Volume 10, Issue 4 (11-2023)
JROS 2023, 10(4): 231-236 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nakhaei Amroodi M, Tabrizian P, Baniasadi M, Bahaeddini M, Merdowsi F, Mokhtari K, et al . The Outcomes of Hook Plate Fixation in Acromioclavicular Injuries. JROS 2023; 10 (4) :231-236
URL: http://jros.iums.ac.ir/article-1-2265-en.html
URL: http://jros.iums.ac.ir/article-1-2265-en.html
Morteza Nakhaei Amroodi1 

 , Pouria Tabrizian1
, Pouria Tabrizian1 

 , Mojtaba Baniasadi1
, Mojtaba Baniasadi1 
 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 

 , Farzaneh Merdowsi2
, Farzaneh Merdowsi2 
 , Khatere Mokhtari3
, Khatere Mokhtari3 

 , Babak Roshanravan4
, Babak Roshanravan4 
 , Saeed Amiri1
, Saeed Amiri1 



 , Pouria Tabrizian1
, Pouria Tabrizian1 

 , Mojtaba Baniasadi1
, Mojtaba Baniasadi1 
 , Mohammadreza Bahaeddini1
, Mohammadreza Bahaeddini1 

 , Farzaneh Merdowsi2
, Farzaneh Merdowsi2 
 , Khatere Mokhtari3
, Khatere Mokhtari3 

 , Babak Roshanravan4
, Babak Roshanravan4 
 , Saeed Amiri1
, Saeed Amiri1 

1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafayahaieyan Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Cellular and Molecular Biology and Microbiology, Faculty of Biological Sciences and Technology, University of Isfahan, Isfahan, Iran.
4- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafayahaieyan Hospital, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Imam Reza Hospital, Birjand University of Medical Sciences, Birjand, Iran.
2- Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
3- Department of Cellular and Molecular Biology and Microbiology, Faculty of Biological Sciences and Technology, University of Isfahan, Isfahan, Iran.
4- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Shafayahaieyan Hospital, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Imam Reza Hospital, Birjand University of Medical Sciences, Birjand, Iran.
Full-Text [PDF 534 kb]
(64 Downloads)
| Abstract (HTML) (312 Views)
Full-Text: (71 Views)
Introduction
The acromioclavicular joint (ACJ) is the articulation between the clavicle and scapula bone and plays a significant role in the functionality of the upper limb. This joint is supported by various constraints, including ligaments [1]. Given its structure, the ACJ is exposed to injuries. Young adult athletes aged 20-30 have the highest AC injury risk. Previous studies have reported >10% of AC injuries in this group [2]. In most cases, the shared mechanism of injury is a fall on the supralateral side of the joint while the arm is in an adducted state [3].
The first attempt to manage an AC injury dates back to the early 20th century [4]. In the coming years, approximately 150 methods have been attempted to manage an AC injury, including open and closed techniques, such as hook plates, synthetic ligaments, clavicle osteotomy, or excision [5]. Numerous surgical methods are available for treating AC injuries, each with a complication risk ranging from 5% to 30%. Nevertheless, the diversity of surgical techniques and their associated risks have made it impossible to reach a consensus on what treatment best suits AC injuries [6].
Balser primarily introduced hook plate fixation as a treatment [7]. Different designs have used hook plates to achieve rigid internal fixation [8, 9]. Hook plates stabilized the coracoclavicular region and ACJ.
Methods
Study design
The present study was a retrospective cohort analysis conducted on patients with subacute ACJ injuries (one four weeks post-injury) who underwent hook plate surgery at Shafayahyaiian Hospital without ligament restoration between 2011 and 2023. Medical data were examined to identify patients. The inclusion criteria included a minimum follow-up of one year and no previous shoulder surgery. The exclusion criteria included all patients with grade I and II injuries, open injuries, polytrauma, neurovascular injury, concurrent shoulder or lower limb injury, and unreachable patients for final evaluation.
A study checklist was used to collect demographic data (age and sex), injury time, operation time, history of postoperative infection, and hook plate removal time. Patients who met the eligibility criteria were contacted and invited to the clinic for final evaluation. During the final evaluation, a goniometer was used to evaluate the active range of motion (ROM), including abduction, adduction, forward flexion, and extension, of the affected and unaffected shoulders.
Assessment tools
Functional outcomes were evaluated using the Constant-Murley shoulder outcome score (CSS), a 100-point rating system that evaluates ROM (40 points), strength (25 points), daily activities (20 points), and discomfort (15 points). This questionnaire does not have a validated Persian version [10]. Furthermore, the FSS was used to assess rotator cuff muscle function. The visual analog scale (VAS), with a score range of 1-10, was used to measure pain. Higher scores corresponded to greater pain. The following conditions were also assessed: Ossification of the coracoclavicular ligaments, osteolysis of the lateral clavicle, post-traumatic arthritis, ACJ instability, weakness, discomfort, and loss of anatomical reduction.
Procedure for surgery
Surgically, a skin incision was created, subcutaneous tissue was freed, and an ACJ needle was inserted to guide the insertion of a hook beneath the acromion. The joint was made smaller by first placing a screw in the hole on the plate closest to the joint and then adding other screws. Hook plates were purchased from Urmia Atra Orthoped. Following appropriate reduction confirmed by radiographic examination, the incision was sealed, and the shoulder was immobilized in a sling.
Statistical analysis
Stata software, version 17 was used for statistical analysis. Mean±SD, frequencies, and percentages are included in the descriptive statistics. Analytical statistics were performed to evaluate shoulder ROM and pain scores based on other variables with a significance level (P<0.05).
Results
In the current study, 38 patients were examined to evaluate the hook plate fixation results in subacute ACJ injury. As shown in Table 1, most participants were men (86.84%).
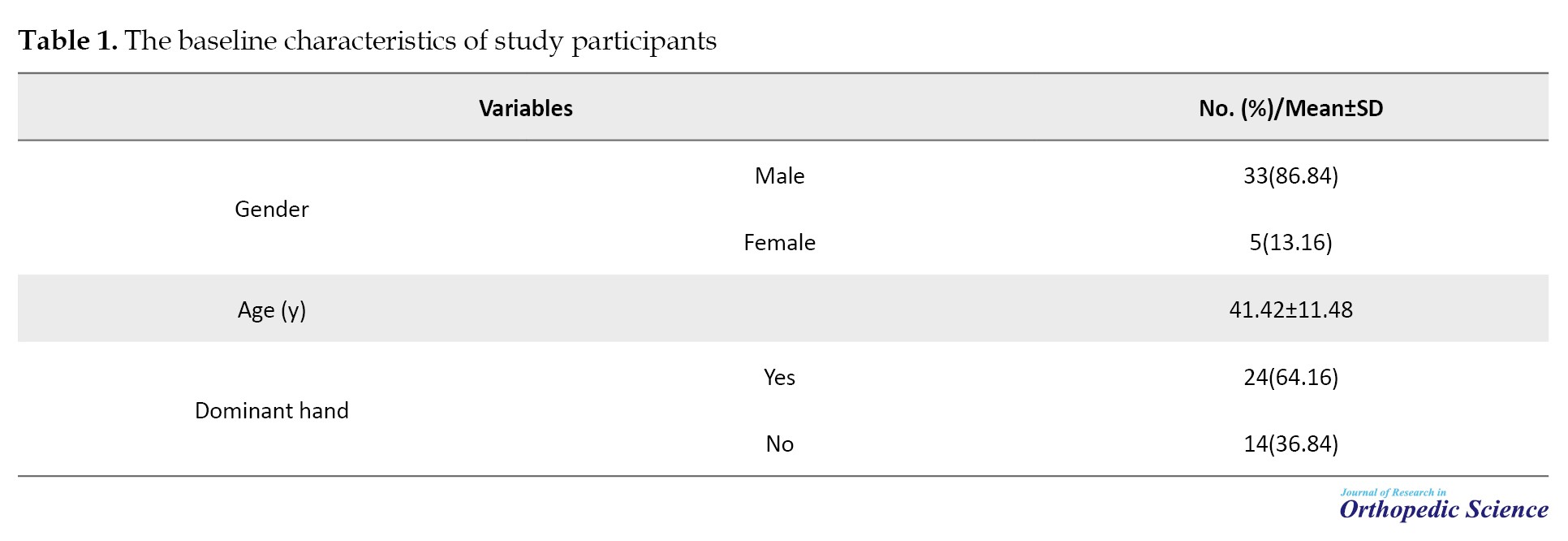
The mean age of the participants was 41.42±11.48 years. Furthermore, hand surgery was performed mainly on the dominant hand (63.16%).
Shoulder ROM following hook plate fixation in treating subacute ACJ injury was evaluated using different movements. The mean ROM of forward flexion was 157.89°, the mean ROM of abduction was 153.95°, and the mean ROM of external rotation was 50.79°, respectively (Table 2).
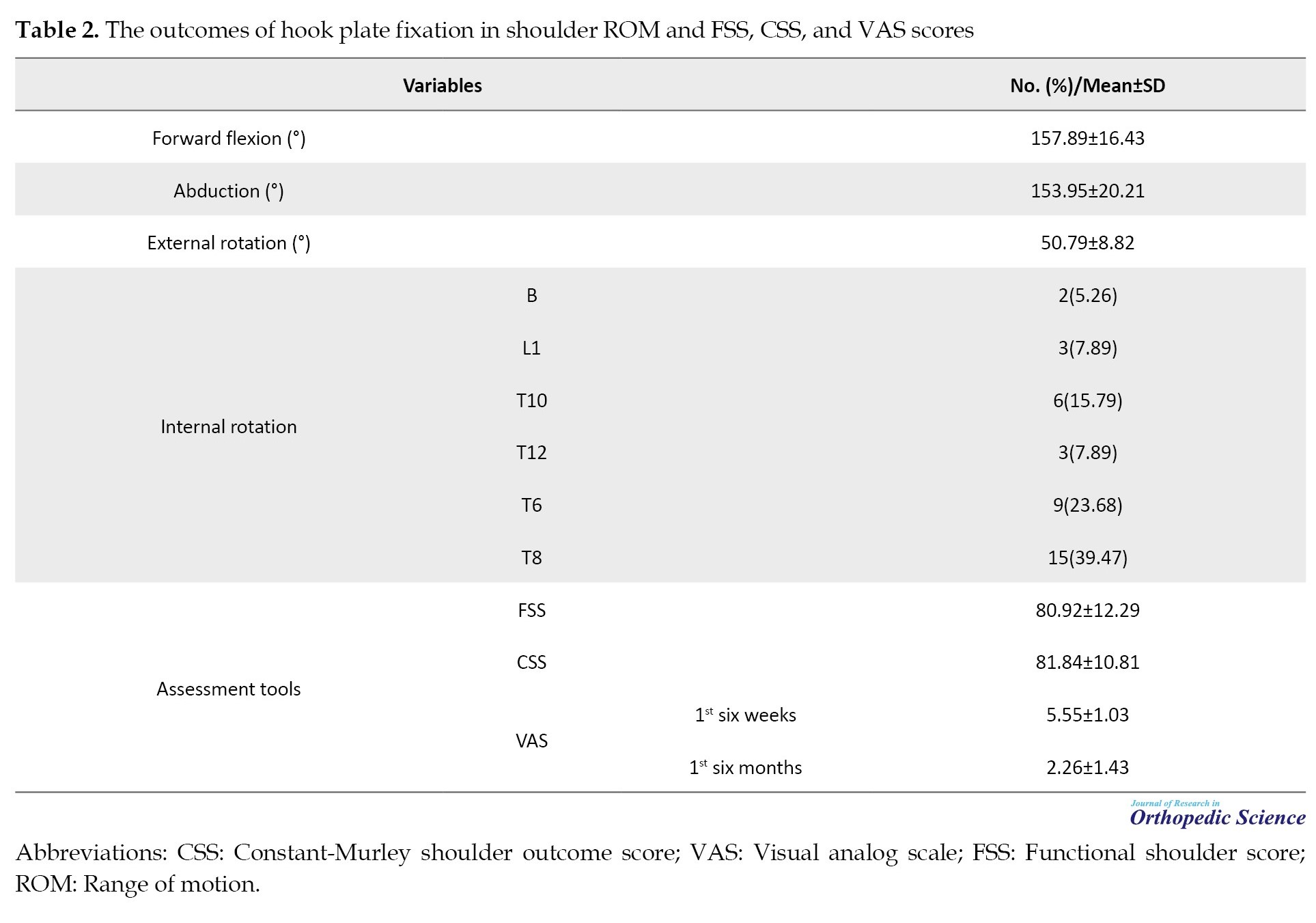
The functional shoulder score (FSS) and CSS questionnaires averaged 80.92 and 81.84, respectively (Table 2). The mean VAS was 5.55±1.03 and 2.26±1.43 in the first six weeks and six months, respectively (Table 2).
Furthermore, we evaluated complications in the study subjects. Thirty-two (84.21%) did not have post-surgical infections, and 37 patients (97.37%) did not require a second surgery.
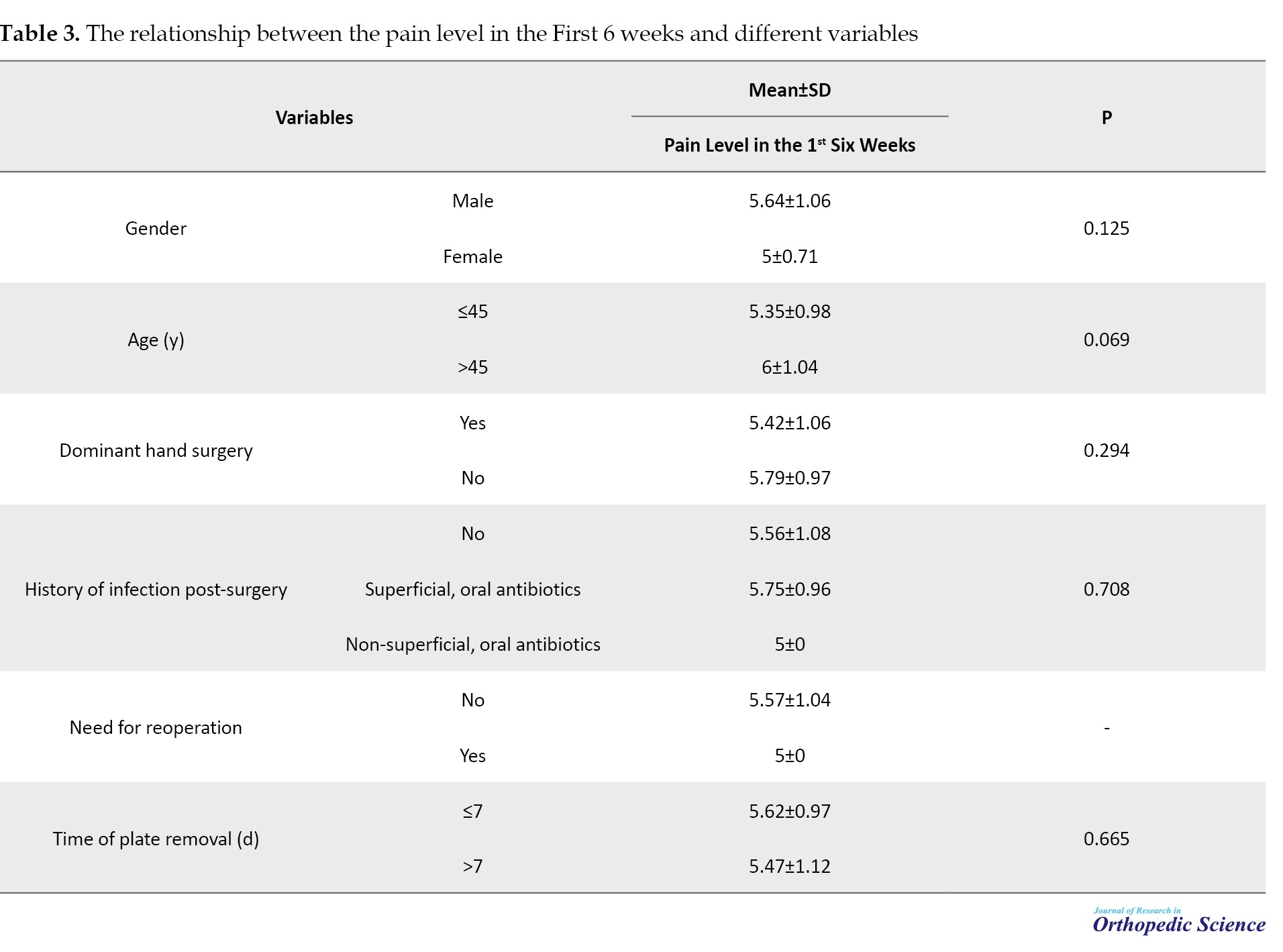
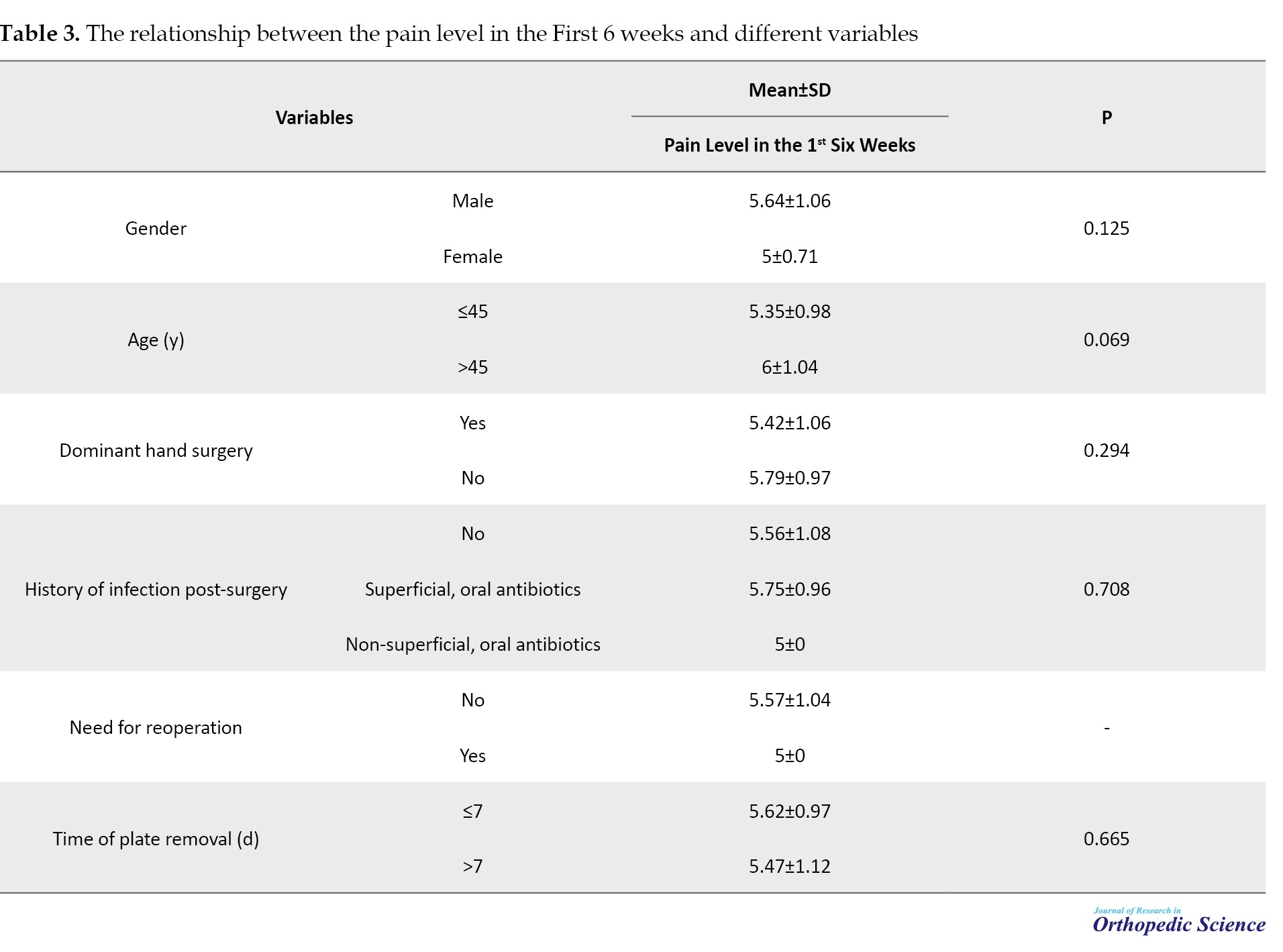
The relationship between pain and other variables during the first six weeks was assessed. None of the variables showed significant relationships. Detailed numbers are listed in Table 3.
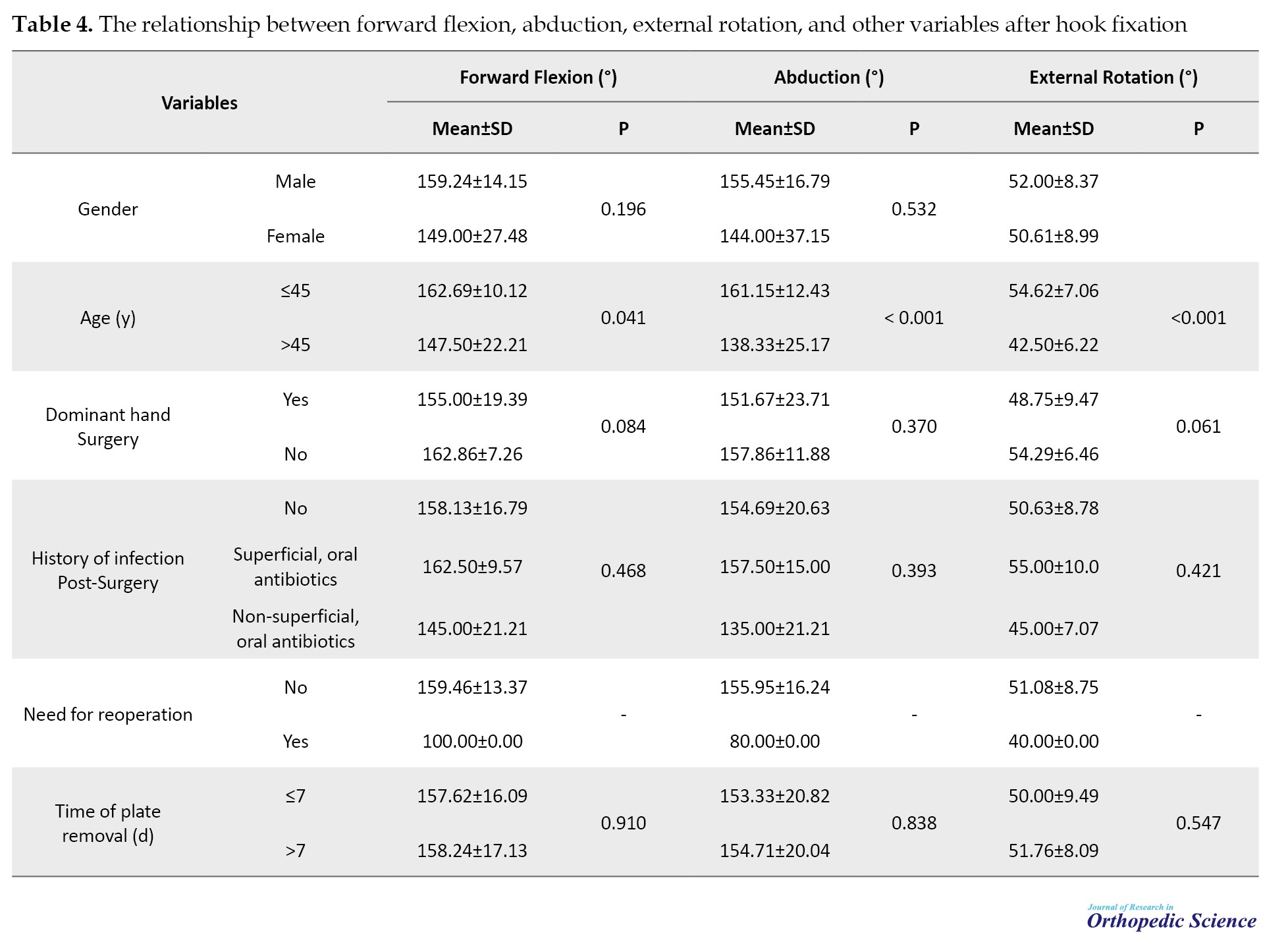
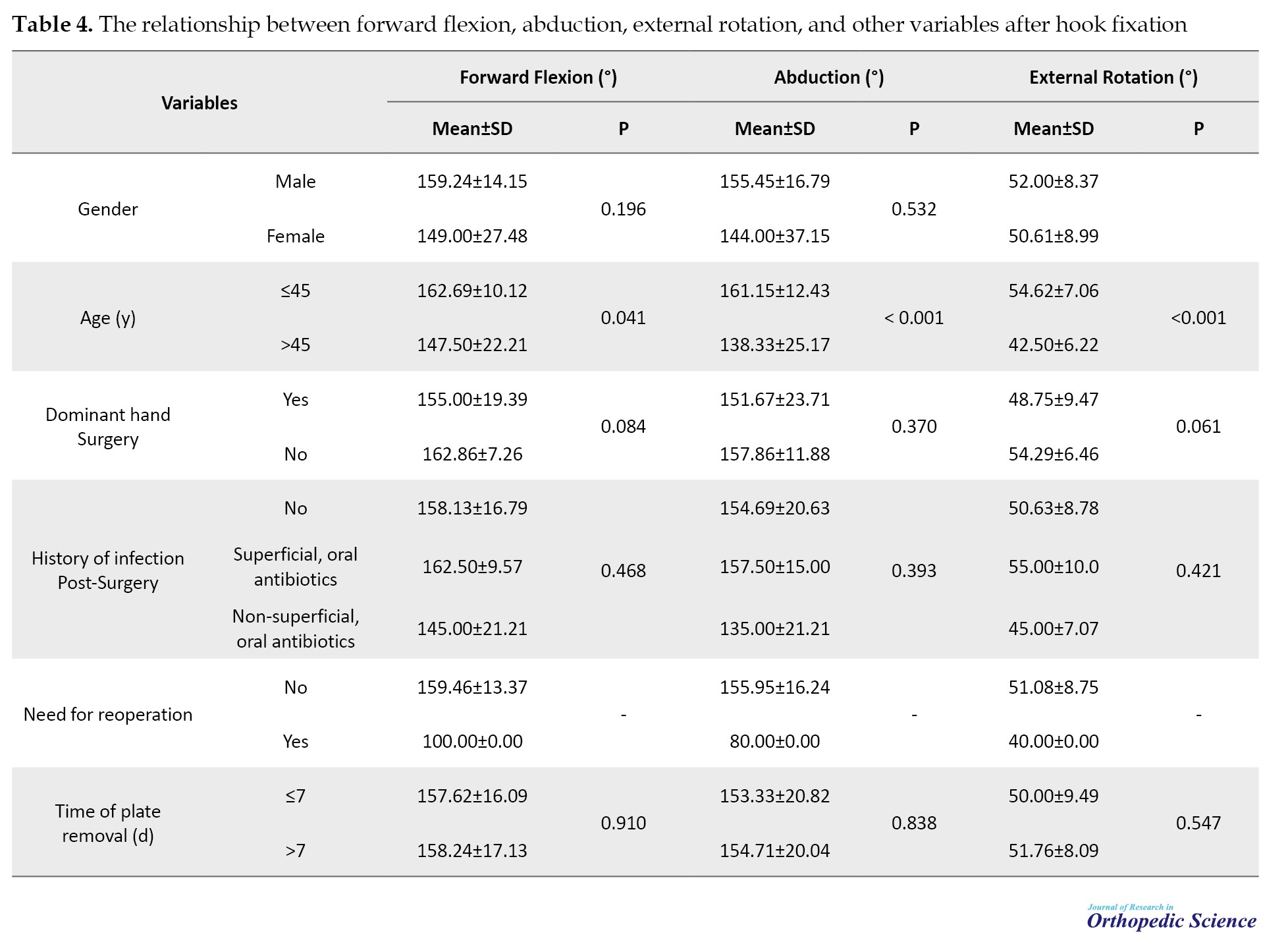
Assessment of the relationship between forward flexion, abduction, and external rotation ROM and different variables showed that only abduction and external rotation ROMs were significantly different between those aged ≤45 and >45 years. The other variables showed no significant differences in shoulder ROM (Table 4).
Discussion
This study investigated the clinical outcomes of hook plate fixation without ligament reconstruction in patients with subacute ACJ injuries. Most patients were men with a mean age of 41 years. The results of this study showed that pain was highest in the first six weeks post-surgery, with a mean of 70%. The pain decreased over time, with <33% reported in the first six months. None of the variables studied showed a significant relationship with the pain scale in the first six weeks. Furthermore, this study showed that age >45 is significantly associated with decreased shoulder ROM. The mean age in this study was 41 years, a few years older than anticipated [11, 12].
Despite different options to treat ACJ injuries, physicians must contemplate the best option. Some of these options are the AO technique with two Kirschner wires and a wire binder of the Zuggurtung type and transclavicular screw. The first is associated with the risk of Kirschner wire migration, while the second method poses a risk of clavicle fracture. Furthermore, in the case of clavicle fracture, the screw should be removed at an early stage, leading to further dislocation and instability of the ACJ. Another method, hook plate fixation, has been used for decades. This method provides optimal joint stability and inserts the plate above the clavicle and the hook underneath the acromion. Nevertheless, this method is also associated with some risks, including subacromial impingement [13].
The VAS score was assessed at six weeks and six months, and the CCS score was at six months in this study. Compared to a previous survey of Yan in 2017, our study showed lower numbers [14]. Some reasons are considered for the pain and reduced mobility. The insertion of the hook plate reduced the width of the subacromial space, leading to a decrease in shoulder function and elevation in bursa pressure. The presence of a hook plate restricts rotation of the humeral greater tuberosity. Direct collision with the greater tuberosity may stimulate and damage the supraspinatus muscle, leading to pain and weakness. Furthermore, the escalation of tension and stimulation originated from the hook plate and was directed toward the subacromial surface. In addition, significant subacromial surface tension may arise during procedures due to variations in shoulder thickness across patients and in insertion angle and position.
Furthermore, regarding the complications in the present study, few patients showed signs of infection or required a second surgery. Two in the hook plate group showed complications in another study of 28 patients grouped in terms of treatment method. The rate of complications in this study was comparable to that in our study; however, this study also showed that the complications that occurred in the hook plate group were not significantly different from those in the AO technique and transclavicular screw groups [13]. Another study showed that hook plate fixation did not significantly reduce complications [15].
Conclusion
Hook plate fixation surgery is effective in patients with subacute injuries of different ages. This operation significantly improves ROM in patients under or equal to 45 years of age than in those over 45, and the results do not differ based on the patient’s sex.
This study has both strengths and limitations. This study achieved a high follow-up rate, ensuring that most of the initial cohort was evaluated for outcomes. Furthermore, this study had an acceptable sample size compared to similar studies. However, the retrospective nature of this study limits its ability to control for confounding variables. Also, we conducted the study at a single hospital, which may have limited the applicability of our results to other settings or populations. However, the absence of a comparison group limits the ability to directly compare the effectiveness of different treatment approaches.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1399.408). All methods were conducted according to relevant guidelines and regulations, and informed consent was obtained from all participants.
Funding
This study was supported by the Iran University of Medical Sciences, Tehran, Iran (Grant No.: 18127).
Authors' contributions
Conceptualization: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, Mohammadreza Bahaeddini, and Babak Roshanravan; Data collection, assembly, data extraction: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, and Mohammadreza Bahaeddini; Writing the original draft: Farzaneh Merdowsi, Khatere Mokhtari, Babak Roshanravan, and Saeed Amiri; Review and editing: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, Mohammadreza Bahaeddini, Farzaneh Merdowsi, Khatere Mokhtari, Babak Roshanravan, and Saeed Amiri; Supervision: Pouria Tabrizian, Mojtaba Baniasadi, and Babak Roshanravan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all individuals who helped them develop this research.
References
The acromioclavicular joint (ACJ) is the articulation between the clavicle and scapula bone and plays a significant role in the functionality of the upper limb. This joint is supported by various constraints, including ligaments [1]. Given its structure, the ACJ is exposed to injuries. Young adult athletes aged 20-30 have the highest AC injury risk. Previous studies have reported >10% of AC injuries in this group [2]. In most cases, the shared mechanism of injury is a fall on the supralateral side of the joint while the arm is in an adducted state [3].
The first attempt to manage an AC injury dates back to the early 20th century [4]. In the coming years, approximately 150 methods have been attempted to manage an AC injury, including open and closed techniques, such as hook plates, synthetic ligaments, clavicle osteotomy, or excision [5]. Numerous surgical methods are available for treating AC injuries, each with a complication risk ranging from 5% to 30%. Nevertheless, the diversity of surgical techniques and their associated risks have made it impossible to reach a consensus on what treatment best suits AC injuries [6].
Balser primarily introduced hook plate fixation as a treatment [7]. Different designs have used hook plates to achieve rigid internal fixation [8, 9]. Hook plates stabilized the coracoclavicular region and ACJ.
Methods
Study design
The present study was a retrospective cohort analysis conducted on patients with subacute ACJ injuries (one four weeks post-injury) who underwent hook plate surgery at Shafayahyaiian Hospital without ligament restoration between 2011 and 2023. Medical data were examined to identify patients. The inclusion criteria included a minimum follow-up of one year and no previous shoulder surgery. The exclusion criteria included all patients with grade I and II injuries, open injuries, polytrauma, neurovascular injury, concurrent shoulder or lower limb injury, and unreachable patients for final evaluation.
A study checklist was used to collect demographic data (age and sex), injury time, operation time, history of postoperative infection, and hook plate removal time. Patients who met the eligibility criteria were contacted and invited to the clinic for final evaluation. During the final evaluation, a goniometer was used to evaluate the active range of motion (ROM), including abduction, adduction, forward flexion, and extension, of the affected and unaffected shoulders.
Assessment tools
Functional outcomes were evaluated using the Constant-Murley shoulder outcome score (CSS), a 100-point rating system that evaluates ROM (40 points), strength (25 points), daily activities (20 points), and discomfort (15 points). This questionnaire does not have a validated Persian version [10]. Furthermore, the FSS was used to assess rotator cuff muscle function. The visual analog scale (VAS), with a score range of 1-10, was used to measure pain. Higher scores corresponded to greater pain. The following conditions were also assessed: Ossification of the coracoclavicular ligaments, osteolysis of the lateral clavicle, post-traumatic arthritis, ACJ instability, weakness, discomfort, and loss of anatomical reduction.
Procedure for surgery
Surgically, a skin incision was created, subcutaneous tissue was freed, and an ACJ needle was inserted to guide the insertion of a hook beneath the acromion. The joint was made smaller by first placing a screw in the hole on the plate closest to the joint and then adding other screws. Hook plates were purchased from Urmia Atra Orthoped. Following appropriate reduction confirmed by radiographic examination, the incision was sealed, and the shoulder was immobilized in a sling.
Statistical analysis
Stata software, version 17 was used for statistical analysis. Mean±SD, frequencies, and percentages are included in the descriptive statistics. Analytical statistics were performed to evaluate shoulder ROM and pain scores based on other variables with a significance level (P<0.05).
Results
In the current study, 38 patients were examined to evaluate the hook plate fixation results in subacute ACJ injury. As shown in Table 1, most participants were men (86.84%).
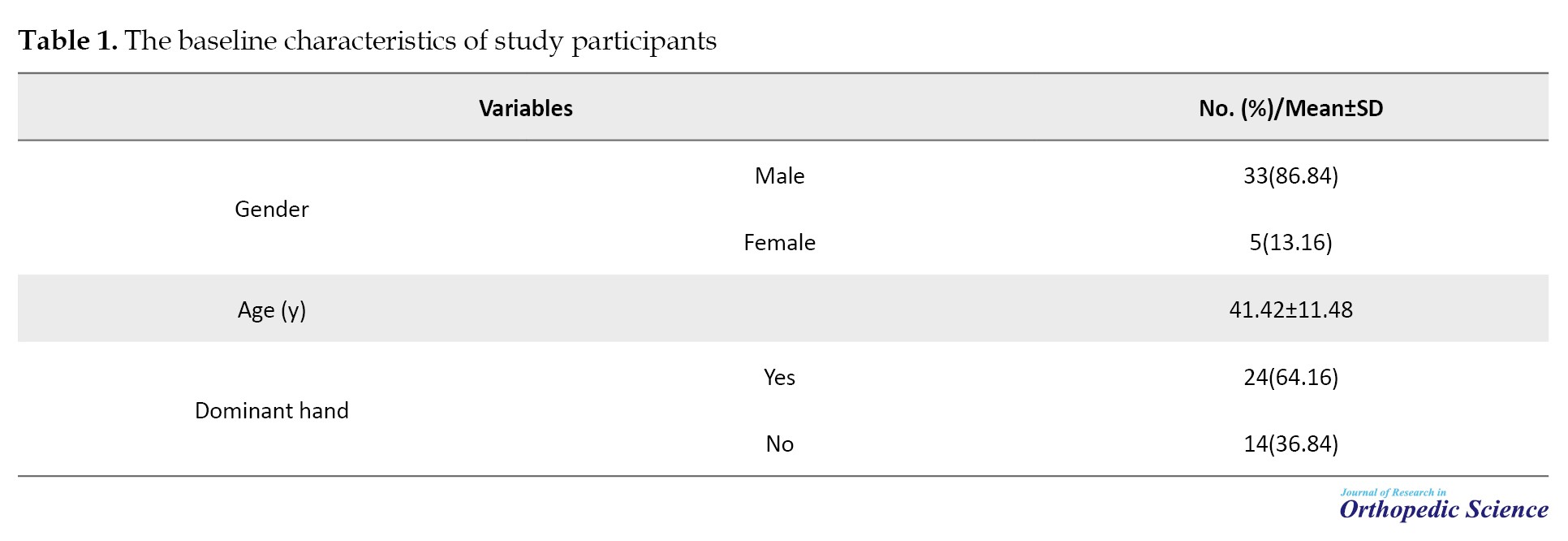
The mean age of the participants was 41.42±11.48 years. Furthermore, hand surgery was performed mainly on the dominant hand (63.16%).
Shoulder ROM following hook plate fixation in treating subacute ACJ injury was evaluated using different movements. The mean ROM of forward flexion was 157.89°, the mean ROM of abduction was 153.95°, and the mean ROM of external rotation was 50.79°, respectively (Table 2).
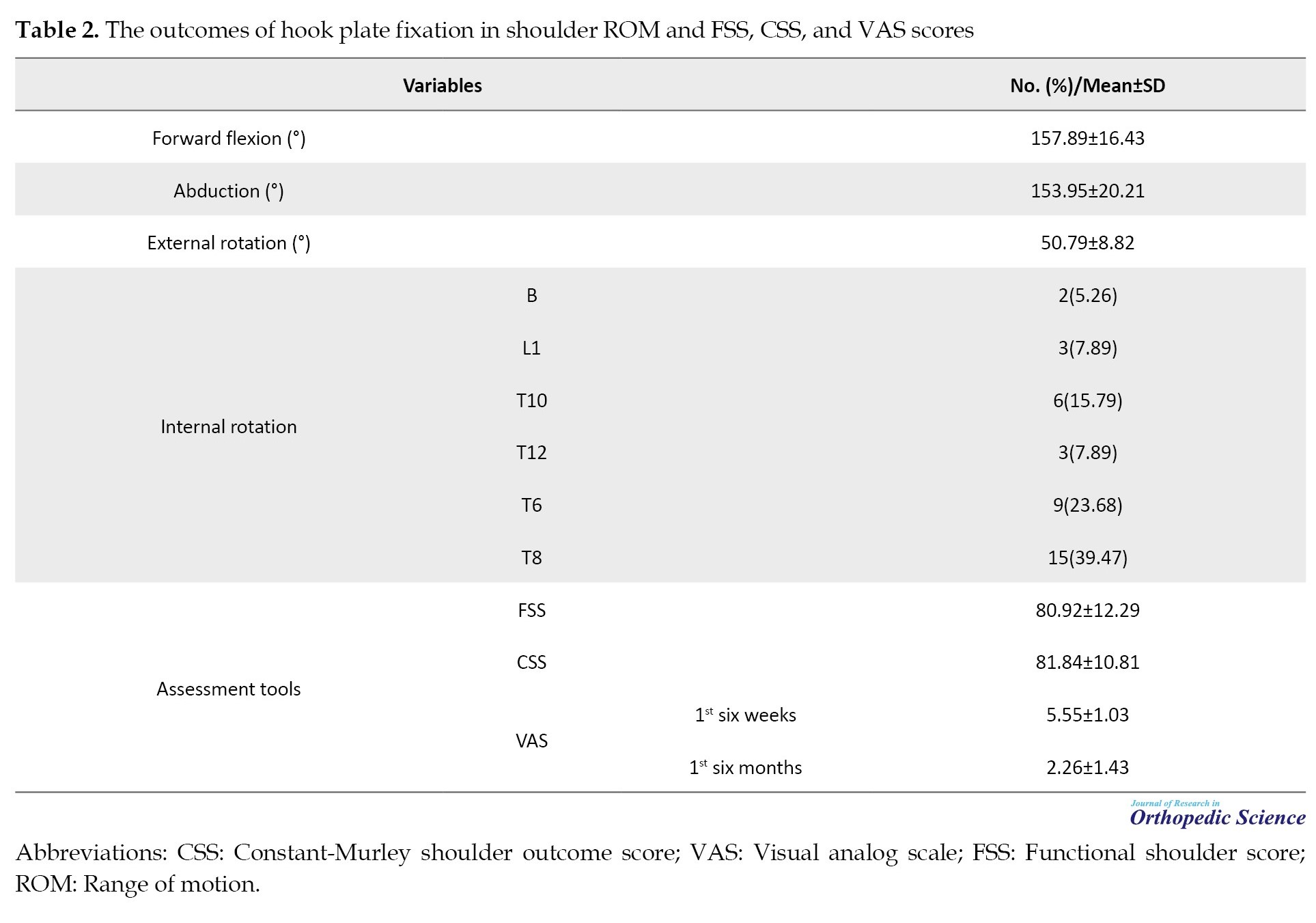
The functional shoulder score (FSS) and CSS questionnaires averaged 80.92 and 81.84, respectively (Table 2). The mean VAS was 5.55±1.03 and 2.26±1.43 in the first six weeks and six months, respectively (Table 2).
Furthermore, we evaluated complications in the study subjects. Thirty-two (84.21%) did not have post-surgical infections, and 37 patients (97.37%) did not require a second surgery.
The relationship between pain and other variables during the first six weeks was assessed. None of the variables showed significant relationships. Detailed numbers are listed in Table 3.
Assessment of the relationship between forward flexion, abduction, and external rotation ROM and different variables showed that only abduction and external rotation ROMs were significantly different between those aged ≤45 and >45 years. The other variables showed no significant differences in shoulder ROM (Table 4).
Discussion
This study investigated the clinical outcomes of hook plate fixation without ligament reconstruction in patients with subacute ACJ injuries. Most patients were men with a mean age of 41 years. The results of this study showed that pain was highest in the first six weeks post-surgery, with a mean of 70%. The pain decreased over time, with <33% reported in the first six months. None of the variables studied showed a significant relationship with the pain scale in the first six weeks. Furthermore, this study showed that age >45 is significantly associated with decreased shoulder ROM. The mean age in this study was 41 years, a few years older than anticipated [11, 12].
Despite different options to treat ACJ injuries, physicians must contemplate the best option. Some of these options are the AO technique with two Kirschner wires and a wire binder of the Zuggurtung type and transclavicular screw. The first is associated with the risk of Kirschner wire migration, while the second method poses a risk of clavicle fracture. Furthermore, in the case of clavicle fracture, the screw should be removed at an early stage, leading to further dislocation and instability of the ACJ. Another method, hook plate fixation, has been used for decades. This method provides optimal joint stability and inserts the plate above the clavicle and the hook underneath the acromion. Nevertheless, this method is also associated with some risks, including subacromial impingement [13].
The VAS score was assessed at six weeks and six months, and the CCS score was at six months in this study. Compared to a previous survey of Yan in 2017, our study showed lower numbers [14]. Some reasons are considered for the pain and reduced mobility. The insertion of the hook plate reduced the width of the subacromial space, leading to a decrease in shoulder function and elevation in bursa pressure. The presence of a hook plate restricts rotation of the humeral greater tuberosity. Direct collision with the greater tuberosity may stimulate and damage the supraspinatus muscle, leading to pain and weakness. Furthermore, the escalation of tension and stimulation originated from the hook plate and was directed toward the subacromial surface. In addition, significant subacromial surface tension may arise during procedures due to variations in shoulder thickness across patients and in insertion angle and position.
Furthermore, regarding the complications in the present study, few patients showed signs of infection or required a second surgery. Two in the hook plate group showed complications in another study of 28 patients grouped in terms of treatment method. The rate of complications in this study was comparable to that in our study; however, this study also showed that the complications that occurred in the hook plate group were not significantly different from those in the AO technique and transclavicular screw groups [13]. Another study showed that hook plate fixation did not significantly reduce complications [15].
Conclusion
Hook plate fixation surgery is effective in patients with subacute injuries of different ages. This operation significantly improves ROM in patients under or equal to 45 years of age than in those over 45, and the results do not differ based on the patient’s sex.
This study has both strengths and limitations. This study achieved a high follow-up rate, ensuring that most of the initial cohort was evaluated for outcomes. Furthermore, this study had an acceptable sample size compared to similar studies. However, the retrospective nature of this study limits its ability to control for confounding variables. Also, we conducted the study at a single hospital, which may have limited the applicability of our results to other settings or populations. However, the absence of a comparison group limits the ability to directly compare the effectiveness of different treatment approaches.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1399.408). All methods were conducted according to relevant guidelines and regulations, and informed consent was obtained from all participants.
Funding
This study was supported by the Iran University of Medical Sciences, Tehran, Iran (Grant No.: 18127).
Authors' contributions
Conceptualization: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, Mohammadreza Bahaeddini, and Babak Roshanravan; Data collection, assembly, data extraction: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, and Mohammadreza Bahaeddini; Writing the original draft: Farzaneh Merdowsi, Khatere Mokhtari, Babak Roshanravan, and Saeed Amiri; Review and editing: Morteza Nakhaei Amroodi, Pouria Tabrizian, Mojtaba Baniasadi, Mohammadreza Bahaeddini, Farzaneh Merdowsi, Khatere Mokhtari, Babak Roshanravan, and Saeed Amiri; Supervision: Pouria Tabrizian, Mojtaba Baniasadi, and Babak Roshanravan.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all individuals who helped them develop this research.
References
- Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013; 29(2):387-97. [DOI:10.1016/j.arthro.2012.11.023] [PMID]
- Fraser-Moodie JA, Shortt NL, Robinson CM. Injuries to the acromioclavicular joint. J Bone Joint Surg Br. 2008; 90(6):697-707. [DOI:10.1302/0301-620X.90B6.20704] [PMID]
- Berthold DP, Muench LN, Dyrna F, Mazzocca AD, Garvin P, Voss A, et al. Current concepts in acromioclavicular joint (AC) instability - A proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet Disord. 2022; 23(1):1078. [DOI:10.1186/s12891-022-05935-0] [PMID] [PMCID]
- FM C. The treatment of dislocations and fractures of the outer end of the clavicle. Int Clin. 1917; 1:145-69. [Link]
- Dyrna F, Berthold DP, Feucht MJ, Muench LN, Martetschläger F, Imhoff AB, et al. The importance of biomechanical properties in revision acromioclavicular joint stabilization: A scoping review. Knee Surg Sports Traumatol Arthrosc. 2019; 27(12):3844-55. [DOI:10.1007/s00167-019-05742-6] [PMID]
- Martetschläger F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013; 41(12):2896-903. [DOI:10.1177/0363546513502459] [PMID]
- Balser D. A new method for the surgical treatment of acromioclavicular dislocation [German]. Chir Prax. 1976; 24:275. [Link]
- Göhring U, Matusewicz A, Friedl W, Ruf W. [Results of treatment after different surgical procedures for management of acromioclavicular joint dislocation (German)]. Chirurg. 1993; 64(7):565-71. [PMID]
- Matsen FA, Cordasco FA, Sperling JW, Lippitt SB. Rockwood and matsen's the shoulder e-book: Rockwood and Matsen's The Shoulder E-Book. Edinburgh: Elsevier Health Sciences; 2021. [Link]
- Hirschmann MT, Wind B, Amsler F, Gross T. Reliability of shoulder abduction strength measure for the constant-murley score. Clin Orthop Relat Res. 2010; 468(6):1565-71. [DOI:10.1007/s11999-009-1007-3] [PMID] [PMCID]
- Chillemi C, Franceschini V, Dei Giudici L, Alibardi A, Salate Santone F, Ramos Alday LJ, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int. 2013; 2013:171609. [DOI:10.1155/2013/171609] [PMID] [PMCID]
- Kumar N, Sharma V. Hook plate fixation for acute acromioclavicular dislocations without coracoclavicular ligament reconstruction: A functional outcome study in military personnel. Strategies Trauma Limb Reconstr. 2015; 10(2):79-85. [DOI:10.1007/s11751-015-0228-0] [PMID] [PMCID]
- Kezunović M, Bjelica D, Popović S. Comparative study of surgical treatment of acromioclavicular luxation. Vojnosanit Pregl. 2013; 70(3):292-7. [DOI:10.2298/VSP1303292K] [PMID]
- Yan HW, Li L, Wang RC, Yang Y, Xie Y, Tang J, et al. Clinical efficacies of coracoclavicular ligament reconstruction using suture anchor versus hook plate in the treatment of distal clavicle fracture. Orthop Traumatol Surg Res. 2017; 103(8):1287-93. [DOI:10.1016/j.otsr.2017.07.006] [PMID]
- McCann PD. Surgical treatment of complete acromioclavicular dislocations. Tech Orthop. 1994; 9(2):126-32. [DOI:10.1097/00013611-199400920-00007]
Type of Study: Research Article |
Subject:
Shoulder / Elbow
Received: 2022/12/21 | Accepted: 2023/10/30 | Published: 2023/11/1
Received: 2022/12/21 | Accepted: 2023/10/30 | Published: 2023/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |