Volume 11, Issue 2 (May 2024)
JROS 2024, 11(2): 107-114 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sobhani A, Seifi Ashkezari A, Fathi A. Radiographic and Functional Outcomes of Tibial Fixation in Patients With Tibiofibular Fractures. JROS 2024; 11 (2) :107-114
URL: http://jros.iums.ac.ir/article-1-2281-en.html
URL: http://jros.iums.ac.ir/article-1-2281-en.html
1- Department of Orthopaedics Surgery, Rasoul Akram Hospital, Iran University of Medical Sciences, Tehran, Iran.
2- School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 584 kb]
(172 Downloads)
| Abstract (HTML) (538 Views)
Full-Text: (197 Views)
Introduction
Simultaneous fractures of the tibia and fibula represent the most prevalent type of diaphyseal fractures among long bones. These injuries typically result from high-energy trauma, such as vehicular accidents, or from low-energy twisting mechanisms [1, 2]. In contemporary society, the proliferation of transportation networks and the escalation of vehicle speeds have contributed to a rising incidence of these fractures [3, 4].
Fractures of the distal tibia constitute 37.8% of all tibial fractures [5]. The etiology of these fractures is often attributed to axial or rotational forces applied to the lower extremity [6, 7]. Complications associated with tibial fractures may include delayed healing or non:union: of the fracture. The management of distal tibia fractures frequently presents a significant challenge, with a notable incidence of adverse outcomes and complications [8, 9].
Various treatment modalities exist for tibial fractures, such as external fixation, intramedullary nailing (IMN), and plating [10]. Among these, IMN is frequently employed due to its ability to maintain extraosseous blood circulation, facilitate weight-bearing, and minimize soft tissue injury [11].
Biomechanical research indicates that while IMN decreases axial weight-bearing capacity, it does not significantly differ from plating in terms of torsional stability [12]. Furthermore, comparative studies reveal that the rates of complications such as infection, mal:union:, non:union:, and the need for reoperation are comparable between IMN and plating. Nonetheless, a notable increase in malalignment has been associated with IMN [13].
IMN is particularly advocated for distal tibial fractures, as it reduces soft tissue trauma and enables patients to bear weight on the injured limb to the greatest extent possible. Overall, IMN is a prevalent approach for managing long bone fractures, offering substantial biological and biomechanical advantages. It is often regarded as the gold standard for treating closed fractures of the femur, tibia, and humeral shaft [14]. The benefits of IMN include expedited healing, a lower incidence of complications, and reduced risks of poor :union: and refracture [15, 16].
The management of tibiofibular fractures that do not extend to the articular surface has remained a subject of debate. IMN, open reduction, and internal fixation utilizing plate application have been recognized as viable treatment options. The primary objectives of these interventions are to achieve :union:, maintain appropriate bone length, ensure alignment, and restore function [17].
Epidemiological data indicate that 77.7% of fibular fractures occur concurrently with tibial fractures. The concept of fibular fixation as a supplementary treatment for fractures of both the tibia and fibula was initially introduced by Morrison et al. [18].
Numerous studies have explored the significance of fibular fixation in the context of tibiofibular fractures. These investigations suggest that fibular fixation plays a crucial role in preventing displacement of the tibial fracture [19]. Additionally, other research has indicated that correct plate positioning in fibular fractures enhances alignment [20].
Conversely, some studies have reported that fibular fixation may result in delayed or non:union:, as it can alleviate pressure on the fracture site and hinder the healing process [21]. Furthermore, the implementation of open reduction and internal fixation of the fibula has been associated with an increased incidence of wound complications [22].
The uncertain significance of tibial fixation in managing concurrent tibiofibular fractures, coupled with the epidemiological relevance of this matter, prompted us to undertake this study. Our objective was to examine the radiographic and functional results of patients with tibiofibular fractures who received tibial fixation exclusively at Rasoul Akram Hospital, Tehran, Iran. This research aims to contribute to a deeper understanding of the underlying pathophysiology and to enhance patient quality of life through more effective treatment strategies.
Methods
This retrospective cohort study was initiated after obtaining the necessary permits from the Ethics Committee of Iran University of Medical Sciences. The inclusion criteria for entering the study were as follows: Patients with tibiofibular fractures who underwent tibial fixation, referred to Rasoul Akram Hospital between 2017 and 2022, had reached skeletal maturity, and had been treated with an IMN for less than 2 weeks since the fracture. Patients with pathological fracture, refracture, physical injury, soft tissue or vascular damage, treated with a plate or an external fixator, were excluded from the study.
After selection of patients based on the inclusion and exclusion criteria, we reviewed the patients’ files and radiographic information. The information was recorded in a pre-designed checklist based on the study variables. Information, including age, gender, underlying diseases, radiographic results based on the radiographic :union: scale in tibial (RUST), and functional results based on the American Orthopedic Foot and Ankle Society (AOFAS) score, was recorded in the patient checklist after the fracture. The patient’s radiographs were examined and compared before surgery, 6 months later, and 12 months later.
The degree of tibial :union: after the fracture was measured by the RUST. In general, the degree of tibial :union: was classified based on the formation of callus of the cortices of the two fractured parts of the tibia towards each other and the visibility of the fracture line. The minimum RUST score is 4, and the maximum score is 12. A score of 4 means that the fracture has not healed, and a score of 12 means that a callus has formed at the fracture site and the fracture line is not visible.
The degree of patient function after surgery was measured by the AOFAS score. The score consists of 42 questions covering 5 domains: Pain (9 questions), daily activities (17 questions), sports activities (5 questions), 4) foot and ankle quality of life (4 questions), and other symptoms such as stiffness, edema, and range of motion (7 questions). For each question, there are five options, each scored on a Likert scale ranging from 0 (never) to 4 (always). The total score of the AOFAS ranges from 0 to 100, with 0 indicating the worst outcomes and 100 indicating the best outcomes. The validity and reliability of the Persian version of this questionnaire were examined and reported to be 0.92 and 0.7, respectively [23].
Finally, the collected information was entered into SPSS software, version 26 for statistical analysis. The qualitative variables were provided using frequency and percentage indicators, while quantitative variables were presented using Mean±SD indicators. The normality of the data was evaluated using the Kolmogorov-Smirnov test. To measure the relationship between the variables, if the data distribution was normal, parametric tests were used; otherwise, the corresponding non-parametric tests were employed. Results with a P<0.05 were considered significant.
Results
This study examined 75 patients with tibiofibular fractures who underwent tibial fixation at Rasoul Akram Hospital between 2017 and 2022. In terms of gender distribution, 57 patients (76.0%) were male and 18(24.0%) were female. The mean age of the patients was 35.60±11.09 years. Thirty-three patients (44.0%) were younger than 35 years, and 42(56.0%) were older than 35 years. Thirty-one patients (41.3%) were smokers. Fourteen patients (18.7%) had diabetes, 13(17.3%) had hypertension, and 3(4.0%) had chronic kidney disease.
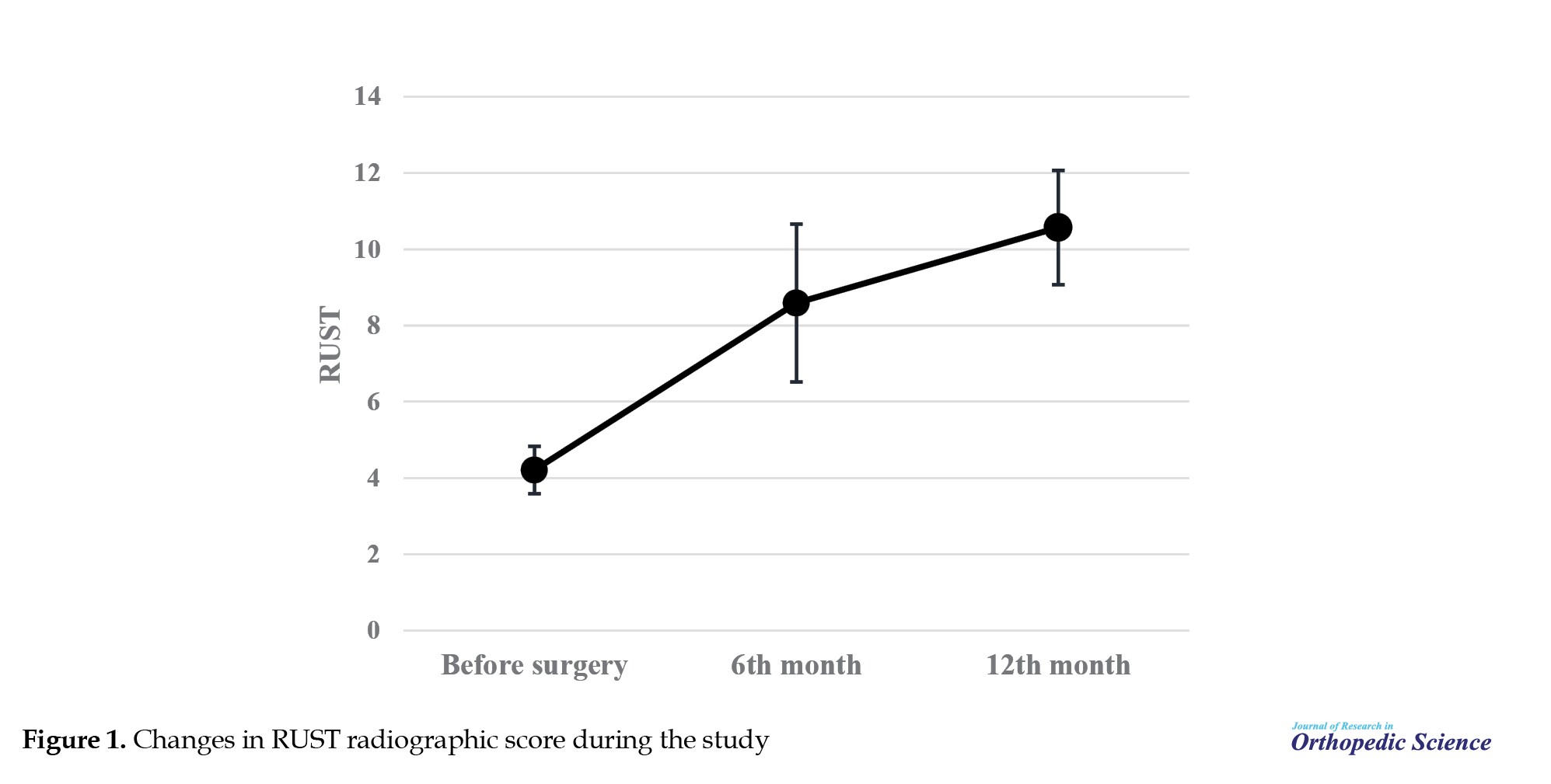
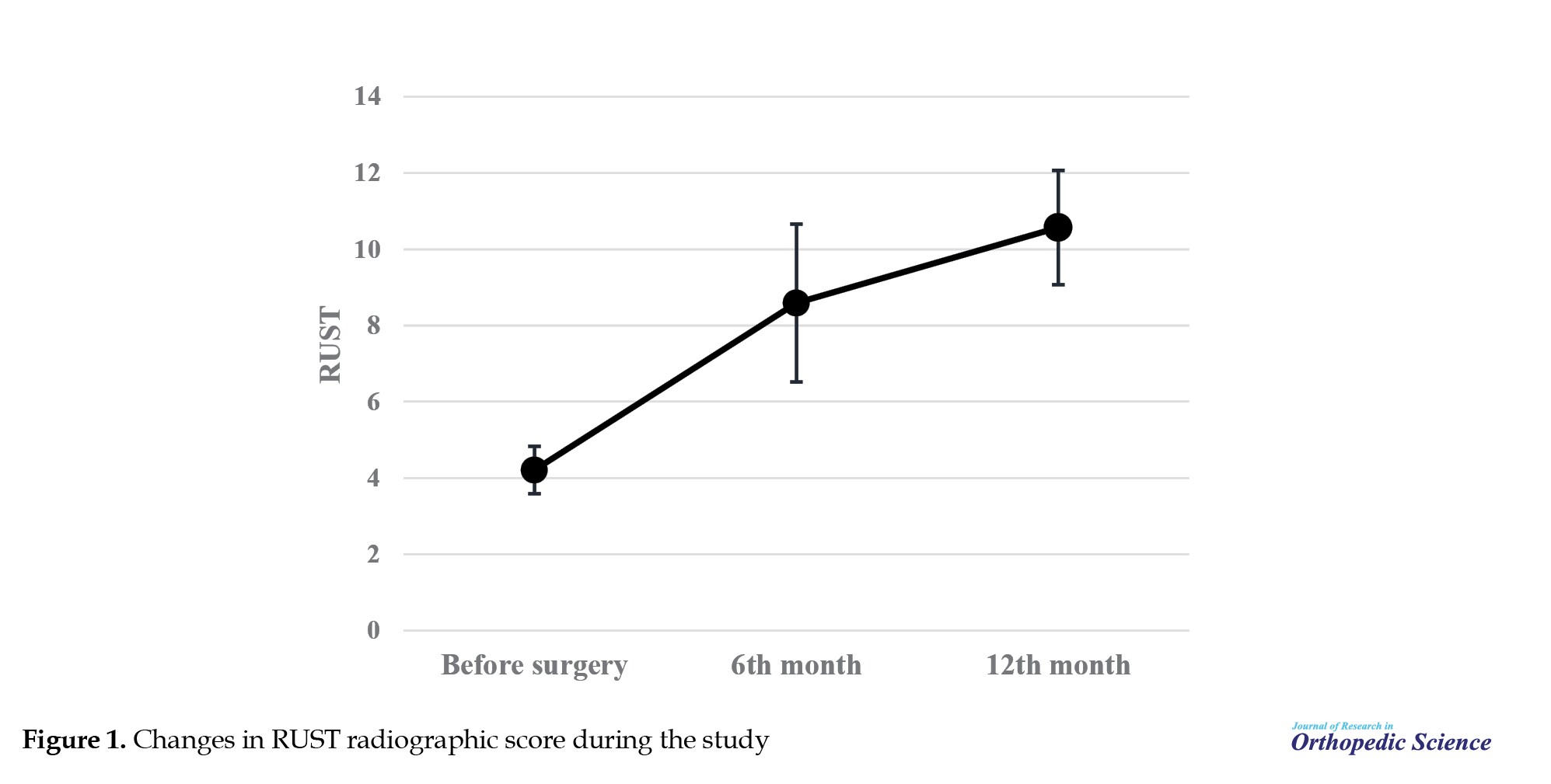
In the study of changes in the radiographic RUST score during the study, the mean RUST score increased from 4.21±0.62 at the beginning of the study to 8.59±2.07 at the sixth month and then to 10.57±1.50 at the 12th month, which was statistically significant (P<0.001) (Figure 1).
In the study, the mean AOFAS score was calculated to be 77.21±9.41 on the patients’ functional scale.
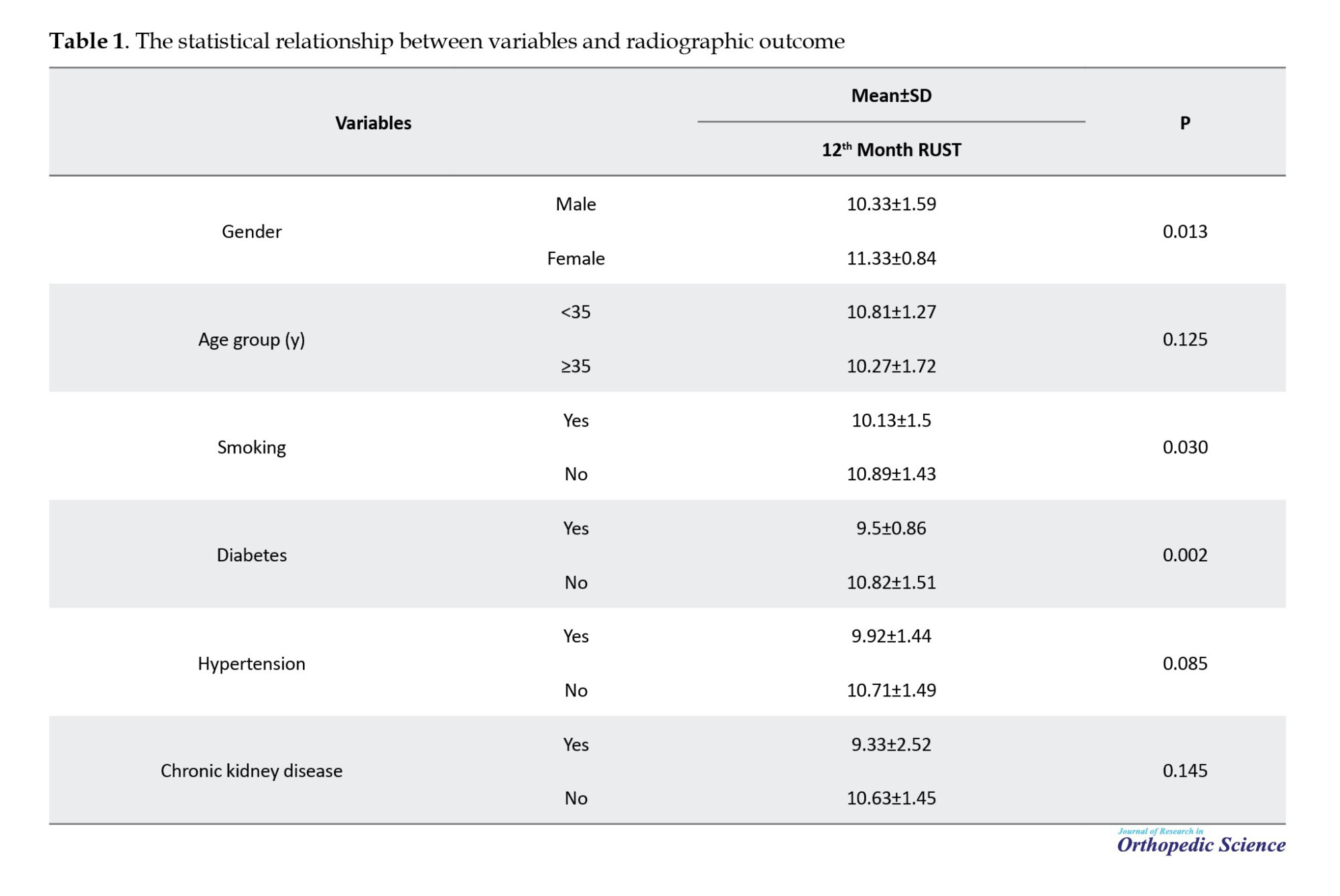
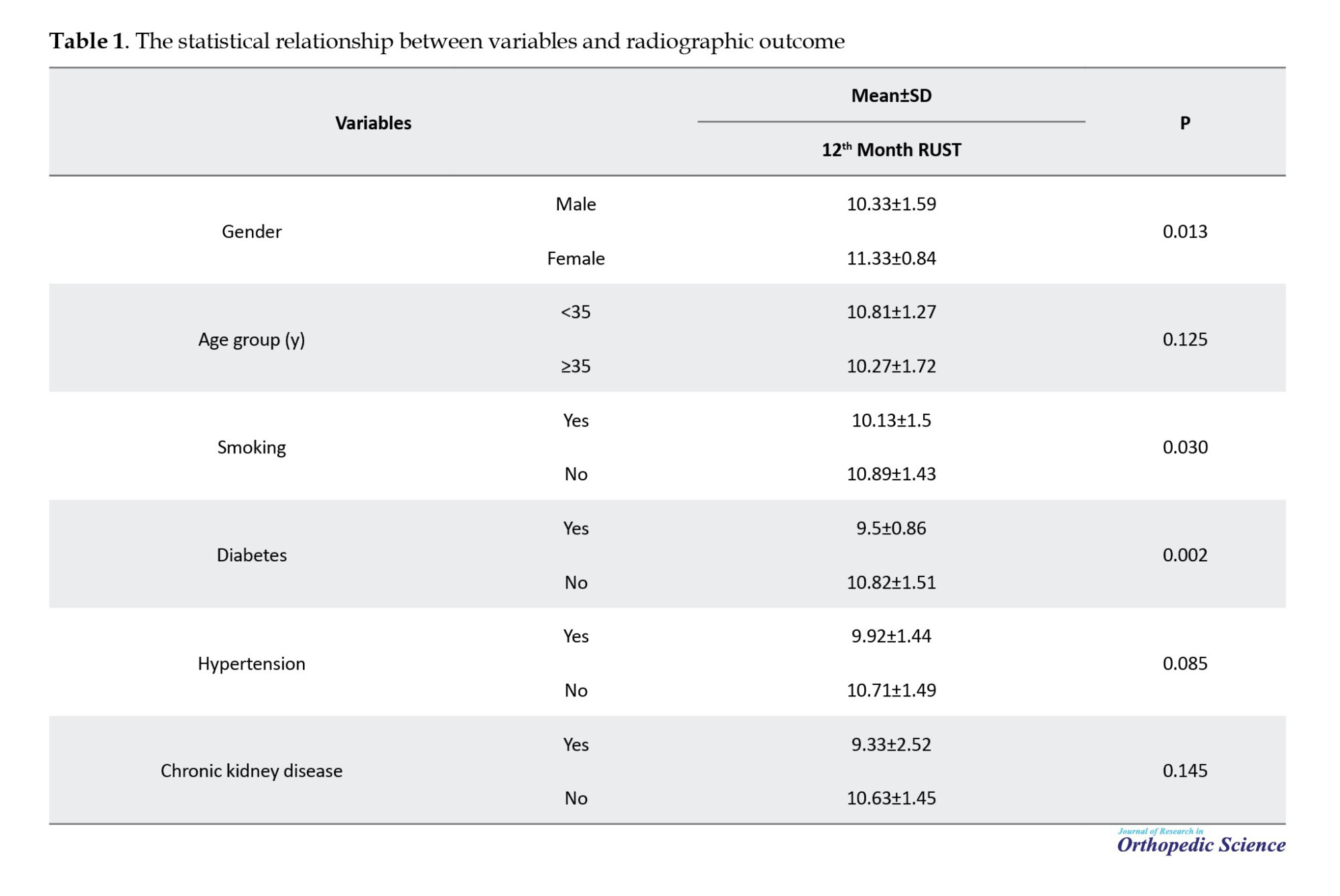
In examining the association between variables and radiographic outcome, a statistically significant association was observed between gender, smoking, and diabetes with 12th month RUST (P<0.05); such that 12th month RUST was significantly lower in men (10.33±1.59 vs 11.33±0.84; P=0.013), smokers (10.13±1.50 vs 10.89±1.43; P=0.030), and diabetics (50.9±0.86 vs 10.82±1.51; P=0.002). Therefore, male gender, smoking, and diabetes were the three factors associated with poorer radiographic outcomes. While there was no statistically significant relationship between age group, hypertension, and chronic kidney disease with radiographic outcome (P>0.05) (Table 1).
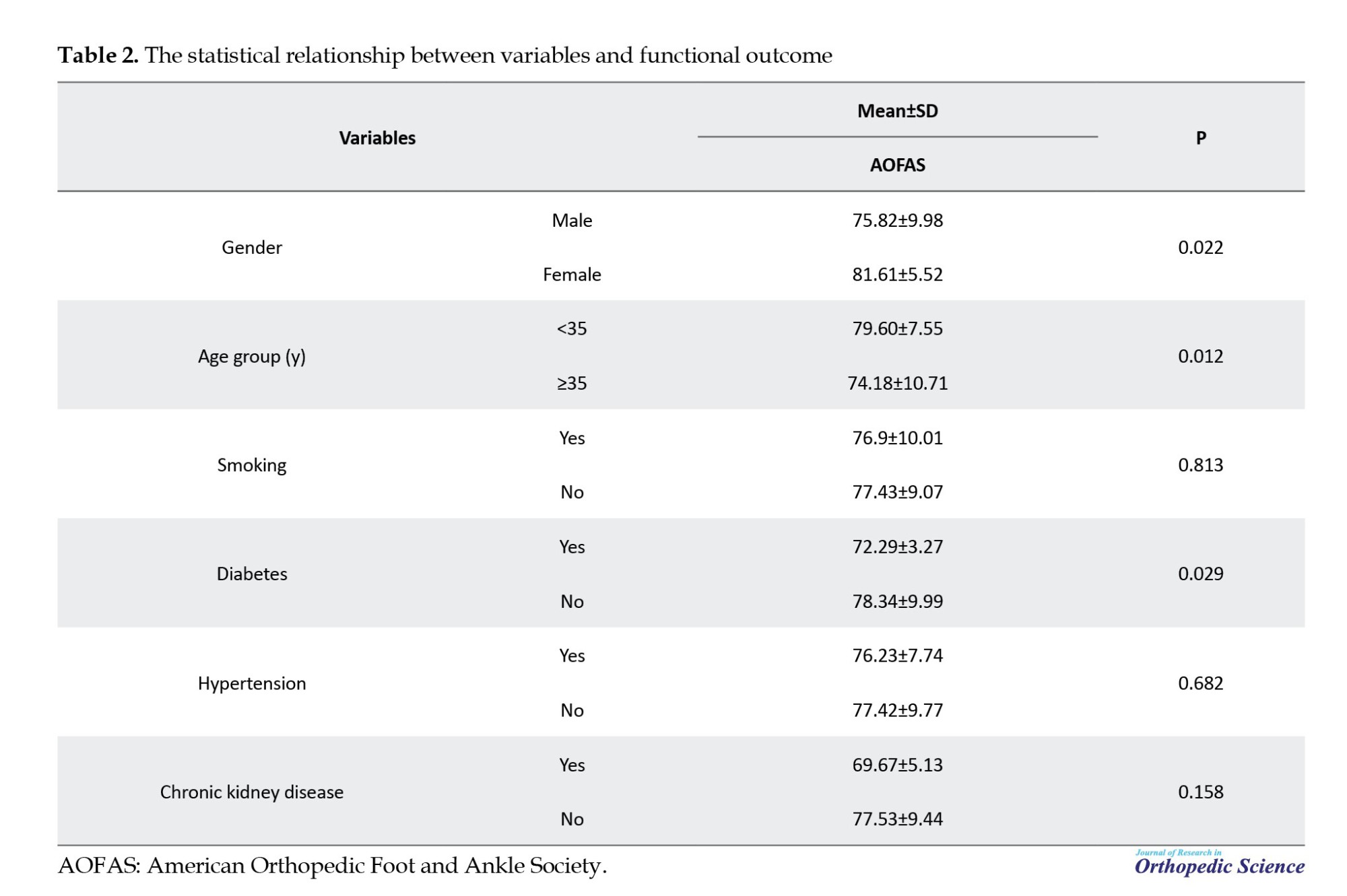
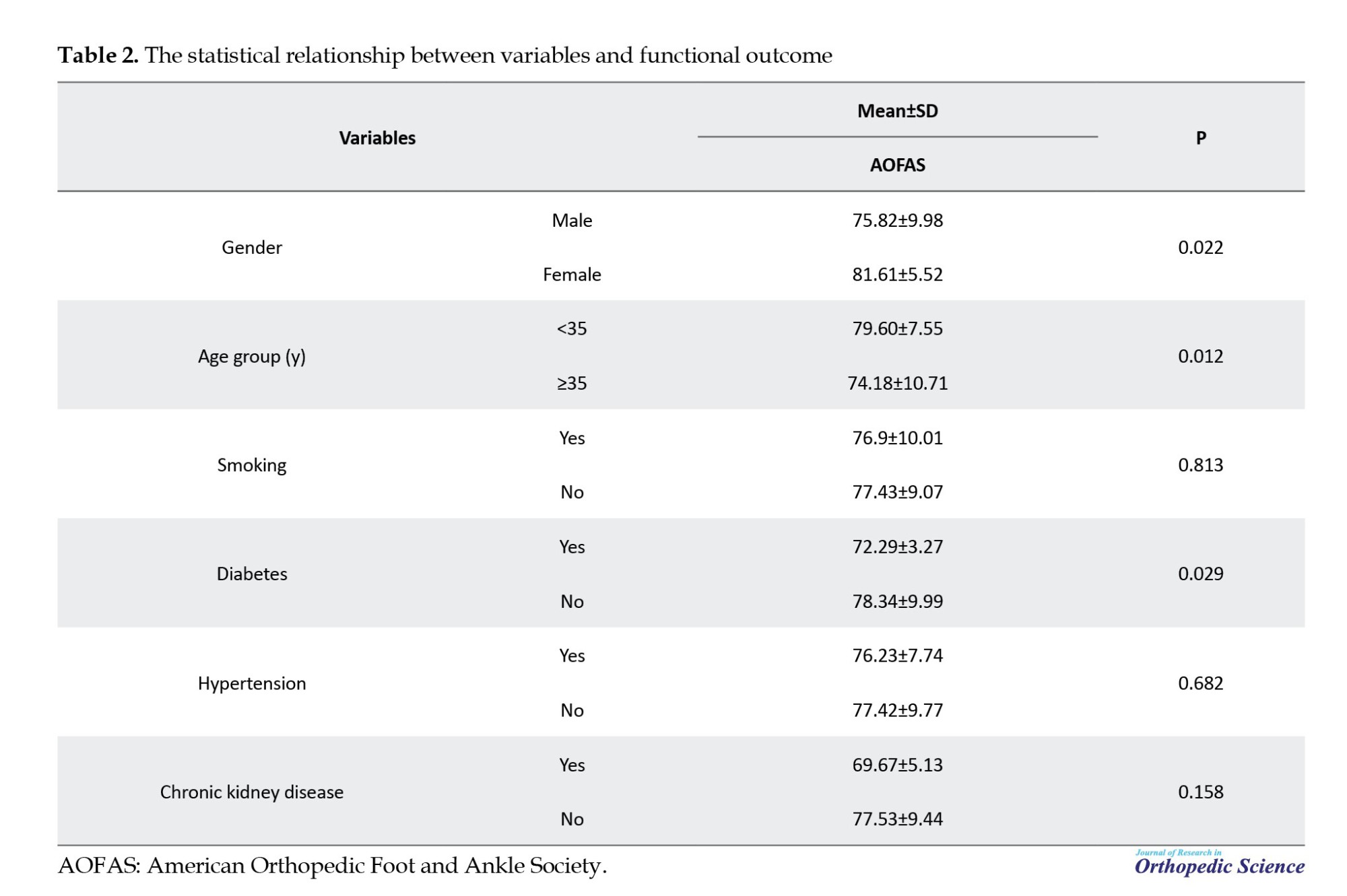
In examining the association between variables with functional outcome, a statistically significant association was seen between gender, age group, and diabetes with AOFAS (P<0.05); AOFAS was significantly lower in men (75.82±9.98 vs 81.61±5.52; P=0.022), patients aged 35 years or older (74.18±10.71 vs 79.60±7.55; P=0.012), and patients with diabetes (72.29±3.27 vs 78.34±9.99; P=0.029). Therefore, male gender, older age, and diabetes were the three factors associated with poorer functional outcomes. While there was no statistically significant relationship between smoking, hypertension, and chronic kidney disease with functional outcome (P>0.05) (Table 2).
Discussion
The unclear implications of tibial fixation in the treatment of simultaneous tibiofibular fractures, along with the epidemiological importance of this issue, led us to conduct this study. Our goal was to analyze the radiographic and functional outcomes of patients with tibiofibular fractures who underwent tibial fixation solely at Rasoul Akram Hospital. This research seeks to provide insights into the fundamental pathophysiology and to improve the quality of life by developing more effective treatment approaches.
The findings of the current study indicate that tibial fixation, as a standalone intervention for patients with tibiofibular fractures, yields satisfactory radiological and functional results. Male gender, smoking, and diabetes were three factors associated with poorer radiographic outcomes, and male gender, older age, and diabetes were three factors associated with poorer functional outcomes. Identifying risk factors associated with a poorer prognosis in patients could help select the most appropriate treatment option for each patient and allocate treatment resources according to patient needs. Future studies could also focus on known risk factors and compare tibial fixation alone with other treatment methods in the group with poorer outcomes.
Compared with other studies, Torkaman et al. conducted a cross-sectional study in Tehran City, Iran, in 2016 to investigate the outcomes of distal tibiofibular fractures treated with IMN alone. Therefore, 40 patients with distal tibiofibular fractures who were candidates for IMN surgery were included in the study. The mean duration of complete :union: was 6.34 months. Fourteen patients had mal:union:. No deep infections, compartment syndromes, or nerve injuries were observed in any of the patients. Therefore, they concluded from this study that the IMN method is a suitable method with a high :union: rate and a low complication rate [24].
In the study of fibular fixation, Rouhani et al. conducted a clinical trial in Tabriz City, Iran, in 2012 to investigate the role of fibular fixation in treating distal one-third tibia fractures. Therefore, 53 patients with simultaneous fibular and tibia fractures were included in the study and divided into two groups. In the first group, fibular fixation was performed, but in the second group, it was not. Overall, 7 patients developed malalignment, 6 of whom were in the control group. In the case group, no cases of non:union: were observed, but in the control group, three patients developed this complication [25]. What is important is a comparative study of these treatment methods with one another, which has not been investigated. It is suggested that different treatment options for simultaneous tibia and fibula fractures be explored in future studies.
Future studies could compare tibial fixation alone with other treatments in patients with poorer treatment outcomes, focusing on known risk factors. Additionally, applying the results of this study in clinical practice may lead to an improvement in patients’ quality of life.
Conclusion
Tibial fixation as a standalone intervention has demonstrated satisfactory radiological and functional results in the treatment of patients with tibiofibular fractures. The presence of male gender, smoking habits, and diabetes emerged as three significant factors linked to poor radiographic outcomes. In contrast, male gender, advanced age, and diabetes were identified as three determinants associated with diminished functional outcomes. Recognizing the risk factors associated with adverse prognoses in patients can facilitate the selection of the most suitable treatment strategies for individual cases and enable the allocation of treatment resources according to each patient’s specific needs.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committees of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1402.470).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: AliAkbar Seifi Ashkezari and Amin Fathi; Study design and writing the original draft: AliAkbar Seifi Ashkezari; Data analysis and statistical analysis: Amin Fathi; Supervision, review and editing: Amir Sobhani.
Conflict of interest
The authors declared no conflict of interest.
References
Simultaneous fractures of the tibia and fibula represent the most prevalent type of diaphyseal fractures among long bones. These injuries typically result from high-energy trauma, such as vehicular accidents, or from low-energy twisting mechanisms [1, 2]. In contemporary society, the proliferation of transportation networks and the escalation of vehicle speeds have contributed to a rising incidence of these fractures [3, 4].
Fractures of the distal tibia constitute 37.8% of all tibial fractures [5]. The etiology of these fractures is often attributed to axial or rotational forces applied to the lower extremity [6, 7]. Complications associated with tibial fractures may include delayed healing or non:union: of the fracture. The management of distal tibia fractures frequently presents a significant challenge, with a notable incidence of adverse outcomes and complications [8, 9].
Various treatment modalities exist for tibial fractures, such as external fixation, intramedullary nailing (IMN), and plating [10]. Among these, IMN is frequently employed due to its ability to maintain extraosseous blood circulation, facilitate weight-bearing, and minimize soft tissue injury [11].
Biomechanical research indicates that while IMN decreases axial weight-bearing capacity, it does not significantly differ from plating in terms of torsional stability [12]. Furthermore, comparative studies reveal that the rates of complications such as infection, mal:union:, non:union:, and the need for reoperation are comparable between IMN and plating. Nonetheless, a notable increase in malalignment has been associated with IMN [13].
IMN is particularly advocated for distal tibial fractures, as it reduces soft tissue trauma and enables patients to bear weight on the injured limb to the greatest extent possible. Overall, IMN is a prevalent approach for managing long bone fractures, offering substantial biological and biomechanical advantages. It is often regarded as the gold standard for treating closed fractures of the femur, tibia, and humeral shaft [14]. The benefits of IMN include expedited healing, a lower incidence of complications, and reduced risks of poor :union: and refracture [15, 16].
The management of tibiofibular fractures that do not extend to the articular surface has remained a subject of debate. IMN, open reduction, and internal fixation utilizing plate application have been recognized as viable treatment options. The primary objectives of these interventions are to achieve :union:, maintain appropriate bone length, ensure alignment, and restore function [17].
Epidemiological data indicate that 77.7% of fibular fractures occur concurrently with tibial fractures. The concept of fibular fixation as a supplementary treatment for fractures of both the tibia and fibula was initially introduced by Morrison et al. [18].
Numerous studies have explored the significance of fibular fixation in the context of tibiofibular fractures. These investigations suggest that fibular fixation plays a crucial role in preventing displacement of the tibial fracture [19]. Additionally, other research has indicated that correct plate positioning in fibular fractures enhances alignment [20].
Conversely, some studies have reported that fibular fixation may result in delayed or non:union:, as it can alleviate pressure on the fracture site and hinder the healing process [21]. Furthermore, the implementation of open reduction and internal fixation of the fibula has been associated with an increased incidence of wound complications [22].
The uncertain significance of tibial fixation in managing concurrent tibiofibular fractures, coupled with the epidemiological relevance of this matter, prompted us to undertake this study. Our objective was to examine the radiographic and functional results of patients with tibiofibular fractures who received tibial fixation exclusively at Rasoul Akram Hospital, Tehran, Iran. This research aims to contribute to a deeper understanding of the underlying pathophysiology and to enhance patient quality of life through more effective treatment strategies.
Methods
This retrospective cohort study was initiated after obtaining the necessary permits from the Ethics Committee of Iran University of Medical Sciences. The inclusion criteria for entering the study were as follows: Patients with tibiofibular fractures who underwent tibial fixation, referred to Rasoul Akram Hospital between 2017 and 2022, had reached skeletal maturity, and had been treated with an IMN for less than 2 weeks since the fracture. Patients with pathological fracture, refracture, physical injury, soft tissue or vascular damage, treated with a plate or an external fixator, were excluded from the study.
After selection of patients based on the inclusion and exclusion criteria, we reviewed the patients’ files and radiographic information. The information was recorded in a pre-designed checklist based on the study variables. Information, including age, gender, underlying diseases, radiographic results based on the radiographic :union: scale in tibial (RUST), and functional results based on the American Orthopedic Foot and Ankle Society (AOFAS) score, was recorded in the patient checklist after the fracture. The patient’s radiographs were examined and compared before surgery, 6 months later, and 12 months later.
The degree of tibial :union: after the fracture was measured by the RUST. In general, the degree of tibial :union: was classified based on the formation of callus of the cortices of the two fractured parts of the tibia towards each other and the visibility of the fracture line. The minimum RUST score is 4, and the maximum score is 12. A score of 4 means that the fracture has not healed, and a score of 12 means that a callus has formed at the fracture site and the fracture line is not visible.
The degree of patient function after surgery was measured by the AOFAS score. The score consists of 42 questions covering 5 domains: Pain (9 questions), daily activities (17 questions), sports activities (5 questions), 4) foot and ankle quality of life (4 questions), and other symptoms such as stiffness, edema, and range of motion (7 questions). For each question, there are five options, each scored on a Likert scale ranging from 0 (never) to 4 (always). The total score of the AOFAS ranges from 0 to 100, with 0 indicating the worst outcomes and 100 indicating the best outcomes. The validity and reliability of the Persian version of this questionnaire were examined and reported to be 0.92 and 0.7, respectively [23].
Finally, the collected information was entered into SPSS software, version 26 for statistical analysis. The qualitative variables were provided using frequency and percentage indicators, while quantitative variables were presented using Mean±SD indicators. The normality of the data was evaluated using the Kolmogorov-Smirnov test. To measure the relationship between the variables, if the data distribution was normal, parametric tests were used; otherwise, the corresponding non-parametric tests were employed. Results with a P<0.05 were considered significant.
Results
This study examined 75 patients with tibiofibular fractures who underwent tibial fixation at Rasoul Akram Hospital between 2017 and 2022. In terms of gender distribution, 57 patients (76.0%) were male and 18(24.0%) were female. The mean age of the patients was 35.60±11.09 years. Thirty-three patients (44.0%) were younger than 35 years, and 42(56.0%) were older than 35 years. Thirty-one patients (41.3%) were smokers. Fourteen patients (18.7%) had diabetes, 13(17.3%) had hypertension, and 3(4.0%) had chronic kidney disease.
In the study of changes in the radiographic RUST score during the study, the mean RUST score increased from 4.21±0.62 at the beginning of the study to 8.59±2.07 at the sixth month and then to 10.57±1.50 at the 12th month, which was statistically significant (P<0.001) (Figure 1).
In the study, the mean AOFAS score was calculated to be 77.21±9.41 on the patients’ functional scale.
In examining the association between variables and radiographic outcome, a statistically significant association was observed between gender, smoking, and diabetes with 12th month RUST (P<0.05); such that 12th month RUST was significantly lower in men (10.33±1.59 vs 11.33±0.84; P=0.013), smokers (10.13±1.50 vs 10.89±1.43; P=0.030), and diabetics (50.9±0.86 vs 10.82±1.51; P=0.002). Therefore, male gender, smoking, and diabetes were the three factors associated with poorer radiographic outcomes. While there was no statistically significant relationship between age group, hypertension, and chronic kidney disease with radiographic outcome (P>0.05) (Table 1).
In examining the association between variables with functional outcome, a statistically significant association was seen between gender, age group, and diabetes with AOFAS (P<0.05); AOFAS was significantly lower in men (75.82±9.98 vs 81.61±5.52; P=0.022), patients aged 35 years or older (74.18±10.71 vs 79.60±7.55; P=0.012), and patients with diabetes (72.29±3.27 vs 78.34±9.99; P=0.029). Therefore, male gender, older age, and diabetes were the three factors associated with poorer functional outcomes. While there was no statistically significant relationship between smoking, hypertension, and chronic kidney disease with functional outcome (P>0.05) (Table 2).
Discussion
The unclear implications of tibial fixation in the treatment of simultaneous tibiofibular fractures, along with the epidemiological importance of this issue, led us to conduct this study. Our goal was to analyze the radiographic and functional outcomes of patients with tibiofibular fractures who underwent tibial fixation solely at Rasoul Akram Hospital. This research seeks to provide insights into the fundamental pathophysiology and to improve the quality of life by developing more effective treatment approaches.
The findings of the current study indicate that tibial fixation, as a standalone intervention for patients with tibiofibular fractures, yields satisfactory radiological and functional results. Male gender, smoking, and diabetes were three factors associated with poorer radiographic outcomes, and male gender, older age, and diabetes were three factors associated with poorer functional outcomes. Identifying risk factors associated with a poorer prognosis in patients could help select the most appropriate treatment option for each patient and allocate treatment resources according to patient needs. Future studies could also focus on known risk factors and compare tibial fixation alone with other treatment methods in the group with poorer outcomes.
Compared with other studies, Torkaman et al. conducted a cross-sectional study in Tehran City, Iran, in 2016 to investigate the outcomes of distal tibiofibular fractures treated with IMN alone. Therefore, 40 patients with distal tibiofibular fractures who were candidates for IMN surgery were included in the study. The mean duration of complete :union: was 6.34 months. Fourteen patients had mal:union:. No deep infections, compartment syndromes, or nerve injuries were observed in any of the patients. Therefore, they concluded from this study that the IMN method is a suitable method with a high :union: rate and a low complication rate [24].
In the study of fibular fixation, Rouhani et al. conducted a clinical trial in Tabriz City, Iran, in 2012 to investigate the role of fibular fixation in treating distal one-third tibia fractures. Therefore, 53 patients with simultaneous fibular and tibia fractures were included in the study and divided into two groups. In the first group, fibular fixation was performed, but in the second group, it was not. Overall, 7 patients developed malalignment, 6 of whom were in the control group. In the case group, no cases of non:union: were observed, but in the control group, three patients developed this complication [25]. What is important is a comparative study of these treatment methods with one another, which has not been investigated. It is suggested that different treatment options for simultaneous tibia and fibula fractures be explored in future studies.
Future studies could compare tibial fixation alone with other treatments in patients with poorer treatment outcomes, focusing on known risk factors. Additionally, applying the results of this study in clinical practice may lead to an improvement in patients’ quality of life.
Conclusion
Tibial fixation as a standalone intervention has demonstrated satisfactory radiological and functional results in the treatment of patients with tibiofibular fractures. The presence of male gender, smoking habits, and diabetes emerged as three significant factors linked to poor radiographic outcomes. In contrast, male gender, advanced age, and diabetes were identified as three determinants associated with diminished functional outcomes. Recognizing the risk factors associated with adverse prognoses in patients can facilitate the selection of the most suitable treatment strategies for individual cases and enable the allocation of treatment resources according to each patient’s specific needs.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethics Committees of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.FMD.REC.1402.470).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Data collection: AliAkbar Seifi Ashkezari and Amin Fathi; Study design and writing the original draft: AliAkbar Seifi Ashkezari; Data analysis and statistical analysis: Amin Fathi; Supervision, review and editing: Amir Sobhani.
Conflict of interest
The authors declared no conflict of interest.
References
- Wang Z, Tan Z, Wang Y, Chen W, Hou Z, Zhang Q, et al. Incidence and risk factors of occult posterior malleolar fracture in patients with spiral distal tibial fracture: Reexamination and analysis. Asian J Surg. 2022; 45(7):1389-95. [DOI:10.1016/j.asjsur.2021.09.042] [PMID]
- Peng J, Long X, Fan J, Chen S, Li Y, Wang W. Concomitant distal tibia-fibula fractures treated with intramedullary nailing, with or without fibular fixation: A meta-analysis. J Foot Ankle Surg. 2021; 60(1):109-13. [DOI:10.1053/j.jfas.2020.05.006] [PMID]
- Podeszwa DA, Mubarak SJ. Physeal fractures of the distal tibia and fibula (Salter-Harris Type I, II, III, and IV fractures). J Pediatr Orthop. 2012; 32(Suppl 1):S62-8. [DOI:10.1097/BPO.0b013e318254c7e5] [PMID]
- Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, et al. Risk factors for proximal humerus fracture. Am J Epidemiol. 2004; 160(4):360-7. [DOI:10.1093/aje/kwh224] [PMID]
- Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM. The epidemiology of open fractures in adults. A 15-year review. Injury. 2012; 43(6):891-7.[DOI:10.1016/j.injury.2011.12.007] [PMID]
- Chaichankul C, Chaichankul C. Fracture motion in distal tibial rodding: Effect of obliquity, load, and locking screw pattern. J Med Assoc Thai. 100(12): 1274-82. [Link]
- Barei DP, Nork SE. Fractures of the tibial plafond. Foot Ankle Clin. 2008; 13(4):571-91. [DOI:10.1016/j.fcl.2008.09.002]
- Egol KA, Weisz R, Hiebert R, Tejwani NC, Koval KJ, Sanders RW. Does fibular plating improve alignment after intramedullary nailing of distal metaphyseal tibia fractures? J Orthop Trauma. 2006; 20(2):94-103. [DOI:10.1097/01.bot.0000199118.61229.70] [PMID]
- Shah K, Quaimkhani S. Long-term outcome after tibial shaft fracture: is mal:union: important?. J Bone Joint Surg Am. 2004; 86(2):436; author reply 436-7. [PMID]
- Germann CA, Perron AD, Sweeney TW, Miller MD, Brady WJ. Orthopedic pitfalls in the ED: Tibial plafond fractures. Am J Emerg Med. 2005; 23(3):357-62. [DOI:10.1016/j.ajem.2004.01.002]
- Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Jt Surg. 2005; 87(6):1213-21. [DOI:10.2106/00004623-200506000-00005]
- Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011; 25(12):736-41. [DOI:10.1097/BOT.0b013e318213f709] [PMID]
- Kuhn S, Greenfield J, Arand C, Jarmolaew A, Appelmann P, Mehler D, et al. Treatment of distal intraarticular tibial fractures: A biomechanical evaluation of intramedullary nailing vs. angle-stable plate osteosynthesis. Injury. 2015; 46(Supplement 4):S99-103. [DOI:10.1016/S0020-1383(15)30026-7]
- Morshed S, Humphrey M, Corrales LA, Millett M, Hoffinger SA. Retention of flexible intramedullary nails following treatment of pediatric femur fractures. Arch Orthop Trauma Surg. 2007; 127:509-14. [DOI:10.1007/s00402-007-0286-y]
- Hutchins CM, Sponseller PD, Sturm P, Mosquero R. Open femur fractures in children: Treatment, complications, and results. J Pediatr Orthop. 2000;2 0(2):183-8. [DOI:10.1097/01241398-200003000-00010] [PMID]
- Yeganeh A, Mahmodi M, Farahini H, Moghtadaei M. Short-term outcomes of induced membrane technique in treatment of long bone defects in Iran. Med Arch. 2016; 70(4):284-7. [DOI:10.5455/medarh.2016.70.284-287] [PMID]
- Sah RK, Akhtar M, Din IM, Nadeem RD, Muhibi AS. Comparative study of effectiveness of rush pin with long arm cast and dynamic compression plate in management of closed diaphyseal fracture of radius and ulna in adults. J Pak Med Assoc. 2019; 69(10):1431-6. [PMID]
- Morrison KM, Ebraheim NA, Southworth SR, Sabin JJ, Jackson WT. Plating of the fibula. Its potential value as an adjunct to external fixation of the tibia. Clin Orthop Relat Res. 1991; (266):209-13. [DOI:10.1097/00003086-199105000-00032]
- Ruecker AH, Hoffmann M, Rupprecht ME, Rueger JM. Distal Tibial Fractures: Intramedullary Nailing. Eur J Trauma Emerg Surg. 2009; 35(6):520-6. [DOI:10.1007/s00068-009-9185-y] [PMID]
- Kumar A, Charlebois SJ, Cain EL, Smith RA, Daniels AU, Crates JM. Effect of fibular plate fixation on rotational stability of simulated distal tibial fractures treated with intramedullary nailing. J Bone Joint Surg Am. 2003; 85(4):604-8. [DOI:10.2106/00004623-200304000-00003] [PMID]
- Chin KR, Nagarkatti DG, Miranda MA, Santoro VM, Baumgaertner MR, Jupiter JB. Salvage of distal tibia metaphyseal non:union:s with the 90 degrees cannulated blade plate. Clin Orthop Relat Res. 2003; (409):241-9. [DOI:10.1097/00003086-200304000-00031] [PMID]
- Williams TM, Marsh JL, Nepola JV, DeCoster TA, Hurwitz SR, Bonar SB. External fixation of tibial plafond fractures: is routine plating of the fibula necessary?. J Orthop Trauma. 1998; 12(1):16-20. [DOI:10.1097/00005131-199801000-00003]
- Negahban H, Mazaheri M, Salavati M, Sohani SM, Askari M, Fanian H, Parnianpour M. Reliability and validity of the foot and ankle outcome score: A validation study from Iran. Clin Rheumatol. 2010; 29(5):479-86. [DOI:10.1007/s10067-009-1344-3] [PMID]
- Torkaman A, Aris A, Yazdi H. Evaluating outcome of distal tibia and fibula fractures treated with intra medullary nailing. Biomed Pharm J. 2016; 9(2):793-8. [DOI:10.13005/bpj/1005]
- Rouhani A, Elmi A, Aghdam HA, Panahi F, Ghafari YD. The role of fibular fixation in the treatment of tibia diaphysis distal third fractures. Orthop Traumatol Surg Res. 2012; 98(8):868-72. [DOI:10.1016/j.otsr.2012.09.009]
Type of Study: Research Article |
Subject:
Foot and Ankle
Received: 2024/02/25 | Accepted: 2024/04/23 | Published: 2024/05/1
Received: 2024/02/25 | Accepted: 2024/04/23 | Published: 2024/05/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









