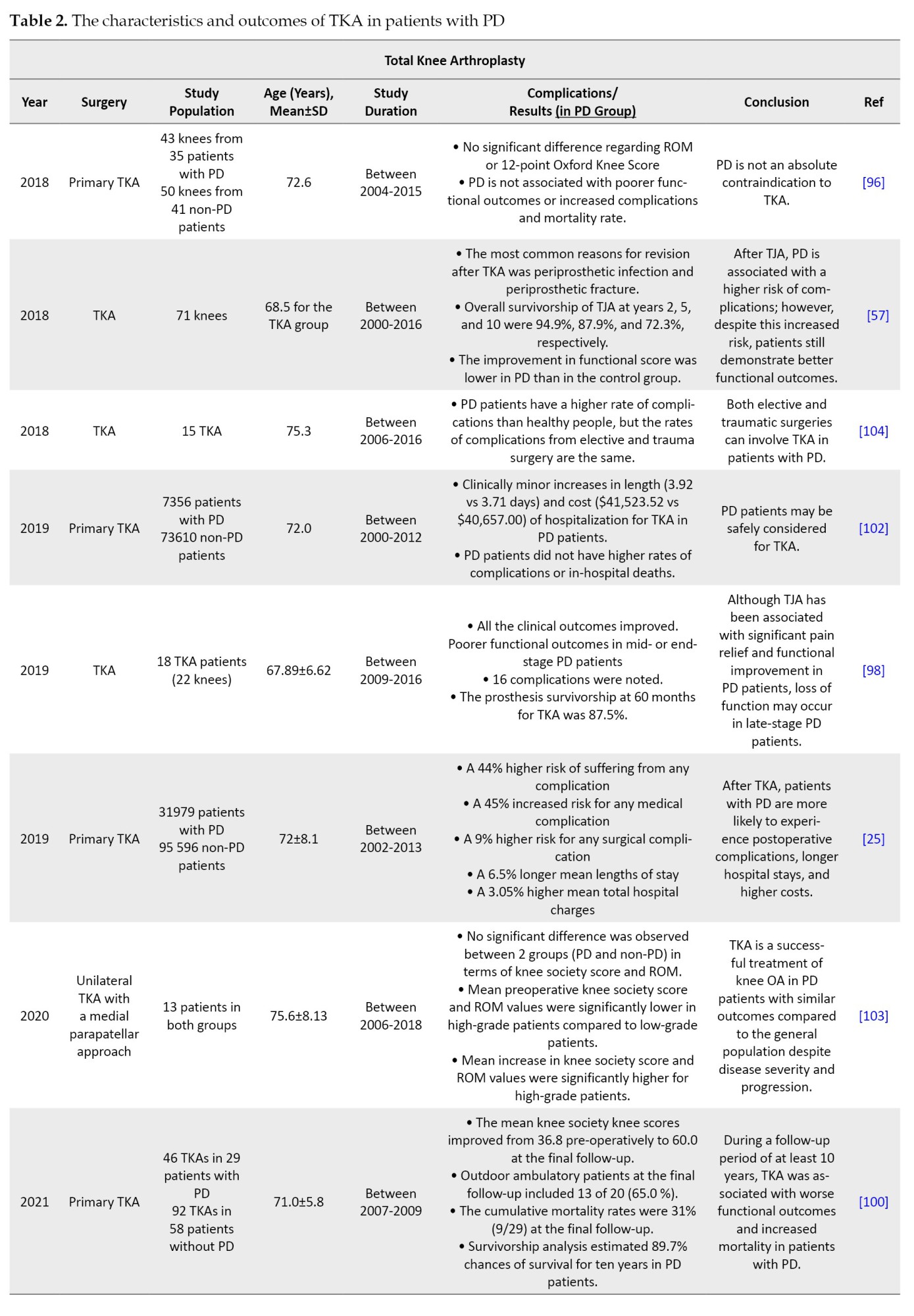
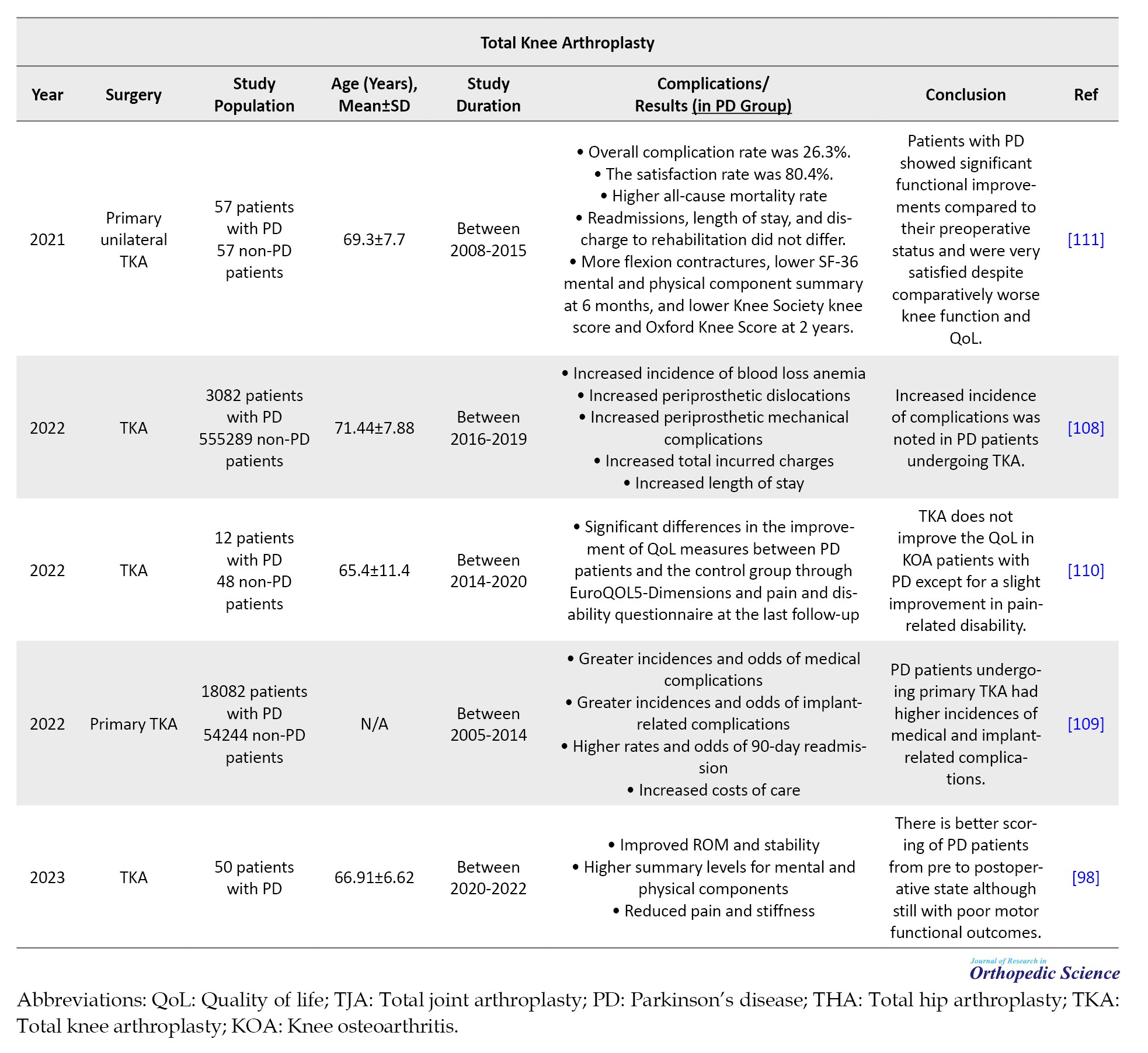
Although not comparable with control groups, some studies demonstrated low complication rates and promising functional outcomes in patients with PD compared to their condition before the surgery. This led to their satisfaction with the outcomes. These results emphasize that TKA remains a potential surgical option for OA in this expanding patient population. However, evaluating the long-term consequences of TKA in these studies was difficult due to the short follow-up period. Therefore, according to the available literature and controversial results, the necessity of TJA in the population of patients with PD should be evaluated, carefully depending on individual needs and conditions. In conclusion, in appropriately selected patients, PD severity and progression do not dramatically affect the outcomes of TJA. Although the effectiveness of TJA in individuals with PD remains a concern, we believe that PD should not prevent surgeons from performing TKA. Table 2 summarizes the characteristics and outcomes of TKA in patients with PD.
Conclusion
Joint arthroplasty is a safe and effective surgical procedure for treating end-stage OA. It can reduce pain, improve ROM, and enhance mobility and function in patients who do not respond to conservative intervention. PD patients have been found to have a higher complication rate after TJA, and the indication of TJA in patients with PD is a matter of debate due to the limited availability of consistent outcomes in existing publications. The available literature consists of a small number of retrospective patient cases, with significant variation in the disease stage and lack of adequate monitoring during postoperative follow-up, all contributing to the absence of a consensus. It is challenging to describe a straightforward approach for patients since PD is a complex condition with non-linear progression rates and considering multiple factors, such as sex, time since diagnosis, occurrence of falls, and response to medical treatment. Consequently, it is difficult to provide recommendations that meet realistic expectations. Surgery is not recommended until pain intensity and features careful analysis and failure of conservative steps. According to the information presented in the existing literature, TKA and THA can be considered safe procedures for patients with PD in terms of mortality rate and short-term complications. However, most studies have reported increased complications (mostly fracture and dislocation), prolonged hospital stays, and escalated costs in these patients.
Ethical Considerations
Compliance with ethical guidelines
This article is a review with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Alireza Ghanbari, Abolfazl Bagherifard, and Babak Roshanravan; Collection, assembly, and data extraction: Hooman Yahyazadeh, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Writing the original draft: Alireza Ghanbari, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Review and editing: Alireza Ghanbari, Hooman Yahyazadeh, Abolfazl Bagherifard, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Supervision: Abolfazl Bagherifard, and Babak Roshanravan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all individuals who helped us develop this research.
References
Total joint replacement of the lower extremities, or total joint arthroplasty (TJA), is a commonly performed and successful procedure in patients with end-stage arthritis. TJA replaces the degenerative joint with synthetic components to reconstruct the worn joint surface, relieve pain, and improve patient mobility [1]. With the development of surgical techniques and implant designs, the number of total knee or hip arthroplasties (TKA and THA) performed worldwide is significantly increasing [2]. The American Joint Replacement Registry (AJRR) revealed 2 244 587 hip and knee arthroplasties (primary or revision) were performed between 2012 and 2020. The annual report for 2020-2021 has shown approximately 2.4 million hip and knee surgeries conducted during this period. They also represented an 18.3% increase in the procedures conducted compared with the previous year [3]. Therefore, the number of replacement procedures in young and elderly age groups continues to increase, and surgeons expect favorable results from adequately selected patients.
Apart from factors related to surgical techniques, patient-related circumstances also significantly influence the overall outcomes and surgery-associated complications of TJA surgeries [4, 5]. Preexisting neurological conditions have been a challenge for arthroplasty surgeons for a long time, and they have avoided performing joint replacements in patients with neurological conditions. This could be due to potentially higher associated complications in these patients, such as contractures, paresis, altered muscular tone, and muscular imbalance [6, 7]. However, these procedures have been conducted in patients considered unsuitable for arthroplasty in the past [6, 8, 9]. In recent years, TKA and THA have become significantly more common in patients with neurological disorders, and the available evidence has expanded considerably. These surgeries may be helpful in well-chosen individuals to relieve pain and increase functional capacity. However, TJA has been reported to have higher complication rates and lower implant survival rates [6, 7, 10].
Parkinson’s disease (PD) is a neurodegenerative disorder often observed in older individuals. The loss of dopamine and dysfunction of the basal ganglia causes this. PD is associated with a higher risk of falling, gait imbalance, and osteoarthritis (OA) [11, 12]. Therefore, patients with PD may require surgical replacement of the hips or knees. However, studies of TJA in these patients are sparse and limited. Orthopedic surgeons are frequently asked to evaluate the suitability of PD patients for TJA. This study aims to review the recent literature regarding TKA and THA procedures in patients with PD. The results of this study can help surgeons in the challenging setting of TJA in neurologically damaged individuals and increase their understanding of possible complications and outcomes.
TKA
TKA, or total knee replacement, is a practical and cost-efficient surgical option for end-stage knee degeneration. It aims to relieve patients’ pain, restore function, and improve their quality of life (QoL) [13-15]. TKA includes resectioning the knee’s damaged articular surfaces and resurfacing with prosthetic components (metal and polyethylene) [16, 17]. The longevity of knee prostheses is affected by several factors, but a median of 15-20 years lifespan is expected [16]. TKA has been developed over the past decades since the 1970s, when it was first conducted at a hospital for special surgery [18]. Significant advancements in TKA procedures and implant design have resulted in approximately 85%-90% of patients being satisfied with their knee replacement outcomes [19].
TKA designs have demonstrated excellent clinical outcomes and survival rates in patients with knee OA and rheumatoid arthritis (RA) [20]. Although the primary diagnosis commonly associated with TKA is knee OA (KOA), other possible underlying conditions are inflammatory arthritis, fracture, and malignancy [21, 22]. With the increasing prevalence of knee arthritis due to aging populations, the popularity and global demand for TKA is also increasing [23]. By 2030, it is estimated that there will be an 85% increase in the number of TKAs, amounting to approximately 1.26 million procedures, only in the US [24].
In recent years, the number of TKA cases has increased in elderly patients owing to their longer life expectancy. This means more people with underlying diseases are now candidates for TKA [25]. Although TKA can expand the envelope of the function of damaged knees safely and predictably, surgeons are encouraged to ensure that other noninvasive modalities are discussed with the patient. Unresponsive pain to pharmaceutical therapy in OA patients is the most commonly reported indication for TKA in the literature, and knee replacement should only be considered after exhaustion of available nonsurgical and conservative treatments [17, 26].
Total hip arthroplasty (THA)
THA is one of the most significant successes in modern medicine. Hip replacement was first attempted by Professor Themistocles Glück in Germany in 1891. Subsequently, an interposition arthroplasty was performed. This technique involves placing different tissues between the articulating hip surfaces of the damaged hip [27]. Smith-Petersen invented mold arthroplasty in 1925 using glass; however, it proved insufficient to endure the forces that passed through the hip joint. Subsequently, he collaborated with Philip Wiles to develop the first THA using stainless steel, which was affixed to the bone using bolts and screws [28, 29]. Charnley is the father of modern THA. In principle, his low-friction arthroplasty procedure was similar to modern THA, in which the acetabulum and femoral head are removed and substituted with prosthetic implants [30, 31].
Due to the considerable benefits of THA, the utilization of this technique has been increasing, making it one of the most commonly conducted surgeries in this field. It is usually utilized in the advanced stages of OA-associated joint failure. It is one of the most effective orthopedic surgeries to relieve pain and improve QoL in these patients [32, 33]. Other indications include femoral fractures, RA, avascular necrosis, traumatic damage, bone tumors, and their extent [34, 35]. The long-term survival of THA is affected by various factors, most notably the implant design, surgical technique, patient characteristics (such as good preoperative physical function and balanced muscular strength), and surgeon capability [36]. Recent implant modifications, including larger femoral heads, porous metals, and alternative bearings, have been introduced to reduce early and late TJA failure [37]. Therefore, owing to evolving implant design and surgical techniques, even children and patients with complex conditions previously managed by salvage procedures can benefit from total hip replacement [10]. According to the British National Joint Registry, 97.5% of patients reported improved hip pain and function with low surgical complications [38]. Similar to TKA, THA should also be considered after noninvasive therapeutic modalities, such as physical therapy and pain-reducing drugs, have failed.
TJA in neurological disorders
Besides factors related to implant design and surgical techniques, patient-related factors also significantly influence overall outcomes and surgery-associated complications in TJA surgery [4, 5]. Neurological conditions affecting the hip or knee have been a serious challenge for surgeons performing joint replacement since the day these techniques were utilized. A recent study demonstrated that individuals with a pre-existing neurological diagnosis had higher mortality rates, dislocations, and adverse outcomes after hip replacement surgery than controls [39]. This could be due to the increased risk of associated complications, such as contractures, altered muscular tone, and muscular imbalance (ranging from flaccidity to spasticity) [6, 7], as well as altered anatomy and problems in post-surgery rehabilitation. Abnormal muscle tone can also cause early replacement surgery failure due to dislocation and loosening [10]. Zhang and coworkers documented a relatively high prevalence (9%) of prosthesis dislocation after THA in those with neuromuscular conditions [40]. This rate was reported to be higher (up to 13%) in some other investigations [41]. Patients who undergo TJA are also more susceptible to complications, such as falls and fractures, as well as a prolonged hospital stay [42, 43]. Consequently, surgeons avoid performing TJA in patients with severe neurological diseases due to the perceived complexity and concerns over potential complications, most importantly dislocation and loosening [7 44]. For instance, the results of a study highlighted that less than 25% of surgeons conducted more than one THA on cerebral palsy (CP) patients within 9 years [45].
Improved medical management of neurological conditions has led to a longer life expectancy in these patients, who are now more likely to develop OA symptoms. Novel techniques and a better understanding of prosthetic joint biomechanics have broadened TJA indications, extending to populations with neurological conditions [10, 45, 46]. Recent investigations have shown that contrary to conventional perceptions, TJA may be associated with favorable outcomes in neurologically disabled patients. A systematic review of 45 studies with 36 251 THA cases indicated that this procedure is helpful in patients with neurological disorders, decreased pain, and improved function. However, a high complication rate has also been noted, with dislocation being the most reported complication (approximately 10.6%) [7]. Ryu et al. investigated dual mobility THA’s clinical performance and survivorship in elderly patients with neuromuscular conditions (CP, polio, hemiplegia, and PD). They reported that THA may be a practical treatment for femoral neck fractures in these patients. They observed no difference in the dislocation rate between patients with and without neuromuscular conditions treated with THA [4]. Another study demonstrated that TKA can reduce patients’ symptoms and improve functional outcomes, but the complication rate was higher in patients with neurological disorders [6]. It is essential to mention that TJA procedures, especially for those with neurological deficits, should be conducted by specialists with adequate surgery experience [7].
Altogether, there are limited and conflicting results regarding the effectiveness and efficiency of TJA in patients with neurological disorders. Well-designed systematic reviews and general data would assist orthopedic surgeons in surgical planning for patients with neurological conditions considering TJA. In this review, we summarize recent literature regarding the effectiveness and complications of THA/TKA in patients with PD.
Methods
The latest updates from several English databases and search engines (Google Scholar, ScienceDirect, PubMed, Web of Science, and Scopus) were evaluated since January 2018 to identify potentially related articles. English keywords, as well as Boolean operators “AND” and “OR” in addition to advanced search options, were applied as: (Total knee arthroplasty OR total knee replacement AND Parkinson’s disease OR PD) and (total hip arthroplasty OR total hip replacement AND Parkinson’s disease OR PD). Articles without English full text, review articles, case reports, and investigations related to other surgeries or neurological conditions were excluded. After eliminating duplicates and irrelevant papers, careful screening of titles and abstracts was conducted. The full-text versions of the remaining publications were read. Any disagreements between the authors were discussed and resolved.
Results
TJA in patients with PD
PD is a degenerative condition caused by loss of dopamine and dysfunction within the basal ganglia. It is the two most common progressive neurodegenerative disorders among older individuals (after Alzheimer’s disease), and its prevalence is projected to double by 2030 (8.7-9.3 million) [47, 48]. PD is characterized by the presence of both motor (tremors and stiffness) and non-motor (psychiatric symptoms) symptoms [11, 12]. In PD, gait changes occur, starting with reduced step length and increased double-limb support. In advanced cases, reduced postural control and an elevated risk of falling are observed [49]. Patients with PD are at a high risk of falling, with an estimated 60.5% of patients experiencing at least one episode and 39% experiencing recurrent falls. This increased frequency of falls leads to a higher risk of fractures [50]. These patients also have lower bone density, probably due to poor nutritional status and reduced physical activity [51, 52]. Medical advancements have prolonged life expectancy, and people are now more likely to show severe osteopenia and OA symptoms. These conditions increase the risk of falling and fractures and necessitate TJA [53]. However, studies on joint replacement in patients with PD are limited.
Although PD was historically assumed to be a contraindication for TJA [54, 55], an increasing number of joint replacement surgeries are now being performed in these patients [43, 56]. For example, the incidence of THA in patients with PD increased from 946 to 1655 in the US between 2000 and 2014 [42]. However, the outcomes of TJA in PD patients are not entirely known. While some studies reported high postoperative mortality rates and associated complications, such as fractures, dislocations, and a higher need for revision surgeries [57] in PD patients undergoing TJA, more recent investigations suggest better outcomes and no difference in post-TJA complication rates compared to the population [58]. Wang et al. reported that PD patients showed significantly higher rates of postoperative wound infection (surgical site, superficial and periprosthetic) following TJA procedures [59]. However, this may also be because patients with PD have longer hospital stays, which increases the risk of hospital-acquired infections.
Managing orthopedic issues in patients with PD can be challenging due to several factors. These patients have tight muscles, poor bone quality, tremors, and instability, all of which may worsen the outcomes of TJA [54, 59]. Additionally, PD patients are more prone to falling due to their instability, which can lead to postoperative dislocation and fracture [50, 60]. Since orthopedic surgeons are frequently requested to evaluate patients’ suitability for surgical hip or knee replacement, it is crucial to determine the clinical outcomes of TJA in patients with PD [2, 56].
Total hip arthroplasty (THA) in PD patients
Hip fractures are the most common skeletal injuries experienced by patients with PD [54, 61, 62]. A recent study revealed that people with PD have twice the risk of hip fracture than those without this condition [63]. These patients are at higher risk of fractures due to postural instability, reduced bone density, and vitamin D deficiency [64, 65]. Additionally, short- and long-term outcomes of hip fracture, such as post-fracture mortality rate, in patients with PD are worse than those in healthy individuals [66, 67]. Patients with PD also have a higher incidence of degenerative joint disorders and OA due to abnormal stresses around the hip joint. Therefore, these patients may experience severe hip pain and mobility limitations, which may require THA [68, 69].
PD has long been linked with intra- and post-operative challenges in patients after THA. However, now more people with PD are undergoing this procedure due to recent advances in arthroplasty techniques. Although THA improves functional status in PD patients, outcomes are still poorer than those in non-PD patients [57, 70], with higher rates of complications, such as fractures and dislocation [71, 72]. However, patient’s hip dislocation rate after THA is controversial [73]. Some studies reported increased dislocation due to muscle rigidity and gait instability [57, 54], while others demonstrated no difference in dislocation rates following THA in patients with PD and populations [76]. The dislocation rate after THA has been reported to range from 0% to 37% in patients with PD [74, 75]. A study evaluated the potential risk factors for early dislocation after THA and reported that PD was significantly associated with short-term dislocation (OR=1.63) [76]. Several strategies have been developed for dislocation management after THA, such as constrained liner, large femoral head, and dual-mobility implants [77-79]. Dual-mobility cups are used in THA cases with a high instability risk, such as patients with neurological deficits. A previous study showed that cementless implants with dual-mobility bearing surfaces could be associated with acceptable long-term outcomes in patients with PD undergoing primary or revision THA. The follow-up time ranged from 4 to 14 years, and Lazennec et al. observed no dislocations at a mean follow-up of 8.3 years. They reported that although all patients experienced an improvement in their pain, disability increased in most patients (68%) at the latest follow-up, which could be due to disease progression in the long term [80]. Another study revealed that dual-mobility hip arthroplasty had good functional results (efficacy and stability) in PD patients with proximal femoral fractures. Cemented components were used in 9 patients, and cementless components were utilized in another 4. They did not report any prosthesis dislocation among patients [75]. Therefore, THA with dual-mobility implants can provide satisfactory outcomes for patients with PD with a low rate of mechanical complications [79]. It seems that the traditional unwillingness to consider THA in patients with PD may be too conservative because the higher long-term mortality rate may be due to the progressive neurological nature of the disease and not surgery, and those with PD report almost the same outcomes as controls [80, 81].
The choice of optimal implant design, surgical technique, and immediate initiation of rehabilitation can improve outcomes (reduce pain and improve function) in patients undergoing THA [75]. Both the direct anterior approach (DAA) and the posterolateral approach (PLA) are safe and effective for femoral and acetabular reconstruction [82]. However, patients with concomitant PD undergoing PLA have a higher risk of postoperative dislocation due to decreased muscle strength. PLA surgery in these patients may cause hip instability and a higher incidence of dislocation [83]. Berliner et al. also indicated that older age, osteoporosis, and PD are significantly associated with an increased risk of early postoperative periprosthetic femoral fractures following DAA in THA [84]. In another study, Yang et al. investigated the efficacy of DAA versus PLA for THA in 209 patients with PD. They demonstrated that the DAA approach resulted in lower dislocation rate and faster recovery of the hip function. However, DAA was associated with more bleeding and prolonged surgery than PLA, possibly due to the special positions and instruments required for lateral femoral prosthesis installation. They found that elderly patients with PD were more prone to hip dislocation after THA due to limb tremors and muscle tonicity. However, neither the DAA nor PLA group showed any significant difference in hip prosthesis dislocation after surgery [85]. Higgins et al. also showed that DAA was superior to PLA in reducing pain and functional recovery time and the risk of postoperative dislocation in patients with PD [86].
Comorbidities, such as PD, are associated with a longer patient stay after THA [87]. Shah et al. reported that Parkinson’s did not increase the risk of revision surgeries following THA. However, longer hospital stays and infection-related complications have been observed among patients [88]. Another study reported that PD increases the risk of myocardial infarction (MI) after THA and MI patients had longer stays and higher costs than non-MI patients [89]. Viswanathan et al. analyzed the National Inpatient Sample (NIS) database between 2016 and 2019. They found that 0.2% of patients who underwent primary THA required transfer to a skilled nursing facility (SNF). The study also identified PD as one of the comorbidities with the highest likelihood of patients being transferred to SNF (OR=3.94; P<0.001) [90]. In conclusion, most investigations documented poorer outcomes and increased complication rates in patients with PD after THA compared to the general population. Yang et al. suggested that the occurrence of prosthesis-related complications after THA is more frequent in patients with PD or dementia (P<0.0001). The authors also reported that dislocation was the most common complication [91]. Newman et al. demonstrated that PD can increase the risk of perioperative surgical and medical complications after THA (30% and 54%, respectively). They reported that delirium and UTI were more common in patients with PD [43]. Almost all investigations reported short-term mortality rates comparable to those of normal populations. Goel et al. revealed that patients suffering from PD who undergo THA require more expensive care, have to stay longer in hospitals, and have higher chances of experiencing post-surgery complications, such as prosthetic dislocation. However, mortality rates were similar between the two groups [70]. In a matched cohort analysis by Kleiner et al., patients with PD undergoing THA experienced higher complication rates (14.6% vs 11.7%) and longer hospital stays (3.1 vs 2.7 days), but no increase in in-hospital mortality [42]. Wojtowicz et al. reported that although THA did not increase the risk of short-term (90 days and one year) mortality in patients with PD, a higher revision risk and long-term mortality rate were documented after nine years [81]. Two previous investigations reported that patients with PD undergoing THA had a higher mortality rate than those without this neurodegenerative disorder [81, 85]. Considering that PD is a progressive disease affecting patients’ QoL and life expectancy, it is challenging to speculate what proportion of this increased mortality rate could be attributed to PD progression itself rather than the THA operation. Table 1 summarizes the characteristics and outcomes of THA in patients with PD.
Total knee arthroplasty (TKA) in PD patients
Better medical treatment of patients with PD is expected to increase life expectancy, which will increase the number of patients undergoing TKA [92]. Patients with PD often have knee OA. The knee joint poses difficulties for PD patients in the advanced stages of the disease, causing pain, stiffness, and instability that may require TKA [93]. However, associated orthopedic conditions, such as a high risk of falls and fractures, rigidity, and poor bone quality in PD patients, can make THA challenging for arthroplasty surgeons [53, 72]. Additionally, PD symptoms, such as tremors, shuffling gait, and instability, can increase post-surgical complications and decrease TKA functional outcomes. Moreover, although knee arthroplasty can improve mechanical problems of the knee, reduce pain, and improve function, it cannot prevent the progression of PD [94].
Recent studies show that arthroplasty procedures can provide considerable pain relief, but data on their outcomes and complications in the PD population still needs to be improved [95, 96]. TKA is a successful treatment for reducing pain in weight-bearing joints. However, TKA’s efficacy with severe PD remains a concern. Several studies have evaluated functional outcomes following TKA in the PD population, each with contradicting results. Although TKA can provide favorable outcomes for patients with PD, those in the advanced stages may experience worsening motor features. Some studies demonstrated poor functional improvement after joint replacement surgery in PD patients [72, 97]. Noor et al. determined the significance of TKA in patients with PD. They found that TKA improved PD patients’ range of motion (ROM) and stability. Surgery also reduces pain and stiffness and improves physical and mental well-being. However, motor functional outcomes remain poor [98]. Rong et al. found that patients with PD who underwent THA or TKA (24 THA and 18 TKA patients) experienced significant improvements in pain and function. The prosthesis survivorship rates for THA and TKA were reported to be 94.1% and 87.5%, respectively (after 60 months). However, those in the mid- or end-stage of the disease have poor functional outcomes [99]. Baek et al. also demonstrated that TKA in patients with PD was associated with weak functional outcomes and increased mortality rates during follow-up. The mortality rates in the Parkinson’s and control groups were significantly different (31% and 6.9%, respectively). Additionally, they showed that the functional results of TKA in patients were closely associated with the progression of PD [100]. In another study, Montiel Terrón et al. [93] retrospectively examined 26 patients with PD and OA who underwent TKA. The mean follow-up was 3.5 years (2–9 years). They found that TKA reduced pain and improved ROM in patients with PD, which aligns with previous investigations [57, 96, 101]. They also demonstrated that the rate of motor symptom progression diminishes with advancing PD. While patients in the early stages had a higher chance of functional outcome deterioration, patients with more progressive PD tended to remain stable after five years. They had a better outcome after surgery [93]. Therefore, it can be concluded that the functional outcomes of PD patients after TKA are correlated with the severity and progression of PD, and doctors should help delay PD progression to optimize TJA outcomes [25, 71, 99].
Most studies have revealed that patients with PD who undergo TKA experience more complications, longer hospital stays, and higher costs than the normal population [26, 102, 103]. Sharma et al. reported that lower extremity TJA (THA and TKA) in patients with PD is associated with higher perioperative complication rates than in those without this neurodegenerative disorder; however, no significant difference was observed in complication rates between elective and trauma surgery settings. They reported a very low local complication rate, with only one local complication in each group (elective and traumatic surgery) [104]. Another study also demonstrated that PD is associated with an increased risk of complications following TJA (52 hips and 71 knees), mostly periprosthetic infection, fracture, and dislocation [57]. The incidence of periprosthetic joint infection has been documented in the literature to be 0.92% and 0.88% after TKA and THA, respectively [105]. Additionally, it has been reported that the dislocation rate following THA ranges from 1% to 3%, while the periprosthetic fracture rate is 0.6% [106, 107]. However, these complications have been reported to be higher with PD payments. Rondon et al. reported that 23.6% of PD patients required revision surgery in an average follow-up of 5.3 years. The survivorship of knee implants at years 5 and 10 was 89.8% and 66.2%, respectively, and hip implant survivorship was 85.3% and 78.7%, respectively. TJA improved functional outcomes in PD patients but not individuals without PD [57]. In a retrospective study of patients who underwent TKA with and without PD, Cheppalli et al. reported an advanced risk of periprosthetic mechanical problems and an increased cost of care patients with PD [108]. Marchand et al. also demonstrated that PD patients undergoing primary TKA have more medical (4.21 vs 1.24%; OR=3.50) and implant-related (5.09 vs 3.15%; OR=1.64) complications, higher readmission rates, and costs compared with controls [109]. Another study indicated that PD increased hospitalization time (6.5%), charge (3.05%), and perioperative complications after TKA. Since most of these complications can be controlled, multi-specialty patient optimization is required [25]. Altogether, these results suggest that patients with PD can benefit from perioperative consultation with a neurological specialist to reduce complications and improve outcomes after TJA.
While the literature reports high complication rates in PD patients undergoing TKA, some investigations demonstrated no significant increase in the studied populations’ complications. Wong et al. compared the outcomes of TKA in those with PD and those without PD. They suggested that PD is not a contraindication for TKA; however, PD patients show outcomes equivalent to those of the general population. No mortalities occurred during the follow-up period. They reported that PD patients exhibited functional outcomes and complications comparable to controls [96]. Kleiner et al. found that patients with PD who underwent TKA experienced slightly longer hospitalizations and higher costs. However, no increase was found in complications or mortality rates, suggesting that patients with PD can be safely considered for TKA [102]. Another study reported that TKA is a successful surgical option for KOA in patients with PD, with comparable results to the population despite the severity and progression of PD. They reported that preoperative function was low in patients with high PD severity, while postoperative function was comparable to that in the severe PD group [101]. Surgery is a suggested treatment for end-stage knee OA with satisfactory results, which may improve patients’ QoL. Studies have reported that TKA can improve the knee function in patients with PD. However, the positive impact of the procedure was less than that in non-PD patients [57]. In 2022, Zong et al. found that TKA did not improve QoL outcomes in patients with KOA and PD, except for a subtle reduction in pain-related disability. Although the two groups had similar preoperative QoL outcomes, those with PD had worse QoL on all three measures (EuroQol five-dimension [EQ-5D], pain and disability questionnaire [PDQ], and patient health questionnaire-9 [PHQ-9]) at the last follow-up [110]. Another study published in 2021 reported that although individuals with PD have diminished knee function and poorer QoL after TKA, they still experience significant functional improvements and high satisfaction compared to their preoperative situation. The complication and mortality rates were higher in PD patients than in the control group (26.3% vs 10.5% and 15.8% vs 5.3%, respectively) [111].
Although not comparable with control groups, some studies demonstrated low complication rates and promising functional outcomes in patients with PD compared to their condition before the surgery. This led to their satisfaction with the outcomes. These results emphasize that TKA remains a potential surgical option for OA in this expanding patient population. However, evaluating the long-term consequences of TKA in these studies was difficult due to the short follow-up period. Therefore, according to the available literature and controversial results, the necessity of TJA in the population of patients with PD should be evaluated, carefully depending on individual needs and conditions. In conclusion, in appropriately selected patients, PD severity and progression do not dramatically affect the outcomes of TJA. Although the effectiveness of TJA in individuals with PD remains a concern, we believe that PD should not prevent surgeons from performing TKA. Table 2 summarizes the characteristics and outcomes of TKA in patients with PD.
Conclusion
Joint arthroplasty is a safe and effective surgical procedure for treating end-stage OA. It can reduce pain, improve ROM, and enhance mobility and function in patients who do not respond to conservative intervention. PD patients have been found to have a higher complication rate after TJA, and the indication of TJA in patients with PD is a matter of debate due to the limited availability of consistent outcomes in existing publications. The available literature consists of a small number of retrospective patient cases, with significant variation in the disease stage and lack of adequate monitoring during postoperative follow-up, all contributing to the absence of a consensus. It is challenging to describe a straightforward approach for patients since PD is a complex condition with non-linear progression rates and considering multiple factors, such as sex, time since diagnosis, occurrence of falls, and response to medical treatment. Consequently, it is difficult to provide recommendations that meet realistic expectations. Surgery is not recommended until pain intensity and features careful analysis and failure of conservative steps. According to the information presented in the existing literature, TKA and THA can be considered safe procedures for patients with PD in terms of mortality rate and short-term complications. However, most studies have reported increased complications (mostly fracture and dislocation), prolonged hospital stays, and escalated costs in these patients.
Ethical Considerations
Compliance with ethical guidelines
This article is a review with no human or animal sample.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Alireza Ghanbari, Abolfazl Bagherifard, and Babak Roshanravan; Collection, assembly, and data extraction: Hooman Yahyazadeh, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Writing the original draft: Alireza Ghanbari, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Review and editing: Alireza Ghanbari, Hooman Yahyazadeh, Abolfazl Bagherifard, Karo Khosravi, Amir Azimi, Reza Ahmadi, and Babak Roshanravan; Supervision: Abolfazl Bagherifard, and Babak Roshanravan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all individuals who helped us develop this research.
References
- Pollock M, Somerville L, Firth A, Lanting B. Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: A systematic review of the literature. JBJS Rev. 2016; 4(12):e4. [DOI:10.2106/JBJS.RVW.16.00002] [PMID]
- Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015; 97(17):1386-97. [DOI:10.2106/JBJS.N.01141] [PMID] [PMCID]
- Siddiqi A, Levine BR, Springer BD. Highlights of the 2021 American joint replacement registry annual report. Arthroplast Today. 2022; 13:205-7. [DOI:10.1016/j.artd.2022.01.020] [PMID] [PMCID]
- Ryu HG, Roh YJ, Oh KJ, Hwang JH, Kim Y, Cho HW, et al. Dual mobility articulation total hip arthroplasty for displaced neck fracture in elderly with neuromuscular disorder. Injury. 2021; 52(6):1480-6. [DOI:10.1016/j.injury.2021.01.005] [PMID]
- Cleveland Clinic OME Arthroplasty Group. Understanding the main predictors of length of stay after total hip arthroplasty: Patient-related or procedure-related risk factors? J Arthroplasty. 2021; 36(5):1663-70. [DOI:10.1016/j.arth.2020.11.029] [PMID]
- Pomeroy E, Fenelon C, Murphy EP, Staunton PF, Rowan FE, Cleary MS. A systematic review of total knee arthroplasty in neurologic conditions: Survivorship, complications, and surgical considerations. J Arthroplasty. 2020; 35(11):3383-92. [DOI:10.1016/j.arth.2020.08.008] [PMID]
- O'Driscoll CS, Hughes AJ, Davey MS, Queally JM, O'Daly BJ. Total hip arthroplasty in patients with neurological conditions: A systematic review. Arthroplast Today. 2022; 19:101068. [DOI:10.1016/j.artd.2022.11.001] [PMID] [PMCID]
- Marsh M, Newman S. Trends and developments in hip and knee arthroplasty technology. J Rehabil Assist Technol Eng. 2021; 8:2055668320952043. [DOI:10.1177/2055668320952043] [PMID] [PMCID]
- Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018; 392(10158):1662-71. [DOI:10.1016/S0140-6736(18)31777-X] [PMID]
- Queally JM, Abdulkarim A, Mulhall KJ. Total hip replacement in patients with neurological conditions. J Bone Joint Surg Br. 2009; 91(10):1267-73. [DOI:10.1302/0301-620X.91B10.22934] [PMID]
- Rodriguez-Oroz MC, Jahanshahi M, Krack P, Litvan I, Macias R, Bezard E, et al. Initial clinical manifestations of Parkinson's disease: Features and pathophysiological mechanisms. Lancet Neurol. 2009; 8(12):1128-39. [DOI:10.1016/S1474-4422(09)70293-5] [PMID]
- Jankovic J. Parkinson's disease: Clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008; 79(4):368-76. [DOI:10.1136/jnnp.2007.131045] [PMID]
- Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, et al. A randomized, controlled trial of total knee replacement. N Engl J Med. 2015; 373(17):1597-606. [DOI:10.1056/NEJMoa1505467] [PMID]
- Chesworth BM, Mahomed NN, Bourne RB, Davis AM; OJRR Study Group. Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol. 2008; 61(9):907-18. [DOI:10.1016/j.jclinepi.2007.10.014] [PMID]
- Jorn LP, Johnsson R, Toksvig-Larsen S. Patient satisfaction, function and return to work after knee arthroplasty. Acta Orthop Scand. 1999; 70(4):343-7. [DOI:10.3109/17453679908997822] [PMID]
- Varacallo M, Luo TD, Johanson NA. Total knee arthroplasty techniques. Treasure Island: StatPearls; 2018. [Link]
- Williams DH, Garbuz DS, Masri BA, Duncan CP, Garbuz DS. Total knee arthroplasty: Techniques and results. BC Med J. 2010; 52(9):447-54. [DOI:10.1097/BTK.0b013e3181d16758]
- Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985; 192:13-22. [DOI:10.1097/00003086-198501000-00003]
- Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: A systematic review. HSS J. 2018; 14(2):192-201. [DOI:10.1007/s11420-018-9614-8] [PMID] [PMCID]
- Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement. A concise follow-up of a previous report. J Bone Joint Surg Am. 2009; 91(6):1419-23. [DOI:10.2106/JBJS.H.01351] [PMID]
- Guo B, Qin S, Ye H. [Research progress of knee-salvage treatment for knee osteoarthritis (Chinese)]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2018; 32(10):1292-6. [DOI:10.7507/1002-1892.201807027] [PMID]
- Ghosh A, Chatterji U. An evidence-based review of enhanced recovery after surgery in total knee replacement surgery. J Perioper Pract. 2019; 29(9):281-90. [DOI:10.1177/1750458918791121] [PMID]
- Tibbo ME, Chalmers BP, Berry DJ, Pagnano MW, Lewallen DG, Abdel MP. Primary total knee arthroplasty in patients with neuropathic (charcot) arthropathy: Contemporary results. J Arthroplasty. 2018; 33(9):2815-20. [DOI:10.1016/j.arth.2018.04.003] [PMID]
- Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018; 100(17):1455-60. [DOI:10.2106/JBJS.17.01617] [PMID]
- Newman JM, Sodhi N, Wilhelm AB, Khlopas A, Klika AK, Naziri Q, et al. Parkinson's disease increases the risk of perioperative complications after total knee arthroplasty: A nationwide database study. Knee Surg Sports Traumatol Arthrosc. 2019; 27(7):2189-95. [DOI:10.1007/s00167-018-4970-y] [PMID]
- Cross WW 3rd, Saleh KJ, Wilt TJ, Kane RL. Agreement about indications for total knee arthroplasty. Clin Orthop Relat Res. 2006; 446:34-9. [DOI:10.1097/01.blo.0000214436.49527.5e] [PMID]
- Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. Lancet. 2007; 370(9597):1508-19. [DOI:10.1016/S0140-6736(07)60457-7] [PMID]
- Wiles P. The surgery of the osteoarthritic hip. Br J Surg. 1958; 45(193):488-97. [DOI:10.1002/bjs.18004519315] [PMID]
- Smith-Petersen M. Evolution of mould arthroplasty of the hip joint. J Bone Joint Surg Br Vol. 1948; 30(1):59-75. [DOI:10.1302/0301-620X.30B1.59]
- Molina CS, Thakore RV, Blumer A, Obremskey WT, Sethi MK. Use of the national surgical quality improvement program in orthopaedic surgery. Clin Orthop Relat Res. 2015; 473(5):1574-81. [DOI:10.1007/s11999-014-3597-7] [PMID] [PMCID]
- Charnley J. Arthroplasty of the hip. A new operation. Lancet. 1961; 1(7187):1129-32. [DOI:10.1016/S0140-6736(61)92063-3] [PMID]
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019; 27(11):1578-89. [DOI:10.1016/j.joca.2019.06.011] [PMID]
- Günther KP, Deckert S, Lützner C, Lange T, Schmitt J, Postler A, et al. Total hip replacement for osteoarthritis-evidence-based and patient-oriented indications. Dtsch Arztebl Int. 2021; 118(43):730-6. [DOI:10.3238/arztebl.m2021.0323] [PMID] [PMCID]
- Crawford RW, Murray DW. Total hip replacement: Indications for surgery and risk factors for failure. Ann Rheum Dis. 1997; 56(8):455-7. [DOI:10.1136/ard.56.8.455] [PMID] [PMCID]
- Vorokov AA, Bortulev PI, Khaydarov VM, Linnik SA, Tkachenko AN. Total hip and knee arthoplasty: On the issue of indications for surgery. Pediatr Traumatol Orthop Reconstr Surg. 2020; 8(3):355-64. [DOI:10.17816/PTORS34164]
- Buirs LD, Van Beers LW, Scholtes VA, Pastoors T, Sprague S, Poolman RW. Predictors of physical functioning after total hip arthroplasty: A systematic review. BMJ Open. 2016; 6(9):e010725. [DOI:10.1136/bmjopen-2015-010725] [PMID] [PMCID]
- Karachalios T, Komnos G, Koutalos A. Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev. 2018; 3(5):232-9. [DOI:10.1302/2058-5241.3.170068] [PMID] [PMCID]
- NHS Digital. Finalised patient reported outcome measures (PROMs) in England for hip and knee replacement procedures (April 2017 to March 2018) [Internet]. 2019 [Updated 2020 February 13]. Available from: [Link]
- Wojtowicz AL, Al-Azzani W, Nåtman J, Rolfson O, Rogmark C, Cnudde PHJ. Hip arthroplasty for acute hip fracture in patients with neurological disorders: A report Of 9,702 cases from the Swedish arthroplasty register. Injury. 2022; 53(3):1202-8. [DOI:10.1016/j.injury.2021.09.028] [PMID]
- Yinchang Z. Hip prosthesis replacement in femoral neck fractures with neuromuscular lesions of the hip. J Wannan Med College. 2019; 38(04):320-22. [Link]
- Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty. 1999; 14(6):662-8. [DOI:10.1016/S0883-5403(99)90219-X] [PMID]
- Kleiner JE, Eltorai AEM, Rubin LE, Daniels AH. Matched cohort analysis of total hip arthroplasty in patients with and without parkinson's disease: Complications, mortality, length of stay, and hospital charges. J Arthroplasty. 2019; 34(7S):S228-31. [DOI:10.1016/j.arth.2019.03.023] [PMID]
- Newman JM, Sodhi N, Dalton SE, Khlopas A, Newman RP, Higuera CA, et al. Does parkinson disease increase the risk of perioperative complications after total hip arthroplasty? A nationwide database study. J Arthroplasty. 2018; 33(7S):S162-6. [DOI:10.1016/j.arth.2018.01.006] [PMID]
- Flynn JM, Miller F. Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg. 2002; 10(3):198-209. [DOI:10.5435/00124635-200205000-00006] [PMID]
- King G, Hunt LP, Wilkinson JM, Blom AW; National Joint Registry for England, Wales, and Northern Ireland. Good outcome of total hip replacement in patients with cerebral palsy: A comparison of 389 patients and 425,813 controls from the National Joint Registry for England and Wales. Acta Orthop. 2016; 87(2):93-9. [DOI:10.3109/17453674.2015.1137439] [PMID] [PMCID]
- Newman JM, Naziri Q, Chughtai M, Khlopas A, Kryzak TJ, Navale SM, et al. Does multiple sclerosis affect the inpatient perioperative outcomes after total hip arthroplasty? J Arthroplasty. 2017; 32(12):3669-74. [DOI:10.1016/j.arth.2017.07.006] [PMID]
- Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007; 68(5):384-6. [DOI:10.1212/01.wnl.0000247740.47667.03] [PMID]
- Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Mov Disord. 2014; 29(13):1583-90. [DOI:10.1002/mds.25945] [PMID]
- Mirelman A, Bonato P, Camicioli R, Ellis TD, Giladi N, Hamilton JL, et al. Gait impairments in Parkinson's disease. Lancet Neurol. 2019; 18(7):697-708. [DOI:10.1016/S1474-4422(19)30044-4] [PMID]
- Allen NE, Schwarzel AK, Canning CG. Recurrent falls in Parkinson's disease: A systematic review. Parkinsons Dis. 2013; 2013:906274. [DOI:10.1155/2013/906274] [PMID] [PMCID]
- van den Bos F, Speelman AD, Samson M, Munneke M, Bloem BR, Verhaar HJ. Parkinson's disease and osteoporosis. Age Ageing. 2013; 42(2):156-62. [DOI:10.1093/ageing/afs161] [PMID]
- Lyell V, Henderson E, Devine M, Gregson C. Assessment and management of fracture risk in patients with Parkinson's disease. Age Ageing. 2015; 44(1):34-41. [DOI:10.1093/ageing/afu122] [PMID]
- Lethbridge L, Johnston GM, Turnbull G. Co-morbidities of persons dying of Parkinson's disease. Prog Palliat Care. 2013; 21(3):140-5. [DOI:10.1179/1743291X12Y.0000000037] [PMID] [PMCID]
- Zuckerman LM. Parkinson's disease and the orthopaedic patient. J Am Acad Orthop Surg. 2009; 17(1):48-55. [DOI:10.5435/00124635-200901000-00007] [PMID]
- Fast A, Mendelsohn E, Sosner J. Total knee arthroplasty in Parkinson's disease. Arch Phys Med Rehabil. 1994; 75(11):1269-70. [DOI:10.1016/0003-9993(94)90018-3] [PMID]
- Tinning CG, Cochrane LA, Singer BR. Primary total knee arthroplasty in patients with Parkinson's disease: Analysis of outcomes. Acta Orthop Belg. 2013; 79(3):301-6. [Link]
- Rondon AJ, Tan TL, Schlitt PK, Greenky MR, Phillips JL, Purtill JJ. Total joint arthroplasty in patients with Parkinson’s disease: Survivorship, outcomes, and reasons for failure. J Arthroplast. 2018; 33(4):1028-32. [DOI:10.1016/j.arth.2017.11.017]
- Mehta S, Vankleunen JP, Booth RE, Lotke PA, Lonner JH. Total knee arthroplasty in patients with Parkinson’s disease: Impact of early postoperative neurologic intervention. Am J Ortho. 2008; 37(10):513-6. [Link]
- Wang Y, Wang S, Yang X. Prevalence of different types of wound infection in subjects with Parkinson's disease and total joint arthroplasty: A meta-Analysis. Int Wound J. 2023; 20(7):2780-7. [DOI:10.1111/iwj.14154] [PMID] [PMCID]
- Penrose CT, Bala A, Dekker TJ, Seyler TM, Randell TR, Green CL, et al. Total hip arthroplasty in patients with Parkinson’s disease. Duke Orthop J. 2019; 9(1):60-8. [DOI:10.4103/DORJ.DORJ_10_19]
- Melton LJ 3rd, Leibson CL, Achenbach SJ, Bower JH, Maraganore DM, Oberg AL, et al. Fracture risk after the diagnosis of Parkinson's disease: Influence of concomitant dementia. Mov Disord. 2006; 21(9):1361-7. [DOI:10.1002/mds.20946] [PMID]
- Gnädinger M, Mellinghoff HU, Kaelin-Lang A. Parkinson's disease and the bones. Swiss Med Wkly. 2011; 141:w13154. [DOI:10.4414/smw.2011.13154] [PMID]
- Nam JS, Kim YW, Shin J, Chang JS, Yoon SY. Hip fracture in patients with parkinson's disease and related mortality: A population-based study in Korea. Gerontology. 2021; 67(5):544-53. [DOI:10.1159/000513730] [PMID]
- Di Monaco M, Vallero F, Di Monaco R, Tappero R, Cavanna A. Bone mineral density in hip-fracture patients with Parkinson's disease: A case-control study. Arch Phys Med Rehabil. 2006; 87(11):1459-62. [DOI:10.1016/j.apmr.2006.07.265] [PMID]
- Fink HA, Kuskowski MA, Orwoll ES, Cauley JA, Ensrud KE; Osteoporotic Fractures in Men (MrOS) Study Group. Association between Parkinson's disease and low bone density and falls in older men: The osteoporotic fractures in men study. J Am Geriatr Soc. 2005; 53(9):1559-64. [DOI:10.1111/j.1532-5415.2005.53464.x] [PMID]
- Walker RW, Chaplin A, Hancock RL, Rutherford R, Gray WK. Hip fractures in people with idiopathic Parkinson's disease: Incidence and outcomes. Mov Disord. 2013; 28(3):334-40. [DOI:10.1002/mds.25297] [PMID]
- Nguyen PV, Hjelholt TJ, Heide-Jørgensen U, Pedersen AB. Postoperative complications, mortality, and quality of in-hospital care among hip fracture patients with Parkinson's disease. Injury. 2022; 53(6):2150-7. [DOI:10.1016/j.injury.2022.03.015] [PMID]
- Fontalis A, Kenanidis E, Bennett-Brown K, Tsiridis E. Clinical outcomes in elective total hip arthroplasty in Parkinson's disease: A systematic review of the literature. EFORT Open Rev. 2020; 5(12):856-65. [DOI:10.1302/2058-5241.5.200034] [PMID] [PMCID]
- Chen YY, Cheng PY, Wu SL, Lai CH. Parkinson's disease and risk of hip fracture: An 8-year follow-up study in Taiwan. Parkinsonism Relat Disord. 2012; 18(5):506-9. [DOI:10.1016/j.parkreldis.2012.01.014] [PMID]
- Goel A, Viswanathan VK, Purudappa PP, Sakthivelnathan V, Mounasamy V, Sambandam S. Cost and early complication analysis following total hip arthroplasty in parkinson's disease patients: A propensity-matched database study. Arch Bone Jt Surg. 2023; 11(1):47-52. [DOI:10.22038/ABJS.2022.65048.3120] [PMID]
- Weber M, Cabanela ME, Sim FH, Frassica FJ, Harmsen WS. Total hip replacement in patients with Parkinson's disease. Int Orthop. 2002; 26(2):66-8. [DOI:10.1007/s00264-001-0308-2] [PMID] [PMCID]
- Mathew PG, Sponer P, Kucera T, Grinac M, Knízek J. Total HIP arthroplasty in patients with Parkinson's disease. Acta Medica. 2013; 56(3):110-6. [DOI:10.14712/18059694.2014.18] [PMID]
- Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006; 447:9-18. [DOI:10.1097/01.blo.0000218754.12311.4a] [PMID]
- Cabanela ME, Weber M. Total hip arthroplasty in patients with neuromuscular disease. Instr Course Lect. 2000; 49:163-8. [DOI:10.2106/00004623-200003000-00014] [PMID]
- Bassiony AA, Gameel S. The dual mobility hip arthroplasty for hip fracture in Parkinson’s disease. Open J Trauma. 2020; 4(1):032-5. [Link]
- Gausden EB, Parhar HS, Popper JE, Sculco PK, Rush BNM. Risk factors for early dislocation following primary elective total hip arthroplasty. J Arthroplasty. 2018; 33(5):1567-71. [DOI:10.1016/j.arth.2017.12.034] [PMID]
- Mohammed R, Hayward K, Mulay S, Bindi F, Wallace M. Outcomes of dual-mobility acetabular cup for instability in primary and revision total hip arthroplasty. J Orthop Traumatol. 2015; 16(1):9-13. [DOI:10.1007/s10195-014-0324-9] [PMID] [PMCID]
- Luthra JS, Al Riyami A, Allami MK. Dual mobility total hip replacement in a high risk population. SICOT J. 2016; 2:43. [DOI:10.1051/sicotj/2016037] [PMID] [PMCID]
- Graversen AE, Jakobsen SS, Kristensen PK, Thillemann TM. No dislocations after primary hip arthroplasty with the dual mobility cup in displaced femoral neck fracture in patients with dementia. A one-year follow-up in 20 patients. SICOT J. 2017; 3:9. [DOI:10.1051/sicotj/2016050] [PMID] [PMCID]
- Lazennec JY, Kim Y, Pour AE. Total hip arthroplasty in patients with parkinson disease: Improved outcomes with dual mobility implants and cementless fixation. J Arthroplasty. 2018; 33(5):1455-61. [DOI:10.1016/j.arth.2017.11.062] [PMID]
- Wojtowicz AL, Mohaddes M, Odin D, Bülow E, Nemes S, Cnudde P. Is parkinson's disease associated with increased mortality, poorer outcomes scores, and revision risk after tha? findings from the swedish hip arthroplasty register. Clin Orthop Relat Res. 2019; 477(6):1347-55. [DOI:10.1097/CORR.0000000000000679] [PMID] [PMCID]
