Volume 11, Issue 1 (2-2024)
JROS 2024, 11(1): 23-28 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aminian A, Aris A, Ettehad H, Goli N. A Promising New Approach to Managing Unstable Intertrochanteric Fractures During Hip Arthroplasty. JROS 2024; 11 (1) :23-28
URL: http://jros.iums.ac.ir/article-1-2273-en.html
URL: http://jros.iums.ac.ir/article-1-2273-en.html
1- Department of Orthopedic Surgery, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
3- Department of Orthopedics, Orthopedic Research Center, Faculty of Medicine, Poorsina Hospital, Guilan University of Medical Sciences, Rasht, Iran.
Keywords: Greater trochanter, Unstable intertrochanteric fractures, Hip arthroplasty, Fixation technique, Orthopedics, Surgery, Patient outcomes
Full-Text [PDF 531 kb]
(211 Downloads)
| Abstract (HTML) (908 Views)
Full-Text: (204 Views)
Introduction
Intertrochanteric fractures in elderly patients with osteoporosis are a significant orthopedic challenge. These fractures can weaken the hip’s structure, resulting in pain, limited mobility, and a lower quality of life. It is important to promptly and effectively address these fractures through surgical intervention to restore function and independence [1]. Treatment aims to improve mobility and prevent complications, such as muscle atrophy, pressure sores, and deep vein thrombosis. Intertrochanteric fractures can be challenging to treat due to the complex nature of the fractures and poor bone quality in elderly patients. Hip arthroplasty is a standard surgical procedure for unstable intertrochanteric fractures, but achieving stable fixation of the greater trochanter is crucial for the procedure’s success. Old fixation techniques often lead to complications, such as non-:union: or mal:union:, and prolonged rehabilitation [2-5]. Recent advancements in surgical techniques and implant design have resulted in the development of new methods to improve outcomes for patients with significant trochanter fractures. The new fixation method may offer better mechanical stability, thereby reducing the risk of displacement or failure of the greater trochanter fragment. Enhanced fixation techniques might promote more efficient bone healing, reducing recovery times for patients. Traditional methods can sometimes lead to complications, such as non-:union:, infection, or implant failure. The new technique could lower these risks, resulting in fewer post-operative complications. A more reliable fixation might result in improved mobility and function, allowing patients to regain strength and return to daily activities more quickly. If the new method is less invasive or requires fewer adjustments post-surgery, it could lead to shorter hospital stays and a more rapid rehabilitation process [6].
These methods aim to provide better stability and promote faster recovery, ultimately reducing the risk of complications. This study evaluated a new technique designed to improve strength and speed up recovery in patients with unstable intertrochanteric fractures undergoing hip arthroplasty. It compared the new fixation technique with traditional methods. The goal was to assess the advantages and potential of the new technique as a standard practice.
Methods
This study retrospectively analyzed patients who underwent hip arthroplasty with associated trochanteric fractures between 2019 and 2022. The study included patients who were 78 years old or younger and those who were 78 years old or older, all of whom had unstable intertrochanteric fractures.
These patients underwent hip arthroplasty using a new fixation technique. Patients with stable intertrochanteric fractures, a history of previous hip surgery on the injured side, or incomplete medical records were excluded from the study. Demographic data, details of the fracture, surgical procedure, and postoperative outcomes were gathered from the patient’s medical records.
The greater trochanter fragment was first reduced using a reduction clamp, followed by initial fixation with 4-5 Kirschner wires (K-wires) of 2 mm and 1.5 mm sizes, attached to the femoral shaft. A wire passer was then used to guide a wire around the femur and secure it on the lateral cortex. The K-wires were bent, and the wire was tightly wrapped and tied around them. If needed, a second wire was applied using the same method.
The Shapiro-Wilk test assessed the normality of the data distribution, while Levene’s test evaluated the homogeneity of variances for pain and mobility scores. Generalized estimation equations (GEE) were used to analyze repeated measures and correlated data points. The chi-square test was used when assumptions were met to examine the relationship between qualitative variables, and Fisher’s exact test was used when assumptions were not met. Statistical analysis was conducted using SPSS software, version 24.
Results
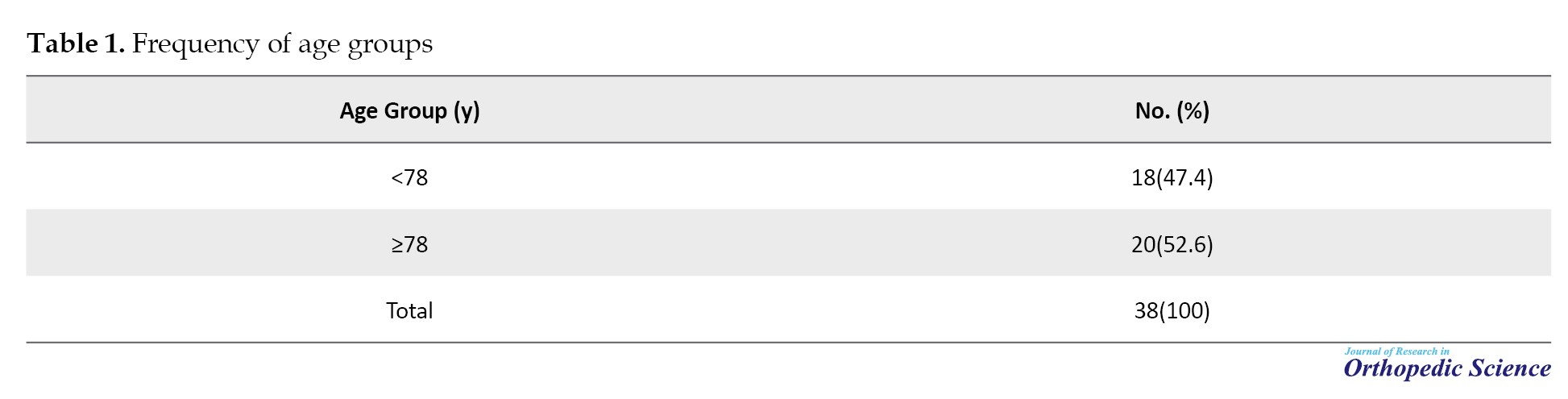
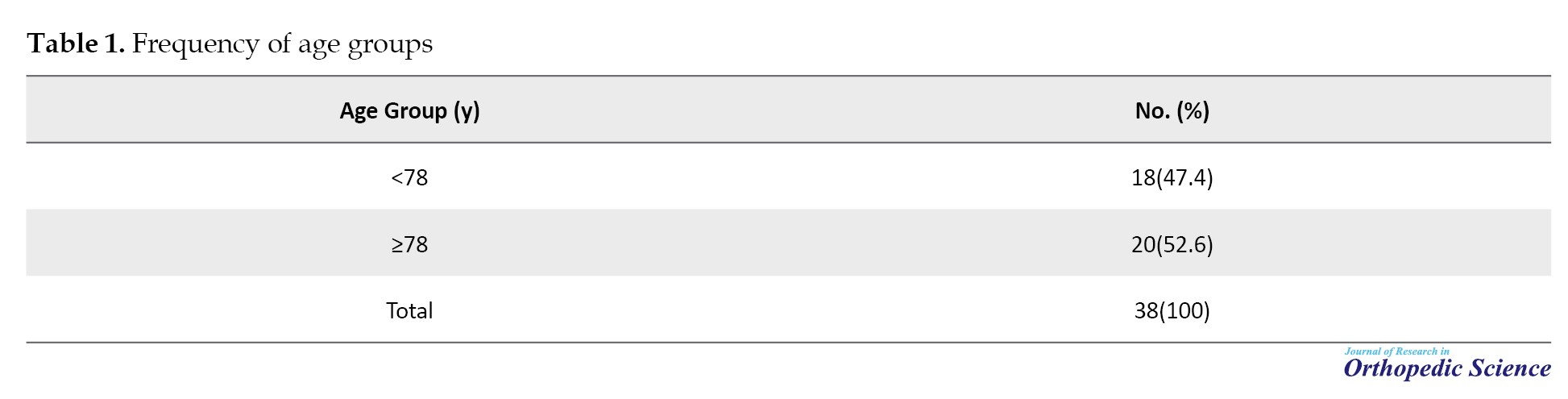
The study included a total of 38 patients with unstable intertrochanteric fractures who underwent hip arthroplasty using the new fixation technique. The frequency distribution of age groups among the subjects showed that 20 individuals (52.6%) were 78 years or older, while the remaining patients were younger than 78. The mean age of the subjects was 77.03±10.54 years, with the youngest being 57 and the oldest 95 years (Table 1).
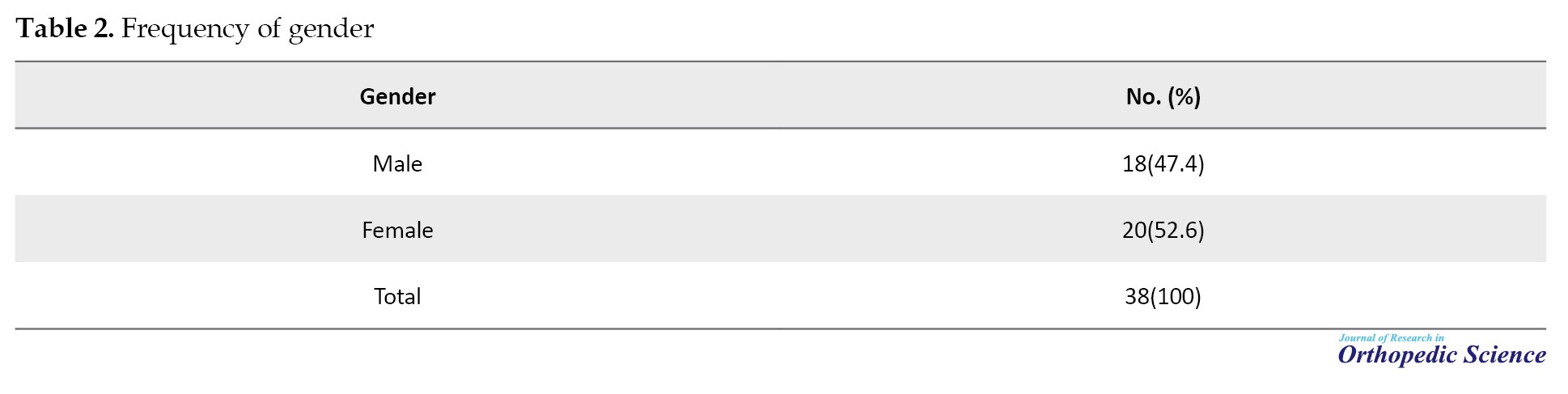
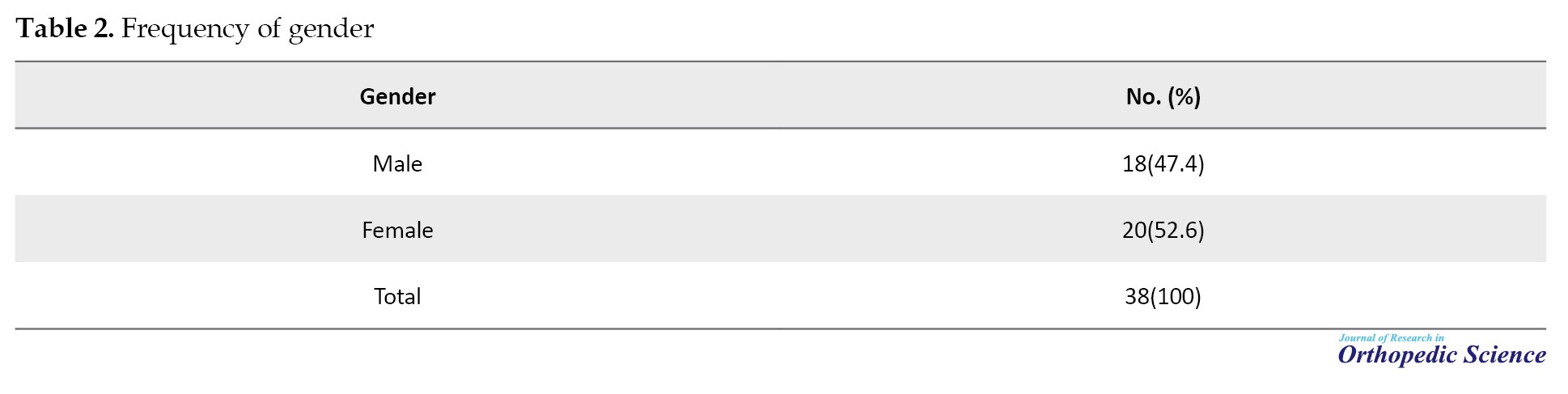
The frequency distribution of gender among the subjects indicated that 20 individuals (52.6%) were female, and the remaining 18 were male (47.4%) (Table 2).
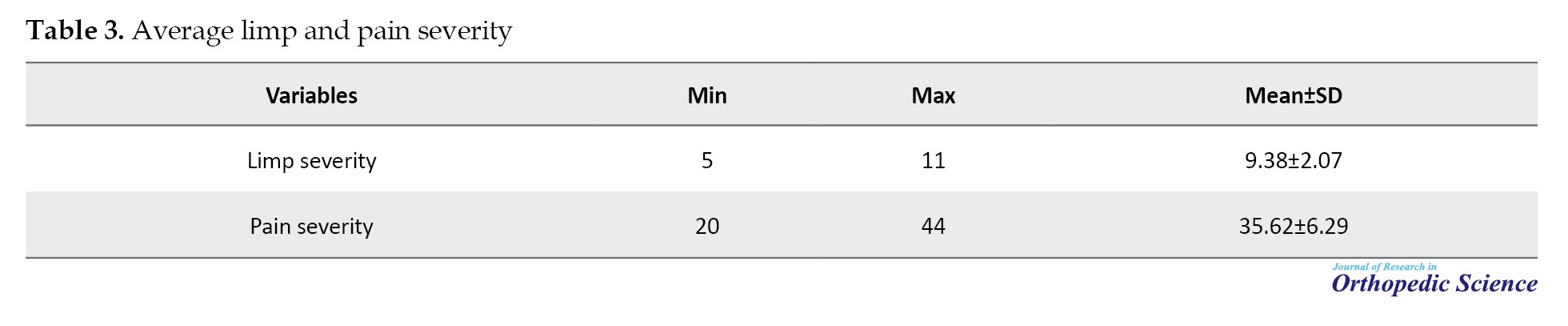
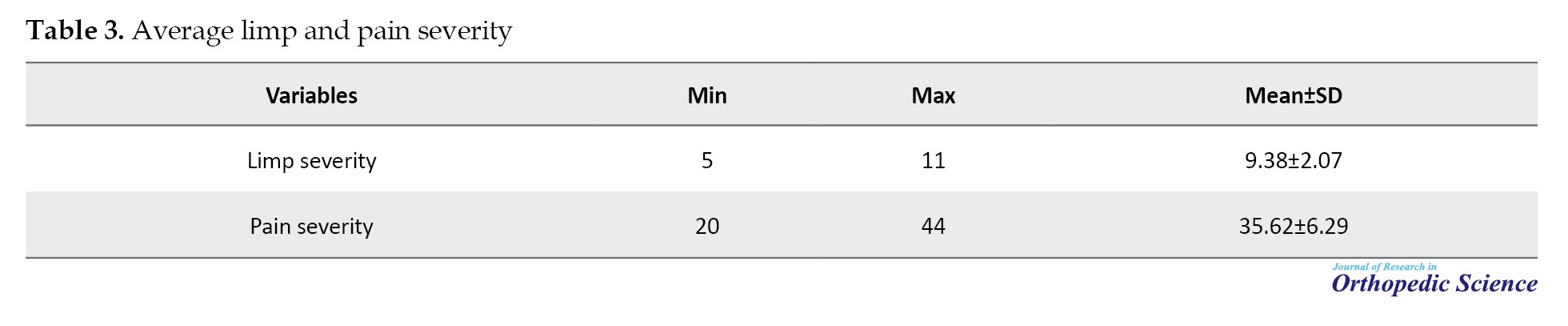
Average limp severity in patients undergoing total hip arthroplasty (THA) with simultaneous greater trochanter reconstruction using the new technique was assessed. The mean limp severity was 9.38±2.07, with the lowest and highest scores being 5 and 11, respectively. In addition, the average pain severity in the greater trochanter area was assessed post-surgery using the new technique. The mean pain severity was 35.62±6.29, with the lowest and highest scores being 20 and 44, respectively (Table 3).
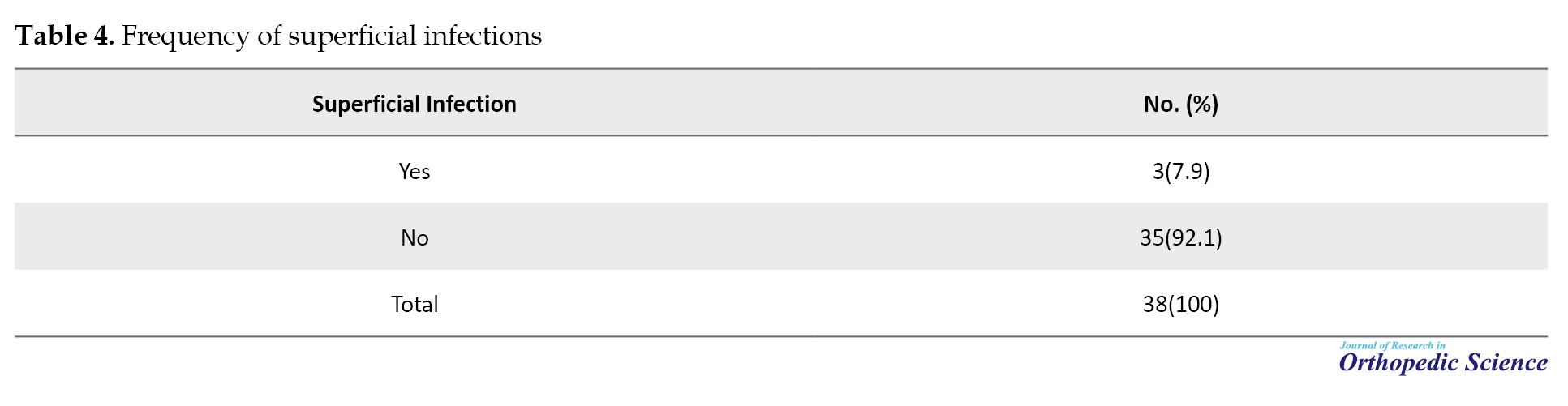
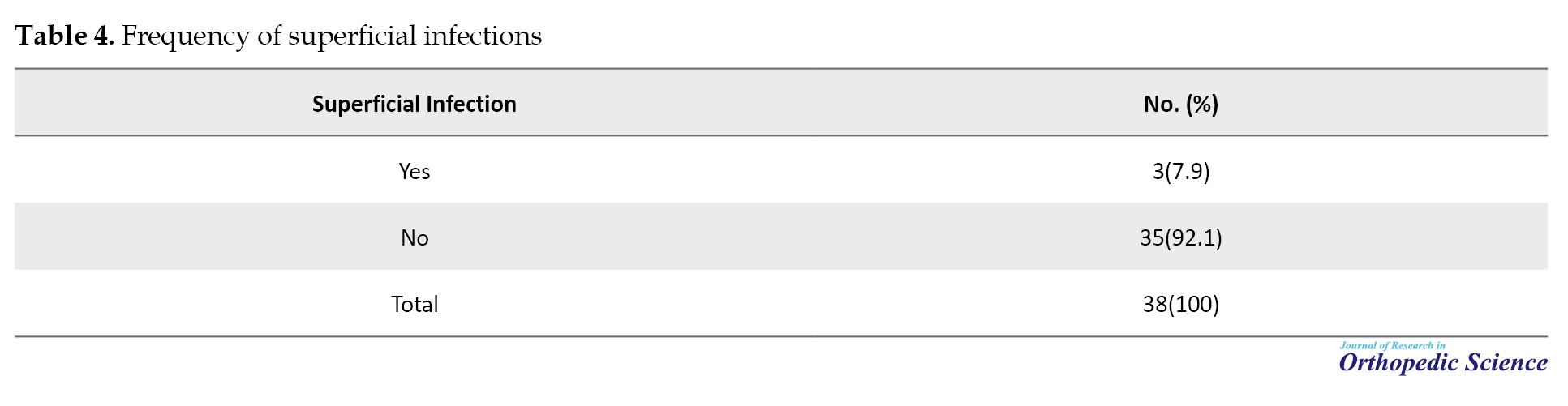
The frequency of superficial infections post-surgery using the new technique was assessed. The results showed that three individuals (7.9%) experienced superficial infections (Table 4).
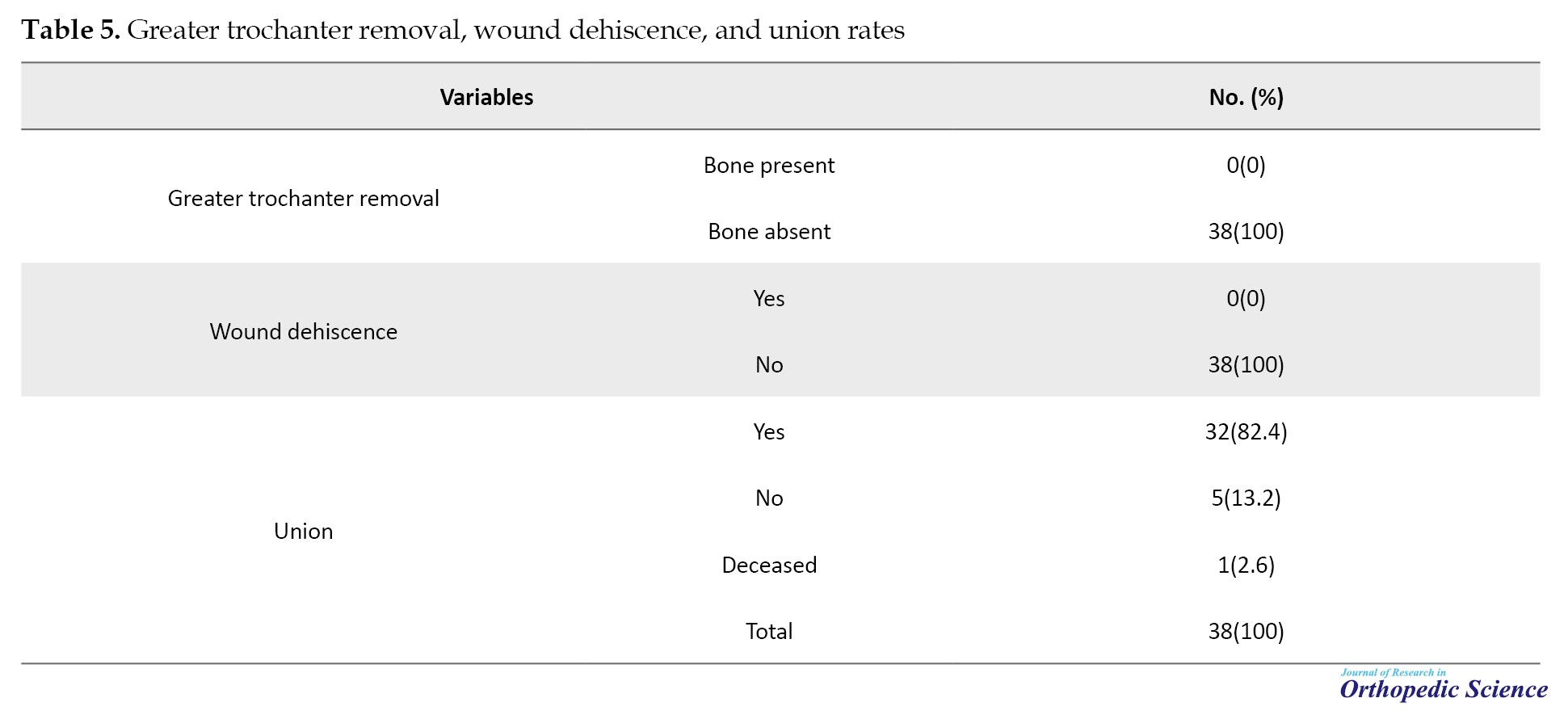
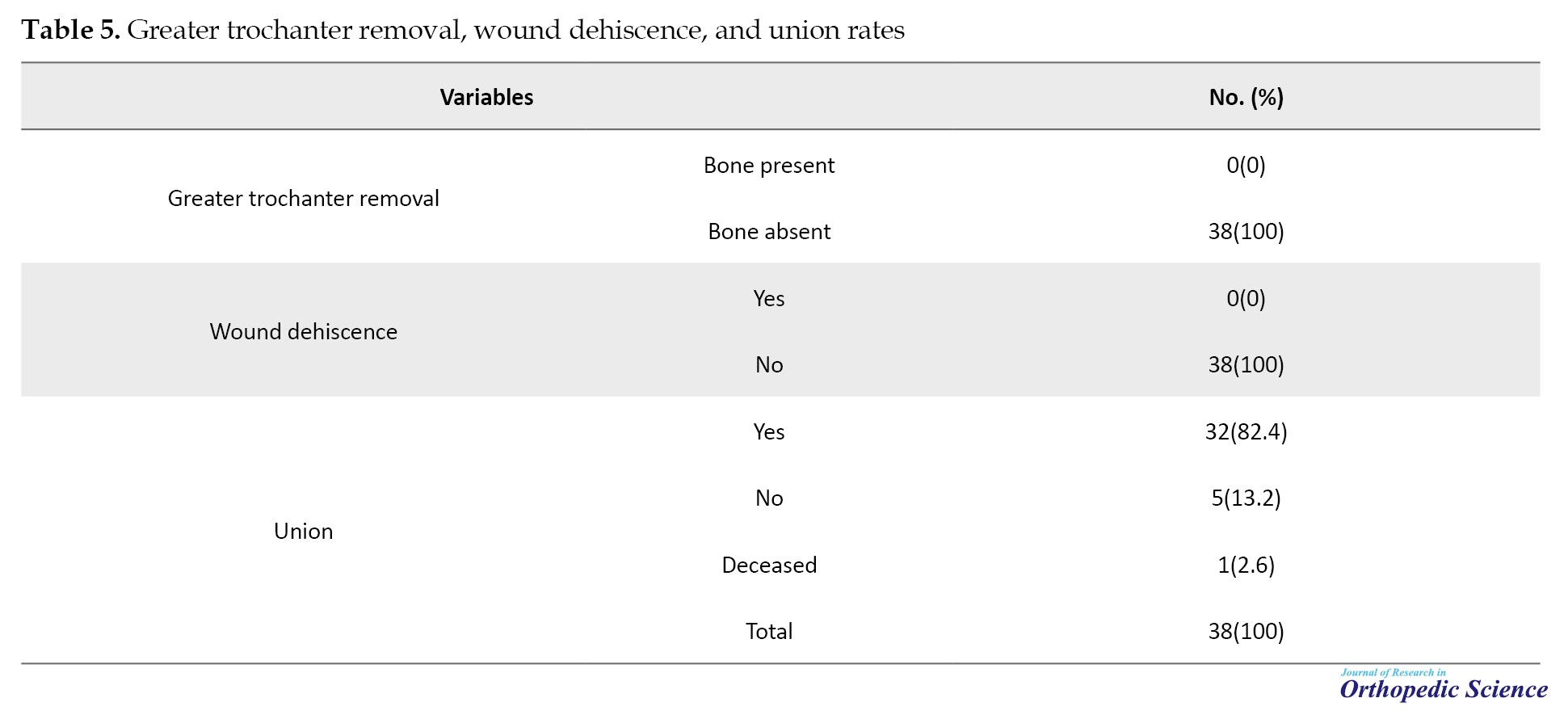
The frequency of greater trochanter removal using the new technique was also evaluated. According to the results, no bone presence was observed in any of the subjects, and the frequency of wound dehiscence was also observed using the new technique. The findings indicated that none of the subjects experienced wound dehiscence. Additionally, the frequency of complete :union: of the greater trochanter using the new reconstruction technique was assessed. The results revealed that 32 individuals (84.2%) achieved complete :union:. One individual (2.6%) passed away due to a cardiac condition within a month post-surgery (Table 5).
These results indicate that the novel fixation technique offers significant benefits over traditional methods regarding healing rates, pain reduction, functional recovery, and complication rates.
Discussion
The current study found no failures in the fixation and reconstruction of the greater trochanter post-surgery. The average age of the subjects was 77.03 years, highlighting the role of age in intertrochanteric fractures. Of the patients, 52.6% were female, which is consistent with global statistics on hip fractures. Post-surgery, patients exhibited low limp scores (9.38) and low pain severity. Only 7.9% of patients developed superficial infections after surgery, which is lower than the typical rate in THA.
In a related study by Hsu et al. on the role of lateral femoral wall thickness in intertrochanteric fractures, 208 patients with intertrochanteric fractures were examined, and their average age was reported to be 78 years [7]. Similarly, a study by Belmont et al. on the risk factors involved in hip fractures reported that 62% of the patients were female [8]. In contrast, a study by Mazure-Bonnefoy et al. on limp severity and patient satisfaction after primary THA showed that 30% of patients experienced limp severity ranging from mild to severe even five years post-arthroplasty. This confirms the high effectiveness of the new treatment studied in the present research [9].
In a study conducted by Reda and Sharaf, various postoperative complications following arthroplasty were examined. They found that the infection rates following simultaneous bilateral knee arthroplasty were relatively low but heterogeneous, as the data showed marked variability. Superficial infections were more common than deep infections; however, there was a small difference in their prevalence. Furthermore, the reliability of our findings was limited owing to significant heterogeneity [10].
D’Amore et al. conducted a study on the incidence of failure in fixation and the need for revision. Through the review and analysis of data from various articles, they reported a 14.8% incidence of failure after internal fixation and a 15.4% rate for the need for revision [11]. Our study results demonstrate the high quality and effectiveness of the new method of greater trochanter fixation, with zero occurrences of greater trochanter removal or revision surgery.
In the present study, wound dehiscence after surgery was not observed in any patients. Multiple studies indicate that the incidence of wound dehiscence after THA surgery ranges between 1 and 2% [12, 13, 14]. In our research, using the new fixation method, the incidence of wound dehiscence was zero, indicating the superiority of this method over conventional THA methods.
According to statistical analyses regarding the complete :union: rate of the greater trochanter in the present study, 82.4% of patients had a wholly healed greater trochanter, indicating a high fusion rate following the implementation of the new method.
We used the new technique for fixation of the greater trochanter in patients with intertrochanteric fractures and demonstrated that patients showed good recovery outcomes. Various factors examined in this study indicate the high effectiveness of this method. It was shown that patients experienced minimal limb shortening after surgery, and the incidence of superficial infection and the need to remove the greater trochanter were very low. Patients reported minimal pain after surgery, and wounds healed well without any observed wound dehiscence. However, this study is one of the few to precisely evaluate a novel fixation technique for significant trochanter fractures in an elderly population, providing valuable insights into its efficacy.
Clinical implications
The novel fixation technique appears to offer a superior alternative to traditional methods, particularly for elderly patients who are at higher risk of complications due to poor bone quality and comorbidities. Implementing this technique in clinical practice could lead to better patient outcomes, reduced healthcare costs, and improved quality of life for elderly patients undergoing hip arthroplasty.
Conclusion
A new fixation technique for significant trochanter fractures significantly improves outcomes for elderly hip arthroplasty patients. This advancement offers better stability, higher healing rates, reduced pain, and lower complication rates than traditional techniques. In conclusion, the novel fixation technique represents a promising innovation in orthopedic surgery for treating more significant trochanter fractures in elderly patients. Further research is needed to confirm these results and explore the long-term benefits and cost-effectiveness of this approach.
Ethical Considerations
Compliance with ethical guidelines
The study received approval from the Ethics Committees of the participating hospitals (Code: IR.GUMS.REC.1401.203), and all patients provided informed consent. Patient confidentiality was maintained. The research followed ethical guidelines and aimed to thoroughly evaluate the new fixation technique for unstable intertrochanteric fractures in hip arthroplasty patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology and project administration: Arash Arish; Resources and validation: Hossein Ettehad; Data curation: Nasibeh Goli; Writing the original draft: Amir Aminian and Nasibeh Goli; Supervision, review and editing: Amir Aminian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to show our gratitude to Razi Clinical Research Development Unit that greatly assisted us in publishing the research.
References
Intertrochanteric fractures in elderly patients with osteoporosis are a significant orthopedic challenge. These fractures can weaken the hip’s structure, resulting in pain, limited mobility, and a lower quality of life. It is important to promptly and effectively address these fractures through surgical intervention to restore function and independence [1]. Treatment aims to improve mobility and prevent complications, such as muscle atrophy, pressure sores, and deep vein thrombosis. Intertrochanteric fractures can be challenging to treat due to the complex nature of the fractures and poor bone quality in elderly patients. Hip arthroplasty is a standard surgical procedure for unstable intertrochanteric fractures, but achieving stable fixation of the greater trochanter is crucial for the procedure’s success. Old fixation techniques often lead to complications, such as non-:union: or mal:union:, and prolonged rehabilitation [2-5]. Recent advancements in surgical techniques and implant design have resulted in the development of new methods to improve outcomes for patients with significant trochanter fractures. The new fixation method may offer better mechanical stability, thereby reducing the risk of displacement or failure of the greater trochanter fragment. Enhanced fixation techniques might promote more efficient bone healing, reducing recovery times for patients. Traditional methods can sometimes lead to complications, such as non-:union:, infection, or implant failure. The new technique could lower these risks, resulting in fewer post-operative complications. A more reliable fixation might result in improved mobility and function, allowing patients to regain strength and return to daily activities more quickly. If the new method is less invasive or requires fewer adjustments post-surgery, it could lead to shorter hospital stays and a more rapid rehabilitation process [6].
These methods aim to provide better stability and promote faster recovery, ultimately reducing the risk of complications. This study evaluated a new technique designed to improve strength and speed up recovery in patients with unstable intertrochanteric fractures undergoing hip arthroplasty. It compared the new fixation technique with traditional methods. The goal was to assess the advantages and potential of the new technique as a standard practice.
Methods
This study retrospectively analyzed patients who underwent hip arthroplasty with associated trochanteric fractures between 2019 and 2022. The study included patients who were 78 years old or younger and those who were 78 years old or older, all of whom had unstable intertrochanteric fractures.
These patients underwent hip arthroplasty using a new fixation technique. Patients with stable intertrochanteric fractures, a history of previous hip surgery on the injured side, or incomplete medical records were excluded from the study. Demographic data, details of the fracture, surgical procedure, and postoperative outcomes were gathered from the patient’s medical records.
The greater trochanter fragment was first reduced using a reduction clamp, followed by initial fixation with 4-5 Kirschner wires (K-wires) of 2 mm and 1.5 mm sizes, attached to the femoral shaft. A wire passer was then used to guide a wire around the femur and secure it on the lateral cortex. The K-wires were bent, and the wire was tightly wrapped and tied around them. If needed, a second wire was applied using the same method.
The Shapiro-Wilk test assessed the normality of the data distribution, while Levene’s test evaluated the homogeneity of variances for pain and mobility scores. Generalized estimation equations (GEE) were used to analyze repeated measures and correlated data points. The chi-square test was used when assumptions were met to examine the relationship between qualitative variables, and Fisher’s exact test was used when assumptions were not met. Statistical analysis was conducted using SPSS software, version 24.
Results
The study included a total of 38 patients with unstable intertrochanteric fractures who underwent hip arthroplasty using the new fixation technique. The frequency distribution of age groups among the subjects showed that 20 individuals (52.6%) were 78 years or older, while the remaining patients were younger than 78. The mean age of the subjects was 77.03±10.54 years, with the youngest being 57 and the oldest 95 years (Table 1).
The frequency distribution of gender among the subjects indicated that 20 individuals (52.6%) were female, and the remaining 18 were male (47.4%) (Table 2).
Average limp severity in patients undergoing total hip arthroplasty (THA) with simultaneous greater trochanter reconstruction using the new technique was assessed. The mean limp severity was 9.38±2.07, with the lowest and highest scores being 5 and 11, respectively. In addition, the average pain severity in the greater trochanter area was assessed post-surgery using the new technique. The mean pain severity was 35.62±6.29, with the lowest and highest scores being 20 and 44, respectively (Table 3).
The frequency of superficial infections post-surgery using the new technique was assessed. The results showed that three individuals (7.9%) experienced superficial infections (Table 4).
The frequency of greater trochanter removal using the new technique was also evaluated. According to the results, no bone presence was observed in any of the subjects, and the frequency of wound dehiscence was also observed using the new technique. The findings indicated that none of the subjects experienced wound dehiscence. Additionally, the frequency of complete :union: of the greater trochanter using the new reconstruction technique was assessed. The results revealed that 32 individuals (84.2%) achieved complete :union:. One individual (2.6%) passed away due to a cardiac condition within a month post-surgery (Table 5).
These results indicate that the novel fixation technique offers significant benefits over traditional methods regarding healing rates, pain reduction, functional recovery, and complication rates.
Discussion
The current study found no failures in the fixation and reconstruction of the greater trochanter post-surgery. The average age of the subjects was 77.03 years, highlighting the role of age in intertrochanteric fractures. Of the patients, 52.6% were female, which is consistent with global statistics on hip fractures. Post-surgery, patients exhibited low limp scores (9.38) and low pain severity. Only 7.9% of patients developed superficial infections after surgery, which is lower than the typical rate in THA.
In a related study by Hsu et al. on the role of lateral femoral wall thickness in intertrochanteric fractures, 208 patients with intertrochanteric fractures were examined, and their average age was reported to be 78 years [7]. Similarly, a study by Belmont et al. on the risk factors involved in hip fractures reported that 62% of the patients were female [8]. In contrast, a study by Mazure-Bonnefoy et al. on limp severity and patient satisfaction after primary THA showed that 30% of patients experienced limp severity ranging from mild to severe even five years post-arthroplasty. This confirms the high effectiveness of the new treatment studied in the present research [9].
In a study conducted by Reda and Sharaf, various postoperative complications following arthroplasty were examined. They found that the infection rates following simultaneous bilateral knee arthroplasty were relatively low but heterogeneous, as the data showed marked variability. Superficial infections were more common than deep infections; however, there was a small difference in their prevalence. Furthermore, the reliability of our findings was limited owing to significant heterogeneity [10].
D’Amore et al. conducted a study on the incidence of failure in fixation and the need for revision. Through the review and analysis of data from various articles, they reported a 14.8% incidence of failure after internal fixation and a 15.4% rate for the need for revision [11]. Our study results demonstrate the high quality and effectiveness of the new method of greater trochanter fixation, with zero occurrences of greater trochanter removal or revision surgery.
In the present study, wound dehiscence after surgery was not observed in any patients. Multiple studies indicate that the incidence of wound dehiscence after THA surgery ranges between 1 and 2% [12, 13, 14]. In our research, using the new fixation method, the incidence of wound dehiscence was zero, indicating the superiority of this method over conventional THA methods.
According to statistical analyses regarding the complete :union: rate of the greater trochanter in the present study, 82.4% of patients had a wholly healed greater trochanter, indicating a high fusion rate following the implementation of the new method.
We used the new technique for fixation of the greater trochanter in patients with intertrochanteric fractures and demonstrated that patients showed good recovery outcomes. Various factors examined in this study indicate the high effectiveness of this method. It was shown that patients experienced minimal limb shortening after surgery, and the incidence of superficial infection and the need to remove the greater trochanter were very low. Patients reported minimal pain after surgery, and wounds healed well without any observed wound dehiscence. However, this study is one of the few to precisely evaluate a novel fixation technique for significant trochanter fractures in an elderly population, providing valuable insights into its efficacy.
Clinical implications
The novel fixation technique appears to offer a superior alternative to traditional methods, particularly for elderly patients who are at higher risk of complications due to poor bone quality and comorbidities. Implementing this technique in clinical practice could lead to better patient outcomes, reduced healthcare costs, and improved quality of life for elderly patients undergoing hip arthroplasty.
Conclusion
A new fixation technique for significant trochanter fractures significantly improves outcomes for elderly hip arthroplasty patients. This advancement offers better stability, higher healing rates, reduced pain, and lower complication rates than traditional techniques. In conclusion, the novel fixation technique represents a promising innovation in orthopedic surgery for treating more significant trochanter fractures in elderly patients. Further research is needed to confirm these results and explore the long-term benefits and cost-effectiveness of this approach.
Ethical Considerations
Compliance with ethical guidelines
The study received approval from the Ethics Committees of the participating hospitals (Code: IR.GUMS.REC.1401.203), and all patients provided informed consent. Patient confidentiality was maintained. The research followed ethical guidelines and aimed to thoroughly evaluate the new fixation technique for unstable intertrochanteric fractures in hip arthroplasty patients.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Methodology and project administration: Arash Arish; Resources and validation: Hossein Ettehad; Data curation: Nasibeh Goli; Writing the original draft: Amir Aminian and Nasibeh Goli; Supervision, review and editing: Amir Aminian.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to show our gratitude to Razi Clinical Research Development Unit that greatly assisted us in publishing the research.
References
- Jegathesan T, Kwek EBK. Are intertrochanteric fractures evolving? Trends in the elderly population over a 10-year period. Clin Orthop Surg. 2022; 14(1):13-20. [DOI:10.4055/cios20204] [PMID]
- Chang SM, Hou ZY, Hu SJ, Du SC. Intertrochanteric femur fracture treatment in Asia: What we know and what the world can learn. Orthop Clin North Am. 2020; 51(2):189-205. [DOI:10.1016/j.ocl.2019.11.011] [PMID]
- Huang G, Zhang M, Qu Z, Zhang Y, Wang X, Kang W, et al. Fixation options for reconstruction of the greater trochanter in unstable intertrochanteric fracture with arthroplasty. Medicine. 2021; 100(26):e26395. [DOI:10.1097/MD.0000000000026395] [PMID]
- Ekegren CL, Edwards ER, de Steiger R, Gabbe BJ. Incidence, costs and predictors of non-:union:, delayed :union: and mal-:union: following long bone fracture. Int J Environ Res Public Health. 2018; 15(12):2845. [DOI:10.3390/ijerph15122845] [PMID]
- Nicholson JA, Makaram N, Simpson A, Keating JF. Fracture non:union: in long bones: A literature review of risk factors and surgical management. Injury. 2021; 52(Suppl 2):S3-11. [DOI:10.1016/j.injury.2020.11.029] [PMID]
- Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018; 19(1):369. [DOI:10.1186/s12891-018-2276-3] [PMID]
- Hsu CE, Shih CM, Wang CC, Huang KC. Lateral femoral wall thickness. A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. Bone Joint J. 2013; 95-B(8):1134-8. [DOI:10.1302/0301-620X.95B8.31495] [PMID]
- Belmont PJ Jr, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ. Risk factors for complications and in-hospital mortality following hip fractures: A study using the national trauma data bank. Arch Orthop Trauma Surg. 2014; 134(5):597-604. [DOI:10.1007/s00402-014-1959-y] [PMID]
- Bonnefoy-Mazure A, Poncet A, Gonzalez A, Barea C, Hannouche D, Lübbeke A. Limping and patient satisfaction after primary total hip arthroplasty: A registry-based cohort study. Acta Orthop. 2022; 93:602-8. [DOI:10.2340/17453674.2022.3489] [PMID]
- Reda B, Sharaf R. Incidence of postoperative infection following simultaneous bilateral knee arthroplasty: A systematic review and meta-analysis. Cureus. 2024; 16(2):e54117. [DOI:10.7759/cureus.54117]
- D'Amore T, Chisari E, Scaramella A, Frenz B, Courtney PM. Intraoperative greater trochanteric fractures during revision total hip arthroplasty may not always need surgical fixation. Orthopedics. 2023; 46(5):297-302. [DOI:10.3928/01477447-20230310-02] [PMID]
- Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014; 29(9):1839-41. [DOI:10.1016/j.arth.2014.04.036] [PMID]
- Purcell RL, Parks NL, Gargiulo JM, Hamilton WG. Severely obese patients have a higher risk of infection after direct anterior approach total hip arthroplasty. J Arthroplasty. 2016; 31(9 Suppl):162-5. [DOI:10.1016/j.arth.2016.03.037] [PMID]
- Watts CD, Houdek MT, Wagner ER, Sculco PK, Chalmers BP, Taunton MJ. High risk of wound complications following direct anterior total hip arthroplasty in obese patients. J Arthroplasty. 2015; 30(12):2296-8. [DOI:10.1016/j.arth.2015.06.016] [PMID]
Type of Study: Research Article |
Subject:
Hip surgery
Received: 2023/01/2 | Accepted: 2023/01/29 | Published: 2024/02/1
Received: 2023/01/2 | Accepted: 2023/01/29 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |