Volume 11, Issue 4 (11-2024)
JROS 2024, 11(4): 221-226 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Najd Mazhar F, Zareie B, Mahmoudi Nasab O, Mohammadi R, Mohammadnab S, Kafiabadi M J et al . Non-operative Management of Terrible Triad Injuries of the Elbow: A Case Series. JROS 2024; 11 (4) :221-226
URL: http://jros.iums.ac.ir/article-1-2282-en.html
URL: http://jros.iums.ac.ir/article-1-2282-en.html
Farid Najd Mazhar1 

 , Bushra Zareie1
, Bushra Zareie1 
 , Omid Mahmoudi Nasab1
, Omid Mahmoudi Nasab1 

 , Reza Mohammadi1
, Reza Mohammadi1 

 , Sajjad Mohammadnab2
, Sajjad Mohammadnab2 

 , Meisam Jafari Kafiabadi3
, Meisam Jafari Kafiabadi3 
 , Hooman Shariatzade1
, Hooman Shariatzade1 




 , Bushra Zareie1
, Bushra Zareie1 
 , Omid Mahmoudi Nasab1
, Omid Mahmoudi Nasab1 

 , Reza Mohammadi1
, Reza Mohammadi1 

 , Sajjad Mohammadnab2
, Sajjad Mohammadnab2 

 , Meisam Jafari Kafiabadi3
, Meisam Jafari Kafiabadi3 
 , Hooman Shariatzade1
, Hooman Shariatzade1 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Department of Orthopedics Surgery, Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedic Surgery, School of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
3- Department of Orthopedics Surgery, Shohada-e Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Terrible triad injury (TT), Elbow dislocation, Radial head fracture, Coronoid process fracture, Non-operative management, Closed reduction, Joint stability
Full-Text [PDF 2417 kb]
(62 Downloads)
| Abstract (HTML) (123 Views)
Full-Text: (9 Views)
Introduction
The terrible triad (TT) injury of the elbow is a complex injury involving ulnohumeral dislocation, radial head fracture, and coronoid process fracture [1, 2]. Historically, surgical intervention has been the standard of care due to the inherent instability of the elbow joint following this injury [3]. However, recent studies have explored the feasibility of non-operative management in select patients who meet specific criteria, such as a congruent joint after closed reduction and a stable range of motion (ROM) [1, 4-6].
This study aims to contribute to the evidence supporting non-operative management by presenting a case series of 17 patients treated between 2015 and 2023. We evaluated functional outcomes, ROM, and complications associated with this approach.
Methods
Between 2015 and 2023, our institution treated 17 patients with TT injuries non-operatively. The inclusion criteria for non-operative management included congruent joint reduction on both anteroposterior (AP) and lateral radiographs after closed reduction, with a humeroulnar distance of less than 4 mm on the lateral view, no indication for surgical intervention for radial head or coronoid fractures (e.g. minimally displaced fractures or fractures that did not compromise joint stability), no block in active supination and pronation up to 60 degrees, absence of intra-articular fragments on computed tomography (CT) scan, stable and pain-free active ROM in the ulnohumeral joint, with a minimum of 45 degrees of extension, motivated and cooperative patients who were willing to adhere to a strict physiotherapy regimen.
The exclusion criteria included patients with significant joint instability or subluxation after closed reduction, displaced or comminuted radial head or coronoid fractures requiring surgical fixation, intra-articular fragments that could not be reduced conservatively, neurovascular compromise or open injuries requiring surgical intervention, history of previous elbow trauma or pre-existing elbow arthritis, and patients who were non-compliant with follow-up or physiotherapy.
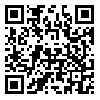
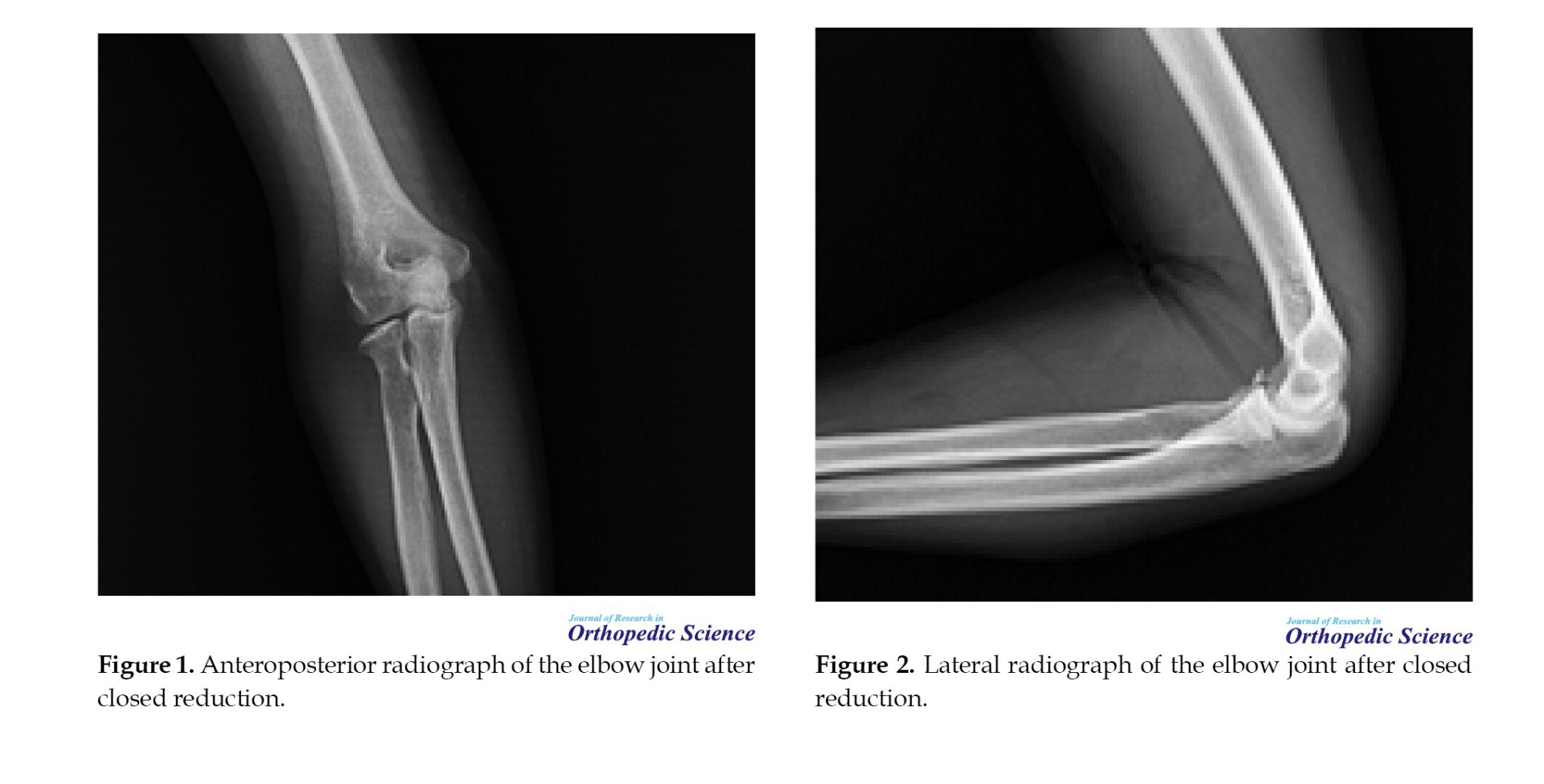
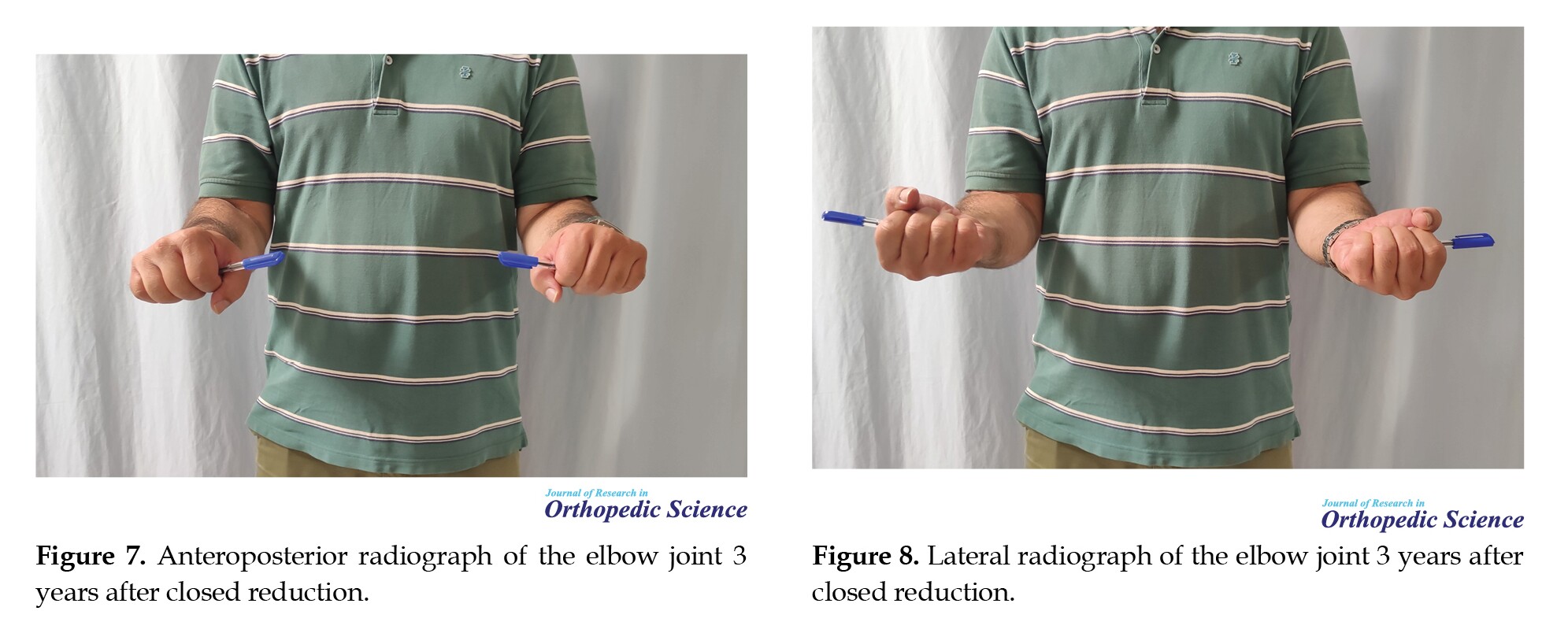
All patients underwent closed reduction under conscious sedation in the operating room. Post-reduction radiographs and CT scans were obtained to confirm joint congruency and assess fracture patterns (Figures 1 and 2).
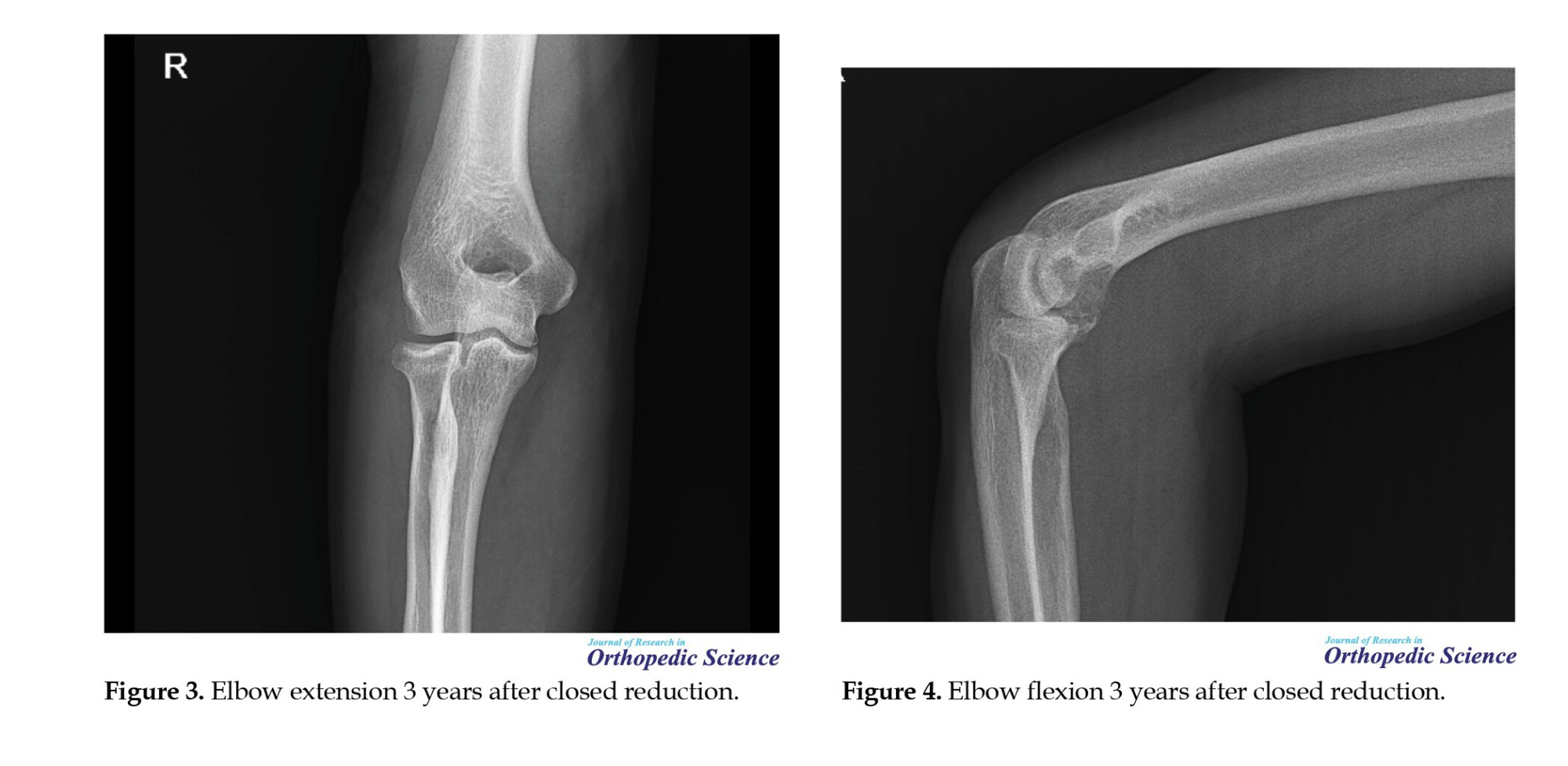
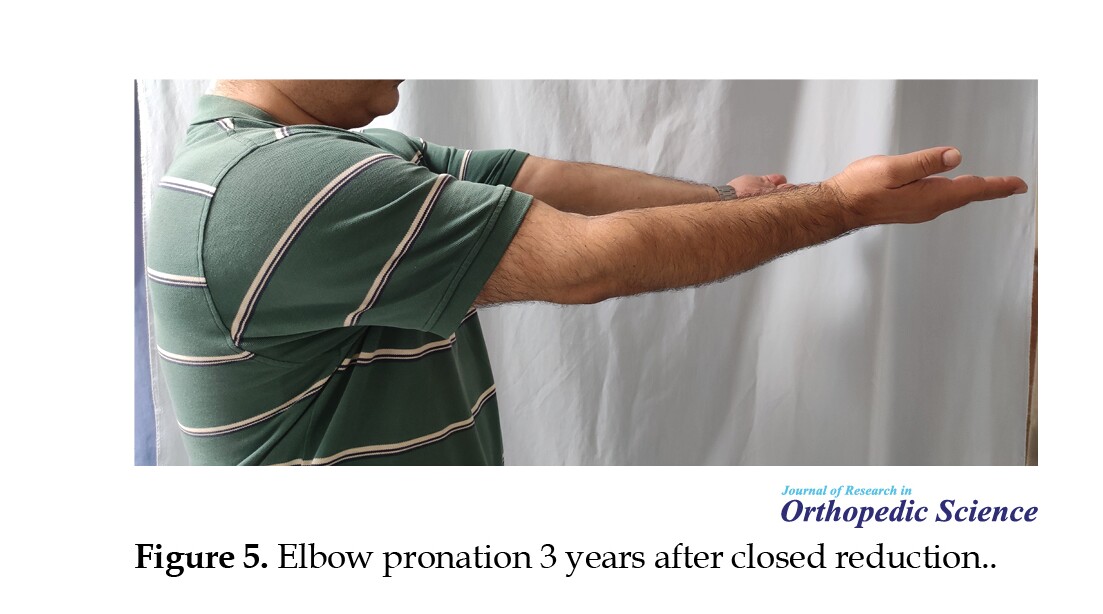
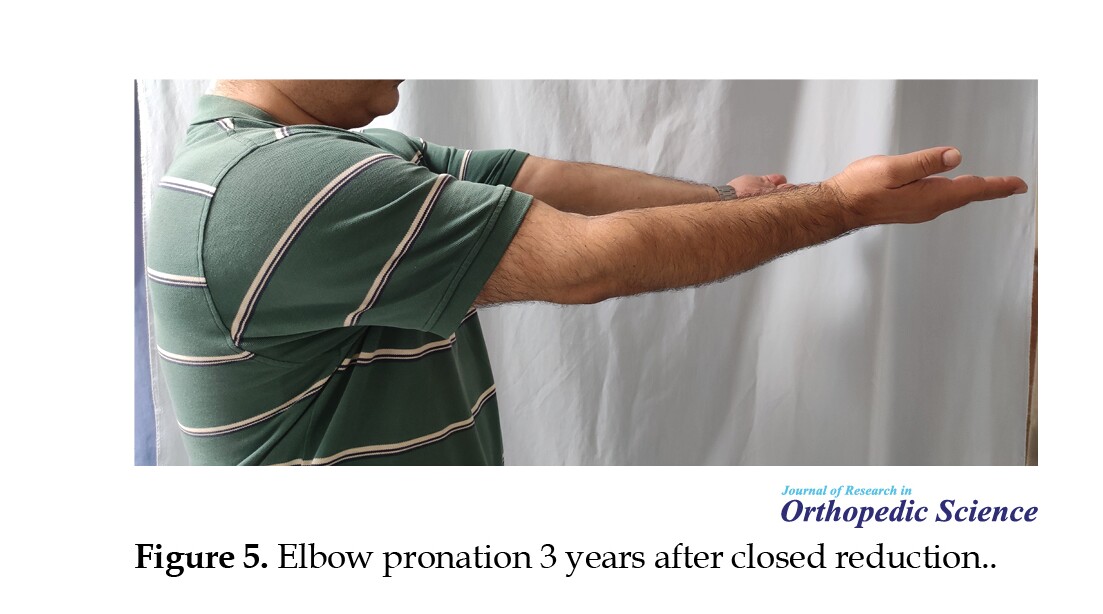
Patients were referred to physiotherapy for early active ROM exercises, with extension initially limited to 45 degrees and gradually increased weekly. Functional outcomes were assessed using the Mayo elbow performance index (MEPI) and the disabilities of the arm, shoulder, and hand (DASH) score. ROM was measured using a goniometer, and radiographic evaluation was performed to determine joint congruency, fracture :union:, and the presence of arthritis (Figures 3, 4, 5 and 6).

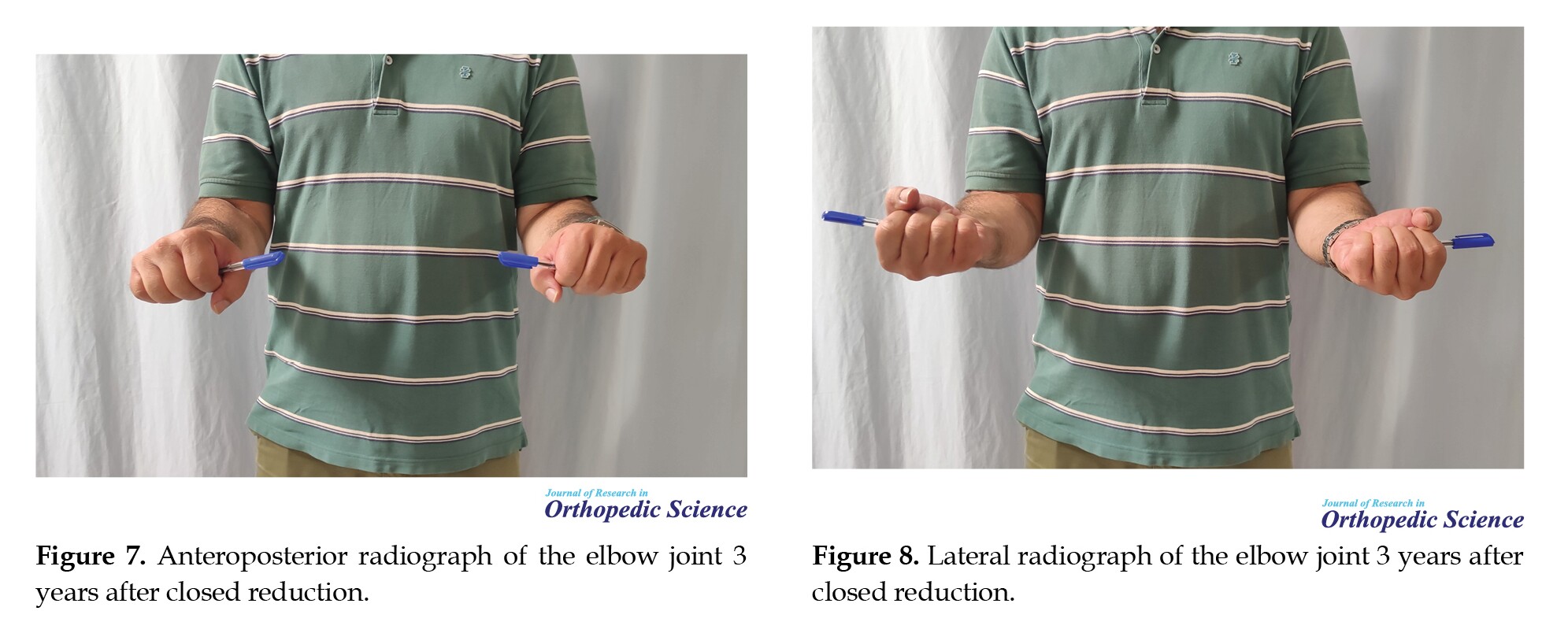
Complications, including symptoms associated with the ulnar nerve and joint instability, were documented (Figures 7 and 8).
Results
The study included 17 patients (14 males and 3 females) with a mean age of 38.12 years (22-57 years). The mean follow-up period was 53.24 months (range: 26-96 months). The demographic and clinical characteristics of the patients are summarized in Table 1.

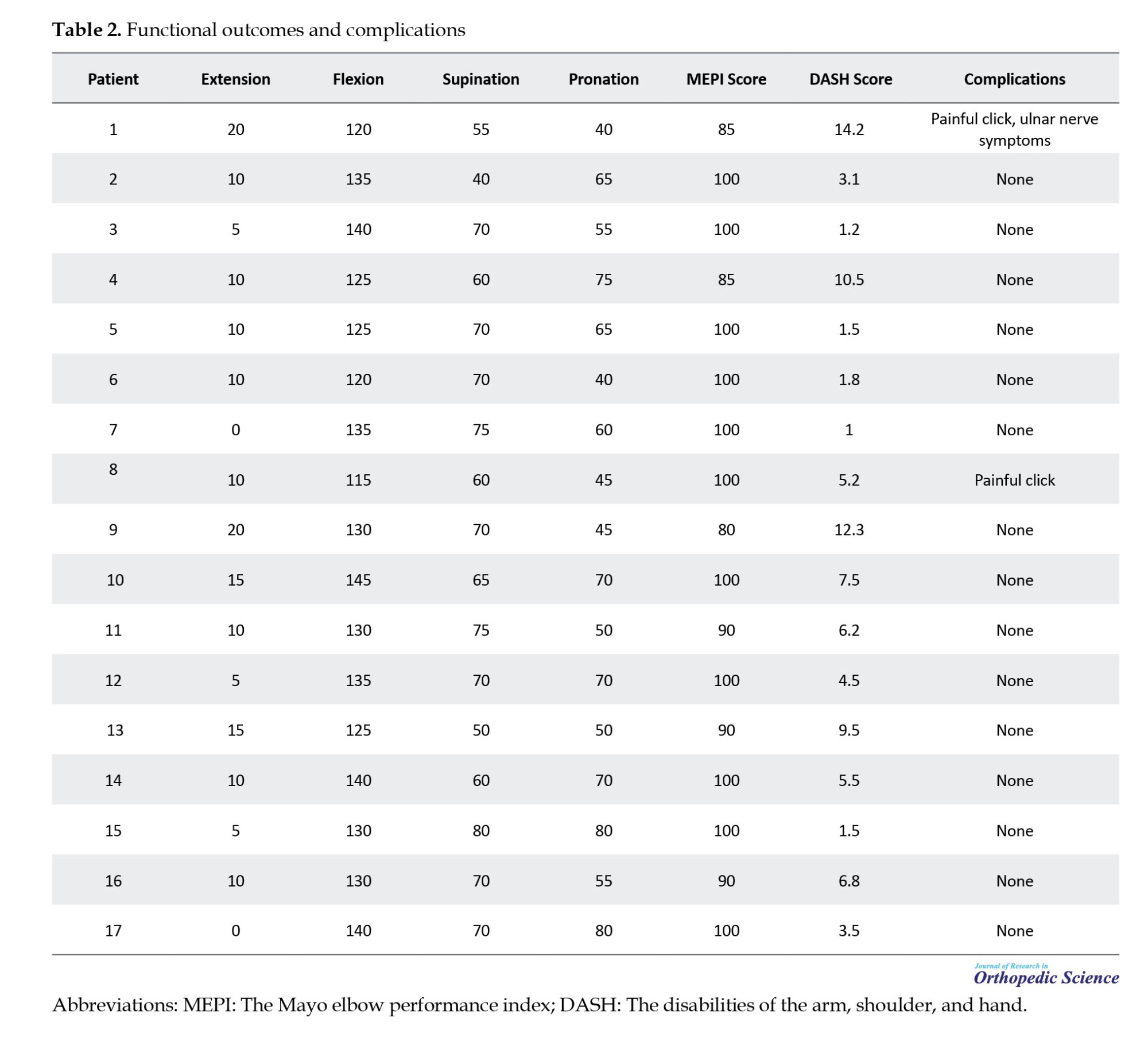
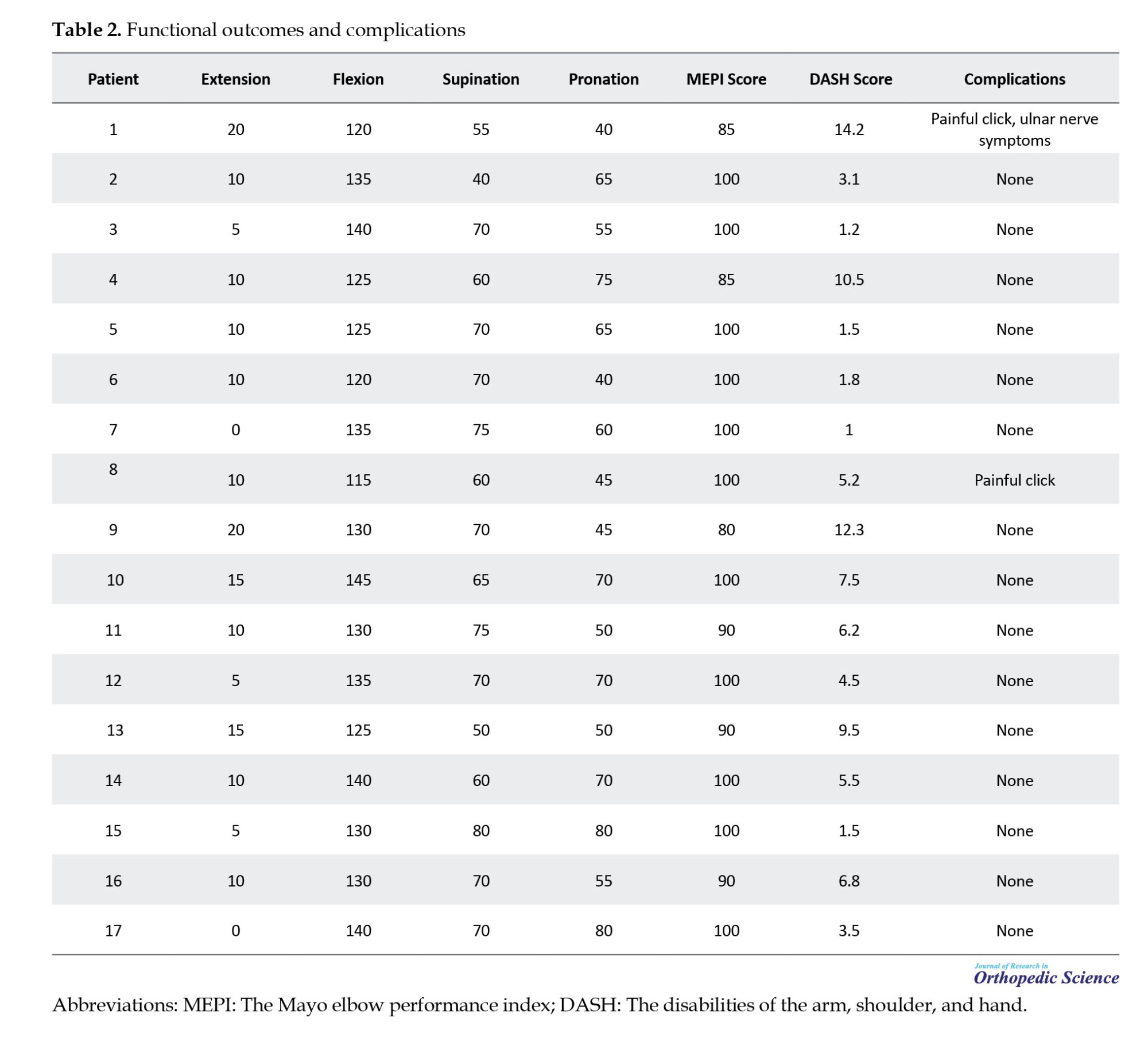
The mean MEPI score was 95.29±6.95, and the mean DASH score was 5.64±4.06. The mean ROM for the affected elbow was 9.71±5.72 degrees in extension, 130.6±8.27 degrees in flexion, 65.29±10.07 degrees in supination, and 59.71±13.4 degrees in pronation. The functional outcomes and complications are summarized in Table 2.
All radial head fractures achieved :union:, while 7 coronoid fractures (41.2%) showed fibrous :union:. One patient developed ulnar nerve symptoms that underwent ulnar neurolysis and anterior transposition of the medial epicondyle, and 2 patients reported occasional painful clicking during supination and pronation. No cases of recurrent dislocation or significant joint instability were observed.
Discussion
Non-operative management of TT injuries has gained traction in recent years, particularly for patients who meet specific stability criteria [4, 5]. Our findings are consistent with previous studies, which have reported acceptable functional outcomes with non-operative treatment in select patients. However, the potential for reduced supination and pronation, as well as the development of post-traumatic arthritis, remains a concern. The mean MEPI score of 95.29 in our study is comparable to that reported by Chan et al., who found a mean MEPI score of 94 in their cohort of non-operatively managed TT injuries [4]. Similarly, the mean DASH score of 5.64 in our study is slightly higher than the 4.76 reported by Najd Mazhar et al. suggesting a minor reduction in functional outcomes [7]. The development of mild arthritic changes in 29.4% of our patients is consistent with previous reports, highlighting the potential for long-term joint degeneration even in patients with initially stable reductions. This finding underscores the importance of careful patient selection and close follow-up to monitor for late complications.
While this study provides valuable insights into the non-operative management of TT injuries of the elbow, several limitations should be acknowledged. The study included only 17 patients, which limits the generalizability of the findings. A larger cohort would provide more robust evidence and allow for subgroup analyses. The patients included in this study were carefully selected based on specific criteria for non-operative management. This selection bias may limit the applicability of the findings to a broader population of TT injuries, many of which may not meet these criteria. The study was conducted retrospectively, which may introduce recall bias and limit the ability to control for confounding variables. A prospective study design would provide stronger evidence. The mean follow-up period was 36.5 months, with a range of 24 to 62 months. While this provides valuable medium-term outcomes, longer follow-up is necessary to assess the long-term effects of non-operative management, particularly the progression of post-traumatic arthritis. The study did not include a control group of patients who underwent surgical management. A direct comparison between surgical and non-operative management would provide more comprehensive insights into the relative benefits and drawbacks of each approach. The study was conducted at a single institution, which may limit the generalizability of the findings to other settings with different patient populations and treatment protocols. While all patients were referred to physiotherapy, there may have been variability in the specific protocols and adherence to these protocols, which could influence the outcomes. The assessment of arthritic changes was based on radiographic findings, which may not fully capture the clinical significance of these changes. Advanced imaging techniques, such as magnetic resonance imaging (MRI), can provide more detailed information. Functional outcomes were assessed using patient-reported measures (MEPI and DASH scores), which may be subject to bias. Objective measures of elbow function and stability could provide additional insights. While the study reported complications such as ulnar nerve symptoms and painful clicking, the small sample size limits the ability to draw definitive conclusions about the incidence and management of these complications.
Conclusion
Non-operative management of TT injuries can yield acceptable functional outcomes in carefully selected patients. However, the potential for reduced supination and pronation, as well as the development of post-traumatic arthritis, should be considered. Further studies with larger cohorts and longer follow-up periods are needed to validate these findings and refine the criteria for non-operative management.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethic Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1403.966), Tehran, Iran. All participants provided written informed consent before participating in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Farid Najd Mazhar; Methodology, software, validation and formal analysis: Bushra Zareie; Investigation and resources, Data collection: Hooman Shariatzade and Farid Najd Mazhar; Writing the original draft: Meisam jafari kafiabadi; Review & editing: Omid mahmoudi nasab; Visualization and Supervision: Reza Mohammadi and Sajjad Mohammadnabi.
Conflict of interest
The authors declared no Conflict of interest.
References
The terrible triad (TT) injury of the elbow is a complex injury involving ulnohumeral dislocation, radial head fracture, and coronoid process fracture [1, 2]. Historically, surgical intervention has been the standard of care due to the inherent instability of the elbow joint following this injury [3]. However, recent studies have explored the feasibility of non-operative management in select patients who meet specific criteria, such as a congruent joint after closed reduction and a stable range of motion (ROM) [1, 4-6].
This study aims to contribute to the evidence supporting non-operative management by presenting a case series of 17 patients treated between 2015 and 2023. We evaluated functional outcomes, ROM, and complications associated with this approach.
Methods
Between 2015 and 2023, our institution treated 17 patients with TT injuries non-operatively. The inclusion criteria for non-operative management included congruent joint reduction on both anteroposterior (AP) and lateral radiographs after closed reduction, with a humeroulnar distance of less than 4 mm on the lateral view, no indication for surgical intervention for radial head or coronoid fractures (e.g. minimally displaced fractures or fractures that did not compromise joint stability), no block in active supination and pronation up to 60 degrees, absence of intra-articular fragments on computed tomography (CT) scan, stable and pain-free active ROM in the ulnohumeral joint, with a minimum of 45 degrees of extension, motivated and cooperative patients who were willing to adhere to a strict physiotherapy regimen.
The exclusion criteria included patients with significant joint instability or subluxation after closed reduction, displaced or comminuted radial head or coronoid fractures requiring surgical fixation, intra-articular fragments that could not be reduced conservatively, neurovascular compromise or open injuries requiring surgical intervention, history of previous elbow trauma or pre-existing elbow arthritis, and patients who were non-compliant with follow-up or physiotherapy.
All patients underwent closed reduction under conscious sedation in the operating room. Post-reduction radiographs and CT scans were obtained to confirm joint congruency and assess fracture patterns (Figures 1 and 2).
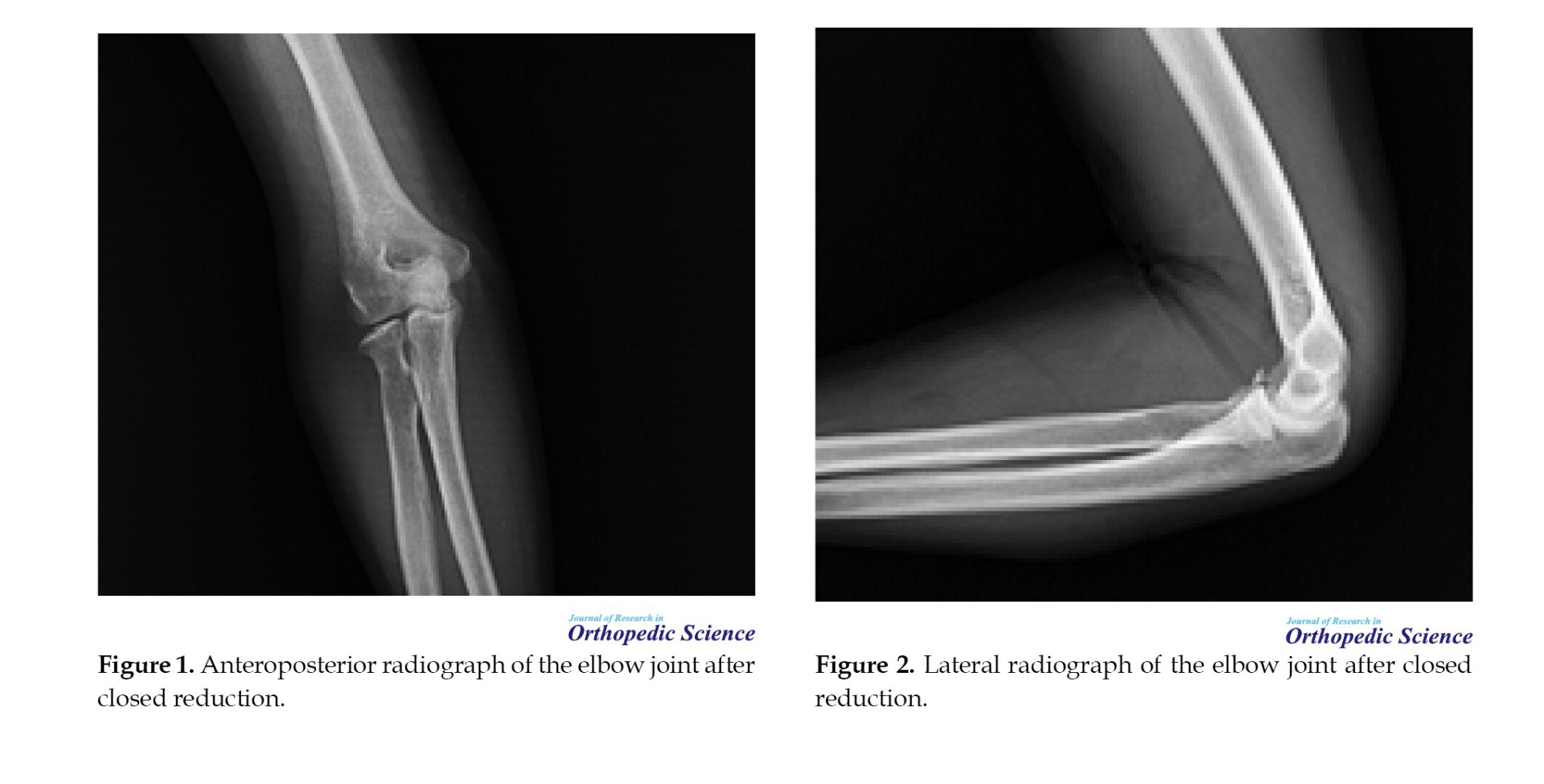
Patients were referred to physiotherapy for early active ROM exercises, with extension initially limited to 45 degrees and gradually increased weekly. Functional outcomes were assessed using the Mayo elbow performance index (MEPI) and the disabilities of the arm, shoulder, and hand (DASH) score. ROM was measured using a goniometer, and radiographic evaluation was performed to determine joint congruency, fracture :union:, and the presence of arthritis (Figures 3, 4, 5 and 6).
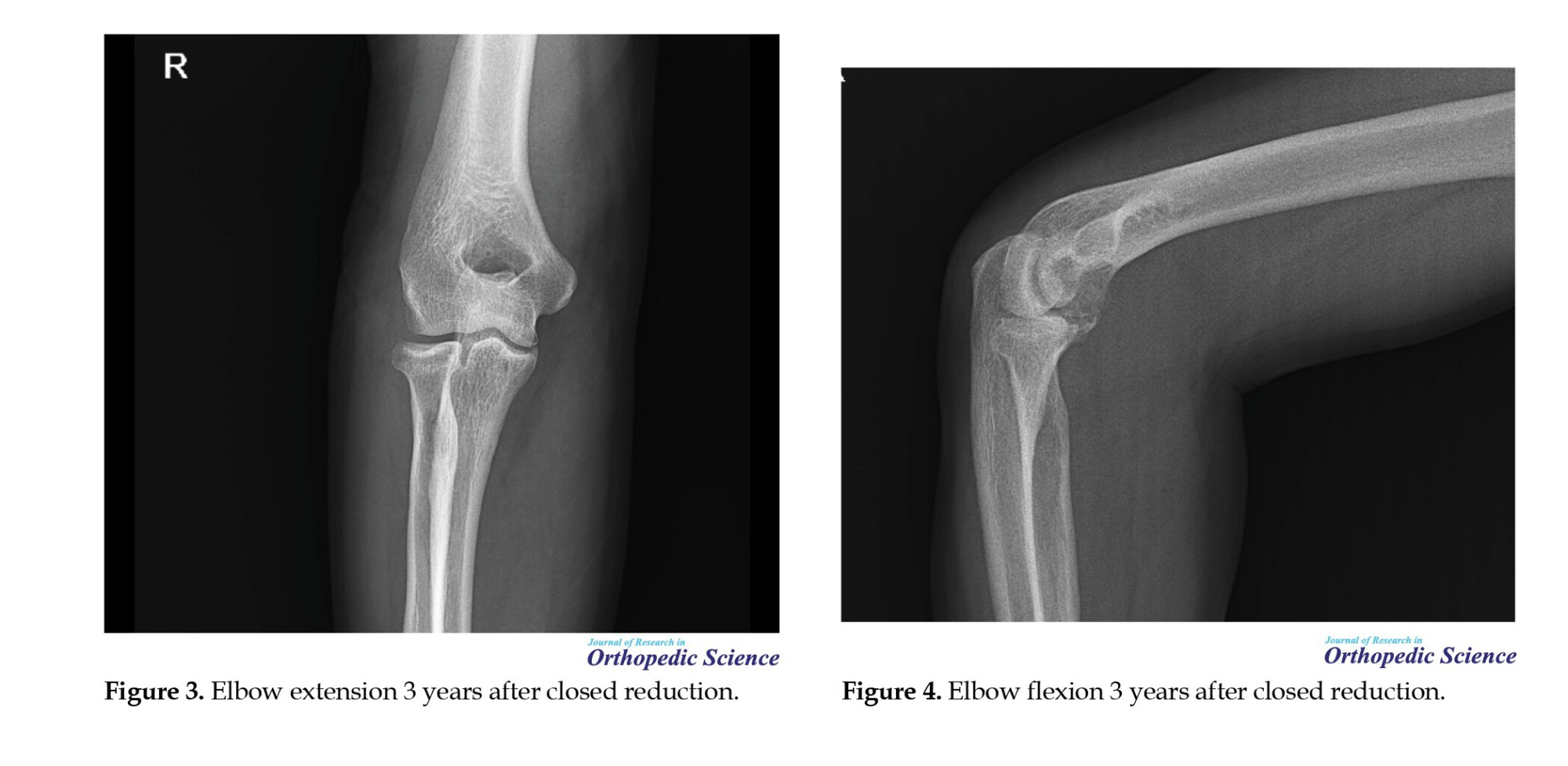

Complications, including symptoms associated with the ulnar nerve and joint instability, were documented (Figures 7 and 8).
Results
The study included 17 patients (14 males and 3 females) with a mean age of 38.12 years (22-57 years). The mean follow-up period was 53.24 months (range: 26-96 months). The demographic and clinical characteristics of the patients are summarized in Table 1.

The mean MEPI score was 95.29±6.95, and the mean DASH score was 5.64±4.06. The mean ROM for the affected elbow was 9.71±5.72 degrees in extension, 130.6±8.27 degrees in flexion, 65.29±10.07 degrees in supination, and 59.71±13.4 degrees in pronation. The functional outcomes and complications are summarized in Table 2.
All radial head fractures achieved :union:, while 7 coronoid fractures (41.2%) showed fibrous :union:. One patient developed ulnar nerve symptoms that underwent ulnar neurolysis and anterior transposition of the medial epicondyle, and 2 patients reported occasional painful clicking during supination and pronation. No cases of recurrent dislocation or significant joint instability were observed.
Discussion
Non-operative management of TT injuries has gained traction in recent years, particularly for patients who meet specific stability criteria [4, 5]. Our findings are consistent with previous studies, which have reported acceptable functional outcomes with non-operative treatment in select patients. However, the potential for reduced supination and pronation, as well as the development of post-traumatic arthritis, remains a concern. The mean MEPI score of 95.29 in our study is comparable to that reported by Chan et al., who found a mean MEPI score of 94 in their cohort of non-operatively managed TT injuries [4]. Similarly, the mean DASH score of 5.64 in our study is slightly higher than the 4.76 reported by Najd Mazhar et al. suggesting a minor reduction in functional outcomes [7]. The development of mild arthritic changes in 29.4% of our patients is consistent with previous reports, highlighting the potential for long-term joint degeneration even in patients with initially stable reductions. This finding underscores the importance of careful patient selection and close follow-up to monitor for late complications.
While this study provides valuable insights into the non-operative management of TT injuries of the elbow, several limitations should be acknowledged. The study included only 17 patients, which limits the generalizability of the findings. A larger cohort would provide more robust evidence and allow for subgroup analyses. The patients included in this study were carefully selected based on specific criteria for non-operative management. This selection bias may limit the applicability of the findings to a broader population of TT injuries, many of which may not meet these criteria. The study was conducted retrospectively, which may introduce recall bias and limit the ability to control for confounding variables. A prospective study design would provide stronger evidence. The mean follow-up period was 36.5 months, with a range of 24 to 62 months. While this provides valuable medium-term outcomes, longer follow-up is necessary to assess the long-term effects of non-operative management, particularly the progression of post-traumatic arthritis. The study did not include a control group of patients who underwent surgical management. A direct comparison between surgical and non-operative management would provide more comprehensive insights into the relative benefits and drawbacks of each approach. The study was conducted at a single institution, which may limit the generalizability of the findings to other settings with different patient populations and treatment protocols. While all patients were referred to physiotherapy, there may have been variability in the specific protocols and adherence to these protocols, which could influence the outcomes. The assessment of arthritic changes was based on radiographic findings, which may not fully capture the clinical significance of these changes. Advanced imaging techniques, such as magnetic resonance imaging (MRI), can provide more detailed information. Functional outcomes were assessed using patient-reported measures (MEPI and DASH scores), which may be subject to bias. Objective measures of elbow function and stability could provide additional insights. While the study reported complications such as ulnar nerve symptoms and painful clicking, the small sample size limits the ability to draw definitive conclusions about the incidence and management of these complications.
Conclusion
Non-operative management of TT injuries can yield acceptable functional outcomes in carefully selected patients. However, the potential for reduced supination and pronation, as well as the development of post-traumatic arthritis, should be considered. Further studies with larger cohorts and longer follow-up periods are needed to validate these findings and refine the criteria for non-operative management.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Research Ethic Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1403.966), Tehran, Iran. All participants provided written informed consent before participating in the study.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: Farid Najd Mazhar; Methodology, software, validation and formal analysis: Bushra Zareie; Investigation and resources, Data collection: Hooman Shariatzade and Farid Najd Mazhar; Writing the original draft: Meisam jafari kafiabadi; Review & editing: Omid mahmoudi nasab; Visualization and Supervision: Reza Mohammadi and Sajjad Mohammadnabi.
Conflict of interest
The authors declared no Conflict of interest.
References
- Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop. 2011; 35(6):851-60. [DOI:10.1007/s00264-010-1024-6] [PMID]
- Ormiston R, Hargreaves D. 'The treatable triad' long-term functional results of surgically treated acute isolated terrible triad injuries: An 18-year follow-up. J Shoulder Elbow Surg. 2025; 34(1):114-21. [DOI:10.1016/j.jse.2024.06.023] [PMID]
- El Koussaify J, Foster BK, Grandizio LC. Modern treatment protocols in the management of terrible triad elbow injuries. Oper Tech Orthop. 2023; 33(1):101023. [DOI:10.1016/j.oto.2023.101023]
- Chan K, MacDermid JC, Faber KJ, King GJ, Athwal GS. Can we treat select terrible triad injuries nonoperatively? Clin Orthop Relat Res. 2014; 472(7):2092-9. [DOI:10.1007/s11999-014-3518-9] [PMID]
- Guitton TG, Ring D. Nonsurgically treated terrible triad injuries of the elbow: Report of four cases. J Hand Surg Am. 2010; 35(3):464-7. [DOI:10.1016/j.jhsa.2009.12.015] [PMID]
- Baker M, Eyre-Brook A, Gokaraju K, Jones V, Thyagarajan D, Ali A, et al. Non-operative management of terrible triad injuries of the elbow; not so terrible? Shoulder Elbow. 2024; 16(2):200-5. [DOI:10.1177/17585732231190599] [PMID]
- Najd Mazhar F, Jafari D, Mirzaei A. Evaluation of functional outcome after nonsurgical management of terrible triad injuries of the elbow. J Shoulder Elbow Surg. 2017; 26(8):1342-7. [DOI:10.1016/j.jse.2017.05.012] [PMID]
Type of Study: Research Article |
Subject:
Hand surgery / Elbow
Received: 2025/03/25 | Accepted: 2025/09/27 | Published: 2024/11/20
Received: 2025/03/25 | Accepted: 2025/09/27 | Published: 2024/11/20
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |