Volume 10, Issue 4 (11-2023)
JROS 2023, 10(4): 225-230 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mahdavi S M, Behjat M, Mirzaei Tirabadi N, Parvandi A, Karimpoor A. Surgical Site Infection in Spinal cord Surgery: The Enhanced and Standard Protocols of Antibiotic Prophylaxis. JROS 2023; 10 (4) :225-230
URL: http://jros.iums.ac.ir/article-1-2268-en.html
URL: http://jros.iums.ac.ir/article-1-2268-en.html
1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 440 kb]
(254 Downloads)
| Abstract (HTML) (1080 Views)
Full-Text: (253 Views)
Introduction
Vhe reasonable and appropriate use of medicines is a common goal among health professionals. This may have crucial economic, clinical, and social implications. Antibiotics are expensive drugs crucial to hospital drug budgets [1]. On the other hand, improper antibiotic prescription, including choosing the wrong antibiotic, prescribing an insufficient dose of the drug, or not prescribing the medicine at the right time, can increase the prevalence of antibiotic-resistant species [2, 3], lead to prolonged hospitalization, cause drug side effects, and waste the treatment budget. The most common source of post-surgical site infection (SSI) is contamination of normal skin flora around the surgical wound, such as Staphylococcus aureus.
SSI is a dangerous complication of spinal surgery, and “proper prevention” is key to the success of these surgeries. Several studies have reported the effectiveness of prophylactic antibiotics in reducing the incidence of SSI. The incidence of SSI in lumbar spine surgery has been reported to be 1%-4% with prophylactic antibiotics and 6%-13% without them [4, 5].
Any occurrence of SSI can increase the cost of care by up to four times the cost of primary spinal surgery [4, 5, 6, 7]. Therefore, efforts to reduce SSI are vital [8, 9].
Furthermore, conflicting reports have been published regarding the ideal timing of antimicrobial prophylaxis and the most effective preoperative skin disinfectant [10]. Based on these studies, infection risk factors and the importance of each of these factors have been identified in different studies. Risk factors for SSI include age, type of surgery, placement of foreign bodies, diabetes, and immune system deficiency. In patients undergoing spinal surgery, the difference between some of these factors can be explained by the variability of environmental and human factors. Based on the available information, we decided to compare the incidence of SSI in spine surgery patients under antibiotic prophylaxis between the improved protocol and the common protocol.
Methods
This study was approved by our institutional review board. We evaluated patients who underwent spine surgery at our center between 2019 and 2021. We divided them into two groups based on the antibiotic prophylaxis protocol used: The common protocol group, which received standard antibiotic prophylaxis, and the advanced protocol group, which received enhanced antibiotic prophylaxis.
The sample size was calculated based on previous studies that reported a SSI incidence of 10% with standard prophylaxis. We aimed to detect a 50% reduction in SSI with the enhanced protocol at a 5% significance level and 80% power, leading to the required sample size of 40 patients per group. The inclusion criteria included adults aged 18 years and older who underwent spine surgery in our hospital during the specified timeframe and received antibiotic prophylaxis before surgery. The exclusion criteria included patients requiring re-surgery within six weeks of the initial procedure, those who died shortly after surgery, individuals under 18 years of age, and patients with immune system deficiencies, uncontrolled diabetes, or active infections.
In the common protocol group, patients received one gram of intravenous cefazolin one hour before surgery, followed by one gram every six hours until discharge (two grams for patients weighing >70 kg). An additional 80 mg of intravenous gentamicin was administered every eight hours for up to 48 h post-surgery. Oral cephalexin and ciprofloxacin were prescribed from discharge until two weeks post-surgery. Cefazolin was repeated if the surgery lasted longer than three hours or if intraoperative bleeding exceeded 1500 cc. In contrast, the advanced protocol group received one gram of vancomycin and 120 mg of gentamicin one hour before surgery, with the dose repeated at 12- and 24-hours post-operation for surgeries involving instrumentation, irrespective of bleeding or duration.
Patient data were collected using a standardized form, capturing demographics, such as sex, age, and body mass index (BMI), as well as surgical details, including urgency, duration (greater than three hours), and intraoperative bleeding (greater than 1500 cc). Medical history factors included the use of corticosteroids, history of chemotherapy or radiotherapy, and intensive care unit (ICU) hospitalization. The primary outcome measured was the incidence of SSI, recorded at two, six, and twelve weeks post-surgery.
Predictors included antibiotic prophylaxis protocol (common vs. advanced), duration of surgery, intraoperative bleeding, use of corticosteroids, and history of chemotherapy/radiotherapy. Potential confounders were age, sex, BMI, and pre-existing medical conditions that could influence infection risk. The effect modifiers were the type of surgery (instrumentation vs. non-instrumentation) and urgency (elective vs. emergency). All surgeries were performed by a single surgeon at the same center to ensure consistency in surgical technique and postoperative care. This methodological framework aims to comprehensively evaluate the efficacy of different antibiotic prophylaxis protocols in reducing SSI in patients undergoing spine surgery.
Statistical analysis
Statistical analyses were performed using SPSS software, version 21. Continuous variables were presented as Means±SD and compared using independent t-tests, while categorical variables were analyzed with chi-square tests. P<0.05 was considered statistically significant.
Multivariate logistic regression was conducted to control for confounding. Variables with a P<0.20 in univariate analyses, including diabetes, ICU stay, and BMI, were entered into the model. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Spearman’s correlation coefficients were used to assess relationships between continuous variables and SSI. The model’s fit was evaluated using the Hosmer-Lemeshow test.
Results
During the study period, 81 patients undergoing spinal surgery were examined. Of these, 33 were in the advanced protocol group, and 48 were in the common protocol group. Table 1 presents the demographic information of the patients.
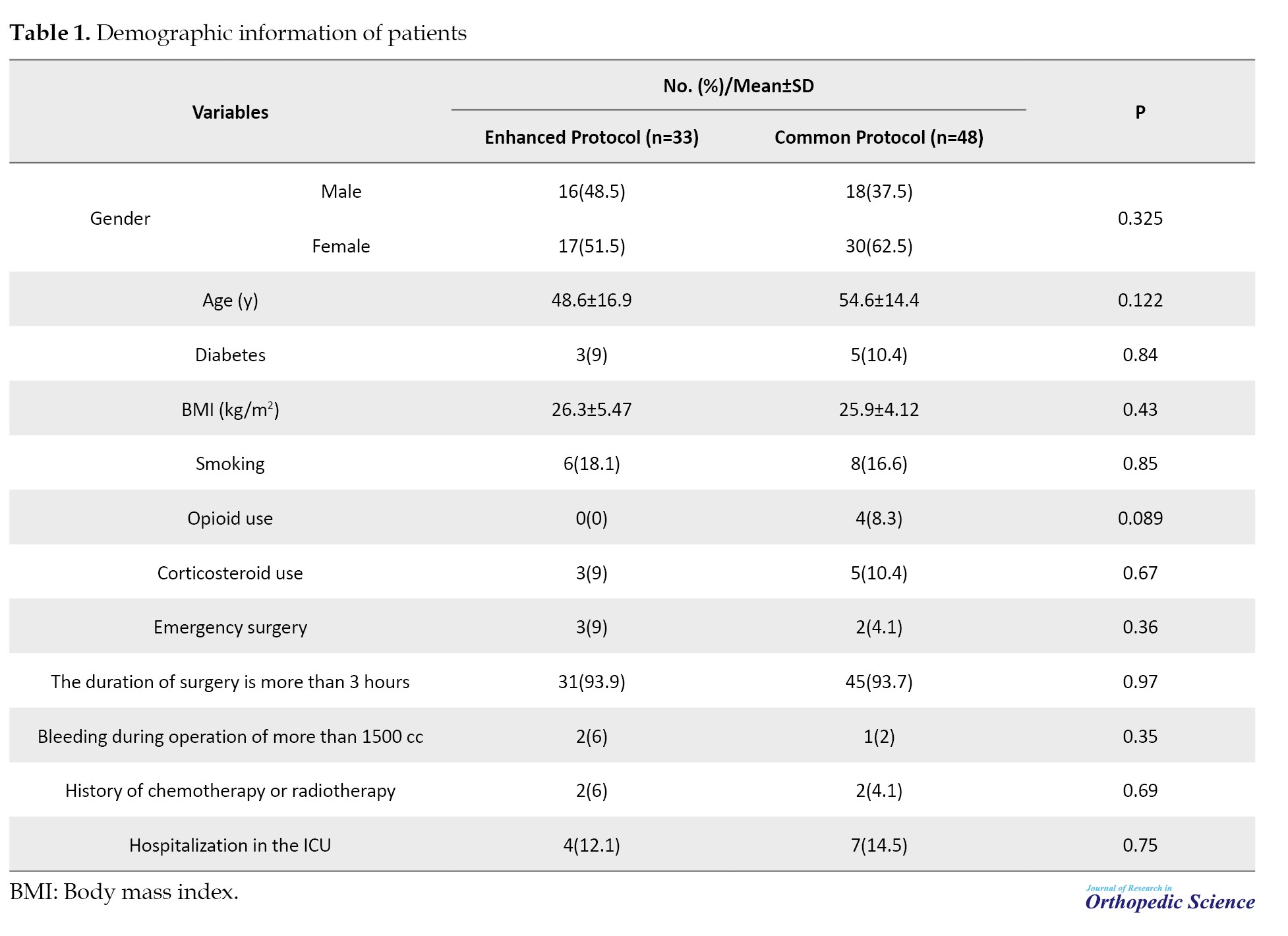
The baseline characteristics of the patients in the enhanced protocol group (n=33) and the common protocol group (n=48) were compared using chi-square tests for categorical variables and independent t-tests for continuous variables. The patients in the two groups did not differ significantly in terms of sex distribution (P=0.325), age (mean age 38.1±21.2 years in the enhanced protocol group vs 38.2±20.8 years in the common protocol group; P=0.85), or BMI (mean BMI 26.3±5.4 in the enhanced protocol group vs 25.9±4.1 in the common protocol group; P=0.43).
The primary outcome, SSI incidence, was 2.5% and 10% in the enhanced protocol group and 10% in the common protocol group, respectively. Logistic regression analysis was used to estimate unadjusted and adjusted ORs for SSI occurrence. In unadjusted analyses, patients in the common protocol group had a significantly higher risk of SSI (OR=4.33; 95% CI, 1.15%, 16.33%; P=0.03). After adjusting for diabetes status, ICU stay, and BMI, the relationship remained significant (adjusted OR=3.95; 95% CI, 1.10%, 15.24%; P=0.04).
The Hosmer-Lemeshow test indicated a good fit for the logistic regression model (P=0.72), and Spearman’s correlation analysis identified a significant correlation between ICU length of stay and SSI occurrence (r=0.47, P=0.001) and between BMI and SSI (r=0.24, P=0.02). This analysis suggests that both prolonged ICU stay and elevated BMI are associated with increased SSI risk, independent of the antibiotic protocol used.
No statistically significant differences were observed between the two groups in any case.
After the investigations, it was found that among the patients in the common protocol group, four people (10%) had an SSI. This was even though in the advanced protocol group, only one person (2.5%) had an infection with a positive culture, and one person (2.5%) had a secretion with a hostile culture. This difference in the incidence of SSI among patients receiving from advanced and common protocols is not statistically significant based on the chi-square test (P=0.33).
Based on Spearman’s correlation coefficient, no correlation was observed between sex (P=0.928) and age (P=0.334) of the patients and SSI. No relationship was found between smoking (P=0.336) and opioid abuse (P=0.111) with the incidence of SSI.
In the common protocol group, 15% of diabetic patients who underwent surgery had SSI. The incidence of SSI in non-diabetic patients was 5%. While in the advanced protocol group, none of the people with diabetics had SSI, and only one non-diabetic person had SSI, which was statistically significant based on Spearman’s correlation coefficient (P=0.001, r=0.431). This indicates that diabetes has a significant relationship with SSI. No significant relationship was observed between the use of corticosteroids and the incidence of SSI (P<0.05).
A total of 76 patients (93.8%) underwent elective surgery, and the rest (5 [6.2%]) underwent emergency surgery. Performing emergency surgery had no significant relationship with gender (P=0.077); however, its relationship with younger age was significant (P=0.001). In the following section, other variables with the possibility of an effect on ISS are mentioned. Because only one person from the advanced protocol group had an SSI. Therefore, the relationship between the mentioned variables and the occurrence of SSI was investigated, and a comparison between the two groups with different protocols was impossible. It should be mentioned that the advanced protocol group had significantly less SSI than the common protocol group based on Spearman’s correlation coefficient (P=0.001). The incidence of SSI in patients who underwent surgery for >3 h was 13.3%, which was equal to 5% for less than three h.
However, the incidence of SSI increases with an increase in the length of the ICU stay. The incidence of SSI in patients who were not admitted to the ICU after surgery was 5%. Based on Spearman’s correlation coefficient (P=0.001, r=0.477), a significant relationship was observed between hospitalization in ICU and SSI.
Also, the incidence of SSI increases with increasing BMI. A significant relationship was observed between high BMI and suffering from SSI based on Spearman’s correlation coefficient (P=0.001, r=0.243). No significant relationship was observed between the volume of bleeding (<1500 cc) and SSI incidence (P<0.05). History of chemotherapy or radiotherapy and suffering from SSI was not statistically significant (P<0.05). The items are listed in Table 1.
Table 2 summarizes the types of surgery performed in the common (n=48) and enhanced (n=33) protocol groups.
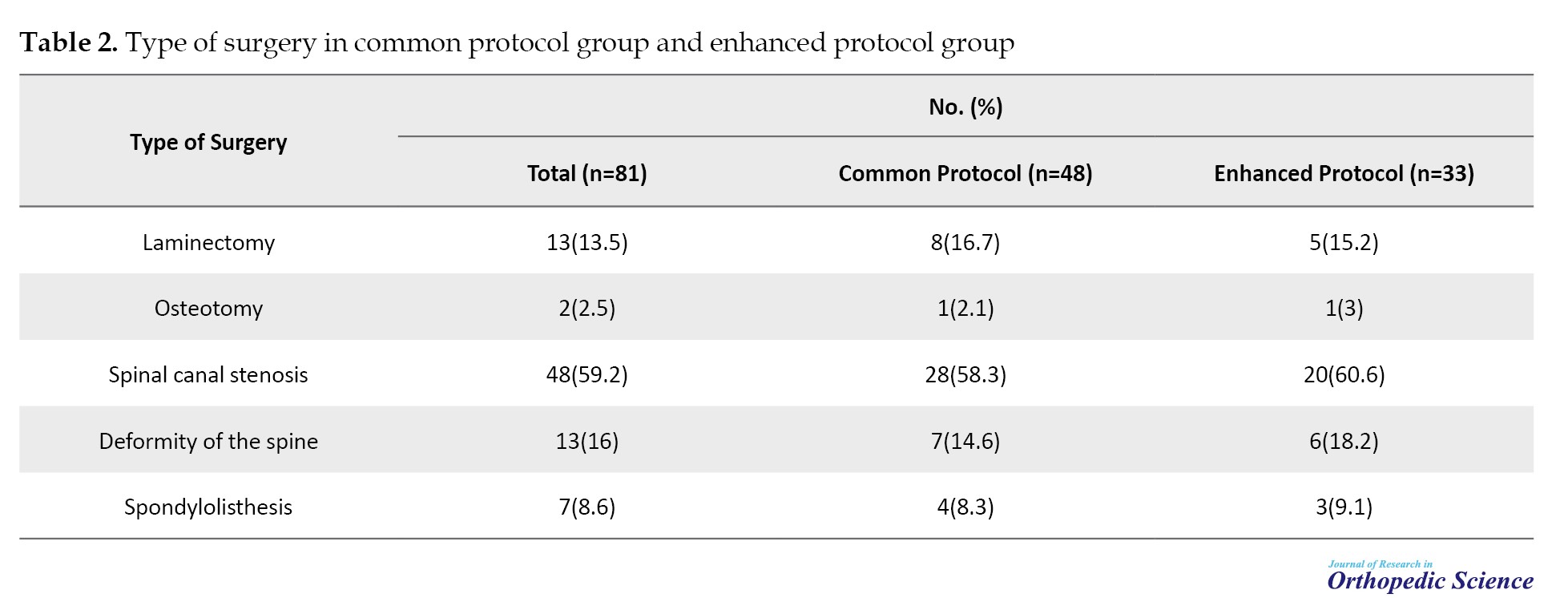
Spinal canal stenosis was the most frequent surgery in both groups (59.2% overall), followed by deformity of the spine (16%) and laminectomy (13.5%). The distribution of surgeries was similar between groups, with no significant differences observed.
Discussion
In the present study, 81 patients undergoing spinal surgery were examined. Of these, 48 were in the advanced protocol group, and 33 were in the common protocol group. In the common protocol group, 18 participants were men and 30 were women; in the advanced protocol group, 16 were men, and 17 were women. Also, the average age of the subjects studied in the advanced and common protocols groups was 48.6±16.9 years and 54.6±14.4 years, respectively, which did not have significant differences. After the investigations, it was found that among the patients in the common protocol group, four (10%) had an SSI. This was even though in the advanced protocol group, only one person (2.5%) had an infection with a positive culture, and one person (2.5%) had a secretion with a hostile culture. This difference in the incidence of SSI among patients receiving the two advanced and common protocols was not statistically significant. In this study, hospitalization in the ICU, diabetes, and BMI >25 were significantly associated with the occurrence of SSI. However, the use of a common protocol, sex, emergency surgery, length of surgery, corticosteroid use, smoking, opioid abuse, bleeding >1500 cc during surgery, and history of chemotherapy or radiotherapy had no significant relationship with the occurrence of SSI. A similar study conducted by Durand et al. in 2013 on the factors influencing SSI in orthopedic surgeries suggested smoking as an influencing factor for SSI [11].
However, in the present study, no relationship was found between smoking, opioid abuse, and the SSI incidence. A similar study conducted by Chen et al. in 2009 on the effect of diabetes on SSI in patients undergoing orthopedic surgery identified diabetes as a factor affecting SSIs [12]. In the present study, a significant relationship between diabetes and the occurrence of SSI was observed compared to the absence of diabetes in the common protocol group. In a study conducted by Compagnoni et al. in 2020 on the relationship between corticosteroid injection and SSI in patients undergoing shoulder joint surgery, a significant relationship was found between the two. However, more studies are recommended in this field [13].
However, no significant relationship was observed between corticosteroid use and SSI incidence in the present study. In similar studies conducted by Blam et al. in 2003 on the factors affecting spinal SSI, hospitalization in the ICU was reported to increase the probability of SSI occurrence [14].
In the present study, the incidence of SSI increased with the length of ICU stay. The incidence of SSI in patients who were not admitted to the ICU after surgery was 5%. A similar study conducted by Mollahosseini in 2009 discussed the risk factors affecting SSI in patients undergoing spine and brain surgery, shunt operation, entering the paranasal sinuses, cerebrospinal fluid leakage, duration of surgery >3 hours, foreign body operation, repeated lumbar punctures, urinary catheterization, hospitalization in the ICU, and the duration of hospitalization in the ICU increased the risk of SSI [15].
Conclusion
In the present study, patients in the improved protocol group suffered less SSI than those in the standard protocol group, although this difference was insignificant. Diabetes and increased duration of hospitalization in the ICU were found to be factors affecting SSI. However, age, sex, corticosteroid use, smoking, emergency or elective surgery, bleeding volume, chemotherapy and radiotherapy, and opening of the dura were not related to SSI.
Limitations
The manuscript on SSI in patients undergoing spinal cord surgery may be affected by several factors. Selection bias is possible due to the study’s single-center design and exclusion criteria, which could limit generalizability. Confounding variables may not be fully controlled, and residual confounding can influence the results. Observer bias may arise since all surgeries were performed by a single surgeon, potentially affecting outcomes assessment. Measurement bias is a concern if the SSI diagnosis criteria or follow-up timing varies. Additionally, recall bias may result from retrospective data collection, and the small sample size may limit the statistical power to detect significant differences. Addressing these potential biases would enhance the study’s validity and reliability.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1399.768).
Funding
This paper was extracted from the residency thesis of Amer Karimpoor, approved by the Department of Orthopedic Surgery, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization, supervision and funding acquisition: Seyed Mani Mahdavi; Software, project administration and formal analysis: Morteza Behjat; Validation, resources and visualization: Nahid Mirzaei Tirabadi; Data curation and writing the original draft: Ava Parvandi; Methodology, investigation, review and editing: Amer Karimpoor.
Conflict of interest
The authors declared no conflict of interest.
Vhe reasonable and appropriate use of medicines is a common goal among health professionals. This may have crucial economic, clinical, and social implications. Antibiotics are expensive drugs crucial to hospital drug budgets [1]. On the other hand, improper antibiotic prescription, including choosing the wrong antibiotic, prescribing an insufficient dose of the drug, or not prescribing the medicine at the right time, can increase the prevalence of antibiotic-resistant species [2, 3], lead to prolonged hospitalization, cause drug side effects, and waste the treatment budget. The most common source of post-surgical site infection (SSI) is contamination of normal skin flora around the surgical wound, such as Staphylococcus aureus.
SSI is a dangerous complication of spinal surgery, and “proper prevention” is key to the success of these surgeries. Several studies have reported the effectiveness of prophylactic antibiotics in reducing the incidence of SSI. The incidence of SSI in lumbar spine surgery has been reported to be 1%-4% with prophylactic antibiotics and 6%-13% without them [4, 5].
Any occurrence of SSI can increase the cost of care by up to four times the cost of primary spinal surgery [4, 5, 6, 7]. Therefore, efforts to reduce SSI are vital [8, 9].
Furthermore, conflicting reports have been published regarding the ideal timing of antimicrobial prophylaxis and the most effective preoperative skin disinfectant [10]. Based on these studies, infection risk factors and the importance of each of these factors have been identified in different studies. Risk factors for SSI include age, type of surgery, placement of foreign bodies, diabetes, and immune system deficiency. In patients undergoing spinal surgery, the difference between some of these factors can be explained by the variability of environmental and human factors. Based on the available information, we decided to compare the incidence of SSI in spine surgery patients under antibiotic prophylaxis between the improved protocol and the common protocol.
Methods
This study was approved by our institutional review board. We evaluated patients who underwent spine surgery at our center between 2019 and 2021. We divided them into two groups based on the antibiotic prophylaxis protocol used: The common protocol group, which received standard antibiotic prophylaxis, and the advanced protocol group, which received enhanced antibiotic prophylaxis.
The sample size was calculated based on previous studies that reported a SSI incidence of 10% with standard prophylaxis. We aimed to detect a 50% reduction in SSI with the enhanced protocol at a 5% significance level and 80% power, leading to the required sample size of 40 patients per group. The inclusion criteria included adults aged 18 years and older who underwent spine surgery in our hospital during the specified timeframe and received antibiotic prophylaxis before surgery. The exclusion criteria included patients requiring re-surgery within six weeks of the initial procedure, those who died shortly after surgery, individuals under 18 years of age, and patients with immune system deficiencies, uncontrolled diabetes, or active infections.
In the common protocol group, patients received one gram of intravenous cefazolin one hour before surgery, followed by one gram every six hours until discharge (two grams for patients weighing >70 kg). An additional 80 mg of intravenous gentamicin was administered every eight hours for up to 48 h post-surgery. Oral cephalexin and ciprofloxacin were prescribed from discharge until two weeks post-surgery. Cefazolin was repeated if the surgery lasted longer than three hours or if intraoperative bleeding exceeded 1500 cc. In contrast, the advanced protocol group received one gram of vancomycin and 120 mg of gentamicin one hour before surgery, with the dose repeated at 12- and 24-hours post-operation for surgeries involving instrumentation, irrespective of bleeding or duration.
Patient data were collected using a standardized form, capturing demographics, such as sex, age, and body mass index (BMI), as well as surgical details, including urgency, duration (greater than three hours), and intraoperative bleeding (greater than 1500 cc). Medical history factors included the use of corticosteroids, history of chemotherapy or radiotherapy, and intensive care unit (ICU) hospitalization. The primary outcome measured was the incidence of SSI, recorded at two, six, and twelve weeks post-surgery.
Predictors included antibiotic prophylaxis protocol (common vs. advanced), duration of surgery, intraoperative bleeding, use of corticosteroids, and history of chemotherapy/radiotherapy. Potential confounders were age, sex, BMI, and pre-existing medical conditions that could influence infection risk. The effect modifiers were the type of surgery (instrumentation vs. non-instrumentation) and urgency (elective vs. emergency). All surgeries were performed by a single surgeon at the same center to ensure consistency in surgical technique and postoperative care. This methodological framework aims to comprehensively evaluate the efficacy of different antibiotic prophylaxis protocols in reducing SSI in patients undergoing spine surgery.
Statistical analysis
Statistical analyses were performed using SPSS software, version 21. Continuous variables were presented as Means±SD and compared using independent t-tests, while categorical variables were analyzed with chi-square tests. P<0.05 was considered statistically significant.
Multivariate logistic regression was conducted to control for confounding. Variables with a P<0.20 in univariate analyses, including diabetes, ICU stay, and BMI, were entered into the model. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Spearman’s correlation coefficients were used to assess relationships between continuous variables and SSI. The model’s fit was evaluated using the Hosmer-Lemeshow test.
Results
During the study period, 81 patients undergoing spinal surgery were examined. Of these, 33 were in the advanced protocol group, and 48 were in the common protocol group. Table 1 presents the demographic information of the patients.
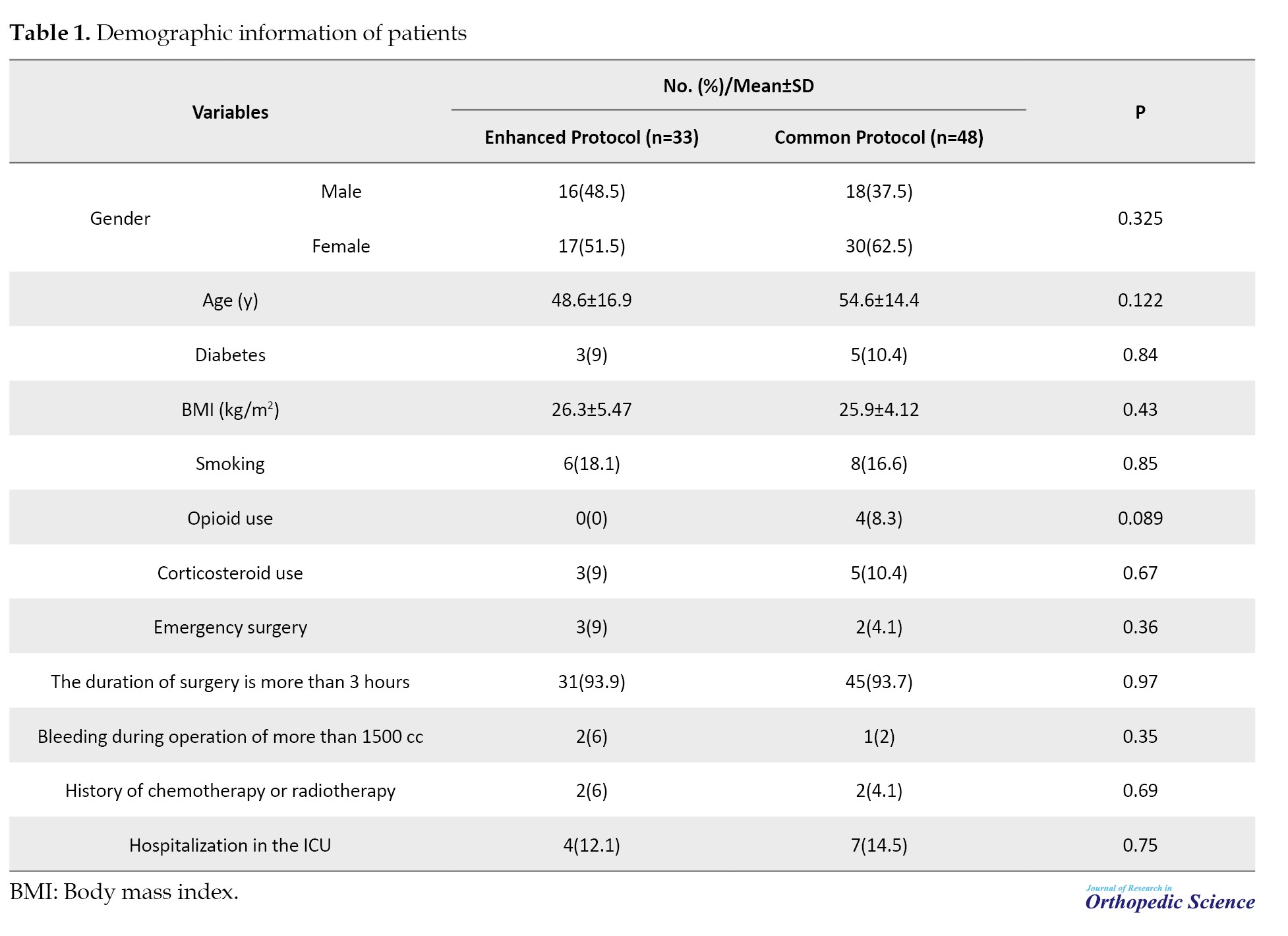
The baseline characteristics of the patients in the enhanced protocol group (n=33) and the common protocol group (n=48) were compared using chi-square tests for categorical variables and independent t-tests for continuous variables. The patients in the two groups did not differ significantly in terms of sex distribution (P=0.325), age (mean age 38.1±21.2 years in the enhanced protocol group vs 38.2±20.8 years in the common protocol group; P=0.85), or BMI (mean BMI 26.3±5.4 in the enhanced protocol group vs 25.9±4.1 in the common protocol group; P=0.43).
The primary outcome, SSI incidence, was 2.5% and 10% in the enhanced protocol group and 10% in the common protocol group, respectively. Logistic regression analysis was used to estimate unadjusted and adjusted ORs for SSI occurrence. In unadjusted analyses, patients in the common protocol group had a significantly higher risk of SSI (OR=4.33; 95% CI, 1.15%, 16.33%; P=0.03). After adjusting for diabetes status, ICU stay, and BMI, the relationship remained significant (adjusted OR=3.95; 95% CI, 1.10%, 15.24%; P=0.04).
The Hosmer-Lemeshow test indicated a good fit for the logistic regression model (P=0.72), and Spearman’s correlation analysis identified a significant correlation between ICU length of stay and SSI occurrence (r=0.47, P=0.001) and between BMI and SSI (r=0.24, P=0.02). This analysis suggests that both prolonged ICU stay and elevated BMI are associated with increased SSI risk, independent of the antibiotic protocol used.
No statistically significant differences were observed between the two groups in any case.
After the investigations, it was found that among the patients in the common protocol group, four people (10%) had an SSI. This was even though in the advanced protocol group, only one person (2.5%) had an infection with a positive culture, and one person (2.5%) had a secretion with a hostile culture. This difference in the incidence of SSI among patients receiving from advanced and common protocols is not statistically significant based on the chi-square test (P=0.33).
Based on Spearman’s correlation coefficient, no correlation was observed between sex (P=0.928) and age (P=0.334) of the patients and SSI. No relationship was found between smoking (P=0.336) and opioid abuse (P=0.111) with the incidence of SSI.
In the common protocol group, 15% of diabetic patients who underwent surgery had SSI. The incidence of SSI in non-diabetic patients was 5%. While in the advanced protocol group, none of the people with diabetics had SSI, and only one non-diabetic person had SSI, which was statistically significant based on Spearman’s correlation coefficient (P=0.001, r=0.431). This indicates that diabetes has a significant relationship with SSI. No significant relationship was observed between the use of corticosteroids and the incidence of SSI (P<0.05).
A total of 76 patients (93.8%) underwent elective surgery, and the rest (5 [6.2%]) underwent emergency surgery. Performing emergency surgery had no significant relationship with gender (P=0.077); however, its relationship with younger age was significant (P=0.001). In the following section, other variables with the possibility of an effect on ISS are mentioned. Because only one person from the advanced protocol group had an SSI. Therefore, the relationship between the mentioned variables and the occurrence of SSI was investigated, and a comparison between the two groups with different protocols was impossible. It should be mentioned that the advanced protocol group had significantly less SSI than the common protocol group based on Spearman’s correlation coefficient (P=0.001). The incidence of SSI in patients who underwent surgery for >3 h was 13.3%, which was equal to 5% for less than three h.
However, the incidence of SSI increases with an increase in the length of the ICU stay. The incidence of SSI in patients who were not admitted to the ICU after surgery was 5%. Based on Spearman’s correlation coefficient (P=0.001, r=0.477), a significant relationship was observed between hospitalization in ICU and SSI.
Also, the incidence of SSI increases with increasing BMI. A significant relationship was observed between high BMI and suffering from SSI based on Spearman’s correlation coefficient (P=0.001, r=0.243). No significant relationship was observed between the volume of bleeding (<1500 cc) and SSI incidence (P<0.05). History of chemotherapy or radiotherapy and suffering from SSI was not statistically significant (P<0.05). The items are listed in Table 1.
Table 2 summarizes the types of surgery performed in the common (n=48) and enhanced (n=33) protocol groups.
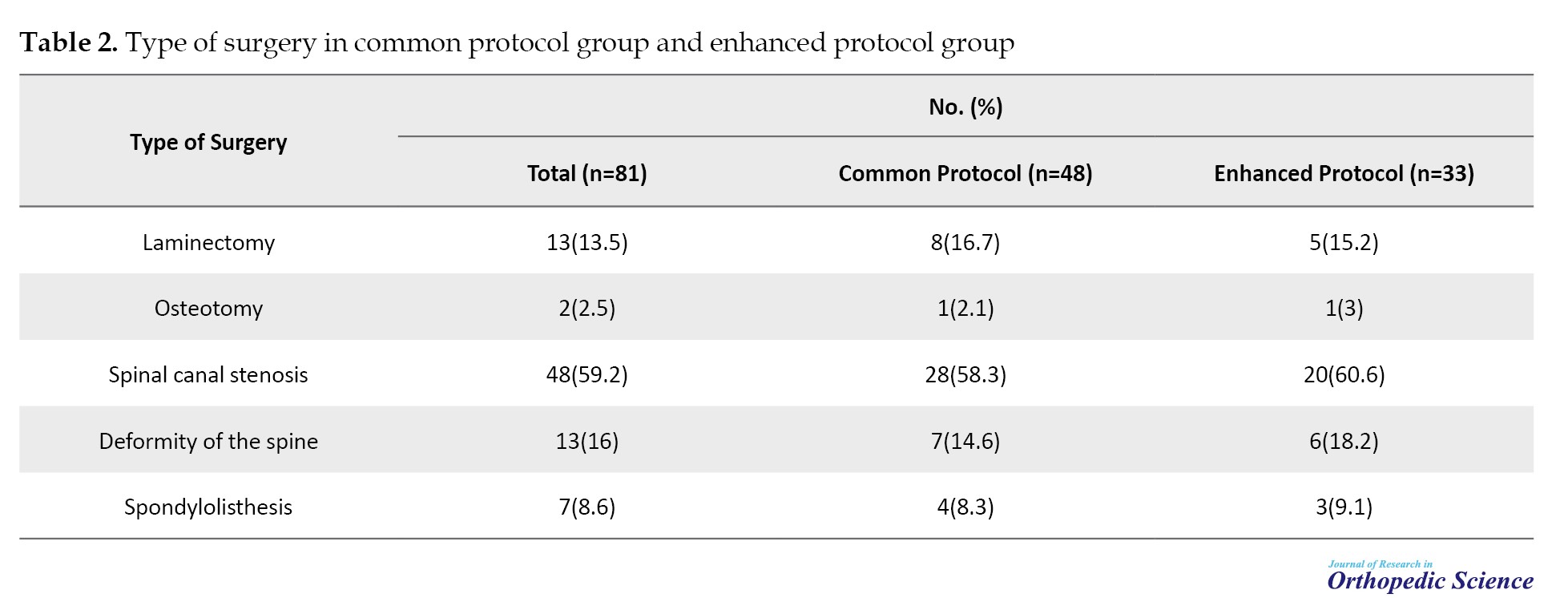
Spinal canal stenosis was the most frequent surgery in both groups (59.2% overall), followed by deformity of the spine (16%) and laminectomy (13.5%). The distribution of surgeries was similar between groups, with no significant differences observed.
Discussion
In the present study, 81 patients undergoing spinal surgery were examined. Of these, 48 were in the advanced protocol group, and 33 were in the common protocol group. In the common protocol group, 18 participants were men and 30 were women; in the advanced protocol group, 16 were men, and 17 were women. Also, the average age of the subjects studied in the advanced and common protocols groups was 48.6±16.9 years and 54.6±14.4 years, respectively, which did not have significant differences. After the investigations, it was found that among the patients in the common protocol group, four (10%) had an SSI. This was even though in the advanced protocol group, only one person (2.5%) had an infection with a positive culture, and one person (2.5%) had a secretion with a hostile culture. This difference in the incidence of SSI among patients receiving the two advanced and common protocols was not statistically significant. In this study, hospitalization in the ICU, diabetes, and BMI >25 were significantly associated with the occurrence of SSI. However, the use of a common protocol, sex, emergency surgery, length of surgery, corticosteroid use, smoking, opioid abuse, bleeding >1500 cc during surgery, and history of chemotherapy or radiotherapy had no significant relationship with the occurrence of SSI. A similar study conducted by Durand et al. in 2013 on the factors influencing SSI in orthopedic surgeries suggested smoking as an influencing factor for SSI [11].
However, in the present study, no relationship was found between smoking, opioid abuse, and the SSI incidence. A similar study conducted by Chen et al. in 2009 on the effect of diabetes on SSI in patients undergoing orthopedic surgery identified diabetes as a factor affecting SSIs [12]. In the present study, a significant relationship between diabetes and the occurrence of SSI was observed compared to the absence of diabetes in the common protocol group. In a study conducted by Compagnoni et al. in 2020 on the relationship between corticosteroid injection and SSI in patients undergoing shoulder joint surgery, a significant relationship was found between the two. However, more studies are recommended in this field [13].
However, no significant relationship was observed between corticosteroid use and SSI incidence in the present study. In similar studies conducted by Blam et al. in 2003 on the factors affecting spinal SSI, hospitalization in the ICU was reported to increase the probability of SSI occurrence [14].
In the present study, the incidence of SSI increased with the length of ICU stay. The incidence of SSI in patients who were not admitted to the ICU after surgery was 5%. A similar study conducted by Mollahosseini in 2009 discussed the risk factors affecting SSI in patients undergoing spine and brain surgery, shunt operation, entering the paranasal sinuses, cerebrospinal fluid leakage, duration of surgery >3 hours, foreign body operation, repeated lumbar punctures, urinary catheterization, hospitalization in the ICU, and the duration of hospitalization in the ICU increased the risk of SSI [15].
Conclusion
In the present study, patients in the improved protocol group suffered less SSI than those in the standard protocol group, although this difference was insignificant. Diabetes and increased duration of hospitalization in the ICU were found to be factors affecting SSI. However, age, sex, corticosteroid use, smoking, emergency or elective surgery, bleeding volume, chemotherapy and radiotherapy, and opening of the dura were not related to SSI.
Limitations
The manuscript on SSI in patients undergoing spinal cord surgery may be affected by several factors. Selection bias is possible due to the study’s single-center design and exclusion criteria, which could limit generalizability. Confounding variables may not be fully controlled, and residual confounding can influence the results. Observer bias may arise since all surgeries were performed by a single surgeon, potentially affecting outcomes assessment. Measurement bias is a concern if the SSI diagnosis criteria or follow-up timing varies. Additionally, recall bias may result from retrospective data collection, and the small sample size may limit the statistical power to detect significant differences. Addressing these potential biases would enhance the study’s validity and reliability.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1399.768).
Funding
This paper was extracted from the residency thesis of Amer Karimpoor, approved by the Department of Orthopedic Surgery, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Authors' contributions
Conceptualization, supervision and funding acquisition: Seyed Mani Mahdavi; Software, project administration and formal analysis: Morteza Behjat; Validation, resources and visualization: Nahid Mirzaei Tirabadi; Data curation and writing the original draft: Ava Parvandi; Methodology, investigation, review and editing: Amer Karimpoor.
Conflict of interest
The authors declared no conflict of interest.
References
- Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: Adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002; 23(4):183-9. [DOI:10.1086/502033] [PMID]
- Woods RK, Dellinger EP. Current guidelines for antibiotic prophylaxis of surgical wounds. Am Fam Phys. 1998; 57(11):2731-40. [Link]
- Salkind AR, Rao KC. Antibiotic prophylaxis to prevent surgical site infections. Am Fam Phys. 2011; 83(5):585-90. [Link]
- Tubaki VR, Rajasekaran S, Shetty AP. Effects of using intravenous antibiotic only versus local intrawound vancomycin antibiotic powder application in addition to intravenous antibiotics on postoperative infection in spine surgery in 907 patients. Spine. 2013; 38(25):2149-55. [DOI:10.1097/BRS.0000000000000015] [PMID]
- Rechtine GR, Bono PL, Cahill D, Bolesta MJ, Chrin AM. Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma. 2001; 15(8):566-9. [DOI:10.1097/00005131-200111000-00006] [PMID]
- Rohde V, Meyer B, Schaller C, Hassler WE. Spondylodiscitis after lumbar discectomy. Incidence and a proposal for prophylaxis. Spine. 1998; 23(5):615-20. [DOI:10.1097/00007632-199803010-00016] [PMID]
- Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003; 85(11):2089-92. [DOI:10.2106/00004623-200311000-00004] [PMID]
- Abdul-Jabbar A, Berven SH, Hu SS, Chou D, Mummaneni PV, et al. Surgical site infections in spine surgery: Identification of microbiologic and surgical characteristics in 239 cases. Spine. 2013; 38(22):E1425-31. [DOI:10.1097/BRS.0b013e3182a42a68] [PMID]
- Lizán-García M, García-Caballero J, Asensio-Vegas A. Risk factors for surgical-wound infection in general surgery: A prospective study. Infect Control Hosp Epidemiol. 1997; 18(5):310-5. [DOI:10.2307/30141223] [PMID]
- Kanayama M, Hashimoto T, Shigenobu K, Oha F, Togawa D. Effective prevention of surgical site infection using a centers for disease control and prevention guideline-based antimicrobial prophylaxis in lumbar spine surgery. J Neurosurg Spine. 2007; 6(4):327-9. [DOI:10.3171/spi.2007.6.4.7] [PMID]
- Durand F, Berthelot P, Cazorla C, Farizon F, Lucht F. Smoking is a risk factor of organ/space surgical site infection in orthopaedic surgery with implant materials. Int Orthop. 2013; 37(4):723-7. [DOI:10.1007/s00264-013-1814-8] [PMID] [PMCID]
- Chen S, Anderson MV, Cheng WK, Wongworawat MD. Diabetes associated with increased surgical site infections in spinal arthrodesis. Clin Orthop Relat Res. 2009; 467(7):1670-3. [DOI:10.1007/s11999-009-0740-y] [PMID] [PMCID]
- Compagnoni R, Randelli P. Correlation between corticosteroid injections and surgical site infections in shoulder arthroscopy. Ann Transl Med. 2020; 8(7):513. [DOI: 10.21037/atm.2020.01.25] [PMID]
- Blam OG, Vaccaro AR, Vanichkachorn JS, Albert TJ, Hilibrand AS, Minnich JM, et al. Risk factors for surgical site infection in the patient with spinal injury. Spine. 2003; 28(13):1475-80. [DOI:10.1097/01.BRS.0000067109.23914.0A] [PMID]
- Mollahoseini R, Ghorbani, M, Moradi Lakeh M. [Risk factor for surgical site infection in neurosurgery patients with antibiotic prophylaxis (Persian)]. Razi J Med Sci. 2009; 16(62):179-85. [Link]
Type of Study: Research Article |
Subject:
Spine surgery
Received: 2022/01/4 | Accepted: 2023/01/7 | Published: 2023/11/1
Received: 2022/01/4 | Accepted: 2023/01/7 | Published: 2023/11/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |