Volume 11, Issue 4 (11-2024)
JROS 2024, 11(4): 213-220 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sami S A, Kargar K, Shams R, Zareie B, Beheshti Fard S, Hamidzadehkhiavi A. Pediatric Tumor Resection and Recon-struction: Outcomes of Osteoarticular Allograft Fix-ation With Stabilized Dynamized Nailing Technique. JROS 2024; 11 (4) :213-220
URL: http://jros.iums.ac.ir/article-1-2290-en.html
URL: http://jros.iums.ac.ir/article-1-2290-en.html
Sam Aliliu Sami1 

 , Khalil Kargar1
, Khalil Kargar1 
 , Roshanak Shams1
, Roshanak Shams1 
 , Bushra Zareie1
, Bushra Zareie1 
 , Shahabaldin Beheshti Fard2
, Shahabaldin Beheshti Fard2 
 , Amin Hamidzadehkhiavi3
, Amin Hamidzadehkhiavi3 




 , Khalil Kargar1
, Khalil Kargar1 
 , Roshanak Shams1
, Roshanak Shams1 
 , Bushra Zareie1
, Bushra Zareie1 
 , Shahabaldin Beheshti Fard2
, Shahabaldin Beheshti Fard2 
 , Amin Hamidzadehkhiavi3
, Amin Hamidzadehkhiavi3 


1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Bone and Joint Reconstruction Research Center, Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
3- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
2- Bone and Joint Reconstruction Research Center, Department of Orthopedics, School of Medicine, Iran University of Medical Sciences, Tehran, Iran
3- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, School of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
Keywords: Pediatric bone tumors, Osteoarticular allograft, Stabilized dynamized nailing, Intramedullary nailing (IMN), Lower limb reconstruction, Tumor resection, Osteosarcoma, Ewing sarcoma, Bone :union:, Fresh frozen allograft, Gentamicin-soaked allograft
Full-Text [PDF 1232 kb]
(82 Downloads)
| Abstract (HTML) (206 Views)
Full-Text: (52 Views)
Introduction
Limb-salvage surgery has transformed the treatment of malignant bone tumors in pediatric patients, becoming the preferred approach over amputation due to advancements in chemotherapy, imaging, and surgical techniques [1, 2]. These innovations have improved survival rates and functional outcomes, enabling patients to maintain limb function while effectively addressing aggressive tumors such as osteosarcoma and Ewing sarcoma [3]. However, reconstructing large bone defects following tumor resection in the lower extremity remains a complex challenge, particularly in growing children, where limb length and joint preservation are critical [4, 5].
The primary reconstruction options for these defects include biological approaches, such as autografts, allografts, or vascularized fibular grafts, as well as mechanical solutions like endoprostheses or allograft-prosthetic composites [3, 6, 7]. Each method has trade-offs: Biological reconstructions promote long-term integration but risk complications like non:union:, fracture, and infection, while mechanical options offer immediate stability but may fail over time due to wear or loosening [8]. Osteoarticular allografts, which preserve joint function by replacing both bone and articular surfaces, are particularly appealing for pediatric patients but are prone to mechanical failures, with reported fracture rates ranging from 8% to 29% and non:union: rates from 17% to 40% in the literature [4, 9].
Fixation techniques play a pivotal role in the success of allograft reconstruction. Intramedullary nailing (IMN) and plate fixation are commonly used, with nails offering advantages like easier alignment and early weight-bearing [10]. However, achieving stable yet dynamic fixation to promote bone :union: without stress-shielding remains a challenge [9]. Excessive rigidity can lead to negative bone remodeling, while inadequate stability increases the risk of fracture or non:union: [6, 9]. Recent studies have explored modifications, such as compressible nails or dynamic locking, to enhance :union: rates; however, data specific to pediatric populations are limited [11, 12].
This study introduces a novel stabilized dynamized nailing technique (SDNT) for fixing osteoarticular allografts in pediatric lower limb tumor resection. By combining IMN with controlled dynamization and antibiotic-soaked allografts, SDNT aims to optimize mechanical stability and bone :union: while minimizing complications. We present the outcomes of 40 pediatric patients treated with this approach, focusing on :union: time, complication rates, and functional prognosis to evaluate its efficacy in this challenging clinical scenario.
Methods
We conducted a retrospective chart review of 41 pediatric cases under limb-salvage surgery for malignant bone tumors of the lower extremity between 2014 and 2024 at our institution. The selection criteria were as follows: 1) tumors of the diaphyseal or metaphyseal location of a long bone (femur or tibia), with preservation of adjacent joints post-resection; 2) wide tumor resection with at least a 2-cm margin, confirmed by preoperative magnetic resonance imaging (MRI) and biopsy; and 3) a minimum postoperative follow-up of 12 months, with regular clinical and radiographic assessments. Diagnoses, confirmed by preoperative biopsy, included osteosarcoma, Ewing sarcoma, or chondrosarcoma. Patients with osteosarcoma or Ewing sarcoma received neo-adjuvant chemotherapy and radiotherapy, while those with chondrosarcoma received only postoperative adjuvant therapy.
Allograft preparation
Fresh frozen osteoarticular allografts (FFOAs) were sourced from a certified bone bank, stored in liquid nitrogen, and sterile-packaged without irradiation. Allografts were age-, size-, and side-matched to the recipient and thawed in 2 L of warm normal saline containing 800 mg of gentamicin immediately before surgery to reduce the risk of infection. To address potential limb length discrepancies in pediatric patients, allografts were selected to be 0.5–1 cm longer than the resected bone segment [13].
Surgical technique
Tumor resection was performed with a wide margin (≥2 cm) based on preoperative MRI planning [14]. After resection, we employed SDNT for allograft fixation. For distal femur or proximal tibia tumors, the host bone’s proximal or distal segment was reamed to accommodate a cloverleaf-slotted intramedullary nail, selected for compatibility with the host bone’s diameter and length. On a separate sterile table, the allograft was similarly reamed, and bone cement was injected into its medullary canal to secure the nail, ensuring a 1-cm cement-free zone at the allograft-host junction to facilitate bone :union:. The nail allograft was then inserted into the host bone, aligning the nail to bridge the resection gap. Soft tissue reconstruction included ligament and capsular repair around the knee, followed by standard layered wound closure with a drain and immobilization in a long leg splint.
Postoperative management
Patients began isometric exercises 1 week after surgery and passive functional exercises at 2 weeks, under the guidance of physiotherapists. They used braces and crutches, remaining non-weight-bearing for the first 6 weeks. Partial and full weight-bearing were introduced gradually after radiographic evidence of healing at the allograft-host junction, typically assessed at 6 and 12 weeks. Follow-up occurred at 6 weeks, 12 weeks, every 3 months for the first 2 years, every 6 months for the next 3 years, and annually thereafter. Evaluations included oncological status, bone :union: (defined as bridging bone across three cortices on anteroposterior and lateral radiographs or disappearance of the osteotomy line), and functional outcomes. Complications, such as non:union:, infection, fracture, or nail bending, were recorded, with the need for allograft removal or replacement considered a treatment failure.
Outcome assessment
We evaluated key outcomes, including time to :union:, complication rates (e.g. delayed :union:, infection, nail bending), disease relapse, metastasis, and mortality. Functional outcomes were assessed by range of motion and clinical symptoms, with radiographic assessments confirming bone healing and implant stability. Data were collected from medical records and analyzed to determine the efficacy of SDNT in achieving stable reconstruction and minimizing complications in this pediatric cohort.
Results
We analyzed data from 40 pediatric patients (Mean±SD age: 11.85±2.93 years) who underwent lower limb tumor resection and reconstruction with osteoarticular allografts fixed using the SDNT between 2014 and 2024. The cohort was predominantly male (68.29%, n=28), with a Mean±SD follow-up of 33.68±20.58 months. Tumors were primarily osteosarcoma (70.73%, n=29), followed by Ewing sarcoma (24.39%, n=10), chondrosarcoma (2.44%, n=1), and neuroblastoma (2.44%, n=1). Most tumors were located in the femur (65.85%, n=27) and the metaphyseal region (75.61%, n=31), with 68.29% (n=28) classified as stage II and 31.71% (n=13) as stage III (Table 1). Neoadjuvant chemotherapy was administered to 95% (n=38) of patients, and 39.02% (n=16) received neoadjuvant radiotherapy.
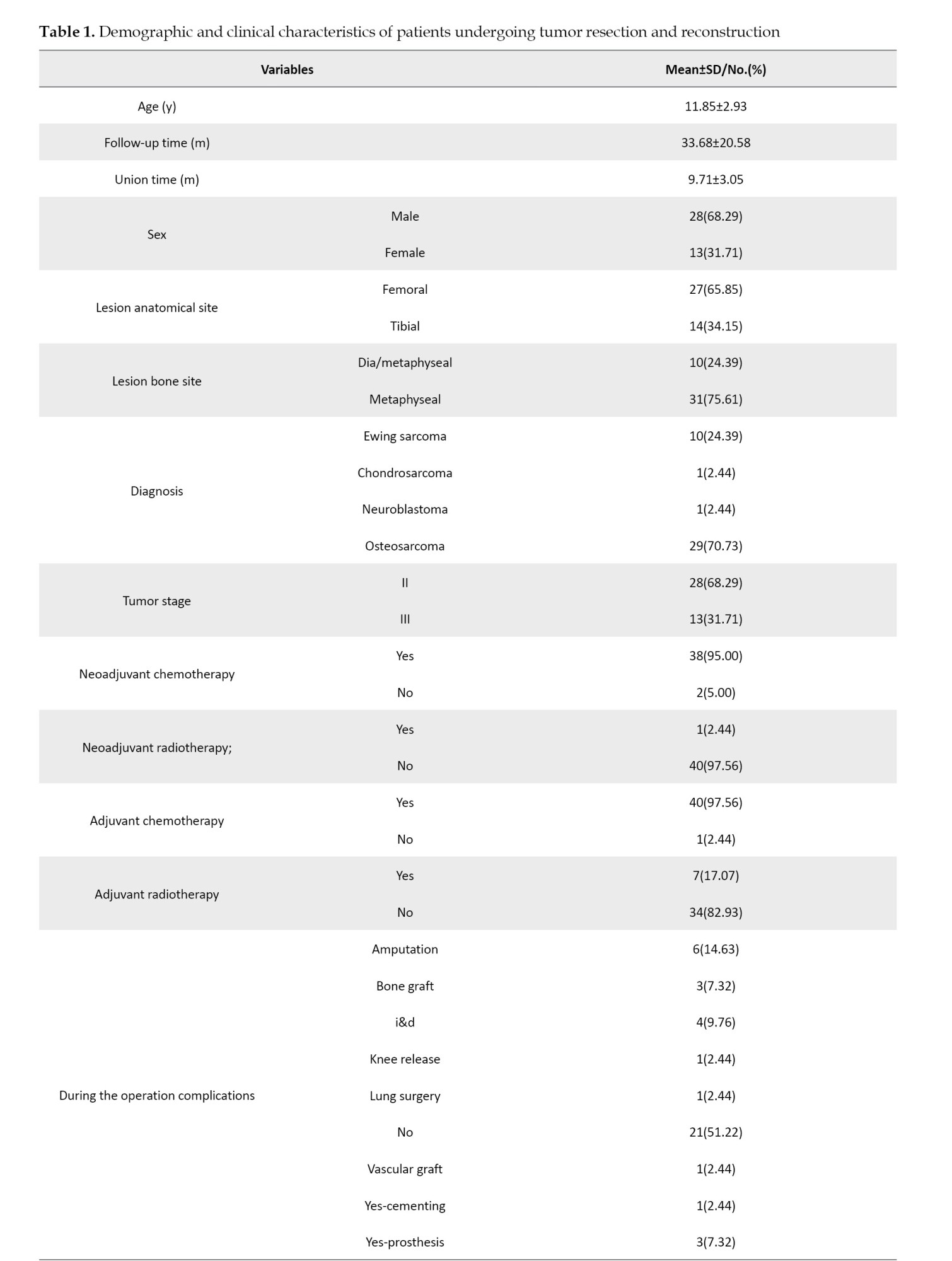

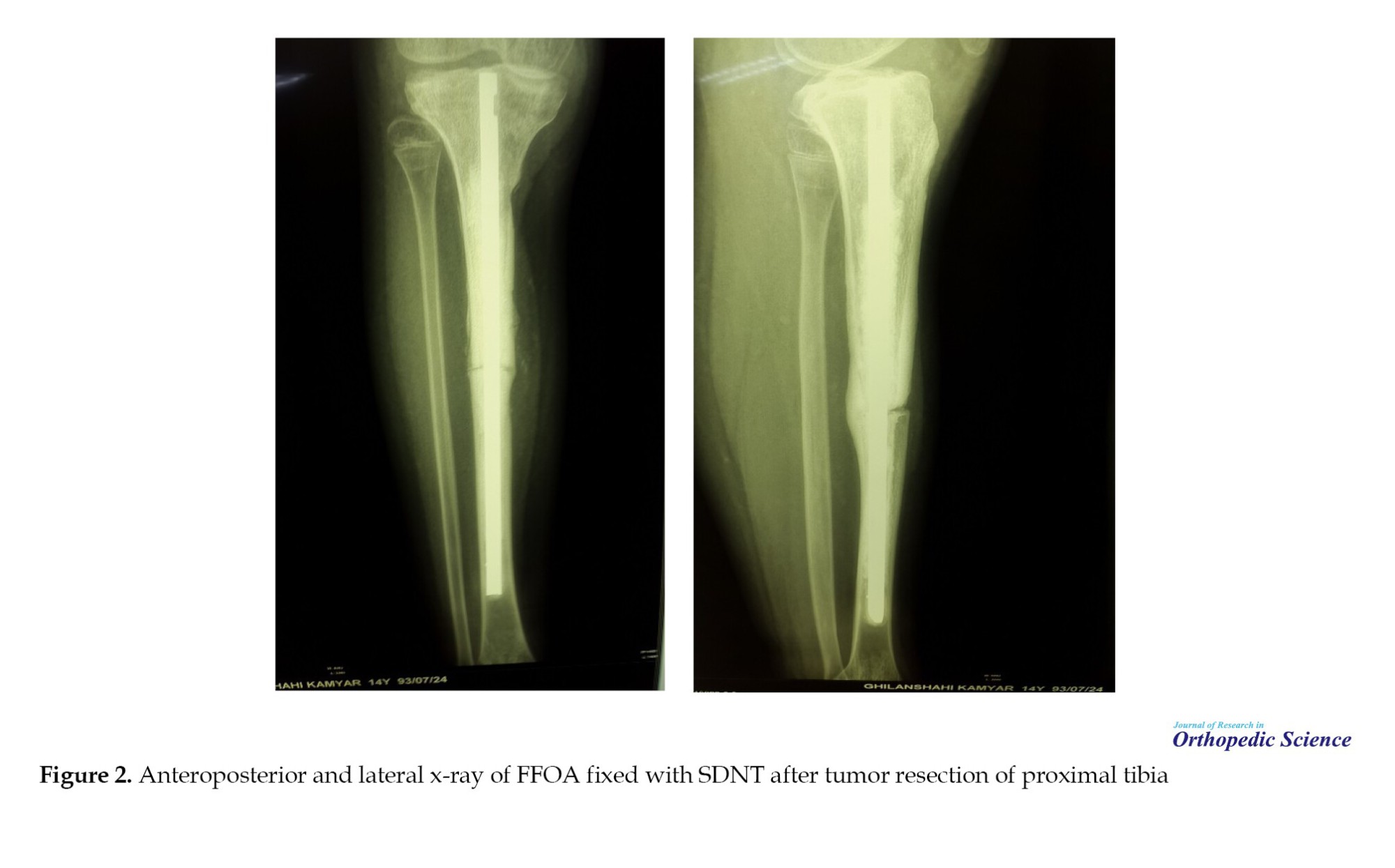
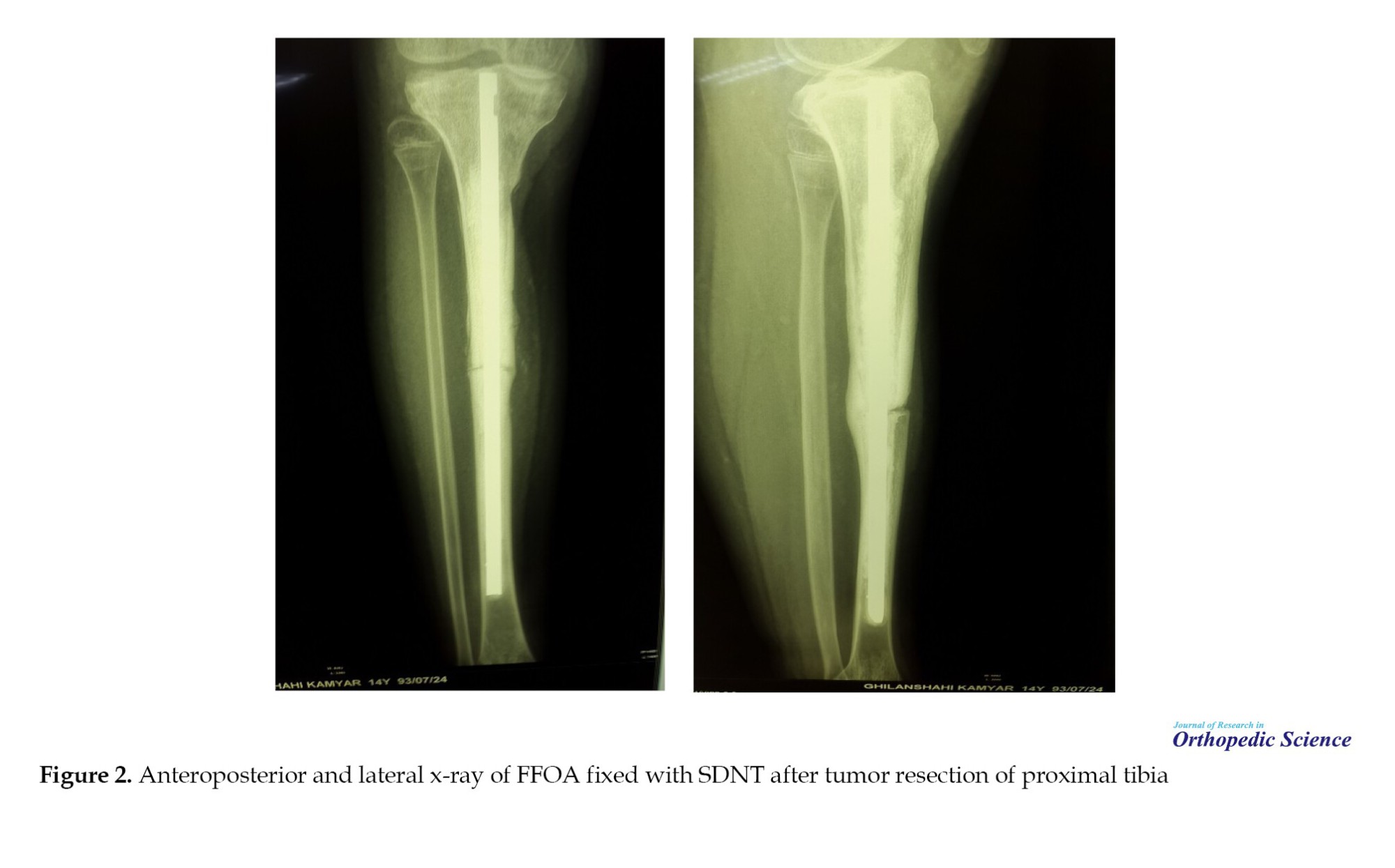
The Mean±SD time to bone :union: was 9.71±3.05 months, with successful allograft-host integration observed radiographically (Figures 1 and 2).
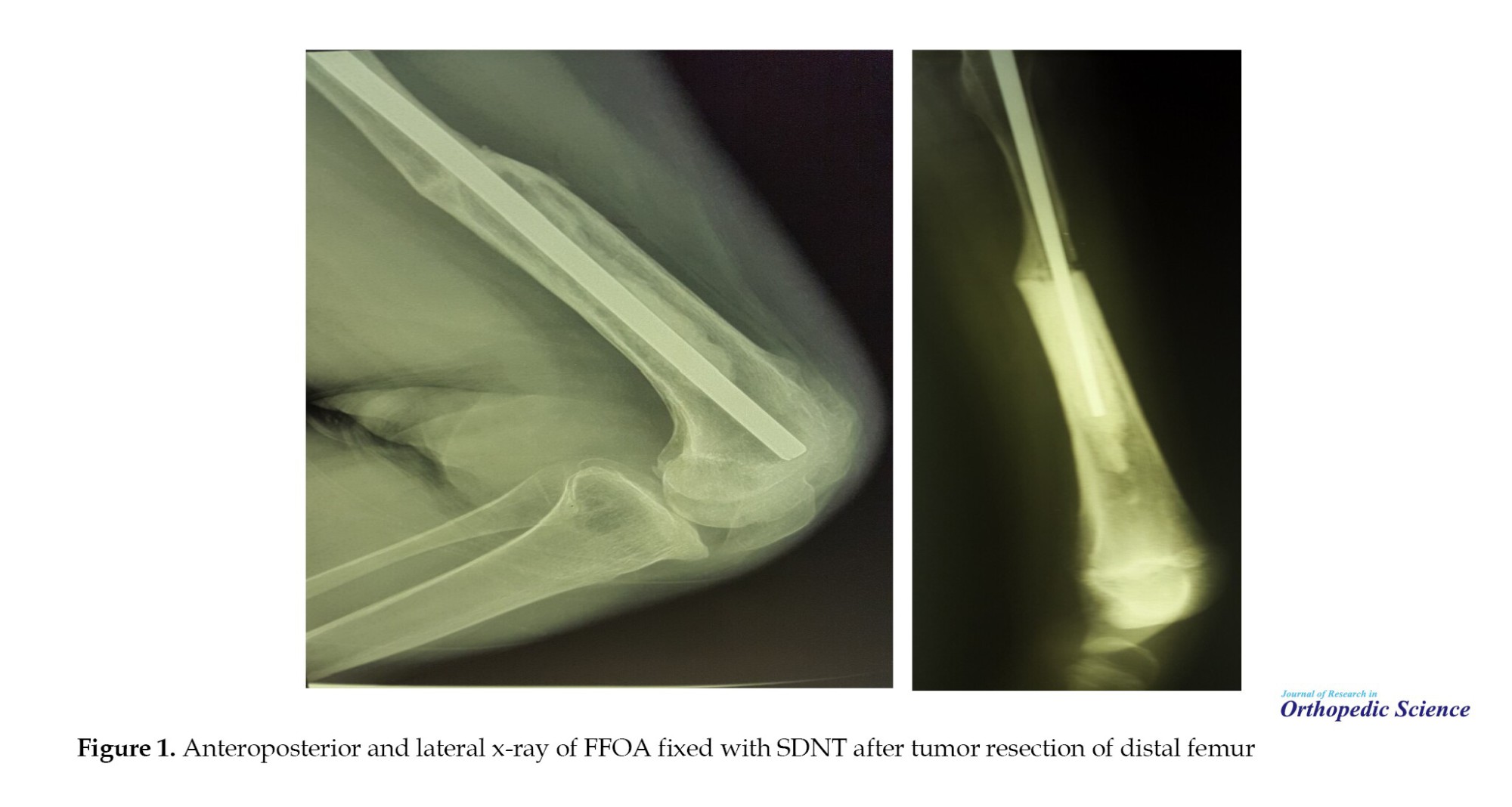
Postoperative complications occurred in 48.88% (n=20) of patients. Delayed :union: was the most common complication (24.39%, n=10), followed by infection (14.64%, n=6), drop foot (4.88%, n=2), nail bending (2.44%, n=1), non:union: (2.44%, n=1), and superficial wound issues (2.44%, n=1) (Table 2). Notably, no allograft fractures occurred, with nail bending being the only mechanical failure observed, as seen in postoperative radiographs of distal femur and proximal tibia reconstructions (Figure 1 for distal femur; Figure 2 for proximal tibia) [1]. Reoperations were required in 48.78% (n=20) of cases, including amputation (14.63%, n=6), bone grafting (7.32%, n=3), irrigation and debridement (9.76%, n=4), knee release (2.44%, n=1), lung surgery (2.44%, n=1), vascular grafting (2.44%, n=1), and prosthesis placement (7.32%, n=3). Intraoperative complications occurred in 12.2% (n=5) of cases.
Oncologic outcomes showed a mortality rate of 29.27% (n=12), with 70.73% (n=29) of patients alive at the last follow-up. Disease relapse occurred in 17.07% (n=7) of patients, and metastasis was observed in 36.58% (n=15), primarily to the lungs (26.83%, n=11), followed by lung and shoulder (4.88%, n=2), bone (2.44%, n=1), and brain-lung (2.44%, n=1) (Table 2). A limited range of motion was reported in 78.05% (n=32) of patients, potentially due to postoperative complications or disease progression. Detailed demographic and clinical characteristics are presented in Table 1, with complication and metastasis data summarized in Table 2.

Discussion
In this retrospective study of 41 pediatric patients undergoing limb-salvage surgery for malignant bone tumors in the lower extremities, we demonstrated that reconstruction using FFOA fixed with a SDNT offers a viable biological option for restoring limb function. The cohort, primarily consisting of young patients with osteosarcoma or Ewing sarcoma, achieved a mean :union: time of approximately 9.7 months, resulting in a low incidence of catastrophic failures. Notably, delayed :union: in 10 patients emerged as the most common complication (24.39%), yet the majority of these cases progressed to eventual :union: without requiring major revisions. Twenty-six patients (63.42%) showed no complications, while infection affected 14.64% of patients, and other issues, such as drop foot or superficial wounds, were infrequent. Critically, no outright allograft fractures occurred, with only one instance of nail bending (2.44%), underscoring the mechanical stability provided by SDNT. These outcomes align with the broader goal of limb-salvage procedures: preserving function while minimizing morbidity in a vulnerable population.
When contextualized within the existing literature on intercalary allograft reconstructions, our findings highlight both similarities and potential advantages of the SDNT approach. For instance, :union:-related challenges persist as a recurring theme across studies. According to a 2023 study by Goldin et al., the median time to fracture-free allograft survival was significantly extended in the IMN group compared to the extramedullary plating (EMP) group. However, other outcomes showed no major disparities between these fixation approaches [10]. Further breaking down the EMP cohort into single-plate (SP) and multiple-plate (MP) subgroups revealed that MP patients faced elevated fracture risks, more frequent revision procedures, and reduced overall allograft longevity. Key metrics from their IMN arm included a 21% non:union: rate across host-graft junctions, 24% fracture occurrence, a median fracture-free survival of 7.9 years, 18% infection prevalence, 82% allograft retention at last follow-up, and a 59% revision surgery rate [10]. By comparison, our investigation reported a mean follow-up of 33.7 months under IMN, where delayed :union: was the leading issue at 24.39%, trailed by infection at 14.64% and foot drop at 4.88%; less common problems encompassed nail bending (2.44%), non:union: (2.44%), and superficial wounds (2.44%), with over half (51.22%) of cases complication-free. In contrast to the Goldin study, in our research, delayed :union: was the most prominent complication (which ultimately united to the host bone), indicating that this method could have promising results. Fracture rates in our study were significantly lower than those in the Goldin study, primarily due to the application of SDNT.
Similarly, a systematic review by Jamshidi et al. [15] reported non:union: in 37% of IMN-fixed intercalary allografts, fractures in 5%, and infections in 4%, with no local recurrences. While our infection rate was higher (14.64%), possibly attributable to the pediatric cohort’s immunocompromised state from neoadjuvant therapies or the extensive soft tissue dissection around the knee, the fracture rate was halved, reinforcing SDNT’s role in enhancing construct durability.
For instance, the method we used reveals that broader comparisons show biological reconstructions compare favorably to mechanical alternatives in select scenarios. Techniques such as allograft-prosthetic composites or endoprostheses, as discussed by Othman et al. [16] in their meta-analysis, often yield higher early functionality but carry risks of aseptic loosening or periprosthetic fractures in the long term, particularly in growing children, where preservation of the growth plate is paramount. Frisoni et al. [17] noted non:union: and fractures as key factors contributing to poor function in femoral allografts. By incorporating dynamization, we showed that SDNT appears to mitigate these biomechanical pitfalls, fostering a more balanced load transfer that supports osteogenesis without excessive rigidity.
The oncologic outcomes in our study—29.27% mortality, 17.07% relapse, and metastasis in about a third of cases—reflect the aggressive nature of these tumors in children, consistent with reports from Liu et al. [18] and Yang et al. [14], where stage II/III sarcomas predominated. Neoadjuvant chemotherapy was administered to 95% of our patients, likely contributing to the wide margins and low local recurrence, though pulmonary metastases remained a concern (26.83%). These systemic challenges underscore that while SDNT excels in local reconstruction, multidisciplinary management is crucial for long-term survival.
Strengths of our approach include the detailed operative protocol, which standardizes cement augmentation for nail stability while preserving a cement-free zone at the junction to avoid interfering with :union:—a nuance not always emphasized in prior IMN descriptions. The mean follow-up of 33.7 months provides mid-term insights, and the focus on pediatric patients fills a gap in the literature, where most data derive from mixed-age cohorts. However, limitations must be acknowledged. As a single-center retrospective review, selection bias may influence results, and the sample size limits statistical power for subgroup analyses, such as by tumor site (femoral vs tibial). Variability in neoadjuvant regimens and the absence of patient-reported outcomes, such as quality-of-life scores, represent areas for improvement. Additionally, while SDNT minimized fractures, the higher infection rate compared to meta-analyses suggests opportunities to refine antibiotic prophylaxis or allograft preparation.
Looking ahead, prospective multicenter trials could validate SDNT’s benefits, possibly incorporating biomechanical modeling, as in Baleani et al. [19], to optimize junction stability. Exploring adjuncts, such as vascularized fibular grafts, in high-risk cases may further reduce the incidence of delayed :union:s. Ultimately, our experience with SDNT affirms its potential as a robust, patient-centered strategy for lower limb reconstruction, balancing biological healing with mechanical support to improve outcomes in young sarcoma survivors.
Conclusion
Our findings underscore the potential of the SDNT as a reliable method for securing osteoarticular allografts in pediatric patients following lower limb tumor resection. With no instances of allograft fracture observed—aside from a single case of nail bending—this approach demonstrates strong mechanical stability. It promotes an effective host-graft :union:, even in the face of challenges such as delayed healing. By facilitating early weight-bearing and minimizing long-term risks such as stress shielding, SDNT emerges as a promising option for enhancing outcomes in limb-salvage surgery, ultimately supporting better functional recovery in young survivors of malignant bone tumors.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all ind ividual participants included in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Sam Aliliu Sami; Investigation: Sam Aliliu Sami, Khalil Kargar, and Amin Hamidzadeh Khiavi; Data curation: Amin Hamidzadeh Khiavi and Bushra Zareie; Formal analysis: Bushra Zareie; Writing the original draft: Amin Hamidzadeh Khiavi, Roshanak Shams, and Shahabaldin Beheshti Fard; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully acknowledge the contributions of all the patients who participated in this study, as well as the surgeons, nurses, and medical staff involved in study and the treatment provided. Special thanks to the multidisciplinary teams whose collaboration made the comprehensive management of these complex cases possible.
References
Limb-salvage surgery has transformed the treatment of malignant bone tumors in pediatric patients, becoming the preferred approach over amputation due to advancements in chemotherapy, imaging, and surgical techniques [1, 2]. These innovations have improved survival rates and functional outcomes, enabling patients to maintain limb function while effectively addressing aggressive tumors such as osteosarcoma and Ewing sarcoma [3]. However, reconstructing large bone defects following tumor resection in the lower extremity remains a complex challenge, particularly in growing children, where limb length and joint preservation are critical [4, 5].
The primary reconstruction options for these defects include biological approaches, such as autografts, allografts, or vascularized fibular grafts, as well as mechanical solutions like endoprostheses or allograft-prosthetic composites [3, 6, 7]. Each method has trade-offs: Biological reconstructions promote long-term integration but risk complications like non:union:, fracture, and infection, while mechanical options offer immediate stability but may fail over time due to wear or loosening [8]. Osteoarticular allografts, which preserve joint function by replacing both bone and articular surfaces, are particularly appealing for pediatric patients but are prone to mechanical failures, with reported fracture rates ranging from 8% to 29% and non:union: rates from 17% to 40% in the literature [4, 9].
Fixation techniques play a pivotal role in the success of allograft reconstruction. Intramedullary nailing (IMN) and plate fixation are commonly used, with nails offering advantages like easier alignment and early weight-bearing [10]. However, achieving stable yet dynamic fixation to promote bone :union: without stress-shielding remains a challenge [9]. Excessive rigidity can lead to negative bone remodeling, while inadequate stability increases the risk of fracture or non:union: [6, 9]. Recent studies have explored modifications, such as compressible nails or dynamic locking, to enhance :union: rates; however, data specific to pediatric populations are limited [11, 12].
This study introduces a novel stabilized dynamized nailing technique (SDNT) for fixing osteoarticular allografts in pediatric lower limb tumor resection. By combining IMN with controlled dynamization and antibiotic-soaked allografts, SDNT aims to optimize mechanical stability and bone :union: while minimizing complications. We present the outcomes of 40 pediatric patients treated with this approach, focusing on :union: time, complication rates, and functional prognosis to evaluate its efficacy in this challenging clinical scenario.
Methods
We conducted a retrospective chart review of 41 pediatric cases under limb-salvage surgery for malignant bone tumors of the lower extremity between 2014 and 2024 at our institution. The selection criteria were as follows: 1) tumors of the diaphyseal or metaphyseal location of a long bone (femur or tibia), with preservation of adjacent joints post-resection; 2) wide tumor resection with at least a 2-cm margin, confirmed by preoperative magnetic resonance imaging (MRI) and biopsy; and 3) a minimum postoperative follow-up of 12 months, with regular clinical and radiographic assessments. Diagnoses, confirmed by preoperative biopsy, included osteosarcoma, Ewing sarcoma, or chondrosarcoma. Patients with osteosarcoma or Ewing sarcoma received neo-adjuvant chemotherapy and radiotherapy, while those with chondrosarcoma received only postoperative adjuvant therapy.
Allograft preparation
Fresh frozen osteoarticular allografts (FFOAs) were sourced from a certified bone bank, stored in liquid nitrogen, and sterile-packaged without irradiation. Allografts were age-, size-, and side-matched to the recipient and thawed in 2 L of warm normal saline containing 800 mg of gentamicin immediately before surgery to reduce the risk of infection. To address potential limb length discrepancies in pediatric patients, allografts were selected to be 0.5–1 cm longer than the resected bone segment [13].
Surgical technique
Tumor resection was performed with a wide margin (≥2 cm) based on preoperative MRI planning [14]. After resection, we employed SDNT for allograft fixation. For distal femur or proximal tibia tumors, the host bone’s proximal or distal segment was reamed to accommodate a cloverleaf-slotted intramedullary nail, selected for compatibility with the host bone’s diameter and length. On a separate sterile table, the allograft was similarly reamed, and bone cement was injected into its medullary canal to secure the nail, ensuring a 1-cm cement-free zone at the allograft-host junction to facilitate bone :union:. The nail allograft was then inserted into the host bone, aligning the nail to bridge the resection gap. Soft tissue reconstruction included ligament and capsular repair around the knee, followed by standard layered wound closure with a drain and immobilization in a long leg splint.
Postoperative management
Patients began isometric exercises 1 week after surgery and passive functional exercises at 2 weeks, under the guidance of physiotherapists. They used braces and crutches, remaining non-weight-bearing for the first 6 weeks. Partial and full weight-bearing were introduced gradually after radiographic evidence of healing at the allograft-host junction, typically assessed at 6 and 12 weeks. Follow-up occurred at 6 weeks, 12 weeks, every 3 months for the first 2 years, every 6 months for the next 3 years, and annually thereafter. Evaluations included oncological status, bone :union: (defined as bridging bone across three cortices on anteroposterior and lateral radiographs or disappearance of the osteotomy line), and functional outcomes. Complications, such as non:union:, infection, fracture, or nail bending, were recorded, with the need for allograft removal or replacement considered a treatment failure.
Outcome assessment
We evaluated key outcomes, including time to :union:, complication rates (e.g. delayed :union:, infection, nail bending), disease relapse, metastasis, and mortality. Functional outcomes were assessed by range of motion and clinical symptoms, with radiographic assessments confirming bone healing and implant stability. Data were collected from medical records and analyzed to determine the efficacy of SDNT in achieving stable reconstruction and minimizing complications in this pediatric cohort.
Results
We analyzed data from 40 pediatric patients (Mean±SD age: 11.85±2.93 years) who underwent lower limb tumor resection and reconstruction with osteoarticular allografts fixed using the SDNT between 2014 and 2024. The cohort was predominantly male (68.29%, n=28), with a Mean±SD follow-up of 33.68±20.58 months. Tumors were primarily osteosarcoma (70.73%, n=29), followed by Ewing sarcoma (24.39%, n=10), chondrosarcoma (2.44%, n=1), and neuroblastoma (2.44%, n=1). Most tumors were located in the femur (65.85%, n=27) and the metaphyseal region (75.61%, n=31), with 68.29% (n=28) classified as stage II and 31.71% (n=13) as stage III (Table 1). Neoadjuvant chemotherapy was administered to 95% (n=38) of patients, and 39.02% (n=16) received neoadjuvant radiotherapy.
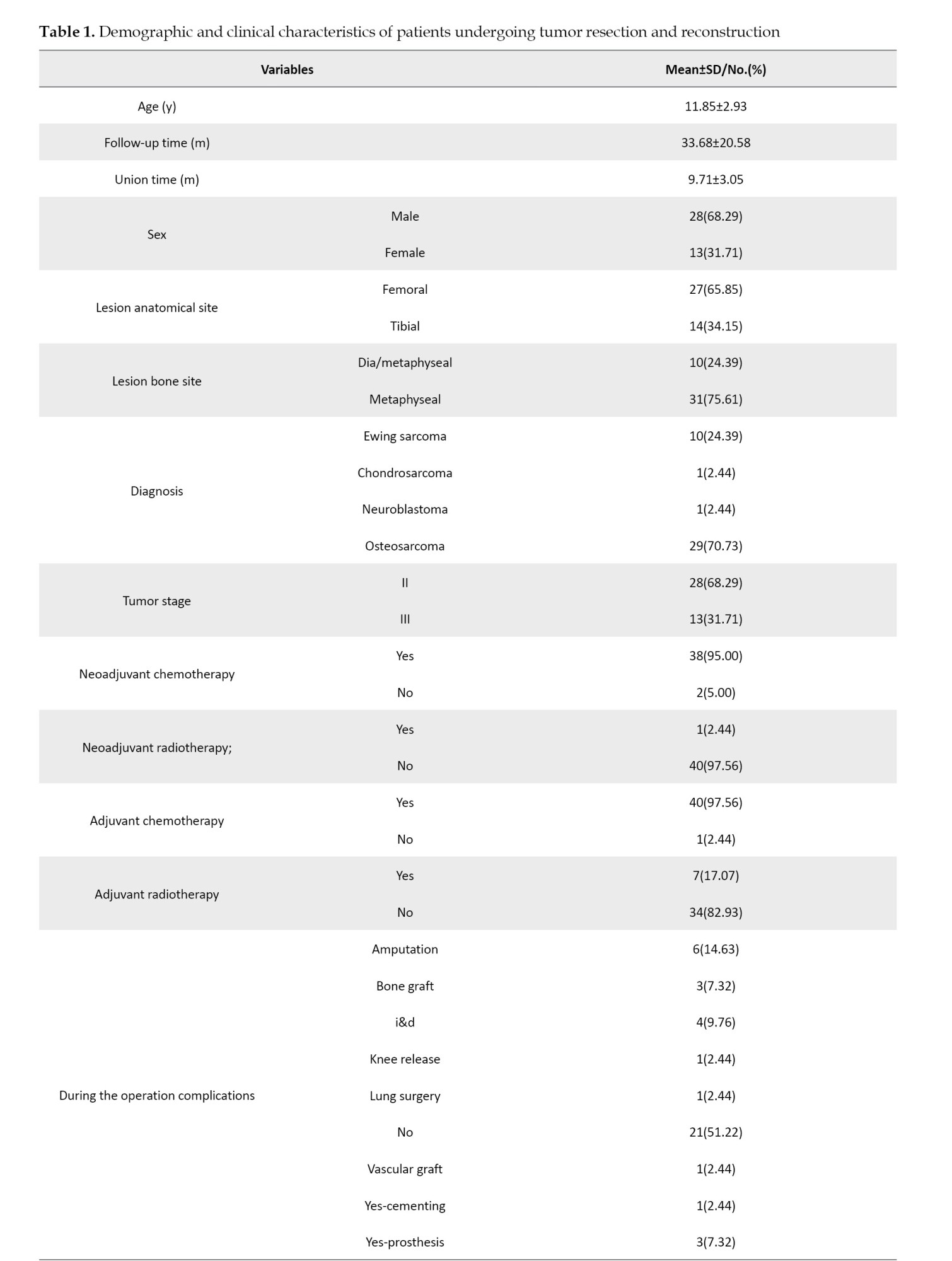

The Mean±SD time to bone :union: was 9.71±3.05 months, with successful allograft-host integration observed radiographically (Figures 1 and 2).
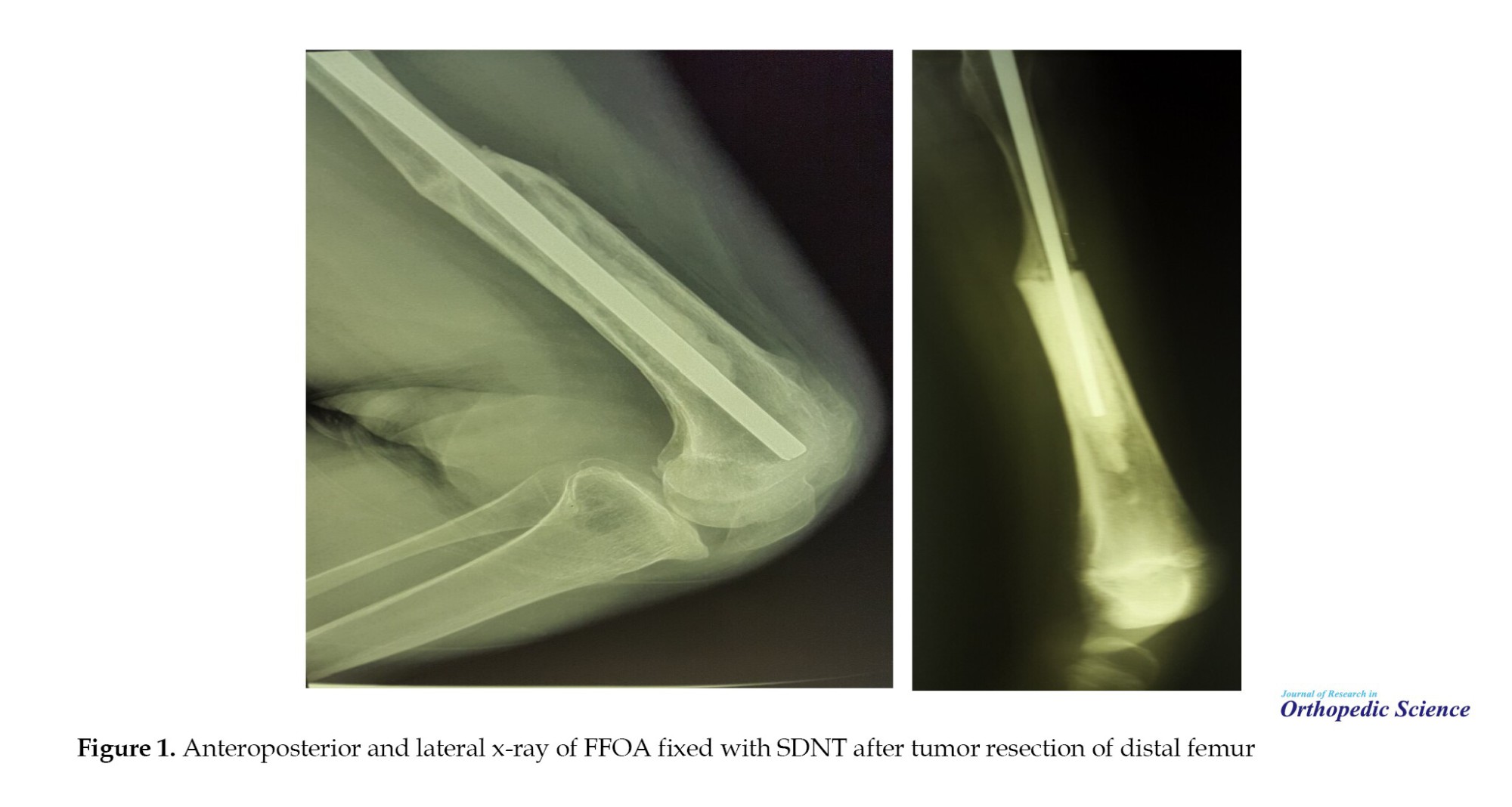
Postoperative complications occurred in 48.88% (n=20) of patients. Delayed :union: was the most common complication (24.39%, n=10), followed by infection (14.64%, n=6), drop foot (4.88%, n=2), nail bending (2.44%, n=1), non:union: (2.44%, n=1), and superficial wound issues (2.44%, n=1) (Table 2). Notably, no allograft fractures occurred, with nail bending being the only mechanical failure observed, as seen in postoperative radiographs of distal femur and proximal tibia reconstructions (Figure 1 for distal femur; Figure 2 for proximal tibia) [1]. Reoperations were required in 48.78% (n=20) of cases, including amputation (14.63%, n=6), bone grafting (7.32%, n=3), irrigation and debridement (9.76%, n=4), knee release (2.44%, n=1), lung surgery (2.44%, n=1), vascular grafting (2.44%, n=1), and prosthesis placement (7.32%, n=3). Intraoperative complications occurred in 12.2% (n=5) of cases.
Oncologic outcomes showed a mortality rate of 29.27% (n=12), with 70.73% (n=29) of patients alive at the last follow-up. Disease relapse occurred in 17.07% (n=7) of patients, and metastasis was observed in 36.58% (n=15), primarily to the lungs (26.83%, n=11), followed by lung and shoulder (4.88%, n=2), bone (2.44%, n=1), and brain-lung (2.44%, n=1) (Table 2). A limited range of motion was reported in 78.05% (n=32) of patients, potentially due to postoperative complications or disease progression. Detailed demographic and clinical characteristics are presented in Table 1, with complication and metastasis data summarized in Table 2.

Discussion
In this retrospective study of 41 pediatric patients undergoing limb-salvage surgery for malignant bone tumors in the lower extremities, we demonstrated that reconstruction using FFOA fixed with a SDNT offers a viable biological option for restoring limb function. The cohort, primarily consisting of young patients with osteosarcoma or Ewing sarcoma, achieved a mean :union: time of approximately 9.7 months, resulting in a low incidence of catastrophic failures. Notably, delayed :union: in 10 patients emerged as the most common complication (24.39%), yet the majority of these cases progressed to eventual :union: without requiring major revisions. Twenty-six patients (63.42%) showed no complications, while infection affected 14.64% of patients, and other issues, such as drop foot or superficial wounds, were infrequent. Critically, no outright allograft fractures occurred, with only one instance of nail bending (2.44%), underscoring the mechanical stability provided by SDNT. These outcomes align with the broader goal of limb-salvage procedures: preserving function while minimizing morbidity in a vulnerable population.
When contextualized within the existing literature on intercalary allograft reconstructions, our findings highlight both similarities and potential advantages of the SDNT approach. For instance, :union:-related challenges persist as a recurring theme across studies. According to a 2023 study by Goldin et al., the median time to fracture-free allograft survival was significantly extended in the IMN group compared to the extramedullary plating (EMP) group. However, other outcomes showed no major disparities between these fixation approaches [10]. Further breaking down the EMP cohort into single-plate (SP) and multiple-plate (MP) subgroups revealed that MP patients faced elevated fracture risks, more frequent revision procedures, and reduced overall allograft longevity. Key metrics from their IMN arm included a 21% non:union: rate across host-graft junctions, 24% fracture occurrence, a median fracture-free survival of 7.9 years, 18% infection prevalence, 82% allograft retention at last follow-up, and a 59% revision surgery rate [10]. By comparison, our investigation reported a mean follow-up of 33.7 months under IMN, where delayed :union: was the leading issue at 24.39%, trailed by infection at 14.64% and foot drop at 4.88%; less common problems encompassed nail bending (2.44%), non:union: (2.44%), and superficial wounds (2.44%), with over half (51.22%) of cases complication-free. In contrast to the Goldin study, in our research, delayed :union: was the most prominent complication (which ultimately united to the host bone), indicating that this method could have promising results. Fracture rates in our study were significantly lower than those in the Goldin study, primarily due to the application of SDNT.
Similarly, a systematic review by Jamshidi et al. [15] reported non:union: in 37% of IMN-fixed intercalary allografts, fractures in 5%, and infections in 4%, with no local recurrences. While our infection rate was higher (14.64%), possibly attributable to the pediatric cohort’s immunocompromised state from neoadjuvant therapies or the extensive soft tissue dissection around the knee, the fracture rate was halved, reinforcing SDNT’s role in enhancing construct durability.
For instance, the method we used reveals that broader comparisons show biological reconstructions compare favorably to mechanical alternatives in select scenarios. Techniques such as allograft-prosthetic composites or endoprostheses, as discussed by Othman et al. [16] in their meta-analysis, often yield higher early functionality but carry risks of aseptic loosening or periprosthetic fractures in the long term, particularly in growing children, where preservation of the growth plate is paramount. Frisoni et al. [17] noted non:union: and fractures as key factors contributing to poor function in femoral allografts. By incorporating dynamization, we showed that SDNT appears to mitigate these biomechanical pitfalls, fostering a more balanced load transfer that supports osteogenesis without excessive rigidity.
The oncologic outcomes in our study—29.27% mortality, 17.07% relapse, and metastasis in about a third of cases—reflect the aggressive nature of these tumors in children, consistent with reports from Liu et al. [18] and Yang et al. [14], where stage II/III sarcomas predominated. Neoadjuvant chemotherapy was administered to 95% of our patients, likely contributing to the wide margins and low local recurrence, though pulmonary metastases remained a concern (26.83%). These systemic challenges underscore that while SDNT excels in local reconstruction, multidisciplinary management is crucial for long-term survival.
Strengths of our approach include the detailed operative protocol, which standardizes cement augmentation for nail stability while preserving a cement-free zone at the junction to avoid interfering with :union:—a nuance not always emphasized in prior IMN descriptions. The mean follow-up of 33.7 months provides mid-term insights, and the focus on pediatric patients fills a gap in the literature, where most data derive from mixed-age cohorts. However, limitations must be acknowledged. As a single-center retrospective review, selection bias may influence results, and the sample size limits statistical power for subgroup analyses, such as by tumor site (femoral vs tibial). Variability in neoadjuvant regimens and the absence of patient-reported outcomes, such as quality-of-life scores, represent areas for improvement. Additionally, while SDNT minimized fractures, the higher infection rate compared to meta-analyses suggests opportunities to refine antibiotic prophylaxis or allograft preparation.
Looking ahead, prospective multicenter trials could validate SDNT’s benefits, possibly incorporating biomechanical modeling, as in Baleani et al. [19], to optimize junction stability. Exploring adjuncts, such as vascularized fibular grafts, in high-risk cases may further reduce the incidence of delayed :union:s. Ultimately, our experience with SDNT affirms its potential as a robust, patient-centered strategy for lower limb reconstruction, balancing biological healing with mechanical support to improve outcomes in young sarcoma survivors.
Conclusion
Our findings underscore the potential of the SDNT as a reliable method for securing osteoarticular allografts in pediatric patients following lower limb tumor resection. With no instances of allograft fracture observed—aside from a single case of nail bending—this approach demonstrates strong mechanical stability. It promotes an effective host-graft :union:, even in the face of challenges such as delayed healing. By facilitating early weight-bearing and minimizing long-term risks such as stress shielding, SDNT emerges as a promising option for enhancing outcomes in limb-salvage surgery, ultimately supporting better functional recovery in young survivors of malignant bone tumors.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all ind ividual participants included in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Sam Aliliu Sami; Investigation: Sam Aliliu Sami, Khalil Kargar, and Amin Hamidzadeh Khiavi; Data curation: Amin Hamidzadeh Khiavi and Bushra Zareie; Formal analysis: Bushra Zareie; Writing the original draft: Amin Hamidzadeh Khiavi, Roshanak Shams, and Shahabaldin Beheshti Fard; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors gratefully acknowledge the contributions of all the patients who participated in this study, as well as the surgeons, nurses, and medical staff involved in study and the treatment provided. Special thanks to the multidisciplinary teams whose collaboration made the comprehensive management of these complex cases possible.
References
- Grimer RJ, Taminiau AM, Cannon SR.Surgical outcomes in osteosarcoma. J Bone Joint Surg Br Vol. 2002; 84(3):395-400. [Link]
- Niculescu SA, Grecu AF, Gheonea C, Grecu DC. Limb salvage surgery in pediatric patients with osteosarcoma. Curr Health Sci J. 2024; 50(3):360-7. [PMID]
- Bus MP, Dijkstra PD, van de Sande MA, Taminiau AH, Schreuder HW, Jutte PC, et al. Intercalary allograft reconstructions following resection of primary bone tumors: A nationwide multicenter study. J Bone Joint Surg Am. 2014; 96(4):e26. [DOI:10.2106/JBJS.M.00655] [PMID]
- Sanders PTJ, Spierings JF, Albergo JI, Bus MPA, Fiocco M, Farfalli GL, et al. Long-term clinical outcomes of intercalary allograft reconstruction for lower-extremity bone tumors. J Bone Joint Surg Am. 2020; 102(12):10429. [DOI:10.2106/JBJS.18.00893] [PMID]
- Hasan BZ, Mesregah MK. Limb salvage in pediatrics with malignant bone tumors: Team approach to orthopedic oncology. EJMO. 2020; 4(1):26-34. [Link]
- Ortiz-Cruz E, Gebhardt MC, Jennings LC, Springfield DS, Mankin HJ. The results of transplantation of intercalary allografts after resection of tumors. A long-term follow-up study. J Bone Joint Surg Am. 1997; 79(1):97-106. [DOI:10.2106/00004623-199701000-00010] [PMID]
- van der Heijden L, Farfalli GL, Balacó I, Alves C, Salom M, Lamo-Espinosa JM, et al. Biology and technology in the surgical treatment of malignant bone tumours in children and adolescents, with a special note on the very young. J Child Orthop. 2021; 15(4):322-30. [DOI:10.1302/1863-2548.15.210095] [PMID]
- Houdek MT, Watts CD, Wyles CC, Rose PS, Taunton MJ, Sim FH. Functional and oncologic outcome of cemented endoprosthesis for malignant proximal femoral tumors. J Surg Oncol. 2016; 114(4):501-6. [DOI:10.1002/jso.24339] [PMID]
- Capanna R, Campanacci DA, Belot N, Beltrami G, Manfrini M, Innocenti M, et al. A new reconstructive technique for intercalary defects of long bones: The association of massive allograft with vascularized fibular autograft. Long-term results and comparison with alternative techniques. Orthop Clin North Am. 2007 ; 38(1):51-60, vi. [DOI:10.1016/j.ocl.2006.10.008] [PMID]
- Goldin AN, Johnson SR, Hajdu KS, Kowalski BL, Volkmar AJ, Moran CP, et al. Surgical Fixation method in lower extremity intercalary allograft reconstruction after oncologic resection: A comparison of plates and nails. J Am Acad Orthop Surg. 2023; 31(16):881-92. [DOI:10.5435/JAAOS-D-23-00025] [PMID]
- Miller BJ, Virkus WW. Intercalary allograft reconstructions using a compressible intramedullary nail: A preliminary report. Clin Orthop Relat Res. 2010; 468(9):2507-13. [DOI:10.1007/s11999-010-1260-5] [PMID]
- Errani C, Tsukamoto S, Almunhaisen N, Mavrogenis A, Donati D. Intercalary reconstruction following resection of diaphyseal bone tumors: A systematic review. J Clin Orthop Trauma. 2021; 19:1-10. [DOI:10.1016/j.jcot.2021.04.033] [PMID]
- Ng VY, Louie P, Punt S, Conrad EU. Allograft Reconstruction for Sarcomas of the Tibia. Open Orthop J. 2017; 11:189-94. [DOI:10.2174/1874325001711010189] [PMID]
- Yang J, Li W, Feng R, Li D. Intercalary frozen autografts for reconstruction of bone defects following meta-/diaphyseal tumor resection at the extremities. BMC Musculoskelet Disord. 2022; 23(1):890. [DOI:10.1186/s12891-022-05840-6] [PMID]
- Jamshidi K, Bahardoust M, Karimi Behnagh A, Bagherifard A, Mirzaei A. How the choice of osteosynthesis affects the complication rate of intercalary allograft reconstruction? A systematic review and meta-analysis. Indian J Orthop. 2021; 56(4):547-58. [DOI:10.1007/s43465-021-00563-7] [PMID]
- Othman S, Bricker JT, Azoury SC, Elfanagely O, Weber KL, Kovach SJ. Allograft alone vs. allograft with intramedullary vascularized fibular graft for lower extremity bone cancer: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2020; 73(7):1221-31. [DOI:10.1016/j.bjps.2020.02.030] [PMID]
- Frisoni T, Cevolani L, Giorgini A, Dozza B, Donati DM. Factors affecting outcome of massive intercalary bone allografts in the treatment of tumours of the femur. J Bone Joint Surg Br. 2012; 94(6):836-41. [DOI:10.1302/0301-620X.94B6.28680] [PMID]
- Liu Q, Long F, Zhang C, Liu Y, He H, Luo W. Biological reconstruction of bone defect after resection of malignant bone tumor by allograft: A single-center retrospective cohort study. World J Surg Oncol. 2023; 21(1):234. [DOI:10.1186/s12957-023-03121-7] [PMID]
- Baleani M, Erani P, Blaise M, Fognani R, Palmas M, Manfrini M. Intercalary reconstruction of long bones by massive allograft: Comparison of construct stability ensured by three different host-graft junctions and two types of fixations in a synthetic femur model. Front Pediatr. 2022; 10:868299. [DOI:10.3389/fped.2022.868299] [PMID]
Type of Study: Research Article |
Subject:
Tumor surgery
Received: 2025/08/26 | Accepted: 2025/09/27 | Published: 2024/11/20
Received: 2025/08/26 | Accepted: 2025/09/27 | Published: 2024/11/20
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