- Wang Z, Hou JZ, Wu CH, Zhou YJ, Gu XM, Wang HH, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res. 2018; 13(1):229. [DOI:10.1186/s13018-018-0929-4] [PMID] [PMCID]
- Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004; 86(1):9-14. [DOI:10.2106/00004623-200401000-00003] [PMID]
- Berliner Z, Yau C, Jahng K, Bas MA, Cooper HJ, Rodriguez JA. Risk factors for periprosthetic femoral fracture in non-cemented total hip arthroplasty through the direct anterior approach. HSS J. 2022; 18(3):368-75. [DOI:10.1177/15563316211050884] [PMID] [PMCID]
- Yang M, Yao M, Chu K, Wei C, Li Z, Huo J, et al. Efficacy of direct anterior approach versus posterior lateral approach for total hip replacement in patients with Parkinson’s disease. Med Sci Monit. 2023; 29:e939682-1. [DOI:10.12659/MSM.939682]
- Higgins BT, Barlow DR, Heagerty NE, Lin TJ. Anterior vs. posterior approach for total hip arthroplasty, A systematic review and meta-analysis. J Arthroplasty. 2015; 30(3):419-34. [DOI:10.1016/j.arth.2014.10.020] [PMID]
- Venishetty N, Beale J, Martinez J, Mounasamy V, Sambandam S. Understanding factors that impact the length of stay after total hip arthroplasty-A national in-patient sample-based study. J Clin Orthop Trauma. 2023; 46:102284. [DOI:10.1016/j.jcot.2023.102284] [PMID] [PMCID]
- Shah NV, Solow M, Lavian JD, Bloom LR, Grieco PW, Stroud SG, et al. Total hip arthroplasty in Parkinson's disease patients: A propensity score-matched analysis with minimum 2-year surveillance. Hip Int. 2020; 30(6):684-9. [DOI:10.1177/1120700019862247] [PMID]
- Mesarick EC, Ratcliff TL, Jose J, Sambandam S. Risk factors for in-patient myocardial infarction following total hip arthroplasty. J Orthop. 2024; 51:60-65. [DOI:10.1016/j.jor.2024.01.007] [PMID]
- Viswanathan VK, Subramanian S, Jones H, Mounasamy V, Sambandam S. Patient disposition after discharge following primary total hip arthroplasty: Home versus skilled nursing facility-A study based on national inpatient sample database. Arch Orthop Trauma Surg. 2024; 144(2):937-45.[DOI:10.1007/s00402-023-05081-9] [PMID]
- Yang Q, Wang J, Xu Y, Chen Y, Lian Q, Zhang Y. Incidence and risk factors of in-hospital prosthesis-related complications following total hip arthroplasty: A retrospective Nationwide Inpatient Sample database study. Int Orthop. 2020; 44(11):2243-52. [DOI:10.1007/s00264-020-04682-y] [PMID]
- Leibson CL, Maraganore DM, Bower JH, Ransom JE, O'brien PC, Rocca WA. Comorbid conditions associated with Parkinson's disease: A population-based study. Mov Disord. 2006; 21(4):446-55. [DOI:10.1002/mds.20685] [PMID]
- Montiel Terrón V, Vitoria M, Lamo de Espinosa Vázquez de Sola JM, Valentí Nin JR, Valentí Azcárate A. Do we really improve life quality after total knee arthroplasty in patients with Parkinson's disease? Arch Orthop Trauma Surg. 2021; 141(2):313-9. [DOI:10.1007/s00402-020-03644-8] [PMID]
- Yoon JR, Yoon TH, Lee SH. The effect of Parkinson's disease on total knee arthroplasty: A systematic review and meta-analysis. Knee Surg Relat Res. 2023; 35(1):6. [DOI:10.1186/s43019-023-00179-1] [PMID] [PMCID]
- Min H, Lin H, Chen G. Effect of Parkinson's disease on primary total joint arthroplasty outcomes: A meta-analysis of matched control studies. Int J Surg. 2019; 71:124-31. [DOI:10.1016/j.ijsu.2019.09.013] [PMID]
- Wong EH, Oh LJ, Parker DA. Outcomes of Primary Total knee arthroplasty in patients with parkinson's disease. J Arthroplasty. 2018; 33(6):1745-8. [DOI:10.1016/j.arth.2018.02.028] [PMID]
- Duffy GP, Trousdale RT. Total knee arthroplasty in patients with parkinson's disease. J Arthroplasty. 1996; 11(8):899-904. [DOI:10.1016/S0883-5403(96)80130-6] [PMID]
- Noor F, Gul N, Ahmed N. Total knee arthroplasty in patients with parkinson’s disease: A critical analysis of available evidence. Pak J Med Health Sci. 2023; 17(03):133. [DOI:10.53350/pjmhs2023173133]
- Rong X, Dahal S, Luo ZY, Zhou K, Yao SY, Zhou ZK. Functional outcomes after total joint arthroplasty are related to the severity of Parkinson's disease: A mid-term follow-up. J Orthop Surg Res. 2019; 14(1):396. [DOI:10.1186/s13018-019-1447-8] [PMID] [PMCID]
- Baek JH, Nam CH, Lee SC, Ahn HS, Ha YC. Poor outcomes of primary total knee arthroplasty in patients with Parkinson's disease. Int Orthop. 2021; 45(3):643-7. [DOI:10.1007/s00264-020-04924-z] [PMID]
- Ergin ÖN, Karademir G, Şahin K, Meriç E, Akgül T, Öztürk İ. Functional outcomes of total knee arthroplasty in patients with Parkinson's disease: A case control study. J Orthop Sci. 2020; 25(3):487-91. [DOI:10.1016/j.jos.2019.06.003] [PMID]
- Kleiner JE, Gil JA, Eltorai AEM, Rubin LE, Daniels AH. Matched cohort analysis of peri-operative outcomes following total knee arthroplasty in patients with and without Parkinson's disease. Knee. 2019; 26(4):876-80. [DOI:10.1016/j.knee.2019.05.003] [PMID]
- Jämsen E, Puolakka T, Peltola M, Eskelinen A, Lehto MU. Surgical outcomes of primary hip and knee replacements in patients with Parkinson's disease: A nationwide registry-based case-controlled study. Bone Joint J. 2014; 96-B(4):486-91. [DOI:10.1302/0301-620X.96B4.33422] [PMID]
- Sharma T, Hönle W, Handschu R, Adler W, Goyal T, Schuh A. Incidence of perioperative complications in total hip and knee arthroplasty in patients with Parkinson disease. Arch Orthop Trauma Surg. 2018; 138(6):765-70. [DOI:10.1007/s00402-018-2899-8] [PMID]
- Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008; 23(7):984-91. [DOI:10.1016/j.arth.2007.10.017] [PMID]
- Bourne RB, Mehin R. The dislocating hip: What to do, what to do. J Arthroplasty. 2004; 19(4 Suppl 1):111-4. [DOI:10.1016/j.arth.2004.02.016] [PMID]
- Dg L. Periprosthetic fracture of the femur after total hip arthroplasty: Treatment and results to date. Instr Course Lect. 1998; 47:243-9. [Link]
- Cheppalli NS, Senthil T, Sakthivelnathan V, Menedal A, Mounasamy V, Sambandam S. Complications during the hospital stay, length of stay, and cost of care in parkinson patients undergoing total knee arthroplasty: A propensity matched database study. J Am Acad Orthop Surg Glob Res Rev. 2022; 6(7):e22.00121. [DOI:10.5435/JAAOSGlobal-D-22-00121] [PMID] [PMCID]
- Marchand KB, Vakharia R, Sodhi N, Anis H, Salem HS, Scuderi GR, et al. Impact of parkinson's disease on complications, readmission rates, and costs of care following primary total knee arthroplasty. J Knee Surg. 2022; 35(1):21-5. [DOI:10.1055/s-0040-1710546] [PMID]
- Zong Y, Hao C, Zhang Y, Wu S. Quality of life assessment after total knee arthroplasty in patients with Parkinson's disease. BMC Musculoskelet Disord. 2022; 23(1):230. [DOI:10.1186/s12891-022-05176-1] [PMID] [PMCID]
- Goh GS, Zeng GJ, Tay DK, Lo NN, Yeo SJ, Liow MHL. Patients with parkinson's disease have poorer function and more flexion contractures after total knee arthroplasty. J Arthroplasty. 2021; 36(7):2325-30. [DOI:10.1016/j.arth.2020.11.016] [PMID]
Type of Study: Review Paper |
Subject:
Knee surgery
Received: 2022/11/16 | Accepted: 2023/10/1 | Published: 2023/11/1
Received: 2022/11/16 | Accepted: 2023/10/1 | Published: 2023/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |