Volume 11, Issue 1 (2-2024)
JROS 2024, 11(1): 29-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shariaatzade H, Bahaeddini M R, Jafari Kafiabadi M, Saffarpour S, Fallahi H, Pahlevan Sabagh A. Short-term Outcomes of Closed Reduction and Percutaneous Pinning in Elderly Patients With Distal Radius Fractures. JROS 2024; 11 (1) :29-42
URL: http://jros.iums.ac.ir/article-1-2274-en.html
URL: http://jros.iums.ac.ir/article-1-2274-en.html
Hooman Shariaatzade1 

 , Mohammad Reza Bahaeddini1
, Mohammad Reza Bahaeddini1 

 , Meisam Jafari Kafiabadi1
, Meisam Jafari Kafiabadi1 

 , Sepideh Saffarpour1
, Sepideh Saffarpour1 

 , Hiva Fallahi1
, Hiva Fallahi1 

 , Alireza Pahlevan Sabagh1
, Alireza Pahlevan Sabagh1 




 , Mohammad Reza Bahaeddini1
, Mohammad Reza Bahaeddini1 

 , Meisam Jafari Kafiabadi1
, Meisam Jafari Kafiabadi1 

 , Sepideh Saffarpour1
, Sepideh Saffarpour1 

 , Hiva Fallahi1
, Hiva Fallahi1 

 , Alireza Pahlevan Sabagh1
, Alireza Pahlevan Sabagh1 


1- Bone and Joint Reconstruction Research Center, School of Medicine, Shafayahyaeian Hospital, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 996 kb]
(201 Downloads)
| Abstract (HTML) (857 Views)
Full-Text: (255 Views)
Introduction
Distal radius fractures are common, accounting for about 16% of all fractures in emergency departments and 20% of accident-related fractures. They predominantly affect elderly women due to osteoporosis and adult men through high-impact activities. Other important risk factors for distal radius fractures in patients older than 50 years include falls, a history of previous fractures, the use of corticosteroids, and advanced age. Dementia is also a risk factor in patients older than 75 years. In older patients, any additional risk factor increases the likelihood of a distal radius fracture. Fractures of the distal radius that extend into the joint are twice as common in women with diabetes [1-3].
Treatment typically involves closed reduction and plaster casting, but unstable fractures may lead to complications, with around 50% of patients experiencing healing issues [4, 5, 6, 7]. Elderly individuals often have a lower demand for their organs, which means they can tolerate some degree of deformity and reduced functionality while still managing to live with them. However, some studies have indicated that a previous fracture in the distal radius may increase the likelihood of fractures in other areas of the body affected by osteoporosis [8-10].
Despite advancements in diagnosing and treating these types of injuries, complications, such as persistent pain, joint stiffness, and decreased strength in the affected joint are still common. These issues can arise not only from severe and complex injuries but also from minor injuries, potentially leading to long-term disability for the patient [11]. Several articles have emphasized the importance of obtaining anatomical reduction and stable fixation and the rapid onset of the range of motion [10, 12].
There is a clear connection between the quality of reduction and the treatment outcomes. Although achieving anatomical reduction does not always ensure positive final results, some patients who did not receive anatomical reduction have still shown good functional outcomes [13, 14].
Intra-articular injuries with severity of trauma evaluation protocol (STEP) score of >2 mm increase the risk of osteoarthritis, while a STEP >1 mm can weaken wrist strength. For extra-articular fractures, radius shortening and volar tilt are key long-term outcome factors. Internal fixation is recommended to maintain reduction [15-18].
Glickel et al. studied closed reduction and percutaneous pinning for distal radius fractures in patients averaging 57 years old, finding excellent long-term outcomes with minimal complications [19]. In a separate study by Vasudevan et al., 490 patients with a mean age of 49.4 years showed high healing rates and excellent operative results, with no serious complications reported [20]. However, Huetteman et al.’s review indicated variability in treatment approaches among different population groups [7]. A 2019 study involving 91 patients over 65 found that surgical treatments led to fewer complications versus conservative methods, emphasizing the importance of thorough diagnosis and communication for treatment decisions [21, 22]. Özkan et al. also confirmed that closed reduction and percutaneous pinning effectively restored function and radiographic parameters post-surgery [23].
Objectives
Choosing the appropriate treatment method for distal radius fractures depends on several factors, primarily the patient’s age and the extent of future use of the injured limb. Given the significance of this issue, the current study aimed to examine the short-term outcomes of percutaneous closure and pinning, which are among the most widely used and least invasive methods for treating distal radius fractures.
Methods
We selected 173 patients over 60 with isolated distal radius fractures at Shafayahyaeian Hospital in Tehran, affiliated with the Iran University of Medical Sciences, between 2022 and 2023. After applying closed immobilization and checking the pins, we included 113 patients. The causes of initial volume loss included the following:
1. Old age and not having a companion to visit the center.
2. Two cases of rheumatoid arthritis
3. Two previous fractures in the same hand
4. Five simultaneous fractures in the limb
5. Two cases of patient death due to gastrointestinal cancer and heart disease
6. Some patients’ residences being far away
7. Returning to job activity after pin removal and related job concerns
8. Satisfaction with the operation a few months after the removal of pins and unwillingness to return
Patients were sampled consecutively from all referrals made during this period. The follow-up period for patients was a minimum of six months, with an average follow-up of nine months. The fractures were classified according to the Fernandez classification (Table 1).

Inclusion criteria
1. Patients with isolated distal radius fracture
2. Patients aged 60 years or older.
3. Patients treated with closed reduction method and pinning through the skin
4. Informed consent to participate in the study
Exclusion criteria
1. History of previous fractures in the hand or elbow
2. History of shoulder fracture
3. Existence of simultaneous fractures in the limb
4. Patients with open fractures
5. Lack of cooperation and follow-up from patients
6. Severe underlying diseases affecting the outcome of the operation, such as rheumatoid arthritis.
Measurement of the active range of motion of the wrist with a goniometer
Extension: With the arm abducted 90 degrees and the elbow bent at 90 degrees in a pronated position, the wrist rests at the table’s edge while the patient flexes the hand upwards. The goniometer’s center is placed on the lateral side of the triforium, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Flexion: The arm is abducted at 90 degrees, and the elbow is flexed at a 90-degree angle with the forearm pronated. The wrist is at the table’s edge, bent downward. The center of the goniometer is placed on the lateral triquetrum, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Radial deviation: The arm is abducted at 90 degrees, and the elbow is flexed at a 90-degree angle with the forearm pronated. The wrist is at the table’s edge, bent downward. The center of the goniometer is placed on the lateral triquetrum, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Ulnar deviation: This involves abducting the arm at 90 degrees, bending the elbow at 90 degrees, pronating the forearm, and placing the wrist at the edge of the table. The patient then turns the hand toward the ulna. The center of the goniometer is positioned on the capitate, with the fixed arm aligned with the forearm’s midline and the movable arm aligned with the third finger.
Pronation: The arm is adducted and placed next to the torso, with the elbow bent at 90 degrees and the forearm in the neutral position. The patient holds a pencil in his/her hand and rotates the forearm toward the body. In this position, the center of the goniometer is on the third finger, the fixed arm is parallel to the humerus, and the movable arm is parallel to the dorsal surface of the forearm.
Supination: The arm is adducted and placed next to the torso, with the elbow bent at 90 degrees and the forearm in the neutral position. The patient holds a pencil in his/her hand and rotates the forearm away from the body. In this position, the center of the goniometer is on the third finger, the fixed arm is parallel to the humerus, and the movable arm is parallel to the volar surface of the forearm.
Functional outcomes of patients were assessed using the disabilities of the arm, shoulder, and hand (QuickDASH) questionnaire six months post-surgery.
QuickDASH is a functional questionnaire that evaluates the upper limb function of a person over the past week. It includes questions to assess the difficulty in performing daily activities, pain during sleep and activity, joint stiffness, and the impact of the upper limb on social and work activities. A higher score indicates greater disability. The QuickDASH questionnaire was validated and confirmed by Mousavi et al. [24] for the Iranian population. Based on QuickDASH scores six months post-surgery, outcomes were classified into four groups: Excellent (0-5), good (6-15), acceptable and satisfactory (16-35), and poor (>35).
Six months after surgery, the patient’s pain was assessed using the visual analog scale (VAS), which ranges from 1 to 10, where a higher number corresponds to more pain.
The grip strength of the injured and healthy hands was measured using a dynamometer six months post-surgery, and its correlation with the patient’s dominant and non-dominant hands was evaluated.
Complications, such as surgical site infection, non:union:, mal:union:, reflex sympathetic dystrophy (RSD), nerve and vascular injury, and the need for reoperation were assessed through examination and radiographic images.
Bone mineral density (BMD) was measured using dual-energy x-ray absorptiometry (DEXA) to assess the quality of the broken bone based on the lowest T score in the lumbar spine and proximal femur. BMD was measured during the first week of hospitalization and classified into three categories according to the World Health Organization (WHO) criteria:
• T score > -1: Normal
• T score between -1 and -2.5: Osteopenia
• T score < -2.5: Osteoporosis
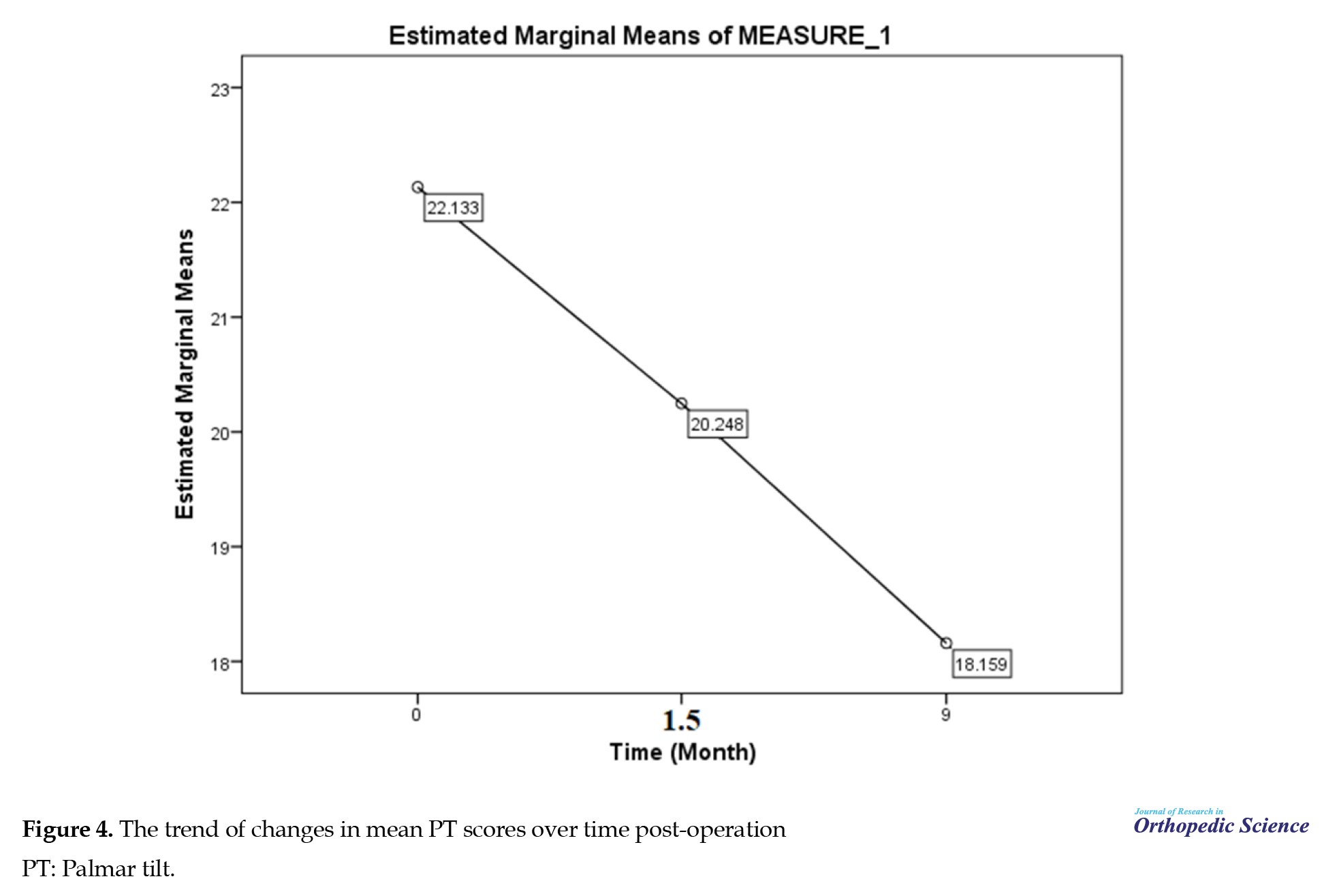
Radiographic findings were assessed using the indices palmar tilt (PT), radial inclination (RI), and radial height (RH) at three time points: 0, 1.5, and 6 months post-surgery. Measurements were recorded, and results were reported as Mean±SD.
• PT: The angle between the line connecting the volar and dorsal edges of the distal radius and the extension of the radius in the lateral view.
• RI: The angle between the line connecting the highest point of the radial styloid to the medial aspect of the distal radius joint surface and the extension of the radius in a periapical (PA) radiograph.
• RH: In a PA radiograph, the distance between the line drawn from the tip of the radial styloid perpendicular to the longitudinal axis of the radius and the line drawn from the distal-most part of the ulna head perpendicular to the longitudinal axis of the radius.
All fractures were treated in the operating room under general or Bier block anesthesia. The fracture reduction was initially checked using fluoroscopy, and after pinning, it was rechecked with a C-arm. Pins of sizes 1.5 mm and 2 mm, or a combination of both, were used for fracture fixation. The number of pins used ranged from two to five, depending on the fracture type and the degree of comminution. The most common pattern was cross-pinning, with two pins on the radial side and one on the ulnar side.
Standard PA and lateral radiographs were taken immediately post-operation, at six weeks, and six months, in coordination with the radiology technician.
A splint or cast was applied to maintain fixation for up to six weeks post-surgery. Pins were removed between five and seven weeks (with a mean of six weeks) after the fracture had healed, based on radiographic evidence of callus formation and the absence of tenderness at the fracture site.
Patients were allowed to resume normal activities 8 to 12 weeks post-surgery. After pin removal, patients were instructed on active and passive wrist and finger movements. Due to limited hand mobility during the follow-up, physiotherapy was prescribed for 16 patients.
Radiographic parameters, wrist range of motion, and grip strength were assessed by the researcher and a hand fellowship specialist who was not involved in the surgery or postoperative care.
Statistical analysis
The data were analyzed using SPSS software. Quantitative data are presented as Mean±SD, while qualitative data are reported as frequencies and percentages. A t-test was used to compare the means of parametric data, while the Mann-Whitney U test was applied for non-parametric data. The chi-square test was used to compare qualitative variables. P<0.05 was considered statistically significant.
Sample size calculation
The sample size for this study was calculated considering P=0.1, d=0.09, and α=95%, based on the appropriate formula. A total of 100 patients with isolated distal radius fractures were included in the study.
Patient information was collected through checklists created by the researcher before the study. Analyzed demographic variables included age, gender, dominant hand, bone density, occupation, mechanism of injury, and underlying health conditions. All collected information is confidential and will not be disclosed. Written informed consent was obtained from all participants.
Results
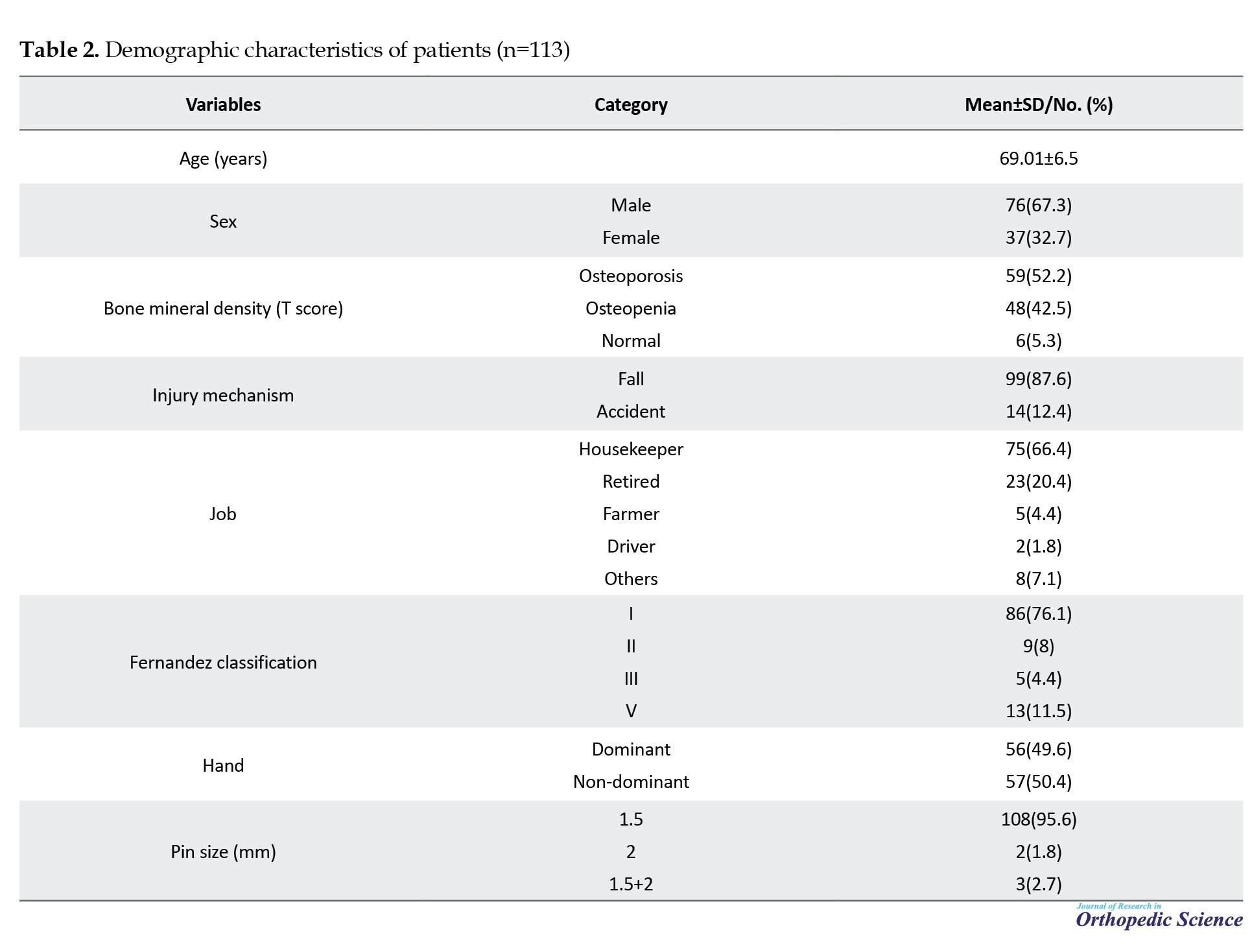
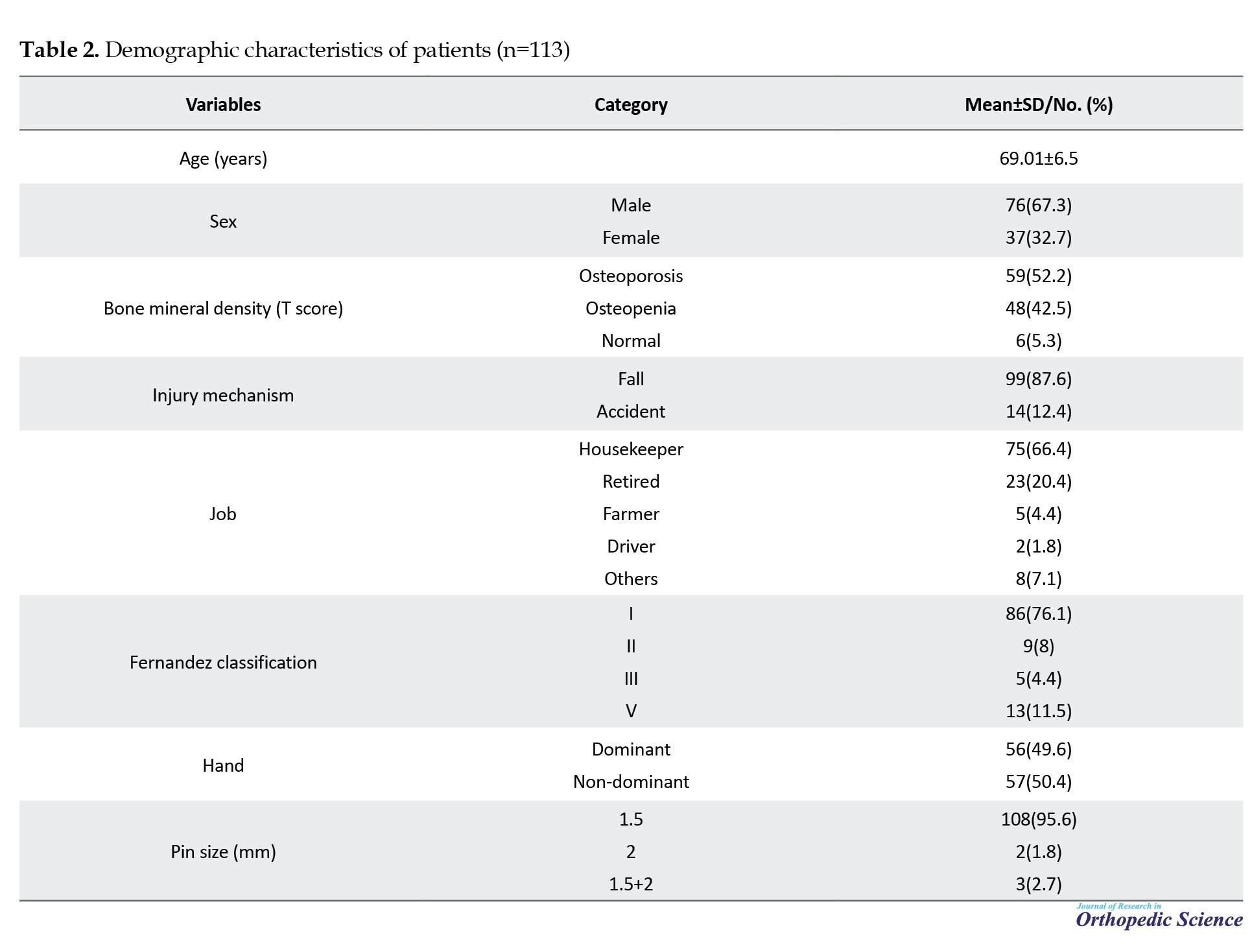
The study involved 113 patients aged over 60 with distal radius fractures who underwent closed reduction and pinning. The mean age was 69.01 years, with 67% of participants being female and 33% male. Fracture types included 76.1% type 1, 8% type 2, 4.4% type 3, and 11.5% type 5 (Figure 1). Regarding bone density, 52.2% had osteoporosis and 42.5% had osteopenia (Figure 2). The primary cause of injury was falls at the same level (87.6%), and 66.4% of patients were housewives. Fractures were almost equally distributed between the dominant hand (49.6%) and the non-dominant hand (50.4%). Demographic characteristics are shown in Table 2.
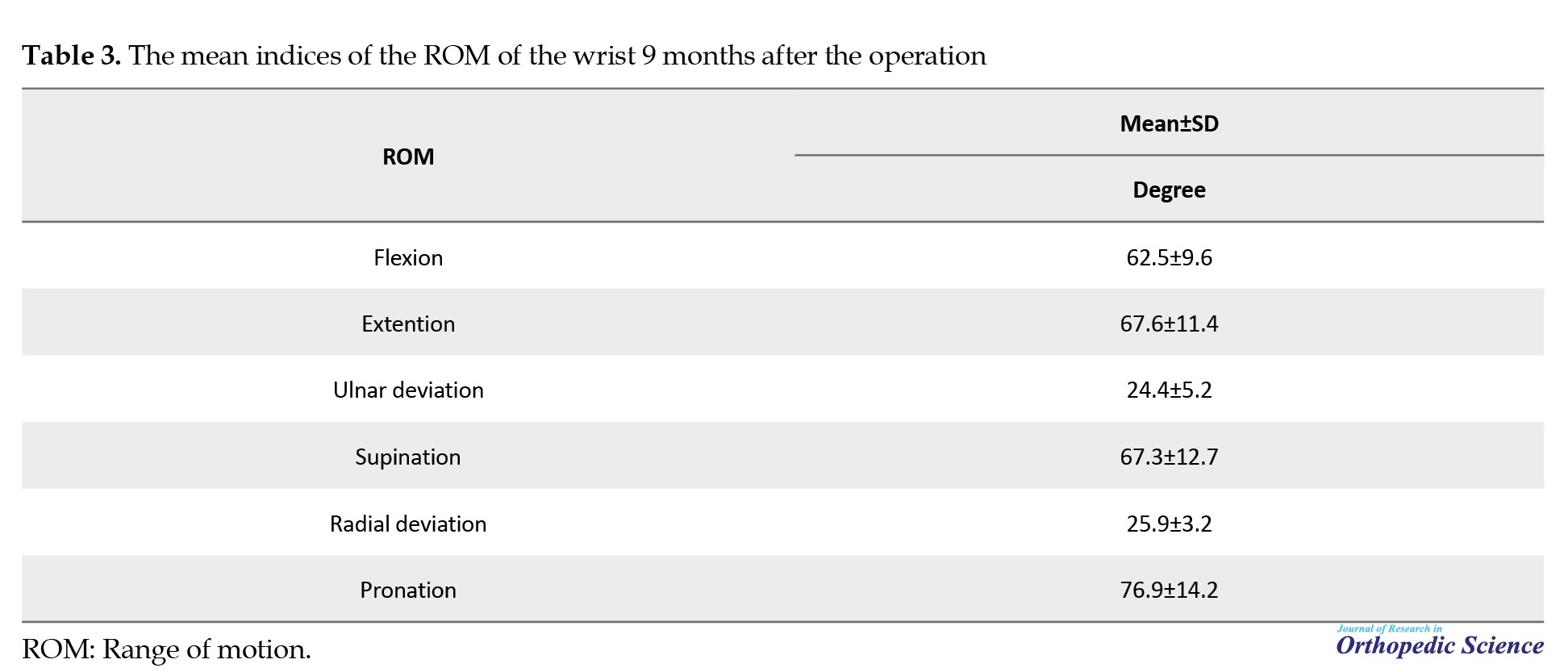
The patient’s wrist motion was evaluated nine months post-surgery by examining extension, flexion, ulnar deviation, supination, radial deviation, and pronation metrics. The mean flexion nine months after the operation was 62.5±9.6 degrees. The mean extension nine months after the operation was 67.6±11.4 degrees. The mean ulnar deviation, supination, radial deviation, and pronation nine months after the operation were 24.4±5.2, 67.3±12.7, 25.9±3.2, and 76.9±14.2 degrees, respectively (Table 3).
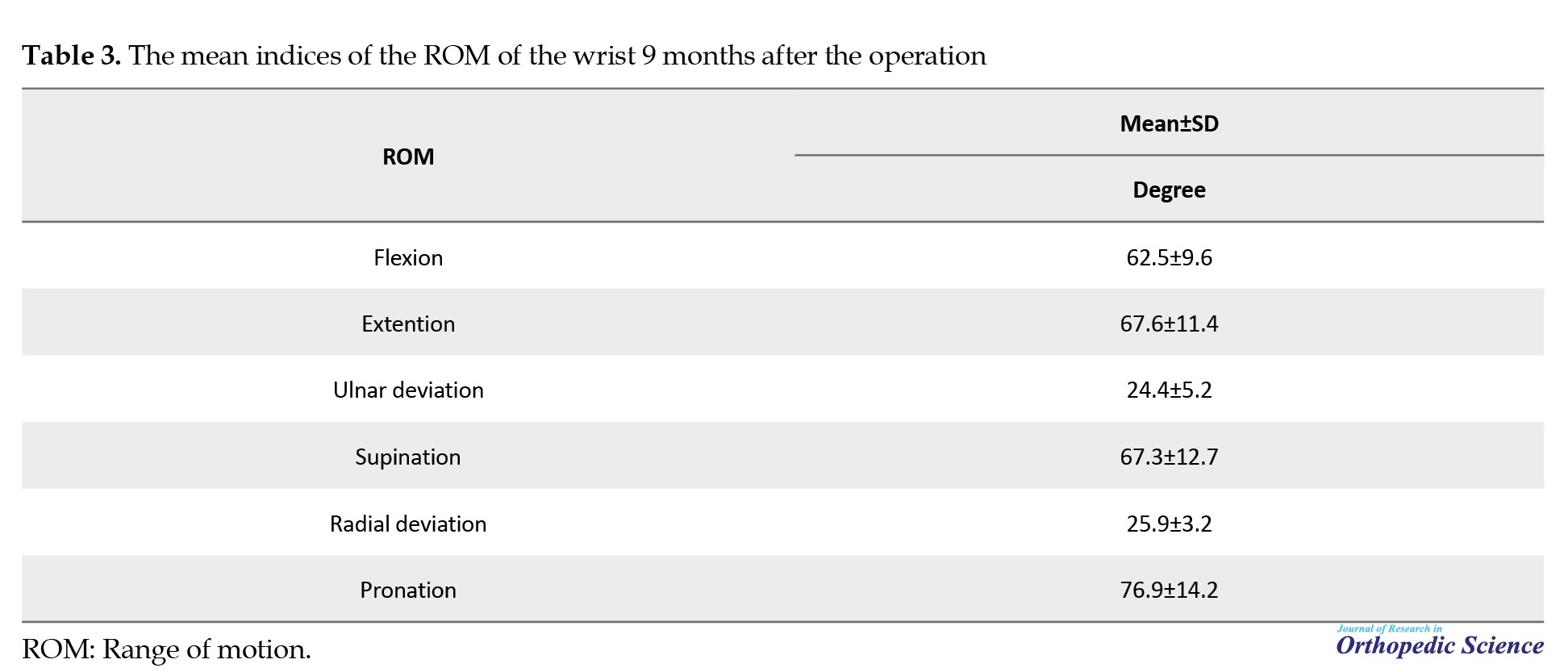
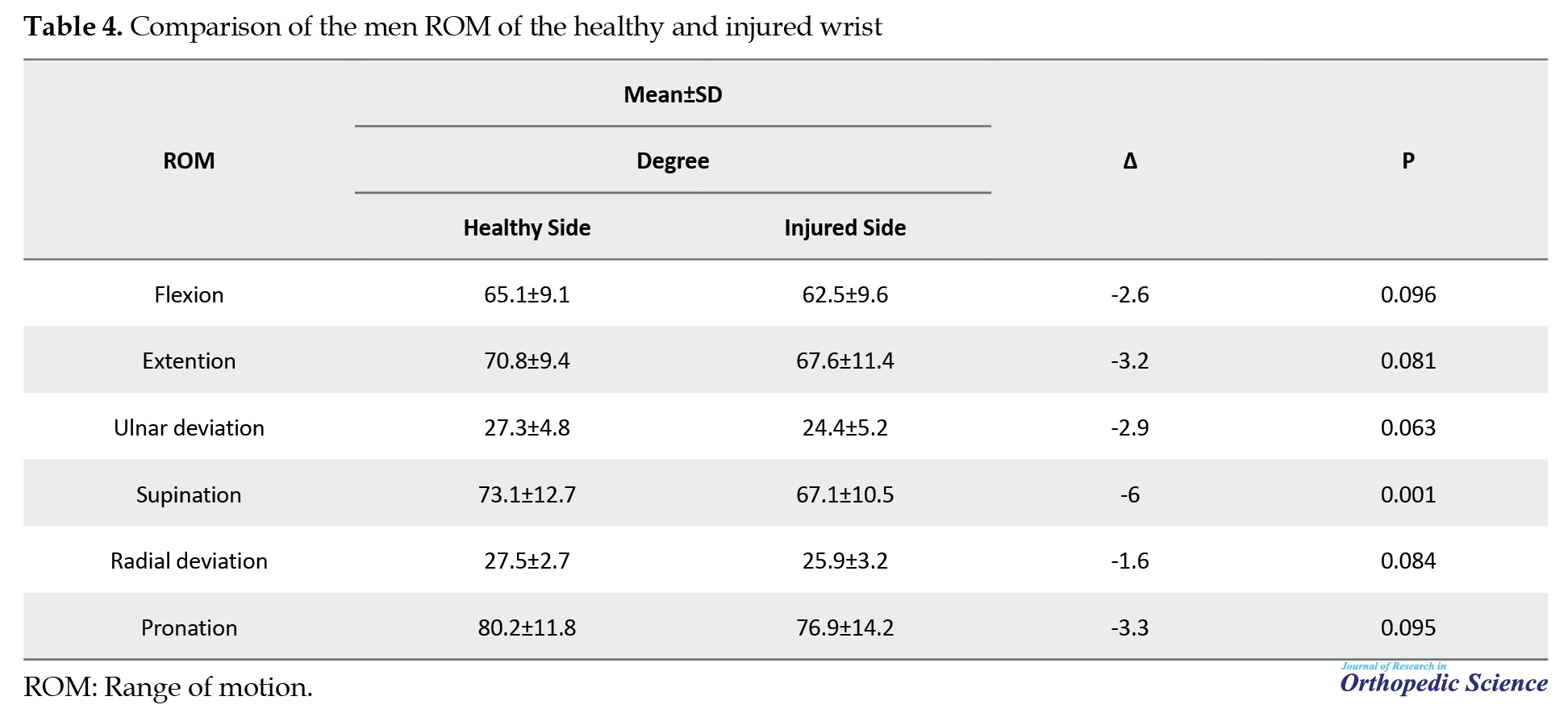
The range of motion of the injured wrist was compared with that of the opposite (healthy) hand. The mean range of motion of the healthy wrist for extension, flexion, ulnar deviation, supination, radial deviation, and pronation indices were 70.8±9.4, 65.1±9.1, 27.3±4.8, 73.1±12.7, 27.5±2.7, and 80.2±11.8 degree, respectively. The mean range of active movement of the injured wrist was similar to that of the healthy hand except for supination, which was 6 degrees lower than that of the healthy hand, and there was no significant difference (Table 4).
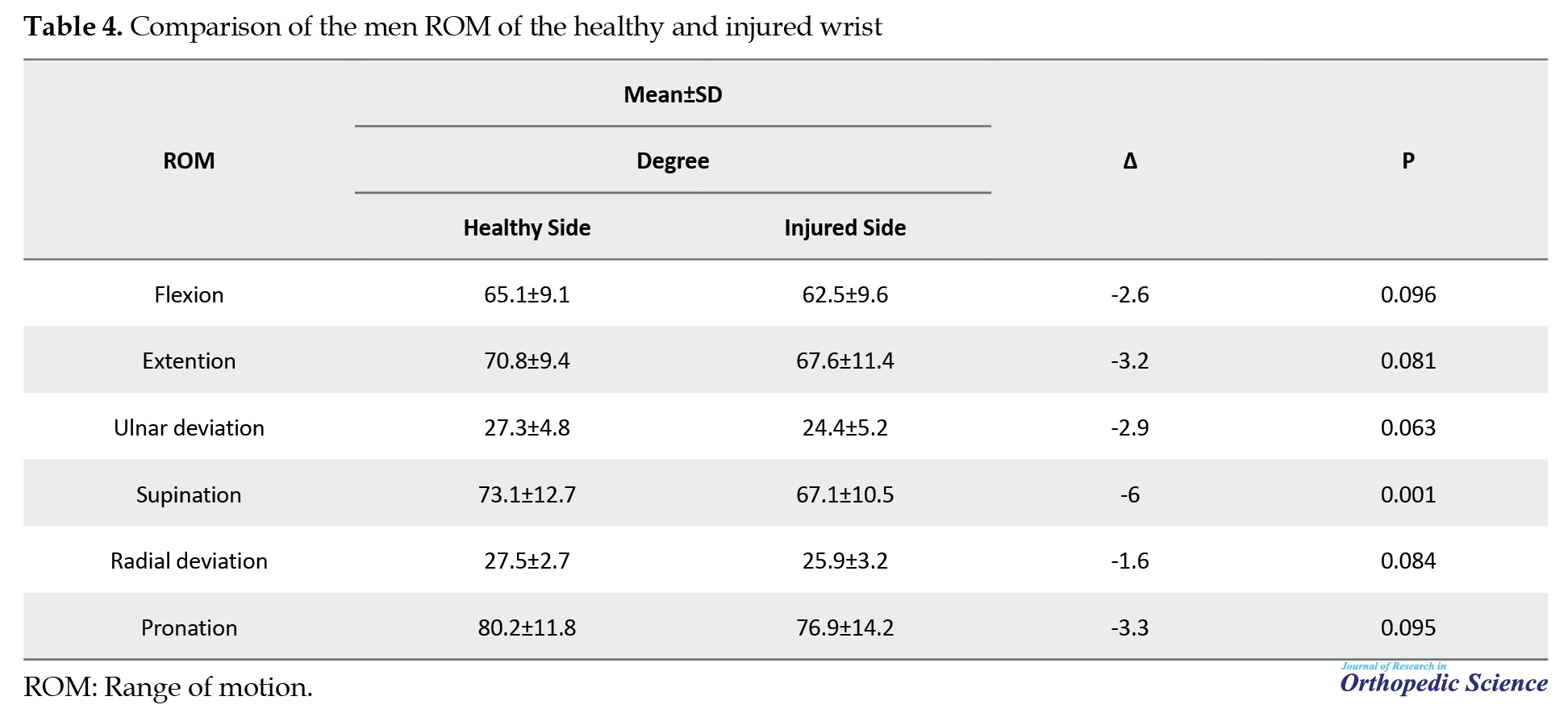
The study found significant positive correlations between wrist range of motion (extension, flexion, supination, pronation, and ulnar deviation) and the DASH-Quick score (P<0.05), indicating that increased motion correlates with improved hand function. Patients with osteoporosis had higher QuickDASH questionnaire scores than those with osteopenia or normal bone density, suggesting that lower bone density is related to decreased function. Nevertheless, no notable correlation was discovered between the QuickDASH questionnaire score and radial deviation or hand strength (P>0.05) (Table 5).
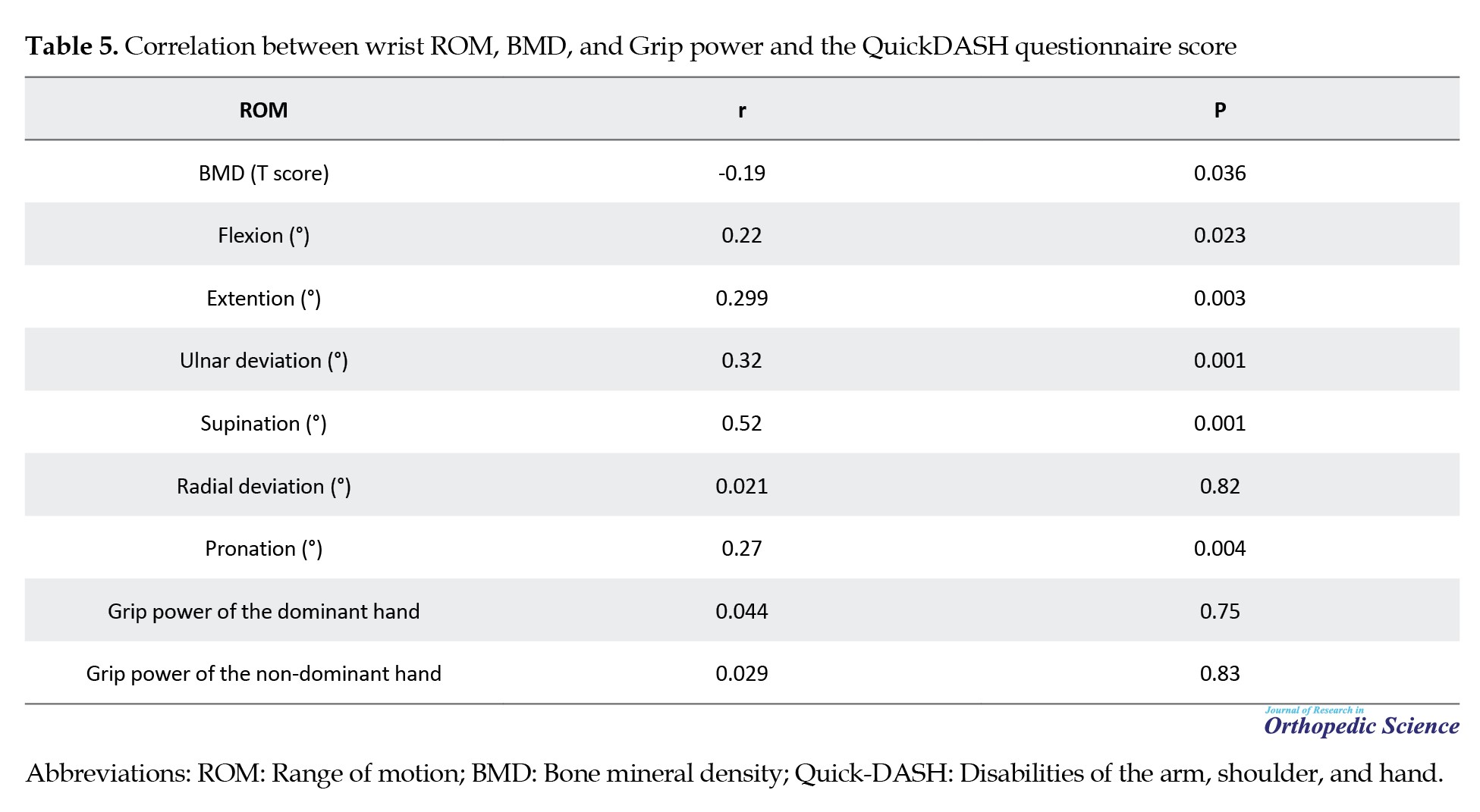
Pearson’s correlation coefficient was used to analyze the relationship between the wrist range of motion, measured nine months post-surgery, and the QuickDASH questionnaire score. While low BMD is often linked to complications, our study found no association between low BMD and loss of reduction, clinical :union:, or fracture type. However, we noted an inverse relationship, where lower BMD corresponded to a higher QuickDASH questionnaire score.
Surgical results based on the QuickDASH questionnaire
Analysis of the QuickDASH questionnaire score nine months after the operation showed that the surgical results were excellent in 40 patients, good in 65 patients, acceptable in six patients, and poor in only two patients (Figure 3). The lowest score was two, and the highest was 37 (mean: 8.06).
Surgical results based on the VAS score
The lowest VAS score recorded at rest was zero, while the highest was six. Nine months after the operation, the mean pain score was 0.93±1.03. Among the patients, 63 individuals (55.8%) reported no pain (VAS score=0), 39 patients (34.5%) experienced mild pain (VAS score=1-3), and 11 patients (9.7%) had moderate to severe pain (VAS score=4-6). No patients reported experiencing severe pain, defined as a VAS score of seven to ten.
Regarding pain during activity, 57 patients reported a VAS score of zero, 43 patients experienced mild pain, and 13 reported moderate to severe pain.
Results of radiographic findings 0, 1.5, and 9 months after the operation based on PT, RI, and RH indicators
The mean PT score decreased 1.5 months after the operation compared to immediately after the operation (P=0.001). The mean PT score immediately, 1.5 months, and 9 months after the operation was 7.04, 6.17, and 5.12 degrees, respectively (Figure 4). The mean RI score decreased by 1.5 months post-operation compared to immediately after (P=0.001), with scores at 22.1, 20.2, and 18.2 degrees immediately, 1.5 months, and 9 months after the operation, respectively (Figures 5 and 6). While mean RH, RI, and PT scores decreased at nine months, this decline was not statistically significant (P>0.05). There were no significant differences in improvements between 1.5 and 9 months post-operation (P>0.05). Changes in radiological indicators are detailed in Table 6.
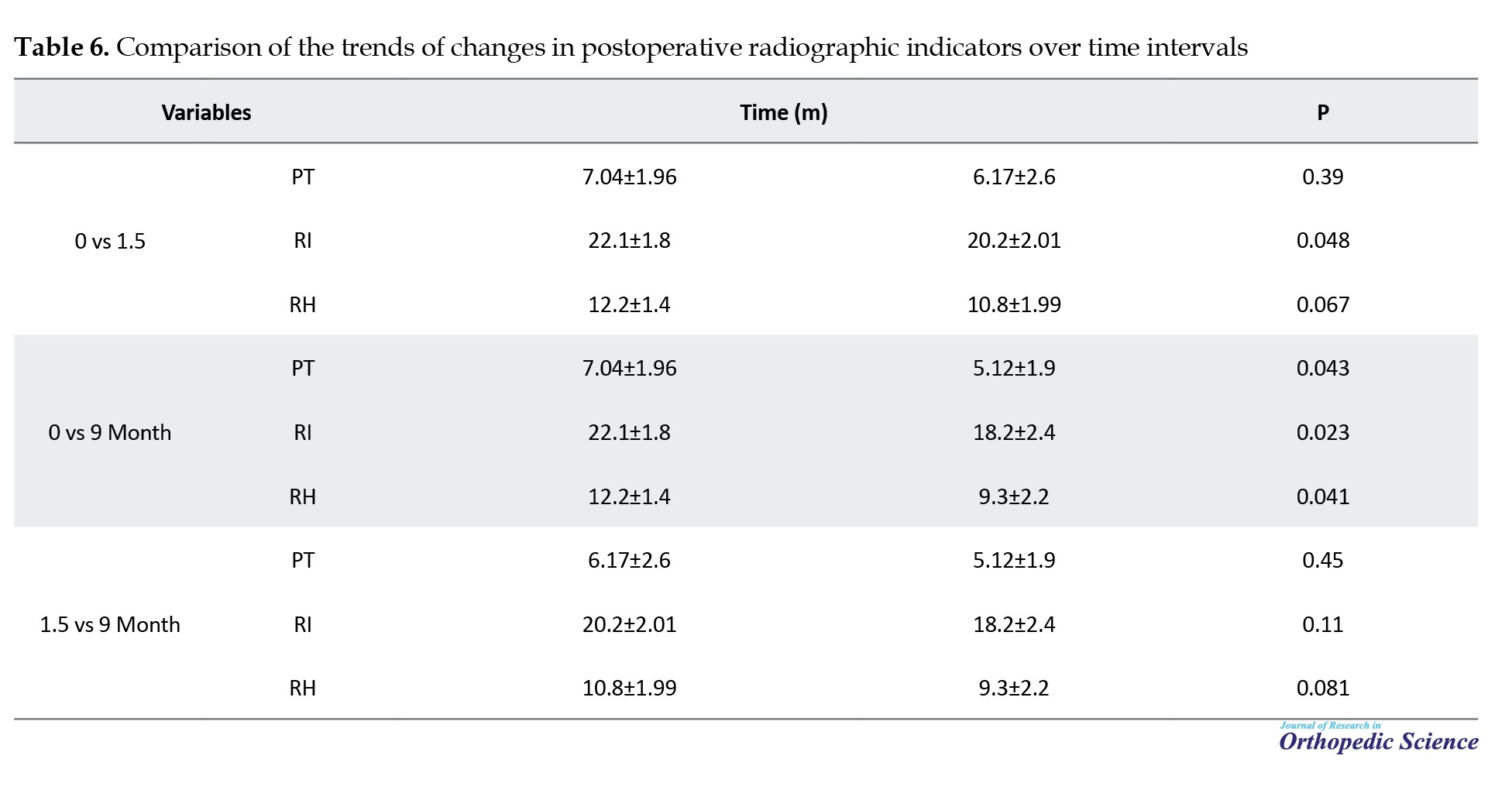
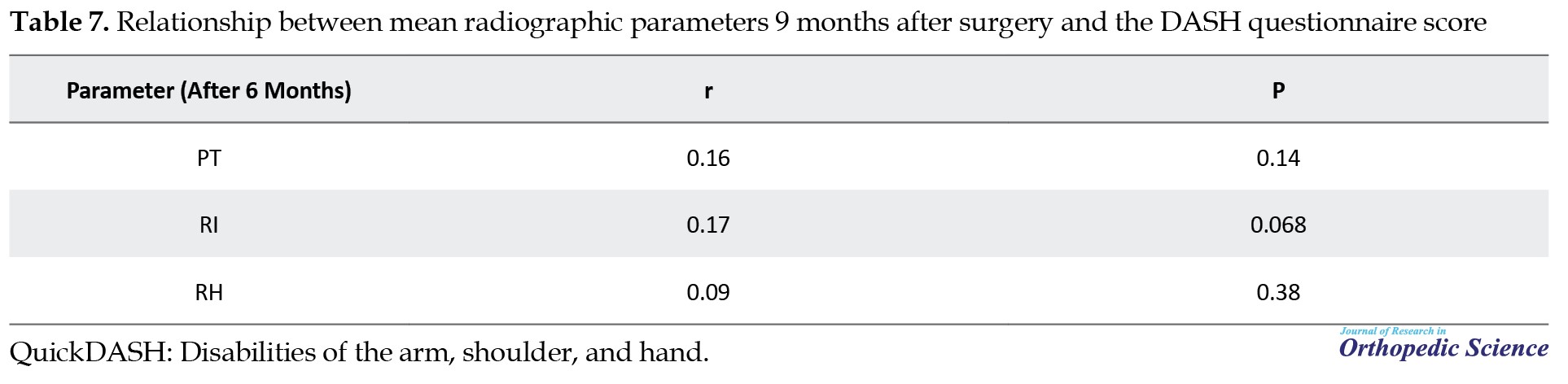
Eight patients with low PT scores (0, 1, and 2 degrees) had a maximum dorsal tilt of 8 degrees during treatment. No significant correlation was found between the radiological indicators measured at nine months and the QuickDASH questionnaire score or BMD, as shown in Table 7.
Pearson’s correlation coefficient was utilized to evaluate the relationship between the mean range of motion indices of the wrist nine months post-surgery and the DASH questionnaire score.
Grip power
The mean hand strength was evaluated in pounds (lbs) nine months after surgery using a dynamometer. There was no significant difference in the mean strength scores of the injured hand compared to the healthy hand, regardless of whether it was the dominant or non-dominant hand. However, this difference was more noticeable in the non-dominant hand that suffered a fracture (Table 8).

Complications
In the course of treatment, four patients developed complex regional pain syndrome (CRPS). The symptoms of three patients improved with physical therapy and drug treatment, while the symptoms of one patient did not improve. Three patients experienced a pin tract infection, and all three cases fully recovered with debridement and oral antibiotics. Additionally, one patient suffered damage to the superficial radial nerve. There were no cases of loss of reduction, need for re-surgery, non-:union:, or poor :union:.
Discussion
Fractures of the distal radius are among the most common orthopedic injuries, particularly in children and individuals over 60 years old. In the elderly population, distal radius fractures account for 18% of all fractures. Various treatment options have been introduced for these fractures, with the choice of treatment typically depending on factors, such as the patient’s age, activity level, and preferences, as well as those of the surgeon. Despite the high incidence of distal radius fractures, there is still no consensus on the most effective treatment method for patients over 60 [25-29].
This study aimed to evaluate the short-term outcomes of closed reduction and pinning surgery in elderly patients with distal radius fractures, involving 113 participants. The results indicated that nine months post-surgery, most patients experienced good or excellent outcomes, with only a few reporting moderate or poor results. Two patients had poor outcomes due to complications, such as RSD and significant bone comminution. Among the six patients with moderate outcomes, some experienced issues, like dorsal tilt or osteoporosis.
In terms of functional outcomes, including wrist movement, the results were generally satisfactory. There was a significant positive correlation between wrist motion parameters—such as extension, flexion, supination, and pronation—and the DASH questionnaire score. This suggests that as wrist motion improved, functional outcomes also improved. Radiographic outcomes, including PT, RI, and RH, showed some decline over time; however, there were no significant differences between the stages of fracture stabilization and healing.
Although there was a reduction in some radiographic indicators, this did not negatively affect the functional outcomes, suggesting that patients were still able to use their operated hand effectively in daily activities. It was noted that while some loss of reduction occurred—particularly in terms of volar tilt—the overall radiographic parameters did not significantly impact treatment outcomes. Pain levels were low; most patients reported no pain nine months after surgery. Additionally, hand strength in the injured hand was similar to that of the uninjured hand in most patients, with no significant differences in grip strength.
The results of this study align with previous findings [19, 20, 22, 30, 31]. These studies show that closed reduction and pinning are effective treatments for distal radius fractures in elderly patients, providing good functional outcomes and low complication rates, thereby making it a reliable and cost-effective treatment option.
Conclusion
In conclusion, this study suggests that closed reduction and pinning are both effective and practical treatment options for distal radius fractures in elderly patients. These methods lead to good functional outcomes, acceptable radiographic results, and minimal complications. Additionally, it is recommended that BMD be assessed in elderly patients with osteoporosis to optimize treatment management.
Overall, this study demonstrated that closed reduction and pinning surgery results in good functional outcomes, adequate range of motion, and acceptable radiographic parameters in patients over 60 with distal radius fractures in the short term. Hand strength and wrist range of motion nine months post-surgery were similar to those of the healthy hand. Closed reduction and pinning are viable and effective options for treating distal radius fractures in patients over 60 and should be considered reliable methods for restoring both radiographic parameters and functional outcomes.
Strengths and weaknesses
Our study had some limitations that should be addressed. The main weakness was the lack of a comparison between the results of this surgical method and a control group treated with a different approach. Due to the design and objectives of the study, the follow-up period for patients was shorter than in other studies. A prospective study with a longer follow-up period could provide a more accurate assessment of the closed reduction and pinning in patients over 60 with distal radius fractures. Another limitation was that several surgeons carried out surgeries in the teaching hospital. A key strength of the current study was the assessment of functional outcomes, wrist range of motion, grip strength, radiographic parameters, and BMD in an appropriately sized sample of patients over 60 with distal radius fractures over the short term. Our study had some limitations that should be addressed. The main weakness was the lack of a comparison between the results of this surgical method and a control group treated with a different approach. Due to the design and objectives of the study, the follow-up period for patients was shorter than in other studies. A prospective study with a longer follow-up period could provide a more accurate assessment of closed reduction and pinning in patients over 60 with distal radius fractures. Another limitation was that several surgeons carried out surgeries in the teaching hospital. A key strength of the current study was the assessment of functional outcomes, wrist range of motion, grip strength, radiographic parameters, and BMD in an appropriately sized sample of patients over 60 with distal radius fractures over the short term.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from all participants. The research adhered to the principles of the Helsinki Convention and received approval from the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1401.527). The patients incurred no additional costs or interventions.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
Distal radius fractures are common, accounting for about 16% of all fractures in emergency departments and 20% of accident-related fractures. They predominantly affect elderly women due to osteoporosis and adult men through high-impact activities. Other important risk factors for distal radius fractures in patients older than 50 years include falls, a history of previous fractures, the use of corticosteroids, and advanced age. Dementia is also a risk factor in patients older than 75 years. In older patients, any additional risk factor increases the likelihood of a distal radius fracture. Fractures of the distal radius that extend into the joint are twice as common in women with diabetes [1-3].
Treatment typically involves closed reduction and plaster casting, but unstable fractures may lead to complications, with around 50% of patients experiencing healing issues [4, 5, 6, 7]. Elderly individuals often have a lower demand for their organs, which means they can tolerate some degree of deformity and reduced functionality while still managing to live with them. However, some studies have indicated that a previous fracture in the distal radius may increase the likelihood of fractures in other areas of the body affected by osteoporosis [8-10].
Despite advancements in diagnosing and treating these types of injuries, complications, such as persistent pain, joint stiffness, and decreased strength in the affected joint are still common. These issues can arise not only from severe and complex injuries but also from minor injuries, potentially leading to long-term disability for the patient [11]. Several articles have emphasized the importance of obtaining anatomical reduction and stable fixation and the rapid onset of the range of motion [10, 12].
There is a clear connection between the quality of reduction and the treatment outcomes. Although achieving anatomical reduction does not always ensure positive final results, some patients who did not receive anatomical reduction have still shown good functional outcomes [13, 14].
Intra-articular injuries with severity of trauma evaluation protocol (STEP) score of >2 mm increase the risk of osteoarthritis, while a STEP >1 mm can weaken wrist strength. For extra-articular fractures, radius shortening and volar tilt are key long-term outcome factors. Internal fixation is recommended to maintain reduction [15-18].
Glickel et al. studied closed reduction and percutaneous pinning for distal radius fractures in patients averaging 57 years old, finding excellent long-term outcomes with minimal complications [19]. In a separate study by Vasudevan et al., 490 patients with a mean age of 49.4 years showed high healing rates and excellent operative results, with no serious complications reported [20]. However, Huetteman et al.’s review indicated variability in treatment approaches among different population groups [7]. A 2019 study involving 91 patients over 65 found that surgical treatments led to fewer complications versus conservative methods, emphasizing the importance of thorough diagnosis and communication for treatment decisions [21, 22]. Özkan et al. also confirmed that closed reduction and percutaneous pinning effectively restored function and radiographic parameters post-surgery [23].
Objectives
Choosing the appropriate treatment method for distal radius fractures depends on several factors, primarily the patient’s age and the extent of future use of the injured limb. Given the significance of this issue, the current study aimed to examine the short-term outcomes of percutaneous closure and pinning, which are among the most widely used and least invasive methods for treating distal radius fractures.
Methods
We selected 173 patients over 60 with isolated distal radius fractures at Shafayahyaeian Hospital in Tehran, affiliated with the Iran University of Medical Sciences, between 2022 and 2023. After applying closed immobilization and checking the pins, we included 113 patients. The causes of initial volume loss included the following:
1. Old age and not having a companion to visit the center.
2. Two cases of rheumatoid arthritis
3. Two previous fractures in the same hand
4. Five simultaneous fractures in the limb
5. Two cases of patient death due to gastrointestinal cancer and heart disease
6. Some patients’ residences being far away
7. Returning to job activity after pin removal and related job concerns
8. Satisfaction with the operation a few months after the removal of pins and unwillingness to return
Patients were sampled consecutively from all referrals made during this period. The follow-up period for patients was a minimum of six months, with an average follow-up of nine months. The fractures were classified according to the Fernandez classification (Table 1).

Inclusion criteria
1. Patients with isolated distal radius fracture
2. Patients aged 60 years or older.
3. Patients treated with closed reduction method and pinning through the skin
4. Informed consent to participate in the study
Exclusion criteria
1. History of previous fractures in the hand or elbow
2. History of shoulder fracture
3. Existence of simultaneous fractures in the limb
4. Patients with open fractures
5. Lack of cooperation and follow-up from patients
6. Severe underlying diseases affecting the outcome of the operation, such as rheumatoid arthritis.
Measurement of the active range of motion of the wrist with a goniometer
Extension: With the arm abducted 90 degrees and the elbow bent at 90 degrees in a pronated position, the wrist rests at the table’s edge while the patient flexes the hand upwards. The goniometer’s center is placed on the lateral side of the triforium, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Flexion: The arm is abducted at 90 degrees, and the elbow is flexed at a 90-degree angle with the forearm pronated. The wrist is at the table’s edge, bent downward. The center of the goniometer is placed on the lateral triquetrum, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Radial deviation: The arm is abducted at 90 degrees, and the elbow is flexed at a 90-degree angle with the forearm pronated. The wrist is at the table’s edge, bent downward. The center of the goniometer is placed on the lateral triquetrum, with the fixed arm parallel to the ulna and the movable arm parallel to the fifth metacarpal.
Ulnar deviation: This involves abducting the arm at 90 degrees, bending the elbow at 90 degrees, pronating the forearm, and placing the wrist at the edge of the table. The patient then turns the hand toward the ulna. The center of the goniometer is positioned on the capitate, with the fixed arm aligned with the forearm’s midline and the movable arm aligned with the third finger.
Pronation: The arm is adducted and placed next to the torso, with the elbow bent at 90 degrees and the forearm in the neutral position. The patient holds a pencil in his/her hand and rotates the forearm toward the body. In this position, the center of the goniometer is on the third finger, the fixed arm is parallel to the humerus, and the movable arm is parallel to the dorsal surface of the forearm.
Supination: The arm is adducted and placed next to the torso, with the elbow bent at 90 degrees and the forearm in the neutral position. The patient holds a pencil in his/her hand and rotates the forearm away from the body. In this position, the center of the goniometer is on the third finger, the fixed arm is parallel to the humerus, and the movable arm is parallel to the volar surface of the forearm.
Functional outcomes of patients were assessed using the disabilities of the arm, shoulder, and hand (QuickDASH) questionnaire six months post-surgery.
QuickDASH is a functional questionnaire that evaluates the upper limb function of a person over the past week. It includes questions to assess the difficulty in performing daily activities, pain during sleep and activity, joint stiffness, and the impact of the upper limb on social and work activities. A higher score indicates greater disability. The QuickDASH questionnaire was validated and confirmed by Mousavi et al. [24] for the Iranian population. Based on QuickDASH scores six months post-surgery, outcomes were classified into four groups: Excellent (0-5), good (6-15), acceptable and satisfactory (16-35), and poor (>35).
Six months after surgery, the patient’s pain was assessed using the visual analog scale (VAS), which ranges from 1 to 10, where a higher number corresponds to more pain.
The grip strength of the injured and healthy hands was measured using a dynamometer six months post-surgery, and its correlation with the patient’s dominant and non-dominant hands was evaluated.
Complications, such as surgical site infection, non:union:, mal:union:, reflex sympathetic dystrophy (RSD), nerve and vascular injury, and the need for reoperation were assessed through examination and radiographic images.
Bone mineral density (BMD) was measured using dual-energy x-ray absorptiometry (DEXA) to assess the quality of the broken bone based on the lowest T score in the lumbar spine and proximal femur. BMD was measured during the first week of hospitalization and classified into three categories according to the World Health Organization (WHO) criteria:
• T score > -1: Normal
• T score between -1 and -2.5: Osteopenia
• T score < -2.5: Osteoporosis
Radiographic findings were assessed using the indices palmar tilt (PT), radial inclination (RI), and radial height (RH) at three time points: 0, 1.5, and 6 months post-surgery. Measurements were recorded, and results were reported as Mean±SD.
• PT: The angle between the line connecting the volar and dorsal edges of the distal radius and the extension of the radius in the lateral view.
• RI: The angle between the line connecting the highest point of the radial styloid to the medial aspect of the distal radius joint surface and the extension of the radius in a periapical (PA) radiograph.
• RH: In a PA radiograph, the distance between the line drawn from the tip of the radial styloid perpendicular to the longitudinal axis of the radius and the line drawn from the distal-most part of the ulna head perpendicular to the longitudinal axis of the radius.
All fractures were treated in the operating room under general or Bier block anesthesia. The fracture reduction was initially checked using fluoroscopy, and after pinning, it was rechecked with a C-arm. Pins of sizes 1.5 mm and 2 mm, or a combination of both, were used for fracture fixation. The number of pins used ranged from two to five, depending on the fracture type and the degree of comminution. The most common pattern was cross-pinning, with two pins on the radial side and one on the ulnar side.
Standard PA and lateral radiographs were taken immediately post-operation, at six weeks, and six months, in coordination with the radiology technician.
A splint or cast was applied to maintain fixation for up to six weeks post-surgery. Pins were removed between five and seven weeks (with a mean of six weeks) after the fracture had healed, based on radiographic evidence of callus formation and the absence of tenderness at the fracture site.
Patients were allowed to resume normal activities 8 to 12 weeks post-surgery. After pin removal, patients were instructed on active and passive wrist and finger movements. Due to limited hand mobility during the follow-up, physiotherapy was prescribed for 16 patients.
Radiographic parameters, wrist range of motion, and grip strength were assessed by the researcher and a hand fellowship specialist who was not involved in the surgery or postoperative care.
Statistical analysis
The data were analyzed using SPSS software. Quantitative data are presented as Mean±SD, while qualitative data are reported as frequencies and percentages. A t-test was used to compare the means of parametric data, while the Mann-Whitney U test was applied for non-parametric data. The chi-square test was used to compare qualitative variables. P<0.05 was considered statistically significant.
Sample size calculation
The sample size for this study was calculated considering P=0.1, d=0.09, and α=95%, based on the appropriate formula. A total of 100 patients with isolated distal radius fractures were included in the study.
Patient information was collected through checklists created by the researcher before the study. Analyzed demographic variables included age, gender, dominant hand, bone density, occupation, mechanism of injury, and underlying health conditions. All collected information is confidential and will not be disclosed. Written informed consent was obtained from all participants.
Results
The study involved 113 patients aged over 60 with distal radius fractures who underwent closed reduction and pinning. The mean age was 69.01 years, with 67% of participants being female and 33% male. Fracture types included 76.1% type 1, 8% type 2, 4.4% type 3, and 11.5% type 5 (Figure 1). Regarding bone density, 52.2% had osteoporosis and 42.5% had osteopenia (Figure 2). The primary cause of injury was falls at the same level (87.6%), and 66.4% of patients were housewives. Fractures were almost equally distributed between the dominant hand (49.6%) and the non-dominant hand (50.4%). Demographic characteristics are shown in Table 2.
The patient’s wrist motion was evaluated nine months post-surgery by examining extension, flexion, ulnar deviation, supination, radial deviation, and pronation metrics. The mean flexion nine months after the operation was 62.5±9.6 degrees. The mean extension nine months after the operation was 67.6±11.4 degrees. The mean ulnar deviation, supination, radial deviation, and pronation nine months after the operation were 24.4±5.2, 67.3±12.7, 25.9±3.2, and 76.9±14.2 degrees, respectively (Table 3).
The range of motion of the injured wrist was compared with that of the opposite (healthy) hand. The mean range of motion of the healthy wrist for extension, flexion, ulnar deviation, supination, radial deviation, and pronation indices were 70.8±9.4, 65.1±9.1, 27.3±4.8, 73.1±12.7, 27.5±2.7, and 80.2±11.8 degree, respectively. The mean range of active movement of the injured wrist was similar to that of the healthy hand except for supination, which was 6 degrees lower than that of the healthy hand, and there was no significant difference (Table 4).
The study found significant positive correlations between wrist range of motion (extension, flexion, supination, pronation, and ulnar deviation) and the DASH-Quick score (P<0.05), indicating that increased motion correlates with improved hand function. Patients with osteoporosis had higher QuickDASH questionnaire scores than those with osteopenia or normal bone density, suggesting that lower bone density is related to decreased function. Nevertheless, no notable correlation was discovered between the QuickDASH questionnaire score and radial deviation or hand strength (P>0.05) (Table 5).
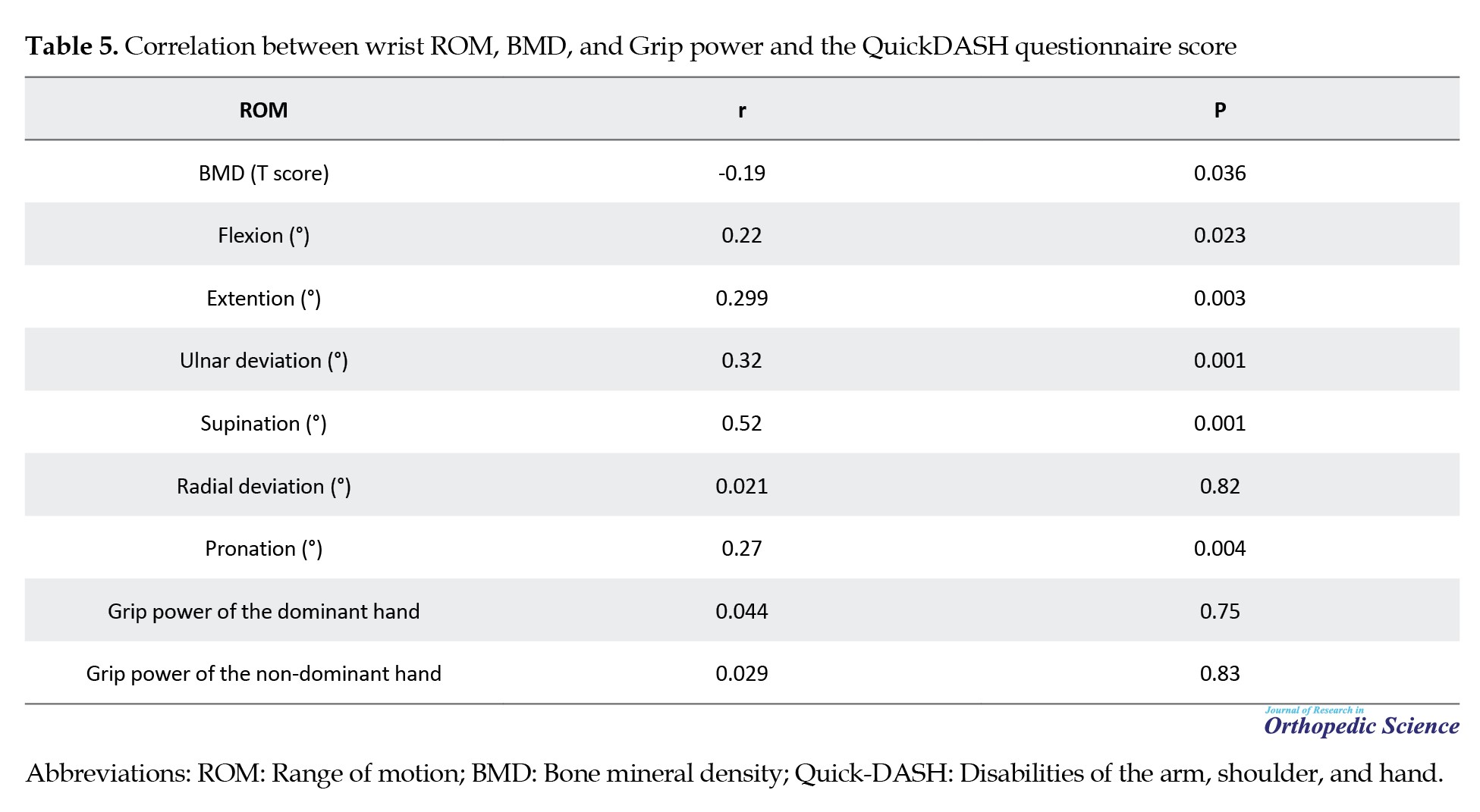
Pearson’s correlation coefficient was used to analyze the relationship between the wrist range of motion, measured nine months post-surgery, and the QuickDASH questionnaire score. While low BMD is often linked to complications, our study found no association between low BMD and loss of reduction, clinical :union:, or fracture type. However, we noted an inverse relationship, where lower BMD corresponded to a higher QuickDASH questionnaire score.
Surgical results based on the QuickDASH questionnaire
Analysis of the QuickDASH questionnaire score nine months after the operation showed that the surgical results were excellent in 40 patients, good in 65 patients, acceptable in six patients, and poor in only two patients (Figure 3). The lowest score was two, and the highest was 37 (mean: 8.06).
Surgical results based on the VAS score
The lowest VAS score recorded at rest was zero, while the highest was six. Nine months after the operation, the mean pain score was 0.93±1.03. Among the patients, 63 individuals (55.8%) reported no pain (VAS score=0), 39 patients (34.5%) experienced mild pain (VAS score=1-3), and 11 patients (9.7%) had moderate to severe pain (VAS score=4-6). No patients reported experiencing severe pain, defined as a VAS score of seven to ten.
Regarding pain during activity, 57 patients reported a VAS score of zero, 43 patients experienced mild pain, and 13 reported moderate to severe pain.
Results of radiographic findings 0, 1.5, and 9 months after the operation based on PT, RI, and RH indicators
The mean PT score decreased 1.5 months after the operation compared to immediately after the operation (P=0.001). The mean PT score immediately, 1.5 months, and 9 months after the operation was 7.04, 6.17, and 5.12 degrees, respectively (Figure 4). The mean RI score decreased by 1.5 months post-operation compared to immediately after (P=0.001), with scores at 22.1, 20.2, and 18.2 degrees immediately, 1.5 months, and 9 months after the operation, respectively (Figures 5 and 6). While mean RH, RI, and PT scores decreased at nine months, this decline was not statistically significant (P>0.05). There were no significant differences in improvements between 1.5 and 9 months post-operation (P>0.05). Changes in radiological indicators are detailed in Table 6.
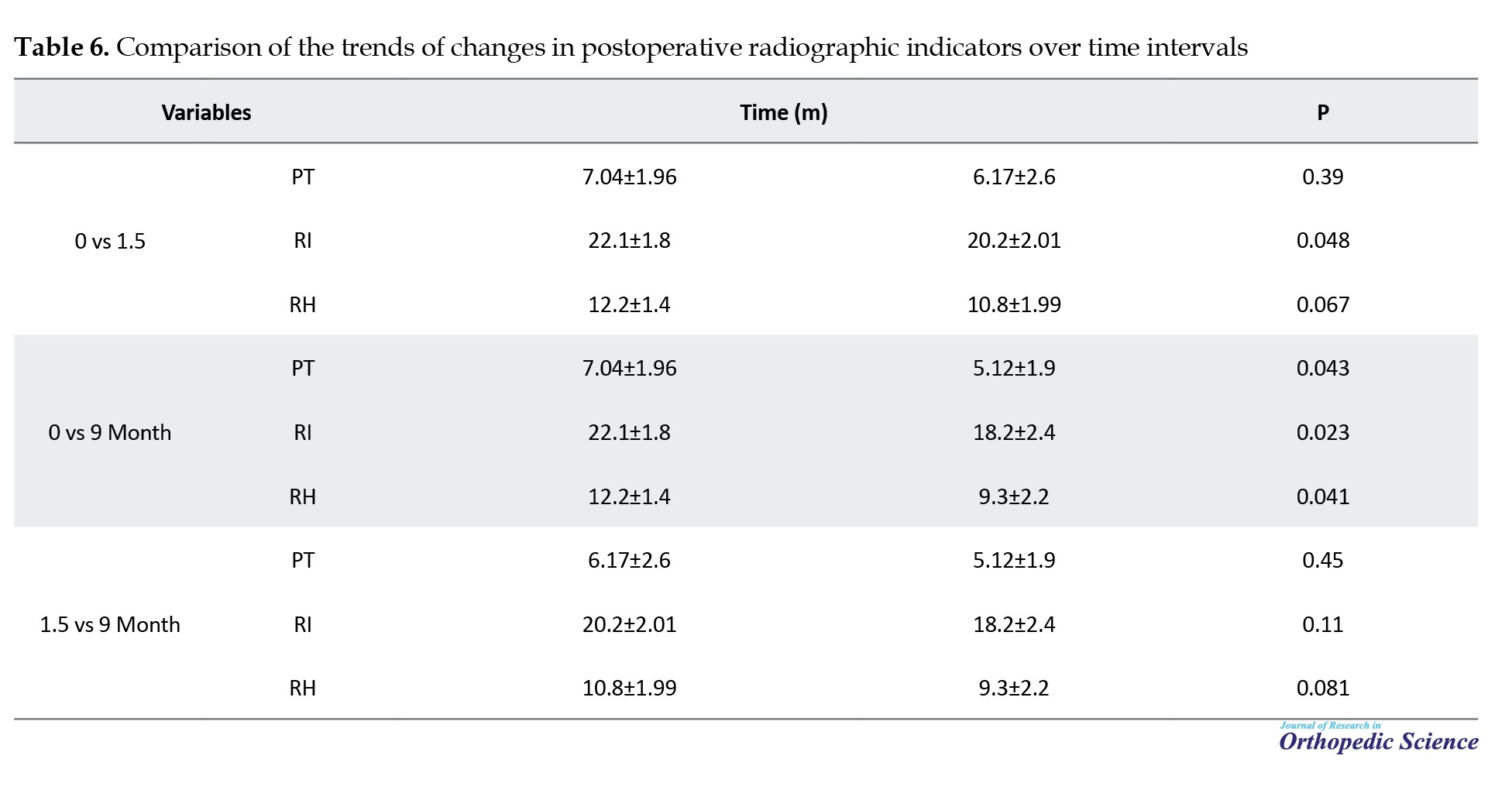
Eight patients with low PT scores (0, 1, and 2 degrees) had a maximum dorsal tilt of 8 degrees during treatment. No significant correlation was found between the radiological indicators measured at nine months and the QuickDASH questionnaire score or BMD, as shown in Table 7.
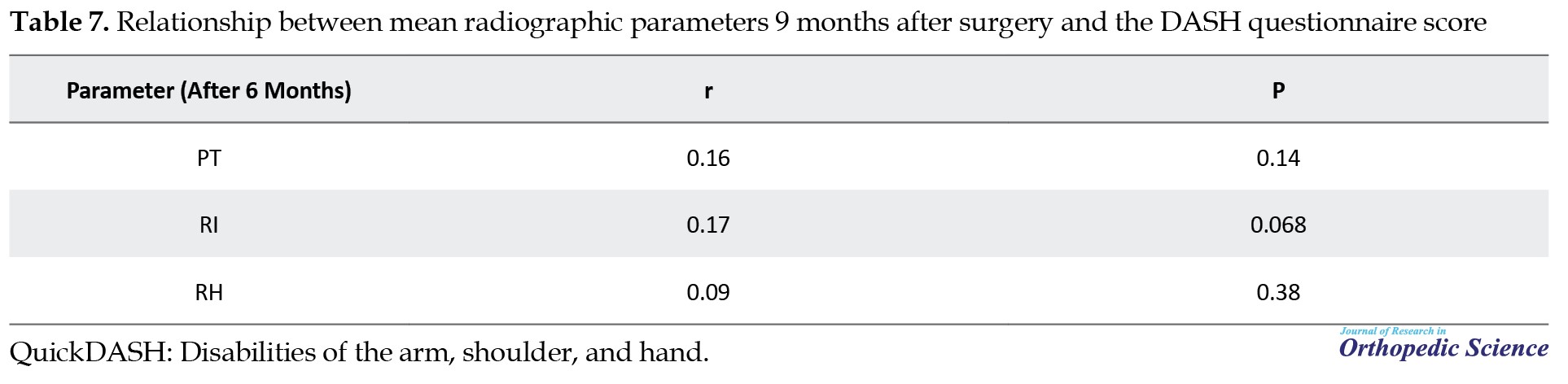
Pearson’s correlation coefficient was utilized to evaluate the relationship between the mean range of motion indices of the wrist nine months post-surgery and the DASH questionnaire score.
Grip power
The mean hand strength was evaluated in pounds (lbs) nine months after surgery using a dynamometer. There was no significant difference in the mean strength scores of the injured hand compared to the healthy hand, regardless of whether it was the dominant or non-dominant hand. However, this difference was more noticeable in the non-dominant hand that suffered a fracture (Table 8).

Complications
In the course of treatment, four patients developed complex regional pain syndrome (CRPS). The symptoms of three patients improved with physical therapy and drug treatment, while the symptoms of one patient did not improve. Three patients experienced a pin tract infection, and all three cases fully recovered with debridement and oral antibiotics. Additionally, one patient suffered damage to the superficial radial nerve. There were no cases of loss of reduction, need for re-surgery, non-:union:, or poor :union:.
Discussion
Fractures of the distal radius are among the most common orthopedic injuries, particularly in children and individuals over 60 years old. In the elderly population, distal radius fractures account for 18% of all fractures. Various treatment options have been introduced for these fractures, with the choice of treatment typically depending on factors, such as the patient’s age, activity level, and preferences, as well as those of the surgeon. Despite the high incidence of distal radius fractures, there is still no consensus on the most effective treatment method for patients over 60 [25-29].
This study aimed to evaluate the short-term outcomes of closed reduction and pinning surgery in elderly patients with distal radius fractures, involving 113 participants. The results indicated that nine months post-surgery, most patients experienced good or excellent outcomes, with only a few reporting moderate or poor results. Two patients had poor outcomes due to complications, such as RSD and significant bone comminution. Among the six patients with moderate outcomes, some experienced issues, like dorsal tilt or osteoporosis.
In terms of functional outcomes, including wrist movement, the results were generally satisfactory. There was a significant positive correlation between wrist motion parameters—such as extension, flexion, supination, and pronation—and the DASH questionnaire score. This suggests that as wrist motion improved, functional outcomes also improved. Radiographic outcomes, including PT, RI, and RH, showed some decline over time; however, there were no significant differences between the stages of fracture stabilization and healing.
Although there was a reduction in some radiographic indicators, this did not negatively affect the functional outcomes, suggesting that patients were still able to use their operated hand effectively in daily activities. It was noted that while some loss of reduction occurred—particularly in terms of volar tilt—the overall radiographic parameters did not significantly impact treatment outcomes. Pain levels were low; most patients reported no pain nine months after surgery. Additionally, hand strength in the injured hand was similar to that of the uninjured hand in most patients, with no significant differences in grip strength.
The results of this study align with previous findings [19, 20, 22, 30, 31]. These studies show that closed reduction and pinning are effective treatments for distal radius fractures in elderly patients, providing good functional outcomes and low complication rates, thereby making it a reliable and cost-effective treatment option.
Conclusion
In conclusion, this study suggests that closed reduction and pinning are both effective and practical treatment options for distal radius fractures in elderly patients. These methods lead to good functional outcomes, acceptable radiographic results, and minimal complications. Additionally, it is recommended that BMD be assessed in elderly patients with osteoporosis to optimize treatment management.
Overall, this study demonstrated that closed reduction and pinning surgery results in good functional outcomes, adequate range of motion, and acceptable radiographic parameters in patients over 60 with distal radius fractures in the short term. Hand strength and wrist range of motion nine months post-surgery were similar to those of the healthy hand. Closed reduction and pinning are viable and effective options for treating distal radius fractures in patients over 60 and should be considered reliable methods for restoring both radiographic parameters and functional outcomes.
Strengths and weaknesses
Our study had some limitations that should be addressed. The main weakness was the lack of a comparison between the results of this surgical method and a control group treated with a different approach. Due to the design and objectives of the study, the follow-up period for patients was shorter than in other studies. A prospective study with a longer follow-up period could provide a more accurate assessment of the closed reduction and pinning in patients over 60 with distal radius fractures. Another limitation was that several surgeons carried out surgeries in the teaching hospital. A key strength of the current study was the assessment of functional outcomes, wrist range of motion, grip strength, radiographic parameters, and BMD in an appropriately sized sample of patients over 60 with distal radius fractures over the short term. Our study had some limitations that should be addressed. The main weakness was the lack of a comparison between the results of this surgical method and a control group treated with a different approach. Due to the design and objectives of the study, the follow-up period for patients was shorter than in other studies. A prospective study with a longer follow-up period could provide a more accurate assessment of closed reduction and pinning in patients over 60 with distal radius fractures. Another limitation was that several surgeons carried out surgeries in the teaching hospital. A key strength of the current study was the assessment of functional outcomes, wrist range of motion, grip strength, radiographic parameters, and BMD in an appropriately sized sample of patients over 60 with distal radius fractures over the short term.
Ethical Considerations
Compliance with ethical guidelines
Written informed consent was obtained from all participants. The research adhered to the principles of the Helsinki Convention and received approval from the Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1401.527). The patients incurred no additional costs or interventions.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors contributed equally to the conception and design of the study, data collection and analysis, interception of the results and drafting of the manuscript. Each author approved the final version of the manuscript for submission.
Conflict of interest
The authors declared no conflict of interest.
References
- Truong JL, Doherty C, Suh N. The effect of socioeconomic factors on outcomes of distal radius fractures: A systematic review. Hand. 2018; 13(5):509-15.[DOI:10.1177/1558944717735945] [PMID]
- Azad A, Kang HP, Alluri RK, Vakhshori V, Kay HF, Ghiassi A. Epidemiological and treatment trends of distal radius fractures across multiple age groups. J Wrist Surg. 2019; 8(4):305-311. [DOI:10.1055/s-0039-1685205] [PMID]
- Mauck BM, Swigler CW. Evidence-based review of distal radius fractures. Orthop Clin North Am. 2018; 49(2):211-22. [DOI:10.1016/j.ocl.2017.12.001] [PMID]
- Rundgren J, Bojan A, Mellstrand Navarro C, Enocson A. Epidemiology, classification, treatment and mortality of distal radius fractures in adults: An observational study of 23,394 fractures from the national Swedish fracture register. BMC Musculoskelet Disord. 2020; 21(1):88. [DOI:10.1186/s12891-020-3097-8] [PMID]
- Costa ML, Achten J, Parsons NR, Rangan A, Griffin D, Tubeuf S, et al. Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: Randomised controlled trial. BMJ. 2014; 349:g4807. [DOI:10.1136/bmj.g4807] [PMID]
- Melton LJ 3rd, Christen D, Riggs BL, Achenbach SJ, Müller R, van Lenthe GH, et al. Assessing forearm fracture risk in postmenopausal women. Osteoporos Int. 2010; 21(7):1161-9. [DOI:10.1007/s00198-009-1047-2] [PMID]
- Huetteman HE, Shauver MJ, Malay S, Chung TT, Chung KC. Variation in the Treatment of Distal Radius Fractures in the United States: 2010 to 2015. Plast Reconstr Surg. 2019; 143(1):159-67. [DOI:10.1097/PRS.0000000000005088] [PMID]
- Beumer A, McQueen MM. Fractures of the distal radius in low-demand elderly patients: Closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003; 74(1):98-100. [DOI:10.1080/00016470310013743] [PMID]
- Schousboe JT, Fink HA, Taylor BC, Stone KL, Hillier TA, Nevitt MC, et al. Association between self-reported prior wrist fractures and risk of subsequent hip and radiographic vertebral fractures in older women: A prospective study. J Bone Miner Res. 2005; 20(1):100-6. [DOI:10.1359/jbmr.2005.20.1.100] [PMID]
- Chhabra AB, Yildirim B. Adult distal radius fracture management. J Am Acad Orthop Surg. 2021; 29(22):e1105-16. [DOI:10.5435/JAAOS-D-20-01335] [PMID]
- Bacorn RW, Kurtzke JF. Colles'fracture: A study of two thousand cases from the New York State workmen's compensation board. JBJS. 1953; 35(3):643-58. [DOI:10.2106/00004623-195335030-00011]
- Campbell DA. Open reduction and internal fixation of intra articular and unstable fractures of the distal radius using the AO distal radius plate. J Hand Surg Br. 2000; 25(6):528-34. [DOI:10.1054/jhsb.2000.0485] [PMID]
- Kurup HV, Mandalia VM, Shaju KA, Singh B, Beaumont AR. Late collapse of distal radius fractures after K-wire removal: Is it significant? J Orthop Traumatol. 2008; 9(2):69-72. [DOI:10.1007/s10195-008-0005-7] [PMID]
- Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable colles type distal radius fractures in patients older than 70 years: Nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009; 23(4):237-42. [DOI:10.1097/BOT.0b013e31819b24e9] [PMID]
- Davis TR. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1987; 69(5):791. [DOI:10.2106/00004623-198769050-00027] [PMID]
- Batra S, Gupta A. The effect of fracture-related factors on the functional outcome at 1 year in distal radius fractures. Injury. 2002; 33(6):499-502. [DOI:10.1016/S0020-1383(01)00174-7] [PMID]
- Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J bone Joint Surg Am Vol. 1984; 66(7):1008-14. [DOI:10.2106/00004623-198466070-00006]
- Minegishi H, Dohi O, An S, Sato H. Treatment of unstable distal radius fractures with the volar locking plate. Ups J Med Sci. 2011; 116(4):280-4. [DOI:10.3109/03009734.2011.594183] [PMID]
- Glickel SZ, Catalano LW, Raia FJ, Barron OA, Grabow R, Chia B. Long-term outcomes of closed reduction and percutaneous pinning for the treatment of distal radius fractures. J Hand Surg Am. 2008; 33(10):1700-5. [DOI:10.1016/j.jhsa.2008.08.002] [PMID]
- Vasudevan PN, Lohith BM. Management of distal radius fractures - A new concept of closed reduction and standardised percutaneous 5-pin fixation. Trauma. 2017; 20(2):121-30. [DOI:10.1177/1460408617725104]
- Arora R, Gabl M, Erhart S, Schmidle G, Dallapozza C, Lutz M. Aspects of current management of distal radius fractures in the elderly individuals. Geriatr Orthop Surg Rehabil. 2011; 2(5-6):187-94. [DOI:10.1177/2151458511426874] [PMID]
- Testa G, Vescio A, Di Masi P, Bruno G, Sessa G, Pavone V. Comparison between surgical and conservative treatment for distal radius fractures in patients over 65 years. J Funct Morphol Kinesiol. 2019; 4(2):26. [DOI:10.3390/jfmk4020026] [PMID]
- Özkan S, Westenberg RF, Helliwell LA, Mudgal CS. Distal radius fractures: Evaluation of closed reduction and percutaneous kirschner wire pinning. J Hand Microsurg. 2018; 10(3):134-8. [DOI:10.1055/s-0038-1648334] [PMID]
- Mousavi SJ, Parnianpour M, Abedi M, Askary-Ashtiani A, Karimi A, Khorsandi A, et al. Cultural adaptation and validation of the Persian version of the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure. Clin Rehabil. 2008; 22:749‑57. [DOI:10.1177/0269215508085]
- MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016; 29(2):136-45. [DOI:10.1016/j.jht.2016.03.003] [PMID]
- Vannabouathong C, Hussain N, Guerra-Farfan E, Bhandari M. Interventions for distal radius fractures: A network meta-analysis of randomized trials. J Am Acad Orthop Surg. 2019; 27(13):e596-605. [DOI:10.5435/JAAOS-D-18-00424] [PMID]
- Gutiérrez-Espinoza H, Araya-Quintanilla F, Cuyul-Vásquez I, Gutiérrez-Monclus R, Reina-Gutiérrez S, Cavero-Redondo I, et al. Effectiveness and safety of different treatment modalities for patients older than 60 years with distal radius fracture: A network meta-analysis of clinical trials. Int J Environ Res Public Health. 2023; 20(4):3697. [DOI:10.3390/ijerph20043697] [PMID]
- Mulders MAM, Detering R, Rikli DA, Rosenwasser MP, Goslings JC, Schep NWL. Association between radiological and patient-reported outcome in adults with a displaced distal radius fracture: A systematic review and meta-analysis. J Hand Surg Am. 2018; 43(8):710-719.e5. [DOI:10.1016/j.jhsa.2018.05.003] [PMID]
- Gutiérrez-Monclus R, Gutiérrez-Espinoza H, Zavala-González J, Olguín-Huerta C, Rubio-Oyarzún D, Araya-Quintanilla F. Correlation between radiological parameters and functional outcomes in patients older than 60 years of age with distal radius fracture. Hand. 2019;14(6):770-5. [DOI:10.1177/1558944718770203] [PMID]
- Cherubino P, Bini A, Marcolli D. Management of distal radius fractures: Treatment protocol and functional results. Injury. 2010; 41(11):1120-6. [DOI:10.1016/j.injury.2010.09.016] [PMID]
- Júnior A, Bufáiçal H, Freitas A, Chaves A. Distal radius fractures: Long term functional and radiological results of percutaneous pinning fixation. Revista Bras Ortop. 2012; 47:31-6. [DOI:10.1590/S0102-36162012000100004]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2023/08/29 | Accepted: 2023/11/29 | Published: 2024/02/1
Received: 2023/08/29 | Accepted: 2023/11/29 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |