Volume 11, Issue 1 (2-2024)
JROS 2024, 11(1): 15-22 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Biglari F, Sabaghzadeh A, Sadighi M, Behnaz F, Goli M, Kafiabadi M J, et al . Risk Factors of Venous Congestion After Reverse Sural Artery Flap. JROS 2024; 11 (1) :15-22
URL: http://jros.iums.ac.ir/article-1-2270-en.html
URL: http://jros.iums.ac.ir/article-1-2270-en.html
Farsad Biglari1 

 , Amir Sabaghzadeh1
, Amir Sabaghzadeh1 

 , Mehrdad Sadighi1
, Mehrdad Sadighi1 

 , Faranak Behnaz2
, Faranak Behnaz2 
 , Mohammadali Goli3
, Mohammadali Goli3 
 , Meisam Jafari Kafiabadi4
, Meisam Jafari Kafiabadi4 

 , Mohammad Ali Okhovatpour5
, Mohammad Ali Okhovatpour5 

 , Adel Ebrahimpour6
, Adel Ebrahimpour6 




 , Amir Sabaghzadeh1
, Amir Sabaghzadeh1 

 , Mehrdad Sadighi1
, Mehrdad Sadighi1 

 , Faranak Behnaz2
, Faranak Behnaz2 
 , Mohammadali Goli3
, Mohammadali Goli3 
 , Meisam Jafari Kafiabadi4
, Meisam Jafari Kafiabadi4 

 , Mohammad Ali Okhovatpour5
, Mohammad Ali Okhovatpour5 

 , Adel Ebrahimpour6
, Adel Ebrahimpour6 


1- Department of Orthopedic Surgery, School of Medicine, Clinical Research Development Unit of Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Anesthesiology, School of Medicine, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Student Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedic Surgery, School of Medicine, Clinical Research Development Unit of Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. & Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Orthopedics, Taleghani Hospital Research Development Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Department of Orthopedic Surgery, School of Medicine, Clinical Research Development Unit of Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. & Physiotherapy Research Center, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Anesthesiology, School of Medicine, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Student Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Orthopedic Surgery, School of Medicine, Clinical Research Development Unit of Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. & Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
5- Department of Orthopedics, Taleghani Hospital Research Development Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
6- Department of Orthopedic Surgery, School of Medicine, Clinical Research Development Unit of Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran. & Physiotherapy Research Center, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Distal tibia, Reverse sural, Artery, Flap, Risk factor, Soft tissue repair, Venous congestion
Full-Text [PDF 3923 kb]
(331 Downloads)
| Abstract (HTML) (846 Views)
Full-Text: (362 Views)
Introduction
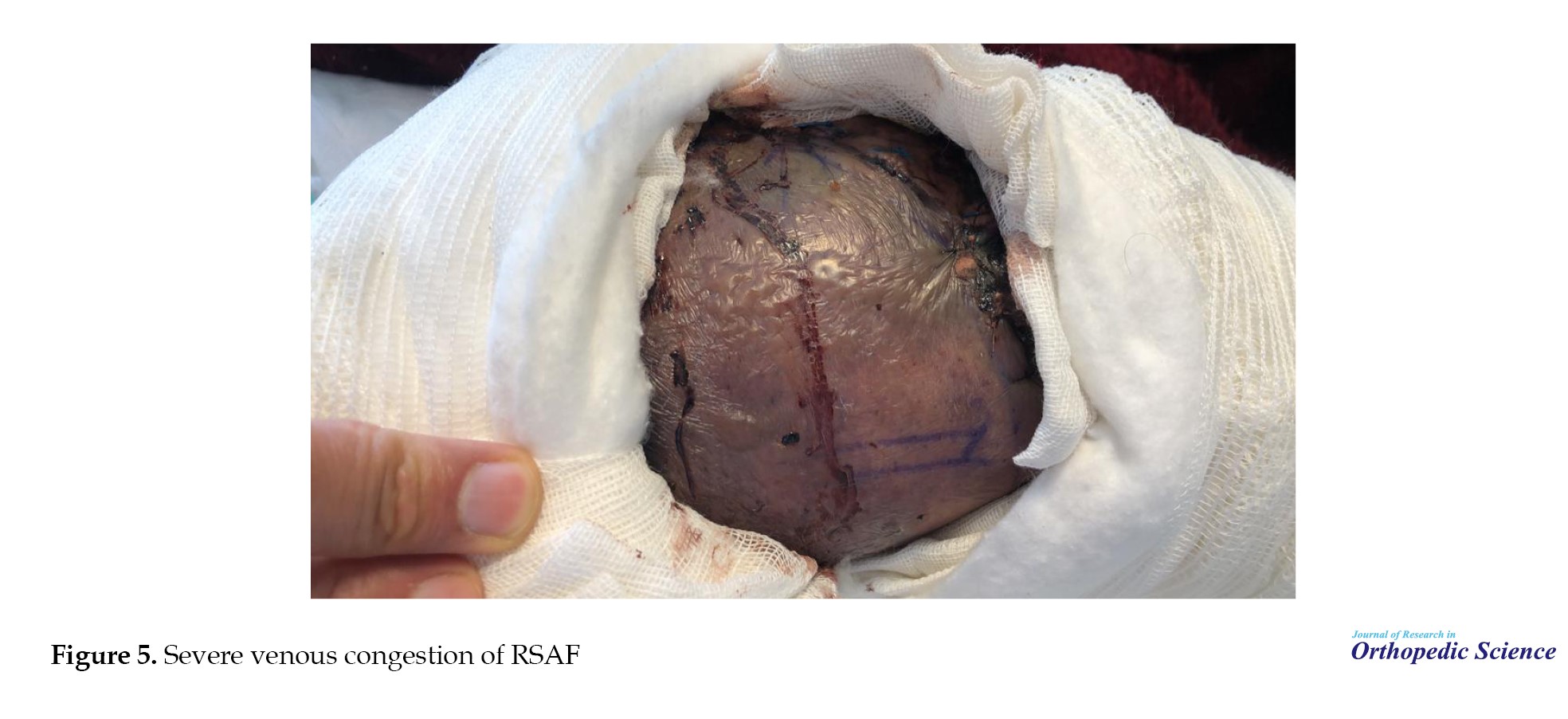
Reconstruction of the soft tissue defects around the ankle remains challenging because of the particular anatomy and the possibility of exposure to bone, tendon, or device [1, 2]. Reverse sural artery flap (RSAF) is commonly used to cover the soft tissue defects of the distal third of the leg, ankle, and foot, which has gained popularity among surgeons in recent years (Figure 1) [3, 4]. This flap is placed on the middle raphe between the medial and lateral heads of the gastrocnemius muscle proximally and posteriorly to the tip of the fibula distally (Figure 2). The types of RSAF include fasciocutaneous, adipofacial, and myocutaneous flaps [5]. The key benefit of this technique is that it is feasible in a minimal-resource center as it does not require microsurgical facilities (Figure 3). The complication rate of RSAF varies among studies and previously published research is limited regarding the rates of complications and associated risk factors. Similar to any other flap, venous congestion can be observed in the RSAF. This complication is highlighted in cases of RSAF, in which the flap’s pedicle is passed through the subcutaneous tissue. According to the GU classification, venous congestion can vary from absence of congestion to severe congestion (Figures 4, 5, and 6) [6]. Venous congestion should be diagnosed and treated promptly after surgery, otherwise, it can lead to flap failure [7].
This study aimed to evaluate different risk factors and their relationship with flap venous congestion as the most common complication of the RSAF reconstructive method.
Methods
We included patients with soft tissue defects of the distal tibial ankle or heel who were admitted to our department from 2019 to 2022 and underwent RSAF. Patients with inadequate follow-up and missing data or those who did not sign the informed consent upon admission were excluded from the study. The clinical records of these patients were reviewed to collect data needed to determine the incidence of venous congestion of the flap and its related factors.
One surgeon operated on all patients (Figures 7, 8 and 9). The formula proposed by Cochran was used to calculate the adequacy of the number of patients included. Patient demographic data, including age, sex, occupation, comorbidities, medications used, smoking status, drug use, and alcohol use, were reviewed and collected. In addition, the surface area of the flap, primary admission versus patients referred from remote hospitals, the time between soft tissue defect development and reconstructive surgery, hospitalization length, and incidence of flap venous congestion at the reconstructed site were recorded.
Data analysis was performed using SPSS software, version 26. Qualitative data were reported using frequency and percentage, and quantitative data using Mean±SD. To analyze the data, Spearman’s rho correlation coefficient and Mann-Whitney U test were used, and P<0.05 was determined as the significance level in statistical tests.
Results
A total of 39 patients were identified through a comprehensive investigation of the clinical records at our hospital, adhering to the specified inclusion and exclusion criteria. The etiology of soft tissue defects in these patients could be attributed to either primary open fracture or secondary open reduction and internal fixation of ankle fractures. Among these defects, the most prevalent locations were the distal tibia (69%), followed by the heel (17%) and the dorsal aspect of the foot (14%).
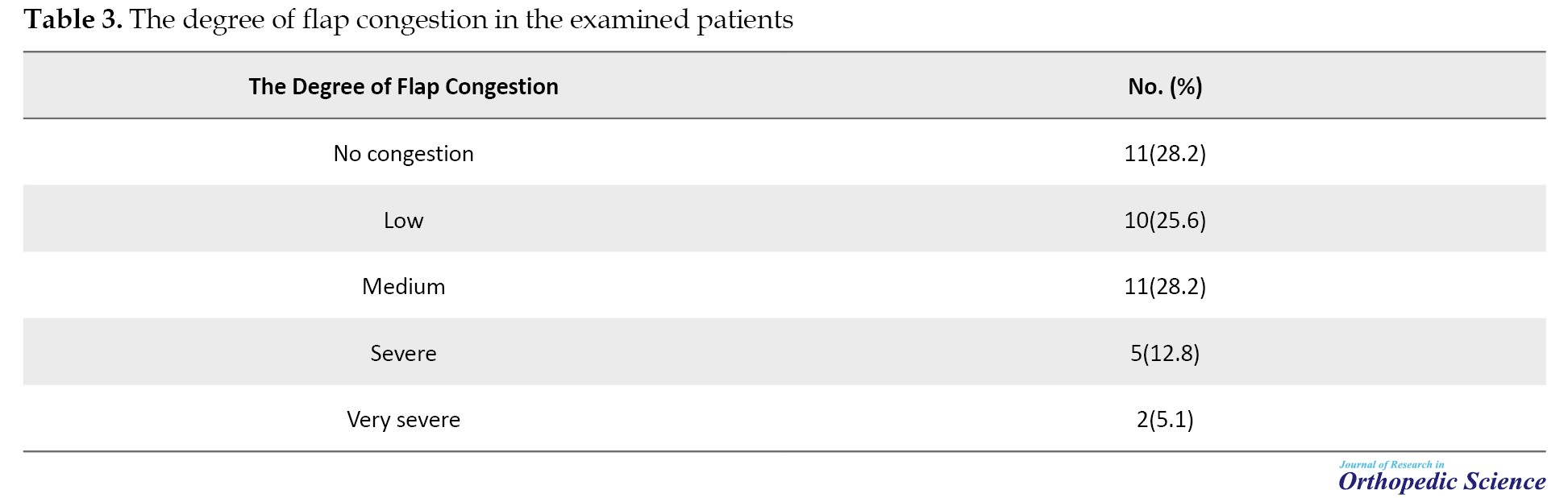
All collected variables were complete, without any missing data. The background characteristics of the patients are summarized in Table 1.
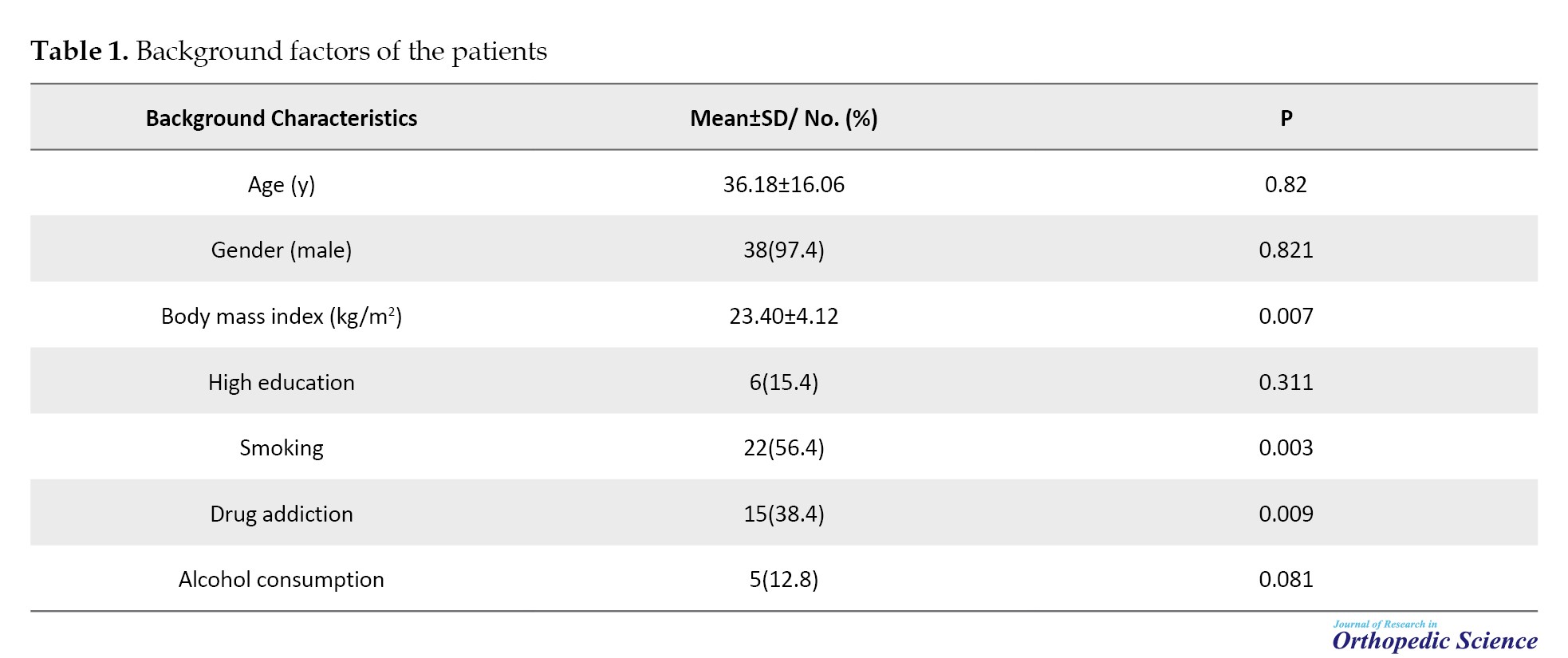
The mean age of the patients was 36.18±16.06 years, and the majority (97.4%) were male. The prevalence of smoking, drug addiction, and alcohol use among patients was 56.4%, 38.4%, and 12.8%, respectively. Interestingly, a substantial proportion of the patients (71.8%) were referred from a remote hospital.
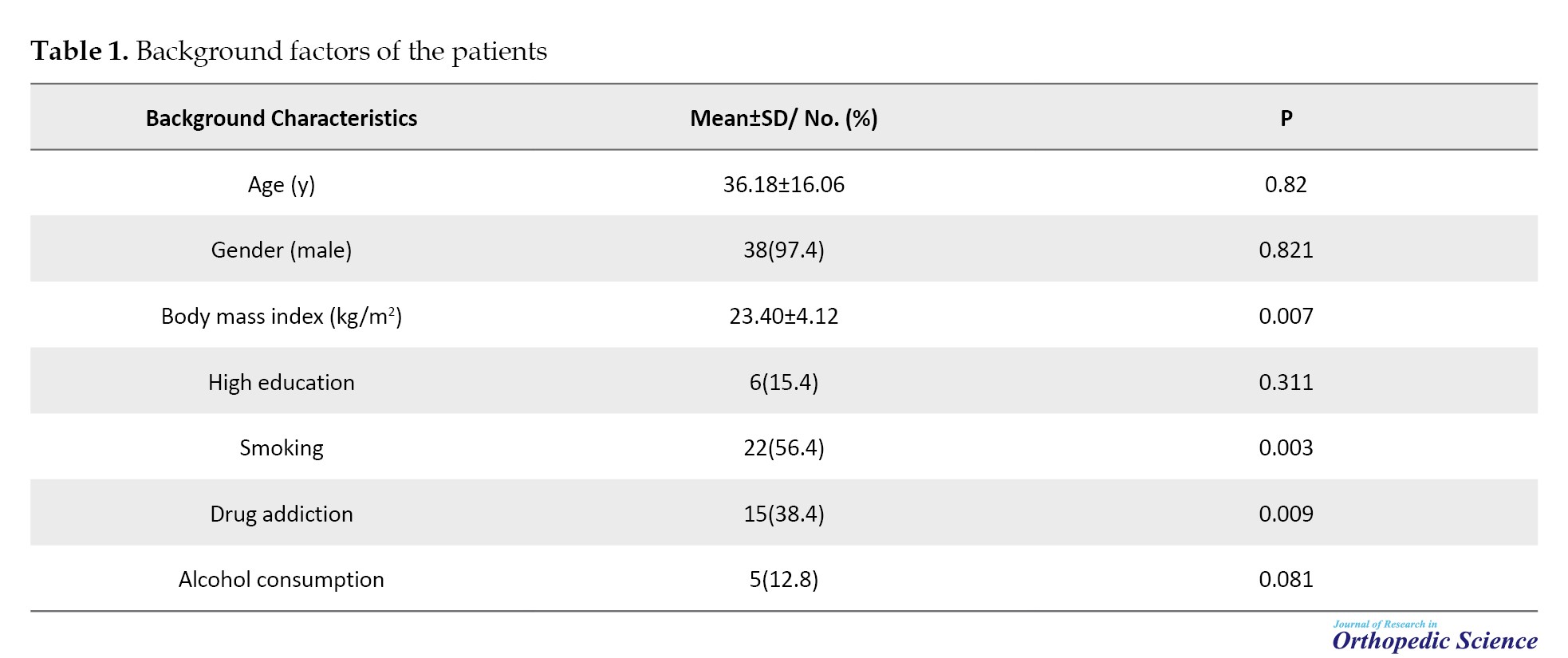
The characteristics of the soft tissue defects are listed in Table 2.
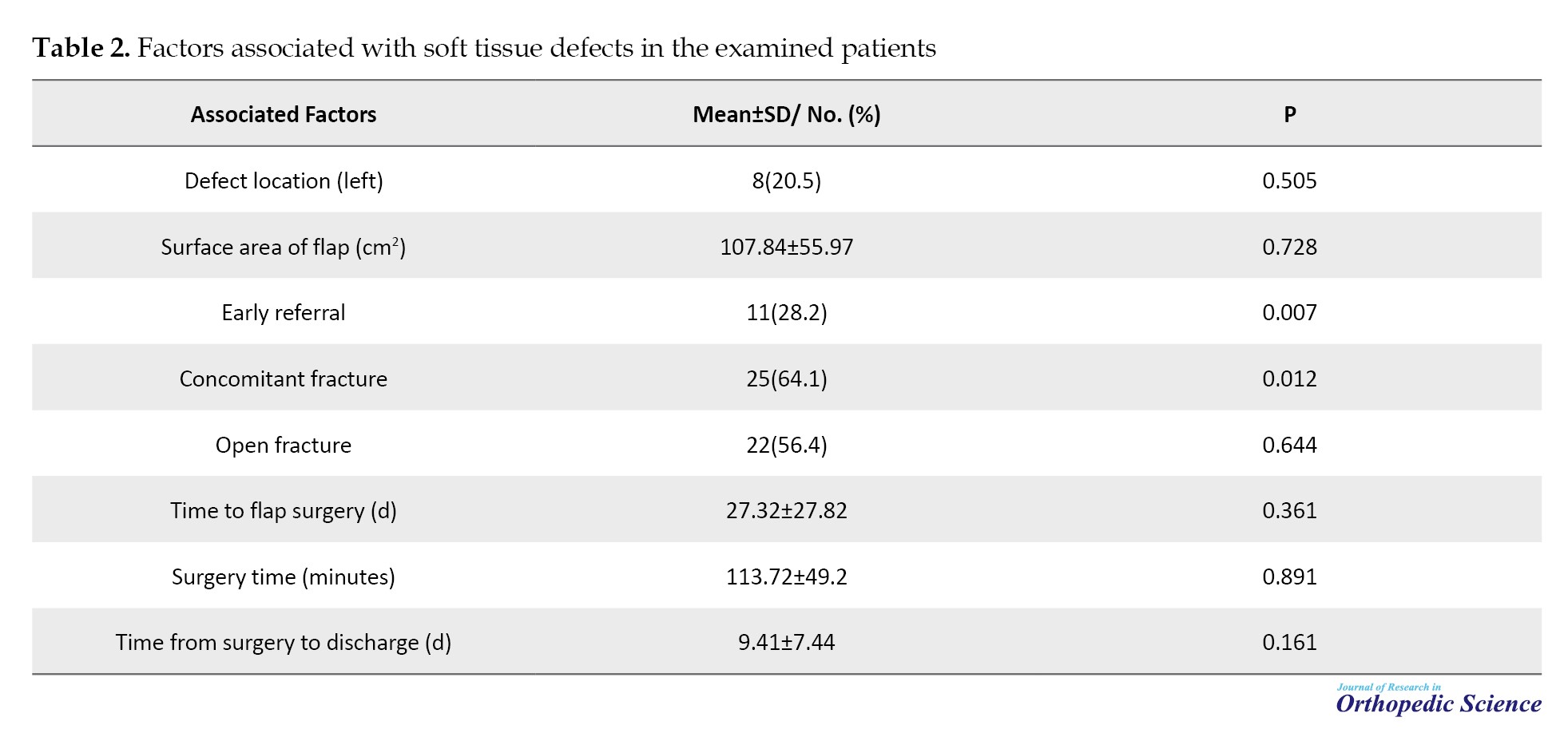
Specifically, the left side was affected in 20.50% of cases, and fractures were reported in 64.10% of patients, with open fractures documented in 56.4% of these cases. The mean surface area of the flap was 107.84±55.97 cm2. The average time interval between the occurrence of the defect and reconstructive surgery was 27.32±27.82 days. Following reconstructive surgery, patients had an average hospitalization duration of 7.44±9.41 days.
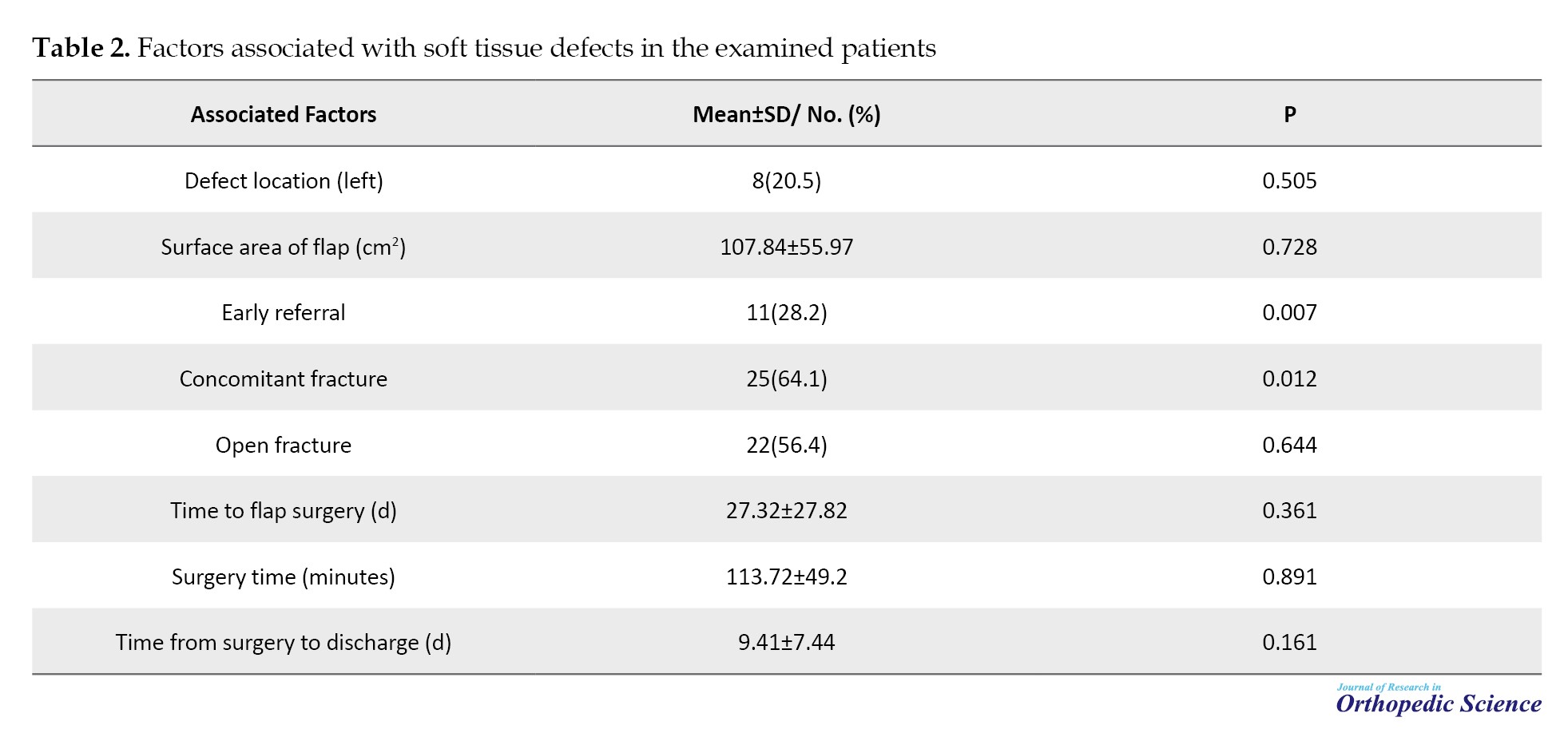
The degree of flap congestion after the reconstructive surgery in the evaluated patients is shown in Table 3.
Flap congestion was not observed in 11 patients (28.2%), whereas the remaining patients (n=28, 71.8%) experienced varying flap congestion.
Correlation analysis was conducted to investigate the potential relationships between background data and the incidence of flap congestion in patients. The results revealed significant positive correlations between smoking (P=0.003), drug addiction (P=0.009), late referral (P=0.007), concomitant fractures (P=0.012), and the occurrence of flap congestion. In contrast, no significant relationships were found between age, sex, level of education, time until surgery, surface area, surgery time, and the incidence of flap congestion after RSAF.
Discussion
Flap congestion after reverse sural flap surgery may occur early or late. Mechanical factors, such as hematoma formation and the compressive effect on the flap pedicle, are the main causes. Prompt diagnosis and intervention are critical. Techniques, such as leech therapy, venous supercharging, and revision surgeries can effectively address varying degrees of congestion [8, 9, 10]. Understanding the risk factors in RSAF can aid in the prevention of flap congestion leading to reducing flap failure [11]. Congestion of the flap in the absence of proper and timely treatment can cause partial or complete necrosis of the flap [12, 8]. The present study was conducted to investigate the incidence of venous congestion in RSAFs used to reconstruct soft tissue defects of the distal tibia, ankle, or heel and to determine the associated risk factors. The results showed that 71.8% of the evaluated patients developed flap venous congestion of various severities. In patients with low degrees of flap congestion, leech therapy was used; in more severe cases, skin grafting was performed after debridement, and in two cases with very severe flap congestion, free flaps were performed. By investigating the underlying factors and incidence of congestion in RSAF, it was found that smoking, drug addiction, late referral, and the simultaneous presence of fractures were associated with increased venous congestion. Different degrees of flap congestion may also be due to a combination of these four risk factors and the small sample size.
In this regard, several studies have been conducted to investigate the outcomes of RSAF in soft tissue reconstructive surgeries of the distal tibia, ankle, and heel. According to previous studies, the prevalence of venous congestion at the repair site reported in these investigations ranged from 3.05% to 75.3% [13-15]. Our study highlights the high prevalence of venous congestion in RSAF patients, with fractures emerging as a critical risk factor due to vascular compromise.
A systematic review study investigated the risk factors of necrosis incidence in RSAF [14]. In this study, smoking was the only suggested risk factor for partial necrosis of the RSAF. Due to the limitations of the reviewed articles regarding the venous congestion incidence determination, Daar et al. made no definitive statements and recommended that researchers in this field report and investigate the incidence of flap venous congestion in the patients treated with RSAF [14]. In this regard, the present study investigated and reported the incidence of venous congestion, its severity, and risk factors for venous congestion at the soft tissue repair site using RSAF. The findings of the present study indicated a significant incidence of venous congestion and determined smoking, drug addiction, late referral of patients, and the simultaneous presence of fractures. Thus, by controlling the suggested risk factors, that is, cessation of smoking, drug abuse, and early referral of patients with soft tissue defects in the distal lower limbs to a skilled surgeon in the field of reconstruction of soft tissue defects, the rate of flap congestion can be decreased, which could reduce the probability of treatment failure. It is also recommended to employ appropriate methods to reduce flap congestion, such as offloading with the Ilizarov technique, leech therapy, and heparin therapy. Furthermore, patients with these risk factors should be monitored at least every hour for 48 hours after surgery [8, 13, 16].
Optimizing flap design and preserving vascularity are essential for reducing congestion. Adjustments, such as a wider pedicle base and careful dissection to minimize compression, can improve outcomes [17, 18]. Subcutaneous tunneling techniques should also be evaluated for their impact on venous drainage [19]. While RSAF is effective, alternative methods, such as perforator flaps and free tissue transfer, offer additional options for specific cases. These approaches should be considered based on the patient’s condition and resource availability.
Conclusion
Flap congestion is common after an RSAF. By controlling the risk factors of this complication, such as smoking cessation and faster referral to a surgeon skilled in reconstructing soft tissue defects, flap congestion can be reduced, thus reducing the possibility of treatment failure.
The most important limitation of our study was its retrospective design, which made the data prone to publication bias. Another limitation of this study was the number of samples included, which provided results with an accuracy of 10%. The data analyzed in this study were collected from a single treatment center. In addition, sufficient data concerning the outcomes of reconstructive surgery in terms of the incidence of partial or complete necrosis were unavailable, which also limited the results of our study. Another limitation was the sex distribution of the patients, which mainly consisted of men, making the results of this study inapplicable to all patients undergoing reconstructive surgery of the soft tissue of the distal tibia. More research with larger sample sizes must be conducted, along with adjustments for risk factors that did not demonstrate significant effects in our study, such as sex and age.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Research Committee of the Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.MSP.REC.1401.543), and informed consent was obtained before the collection of data from participants.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
Reconstruction of the soft tissue defects around the ankle remains challenging because of the particular anatomy and the possibility of exposure to bone, tendon, or device [1, 2]. Reverse sural artery flap (RSAF) is commonly used to cover the soft tissue defects of the distal third of the leg, ankle, and foot, which has gained popularity among surgeons in recent years (Figure 1) [3, 4]. This flap is placed on the middle raphe between the medial and lateral heads of the gastrocnemius muscle proximally and posteriorly to the tip of the fibula distally (Figure 2). The types of RSAF include fasciocutaneous, adipofacial, and myocutaneous flaps [5]. The key benefit of this technique is that it is feasible in a minimal-resource center as it does not require microsurgical facilities (Figure 3). The complication rate of RSAF varies among studies and previously published research is limited regarding the rates of complications and associated risk factors. Similar to any other flap, venous congestion can be observed in the RSAF. This complication is highlighted in cases of RSAF, in which the flap’s pedicle is passed through the subcutaneous tissue. According to the GU classification, venous congestion can vary from absence of congestion to severe congestion (Figures 4, 5, and 6) [6]. Venous congestion should be diagnosed and treated promptly after surgery, otherwise, it can lead to flap failure [7].
This study aimed to evaluate different risk factors and their relationship with flap venous congestion as the most common complication of the RSAF reconstructive method.
Methods
We included patients with soft tissue defects of the distal tibial ankle or heel who were admitted to our department from 2019 to 2022 and underwent RSAF. Patients with inadequate follow-up and missing data or those who did not sign the informed consent upon admission were excluded from the study. The clinical records of these patients were reviewed to collect data needed to determine the incidence of venous congestion of the flap and its related factors.
One surgeon operated on all patients (Figures 7, 8 and 9). The formula proposed by Cochran was used to calculate the adequacy of the number of patients included. Patient demographic data, including age, sex, occupation, comorbidities, medications used, smoking status, drug use, and alcohol use, were reviewed and collected. In addition, the surface area of the flap, primary admission versus patients referred from remote hospitals, the time between soft tissue defect development and reconstructive surgery, hospitalization length, and incidence of flap venous congestion at the reconstructed site were recorded.
Data analysis was performed using SPSS software, version 26. Qualitative data were reported using frequency and percentage, and quantitative data using Mean±SD. To analyze the data, Spearman’s rho correlation coefficient and Mann-Whitney U test were used, and P<0.05 was determined as the significance level in statistical tests.
Results
A total of 39 patients were identified through a comprehensive investigation of the clinical records at our hospital, adhering to the specified inclusion and exclusion criteria. The etiology of soft tissue defects in these patients could be attributed to either primary open fracture or secondary open reduction and internal fixation of ankle fractures. Among these defects, the most prevalent locations were the distal tibia (69%), followed by the heel (17%) and the dorsal aspect of the foot (14%).
All collected variables were complete, without any missing data. The background characteristics of the patients are summarized in Table 1.
The mean age of the patients was 36.18±16.06 years, and the majority (97.4%) were male. The prevalence of smoking, drug addiction, and alcohol use among patients was 56.4%, 38.4%, and 12.8%, respectively. Interestingly, a substantial proportion of the patients (71.8%) were referred from a remote hospital.
The characteristics of the soft tissue defects are listed in Table 2.
Specifically, the left side was affected in 20.50% of cases, and fractures were reported in 64.10% of patients, with open fractures documented in 56.4% of these cases. The mean surface area of the flap was 107.84±55.97 cm2. The average time interval between the occurrence of the defect and reconstructive surgery was 27.32±27.82 days. Following reconstructive surgery, patients had an average hospitalization duration of 7.44±9.41 days.
The degree of flap congestion after the reconstructive surgery in the evaluated patients is shown in Table 3.
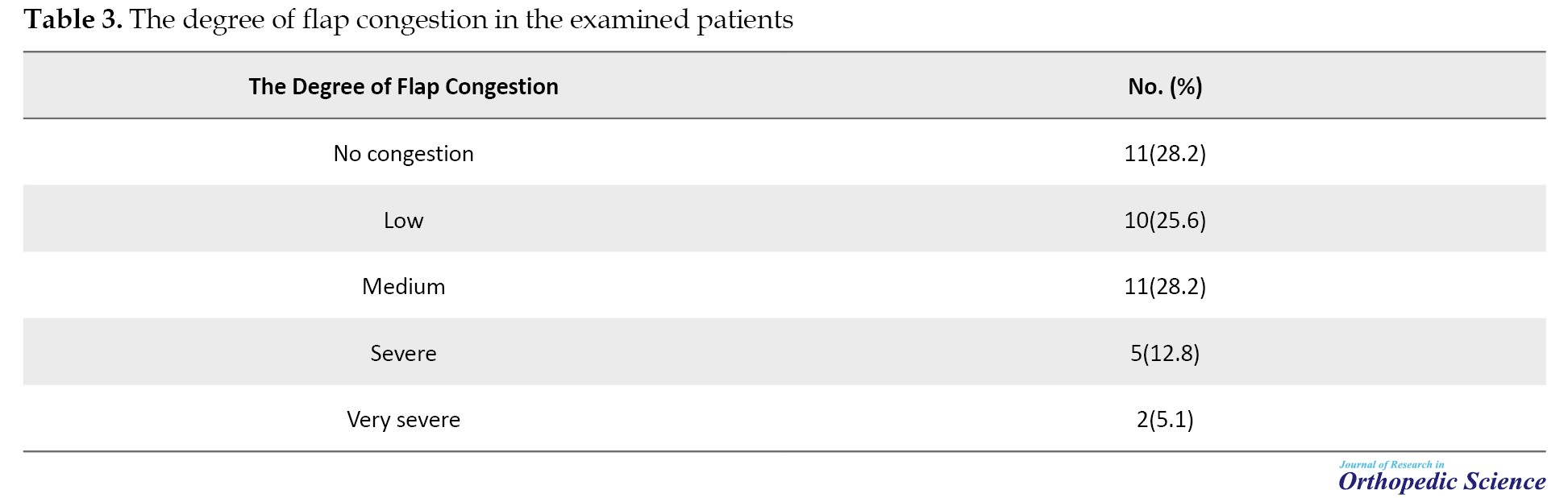
Flap congestion was not observed in 11 patients (28.2%), whereas the remaining patients (n=28, 71.8%) experienced varying flap congestion.
Correlation analysis was conducted to investigate the potential relationships between background data and the incidence of flap congestion in patients. The results revealed significant positive correlations between smoking (P=0.003), drug addiction (P=0.009), late referral (P=0.007), concomitant fractures (P=0.012), and the occurrence of flap congestion. In contrast, no significant relationships were found between age, sex, level of education, time until surgery, surface area, surgery time, and the incidence of flap congestion after RSAF.
Discussion
Flap congestion after reverse sural flap surgery may occur early or late. Mechanical factors, such as hematoma formation and the compressive effect on the flap pedicle, are the main causes. Prompt diagnosis and intervention are critical. Techniques, such as leech therapy, venous supercharging, and revision surgeries can effectively address varying degrees of congestion [8, 9, 10]. Understanding the risk factors in RSAF can aid in the prevention of flap congestion leading to reducing flap failure [11]. Congestion of the flap in the absence of proper and timely treatment can cause partial or complete necrosis of the flap [12, 8]. The present study was conducted to investigate the incidence of venous congestion in RSAFs used to reconstruct soft tissue defects of the distal tibia, ankle, or heel and to determine the associated risk factors. The results showed that 71.8% of the evaluated patients developed flap venous congestion of various severities. In patients with low degrees of flap congestion, leech therapy was used; in more severe cases, skin grafting was performed after debridement, and in two cases with very severe flap congestion, free flaps were performed. By investigating the underlying factors and incidence of congestion in RSAF, it was found that smoking, drug addiction, late referral, and the simultaneous presence of fractures were associated with increased venous congestion. Different degrees of flap congestion may also be due to a combination of these four risk factors and the small sample size.
In this regard, several studies have been conducted to investigate the outcomes of RSAF in soft tissue reconstructive surgeries of the distal tibia, ankle, and heel. According to previous studies, the prevalence of venous congestion at the repair site reported in these investigations ranged from 3.05% to 75.3% [13-15]. Our study highlights the high prevalence of venous congestion in RSAF patients, with fractures emerging as a critical risk factor due to vascular compromise.
A systematic review study investigated the risk factors of necrosis incidence in RSAF [14]. In this study, smoking was the only suggested risk factor for partial necrosis of the RSAF. Due to the limitations of the reviewed articles regarding the venous congestion incidence determination, Daar et al. made no definitive statements and recommended that researchers in this field report and investigate the incidence of flap venous congestion in the patients treated with RSAF [14]. In this regard, the present study investigated and reported the incidence of venous congestion, its severity, and risk factors for venous congestion at the soft tissue repair site using RSAF. The findings of the present study indicated a significant incidence of venous congestion and determined smoking, drug addiction, late referral of patients, and the simultaneous presence of fractures. Thus, by controlling the suggested risk factors, that is, cessation of smoking, drug abuse, and early referral of patients with soft tissue defects in the distal lower limbs to a skilled surgeon in the field of reconstruction of soft tissue defects, the rate of flap congestion can be decreased, which could reduce the probability of treatment failure. It is also recommended to employ appropriate methods to reduce flap congestion, such as offloading with the Ilizarov technique, leech therapy, and heparin therapy. Furthermore, patients with these risk factors should be monitored at least every hour for 48 hours after surgery [8, 13, 16].
Optimizing flap design and preserving vascularity are essential for reducing congestion. Adjustments, such as a wider pedicle base and careful dissection to minimize compression, can improve outcomes [17, 18]. Subcutaneous tunneling techniques should also be evaluated for their impact on venous drainage [19]. While RSAF is effective, alternative methods, such as perforator flaps and free tissue transfer, offer additional options for specific cases. These approaches should be considered based on the patient’s condition and resource availability.
Conclusion
Flap congestion is common after an RSAF. By controlling the risk factors of this complication, such as smoking cessation and faster referral to a surgeon skilled in reconstructing soft tissue defects, flap congestion can be reduced, thus reducing the possibility of treatment failure.
The most important limitation of our study was its retrospective design, which made the data prone to publication bias. Another limitation of this study was the number of samples included, which provided results with an accuracy of 10%. The data analyzed in this study were collected from a single treatment center. In addition, sufficient data concerning the outcomes of reconstructive surgery in terms of the incidence of partial or complete necrosis were unavailable, which also limited the results of our study. Another limitation was the sex distribution of the patients, which mainly consisted of men, making the results of this study inapplicable to all patients undergoing reconstructive surgery of the soft tissue of the distal tibia. More research with larger sample sizes must be conducted, along with adjustments for risk factors that did not demonstrate significant effects in our study, such as sex and age.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Research Committee of the Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: IR.SBMU.MSP.REC.1401.543), and informed consent was obtained before the collection of data from participants.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
- Chang SM, Li XH, Gu YD. Distally based perforator sural flaps for foot and ankle reconstruction. World J Orthop. 2015; 6(3):322-30. [DOI:10.5312/wjo.v6.i3.322] [PMID]
- Mohamed ME, Al Mobarak BA. Role of reversed sural artery flap in reconstruction of lower third of the leg, ankle and foot defects. Mod Plast Surg. 2018; 8(3):50-9. [DOI:10.4236/mps.2018.83007]
- Boopalan PR, Nithyananth M, Titus VT, Cherian VM, Jepegnanam TS. Experience of using local flaps to cover open lower limb injuries at an Indian trauma center. J Emerg Trauma Shock. 2011; 4(3):325-9. [DOI:10.4103/0974-2700.83806] [PMID]
- Sugg KB, Schaub TA, Concannon MJ, Cederna PS, Brown DL. The reverse superficial sural artery flap revisited for complex lower extremity and foot reconstruction. Plast Reconstr Surg Glob Open. 2015; 3(9):e519. [DOI:10.1097/GOX.0000000000000500] [PMID]
- Follmar KE, Baccarani A, Baumeister SP, Levin LS, Erdmann D. The distally based sural flap. Plast Reconstr Surg. 2007; 119(6):138e-48e. [DOI:10.1097/01.prs.0000259203.79909.7e] [PMID]
- Chang SM, Wang X, Huang YG, Zhu XZ, Tao YL, Zhang YQ. Distally based perforator propeller sural flap for foot and ankle reconstruction: A modified flap dissection technique. Ann Plast Surg. 2014; 72(3):340-5. [DOI:10.1097/SAP.0b013e31826108f1] [PMID]
- Baumeister SP, Spierer R, Erdmann D, Sweis R, Levin LS, Germann GK. A realistic complication analysis of 70 sural artery flaps in a multimorbid patient group. Plast Reconstr Surg. 2003; 112(1):129-40. [DOI:10.1097/01.PRS.0000066167.68966.66] [PMID]
- Boissiere F, Gandolfi S, Riot S, Kerfant N, Jenzeri A, Hendriks S, et al. Flap venous congestion and salvage techniques: a systematic literature review. Plast Reconstr Surg Glob Open. 2021; 9(1):e3327. [DOI:10.1097/GOX.0000000000003327] [PMID]
- Herlin C, Bertheuil N, Bekara F, Boissiere F, Sinna R, Chaput B. Leech therapy in flap salvage: Systematic review and practical recommendations. Ann Chir Plast Esthet. 2017; 62(2):e1-13. [DOI:10.1016/j.anplas.2016.06.004] [PMID]
- Herlin C, Bekara F, Bertheuil N, Carloni R, Dast S, Sinna R, et al. Venous supercharging reduces complications and improves outcomes of distally based sural flaps. J Reconstr Microsurg. 2017; 33(5):343-51. [DOI:10.1055/s-0037-1598620] [PMID]
- Blair JA, Puneky GA, Dickerson TE, Faith HD, Davis JM. Posttraumatic soft tissue coverage of the lower leg for the orthopedic surgeon. Orthop Clin North Am. 2022;5 3(3):297-310. [PMID]
- de Blacam C, Colakoglu S, Ogunleye AA, Nguyen JT, Ibrahim AM, Lin SJ, et al. Risk factors associated with complications in lower-extremity reconstruction with the distally based sural flap: A systematic review and pooled analysis. J Plast Reconstr Aesthet Surg. 2014; 67(5):607-16. [DOI:10.1016/j.bjps.2014.01.044] [PMID]
- Tripathee S, Basnet SJ, Lamichhane A, Hariani L. How safe is reverse sural flap? A systematic review. Eplasty. 2022; 22:e18. [PMID]
- Daar DA, Abdou SA, David JA, Kirby DJ, Wilson SC, Saadeh PB. Revisiting the reverse sural artery flap in distal lower extremity reconstruction: A systematic review and risk analysis. Ann Plast Surg. 2020; 84(4):463-470. [DOI:10.1097/SAP.0000000000002041] [PMID]
- Yammine K, Eric M, Nasser J, Chahine A. Effectiveness of the reverse sural flap in covering diabetic foot ulcers: A systematic review and meta-analysis. Plast Surg. 2022; 30(4):368-77. [DOI:10.1177/22925503211019617] [PMID]
- Jafari Kafiabadi M, Biglari F, Sadighi M, Sabaghzadeh A, Ebrahimpour A. Pilot study of additive effect of "offloading ilizarov frame" to reduce "reverse sural flap" surgery complications: A clinical trial. World J Plast Surg. 2022; 11(3):38-46. [DOI:10.52547/wjps.11.3.38] [PMID]
- Ehrenfeld M, Cornelius CP. Pedicled Flaps. In: Eufinger H, Kübler A, Schliephake H, editors. Oral and maxillofacial surgery: Surgical textbook and atlas. Berlin: Springer; 2023. [DOI:10.1007/978-3-662-66844-3_20]
- Herlin C, Sinna R, Hamoui M, Canovas F, Captier G, Chaput B. Distal lower extremity coverage by distally based sural flaps: Methods to increase their vascular reliability. Ann Chir Plast Esthet. 2017; 62(1):45-54. [DOI:10.1016/j.anplas.2015.11.002] [PMID]
- Anlatici R. Reverse sural flap for repair of foot and ankle defects: Our cases, modifications, and a literature review. Plastic Surgery Case Studies. 2020; 6:2513826X20947981. [DOI:10.1177/2513826X20947981]
Type of Study: Research Article |
Subject:
Trauma
Received: 2023/01/14 | Accepted: 2024/01/10 | Published: 2024/02/1
Received: 2023/01/14 | Accepted: 2024/01/10 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |