Volume 11, Issue 1 (2-2024)
JROS 2024, 11(1): 43-50 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hajialiloo Sami S, Kargar K, Zareie B, Shams R, Hamidzadeh Khiavi A. Outcomes of Shelf Procedure in Acetabulum Reconstruction for Preventing Hip Dislocation Following Proximal Femur Tumor Resection. JROS 2024; 11 (1) :43-50
URL: http://jros.iums.ac.ir/article-1-2277-en.html
URL: http://jros.iums.ac.ir/article-1-2277-en.html
1- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
2- Department of Orthopedics, Bone and Joint Reconstruction Research Center, School of Medicine, Iran University of Medical Sciences, Tehran, Iran. & Department of Orthopedic Surgery, Faculty of Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran.
Full-Text [PDF 518 kb]
(250 Downloads)
| Abstract (HTML) (966 Views)
Full-Text: (186 Views)
Introduction
Primary and metastatic bone tumors often affect the proximal femur, making it the third most common site for metastatic disease after the lungs and liver [1, 2]. The proximal femur is also the most frequently affected long bone with metastatic tumors [3, 4]. Treatment primarily aims to alleviate pain and enhance the patient’s quality of life [3]. Osteosarcomas and Ewing’s sarcomas are the most common primary bone tumors arising in the lower limbs [5, 6]. Previously, amputation was the primary treatment method, significantly affecting patient function and well-being [6]. Limb salvage surgery (LSS) is now the preferred approach for treating lower limb bone sarcomas, offering various reconstructive techniques, such as biological and endoprosthetic methods [2, 6]. Over the past few decades, various reconstructive options for LSS following oncological treatment have been developed. These options can be broadly categorized into biological, endoprosthetic, and composite reconstructions. Biological reconstructions involve techniques, such as allografts, vascularized autografts (including bone grafts, flaps, or free flaps), non-vascularized bone autografts, extracorporeal radiation, and segmental bone transport. Endoprosthetic, or non-biological reconstructions, utilize metal prostheses, 3D-printed implants, and expandable endoprostheses [6, 7]. Reconstruction of the bone defect is necessary after tumor resection with LSS. Advances in metallurgy and implant design have made megaprosthetic reconstruction more effective and widely accepted, particularly for patients with bone metastases or at risk of pathological fractures [1, 8]. Moreover, the improved survival rates among patients with bone metastases, combined with the common failure of fixation devices in this area, have resulted in the widespread adoption of megaprosthetic reconstruction for treating impending or existing pathological fractures [1, 9].
However, although modern modular mega prostheses are undoubtedly an advancement over older custom-made versions, they are more expensive than traditional internal fixation methods and are still associated with complications [1]. Reconstructing the hip while preserving it for patients with extremely short proximal femur segments after extensive tumor resection in the femoral diaphysis is a highly challenging procedure [10]. On the other hand, advances in cancer treatments have led to longer survival rates, resulting in a growing number of patients with skeletal metastases who experience fractures or impending fractures, particularly in the proximal femur. These skeletal complications significantly impair the patient’s quality of life. Fracture healing is often compromised in diseased or irradiated bone, and surgeons must consider the possibility that these fractures may not heal properly [3]. Consequently, there has been a rise in the use of excision and proximal femoral replacement (PFR) to treat these lesions, with most procedures being carried out at specialized regional sarcoma centers [1]. Patients who undergo extensive tumor resection and total femur replacement (TFR) are at a high risk of complications, such as hip dislocation and infection, which frequently necessitate multiple implant revisions or even hip disarticulation. These issues can severely affect their independence and overall prognosis. Furthermore, their reduced life expectancy is influenced by difficulties in achieving complete local tumor removal and controlling metastatic spread [11]. The five primary complications associated with hemiarthroplasty or standard hip arthroplasty following PFR include infections, dislocations, acetabular wear, deep vein thrombosis, and aseptic loosening [2, 3, 12-14].
Dislocation is the most frequent and challenging complication after both proximal and total femur endoprosthetic reconstruction [7, 15, 16]. Preserving the abductor muscles and achieving a wide tumor resection margin can help prevent postoperative dislocation and local recurrence [11]. Several factors, such as the surgical technique, the condition of the abductor muscles, prior hip surgeries, and the positioning of the implant components, are recognized as key contributors influencing the dislocation rate [2]. Hemiarthroplasty megaprosthetic reconstruction of the proximal femur following tumor resection is a widely used procedure in orthopedic oncology [8]. Dislocation rates are reportedly lower in patients undergoing proximal femoral hemiarthroplasty compared to those receiving hip arthroplasty for neoplastic conditions [17]. PFR is a salvage procedure initially developed for reconstruction after sarcoma or metastatic cancer resection. These techniques can also be adapted for non-oncologic cases involving significant proximal bone loss [18, 19]. This study aimed to assess the treatment outcomes of patients who underwent proximal femoral or total femoral resection due to bone and soft tissue tumors, followed by endoprosthetic reconstruction using a bipolar hemiarthroplasty type of hip articulation [20]. To contribute to the existing literature, this study seeks to report the survival and functional outcomes of a cohort of patients who underwent proximal femoral resection and reconstruction with a modular resection prosthesis, while also evaluating implant-related survival and complications.
Methods
Study design and eligibility criteria
This retrospective, single-center cohort study analyzed data from 34 patients who underwent bipolar femur replacement with cemented shelf procedures following proximal femoral tumor resection. Inclusion criteria comprised patients diagnosed with proximal femoral tumors who underwent hip replacement after tumor resection. Exclusion criteria included revision surgeries and patients unavailable for follow-up. Two patients were lost to follow-up before six months, leaving 32 patients for analysis. Data were collected from tumor databases, operating records, prosthesis registries, and pathology reports.
Data collection and outcome measures
Demographic information, lesion characteristics, and follow-up duration were documented. The primary outcome was the dislocation rate, while secondary outcomes included fractures, infections, and implant survival. Functional outcomes were assessed using the Musculoskeletal Tumor Society (MSTS) scoring system, which evaluates pain, activity, emotional acceptance, brace use, walking ability, and gait. Each category was rated on a 5-point scale, with a maximum total score of 30 (100%), where higher scores indicate better functional outcomes [21].
Surgical procedure
All patients underwent a core needle biopsy prior to definitive tumor resection. Surgeries were performed in clean-air operating rooms with antibiotic prophylaxis by an experienced orthopedic oncology team. Resection methods for metastatic lesions mirrored those for primary tumors, aiming for wide soft tissue margins while preserving key neurovascular structures to optimize functional outcomes. The femur was reconstructed using cemented bipolar femur replacements, allowing for the reattachment of the gluteus medius and minimus to preserve abductor function. In cases where the greater trochanter was unsalvageable, soft tissue reconstruction was performed. Postoperatively, patients were closely monitored before initiating weight-bearing rehabilitation.
Statistical analysis
Continuous variables, including MSTS scores and implant survival, were presented as Mean±SD. Categorical variables, such as complications and survivorship, were expressed as counts with percentages. Statistical significance was set at P<0.05. SPSS software version 26 (IBM, Armonk, NY, USA) was used for data analysis. Inter-observer agreement for functional and radiographic measurements was assessed using the concordance correlation coefficient, with mean results used for final analysis to minimize variability [21].
Study questions
1. What are the revision-free and overall implant survival rates of conventional bipolar femur replacements with cemented shelf procedures in patients treated for sarcoma?
2. How frequently do dislocations occur following these procedures?
Results
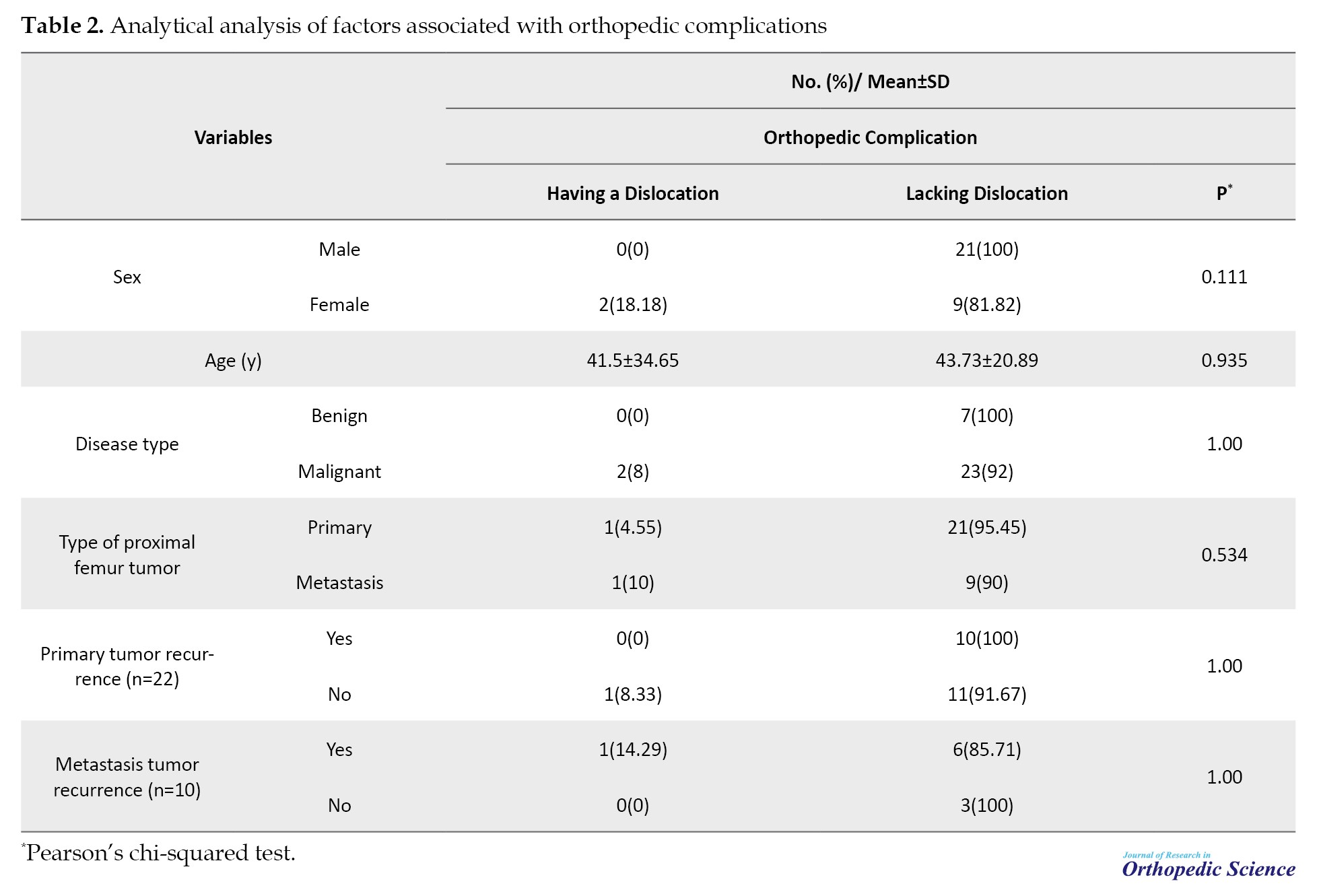
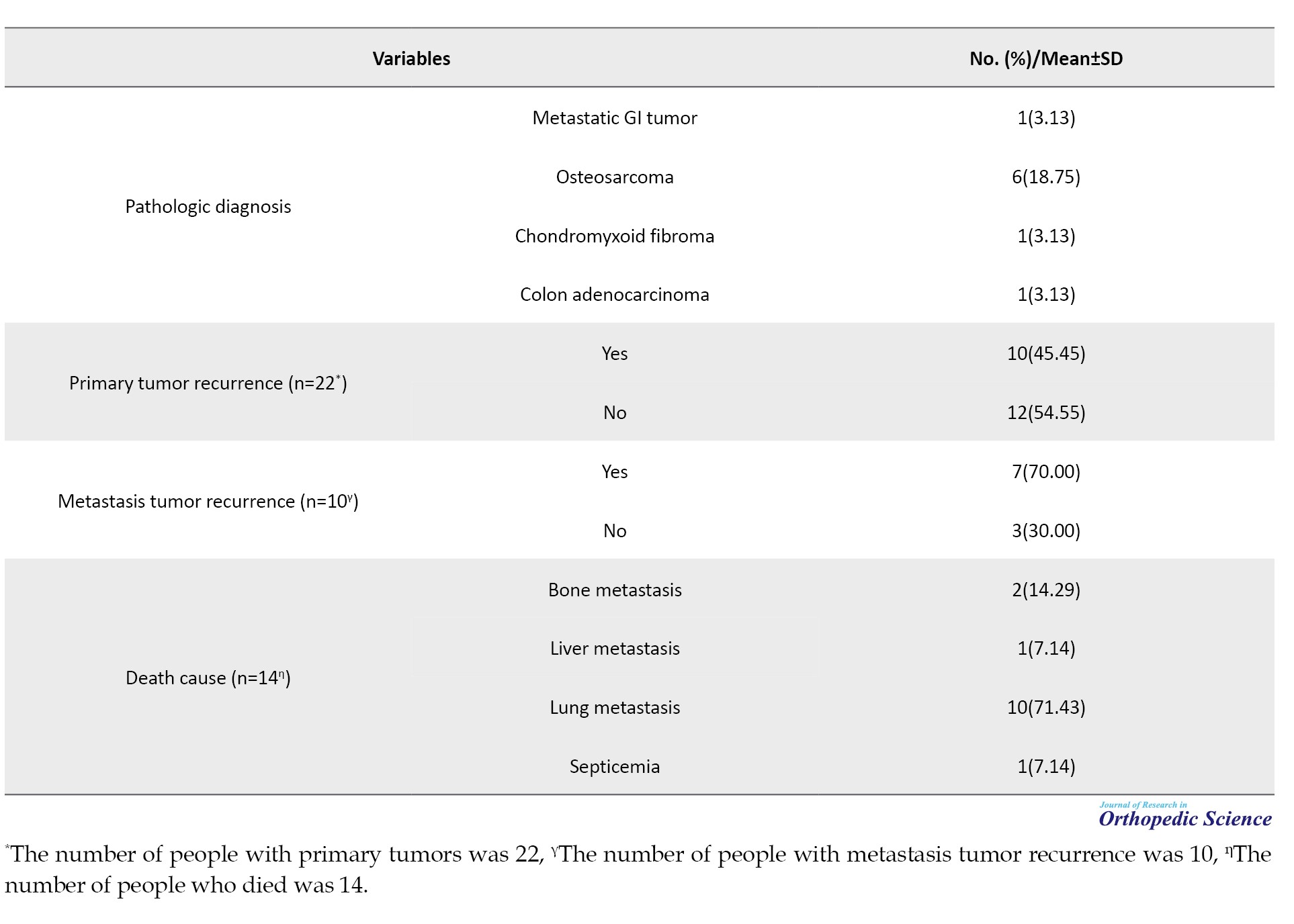
The study included a total of 32 patients, with a gender distribution of 21 males (65.63%) and 11 females (34.38%). The mean follow-up period for these patients was approximately 77.46±57.52 months (range: 7 to 216 months). Of these patients, 68.75% had primary tumors, while the remaining 31.25% presented with metastatic disease. Tumor recurrence rates were approximately 45% for primary cases and 70% for metastatic cases. Orthopedic complications were observed in 25 patients (78.1%) who did not experience any complications, three patients (9.4%) with fractures, two patients (6.3%) with dislocations, and two patients (6.3%) with infections. Chondrosarcoma and osteosarcoma each accounted for about 19% of the pathological diagnoses. Table 1 provides additional details, including biopsy results, metastasis, type of shelf, cause of death, and oncology-related complications.
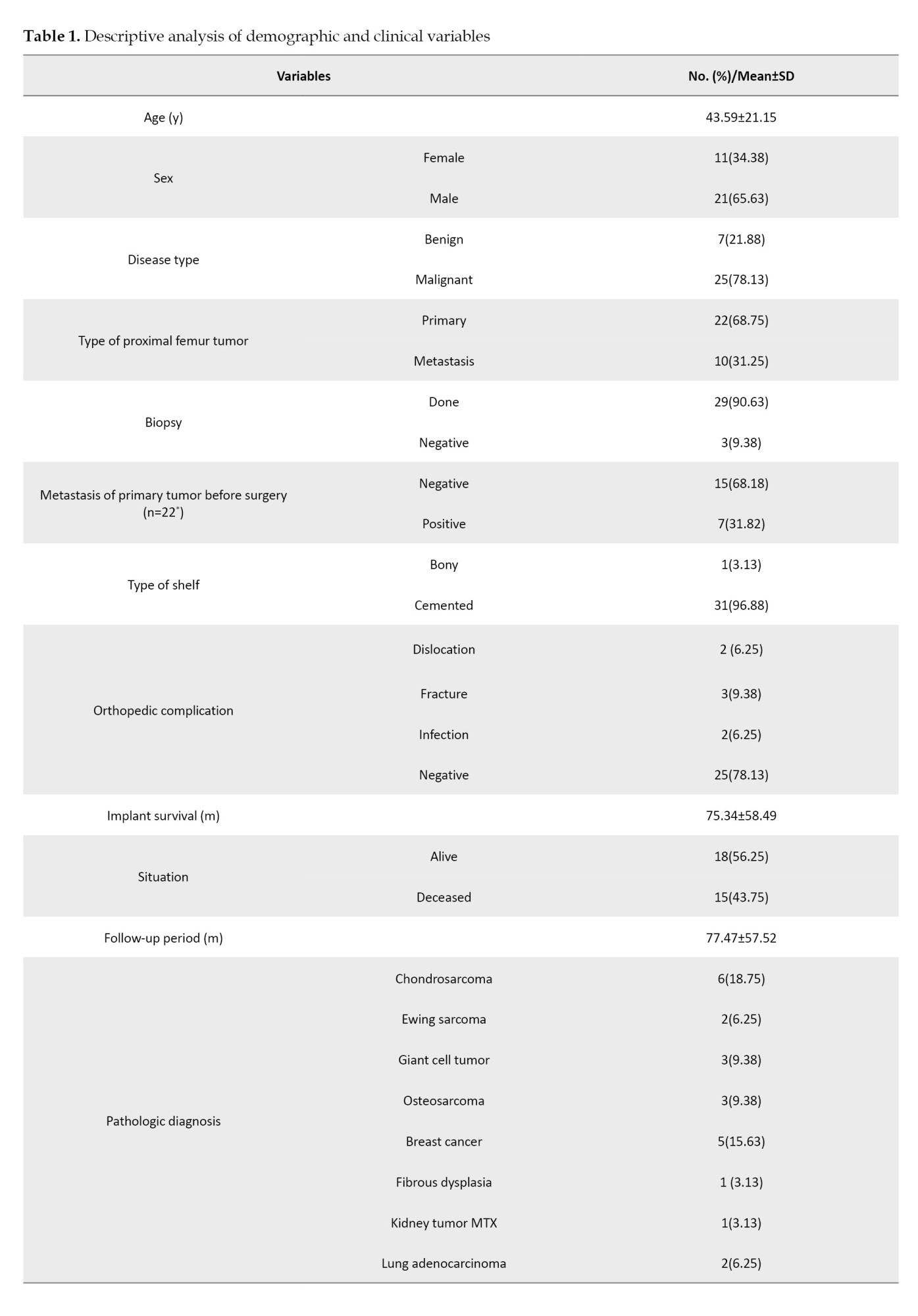
The mean implant survival was 75.34±58.49 months. Among the 14 patients who died, lung metastasis was the leading cause of death, accounting for 71.43% of cases, highlighting its significant impact on mortality in this group.
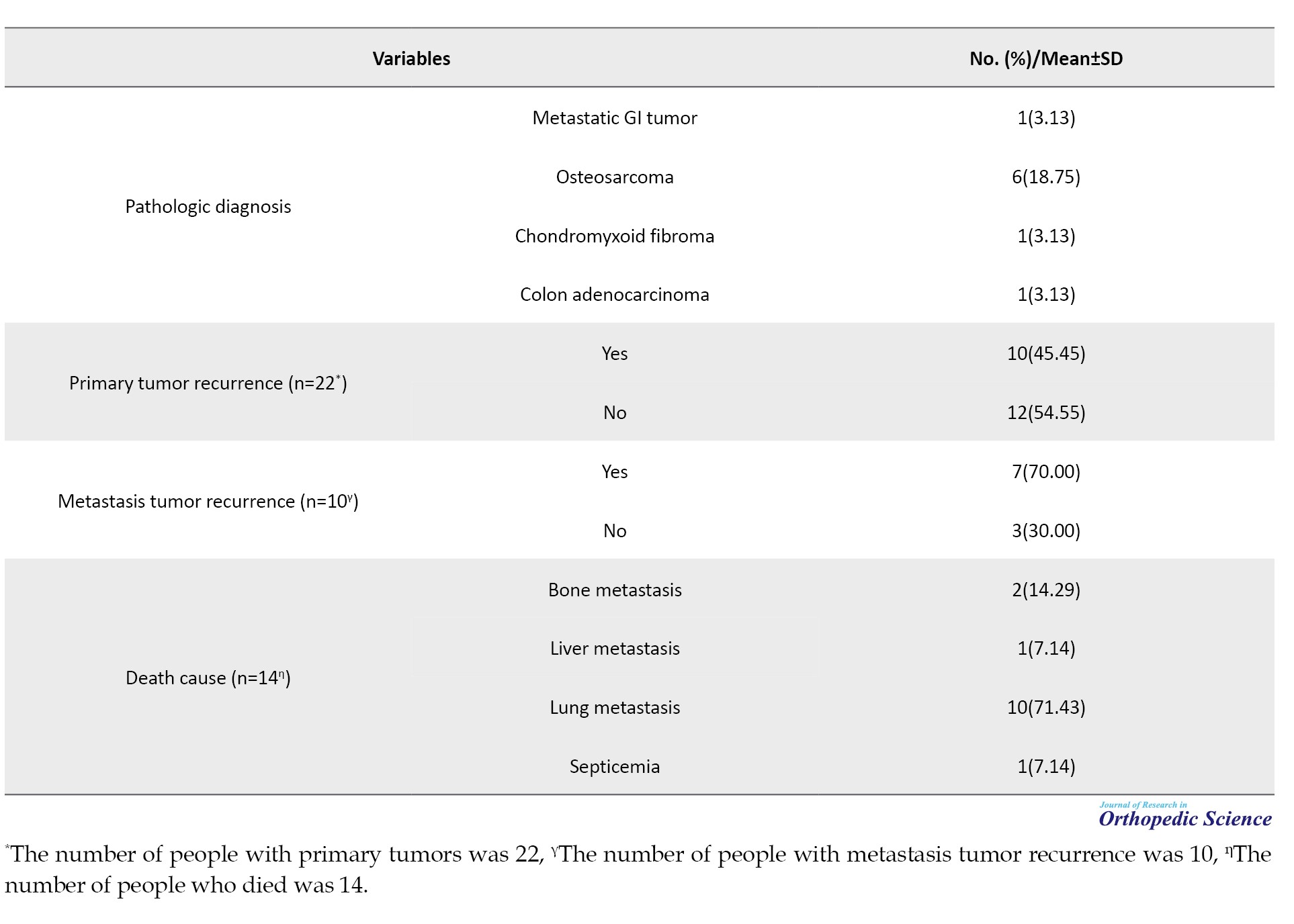
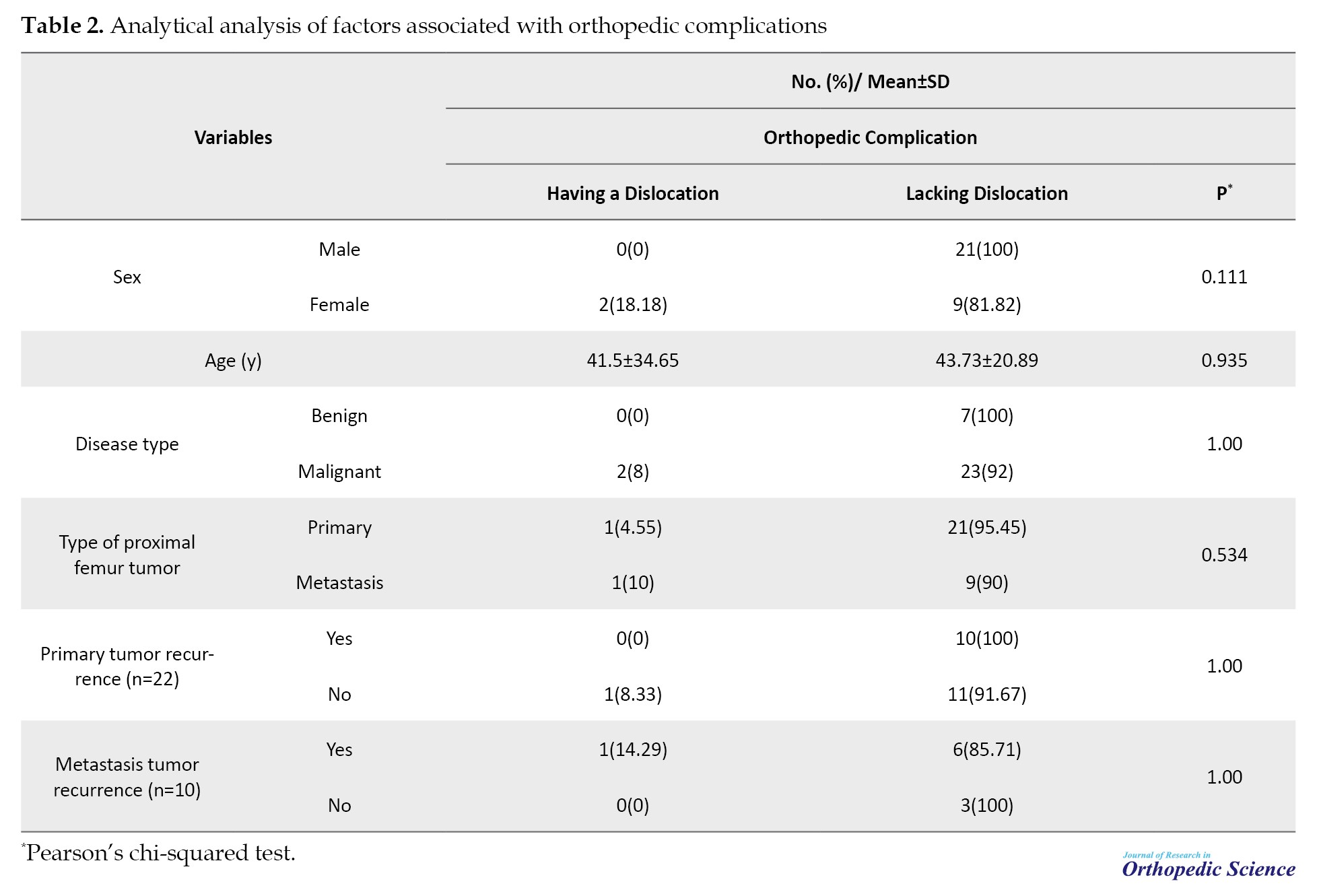
The study also analyzed the distribution of gender, mean age, recurrence of primary and metastatic tumors, and the type of proximal femur tumor based on the presence or absence of dislocation using two-way tables. No statistically significant differences were found between these variables and the occurrence of dislocation. The mean age of patients who experienced dislocation was 41.5±34.65 years, while those without dislocation had a mean age of 43.7±20.89 years. Dislocation occurred in 8% of patients without primary tumor recurrence, but no dislocations were observed in patients with primary tumor recurrence. Additionally, dislocation was reported in over 14% of patients with metastatic tumor recurrence, while none of the patients without metastatic tumor recurrence experienced dislocation. Overall, there was no significant correlation between primary or metastatic tumor recurrence and the presence of dislocation (P=1.00) (Table 2).
Discussion
This study evaluated the clinical outcomes of acetabulum reconstruction using the shelf procedure in patients undergoing bipolar hemiarthroplasty following proximal femoral tumor resection. The findings demonstrate that this approach provides favorable functional outcomes, with a notably low dislocation rate of 6.3%, which is significantly lower than rates reported in previous studies. For instance, Ashford et al. reported a dislocation rate of 35% in patients undergoing PFR. The reduced dislocation rate in our cohort can be attributed to the meticulous surgical technique, including preservation of the acetabulum, capsulorrhaphy, and reconstruction of the abductor mechanism, which collectively enhance hip stability, as reported by Bickels et al. in 2000 [1, 15]. The functional outcomes, as assessed by the MSTS scoring system, further underscore the efficacy of this approach. The ability to reattach the gluteus medius and minimus during the reconstruction of the bone plays a critical role in maintaining abductor function, which is essential for gait and overall hip stability [17]. This is particularly important in patients with extensive proximal femoral resections, where abductor function is often compromised. The use of cemented bipolar femur replacements provides immediate stability, which is advantageous in patients with metastatic disease or those at risk of pathological fractures [9]. Orthopedic complications, including fractures and infections, were observed in a small percentage of cases, consistent with the known risks associated with endoprosthetic reconstruction [11, 12]. However, the absence of a significant correlation between tumor recurrence and dislocation suggests that the surgical technique and implant positioning are more critical determinants of stability than the oncological status of the patient. This finding highlights the importance of surgical precision and the role of the shelf procedure in achieving stable hip articulation, even in cases with aggressive tumor biology. The high rate of lung metastasis as the leading cause of death (71.43%) in this study underscores the aggressive nature of metastatic bone disease and the importance of systemic oncological management in these patients [4]. Despite this, the low dislocation rate and satisfactory functional outcomes indicate that bipolar hemiarthroplasty with acetabulum reconstruction remains a viable option for improving the quality of life in patients with limited life expectancy. This is particularly relevant given the growing emphasis on palliative care and the need to balance oncological control with functional restoration in patients with advanced disease [5, 6]. In comparison to total hip replacement, bipolar hemiarthroplasty with the shelf procedure offers enhanced stability and a lower risk of dislocation, making it particularly suitable for patients with extensive proximal femoral resections [20]. The findings of this study align with recent literature supporting the use of bipolar hemiarthroplasty in oncological reconstructions, reinforcing its role as a reliable method for hip articulation in complex cases [21]. The modular design of modern endoprostheses allows for customization based on the extent of resection, further enhancing their utility in LSS [8].
Conclusion
In conclusion, this study provides robust evidence that bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure is a safe and effective option for patients undergoing proximal femoral resection due to musculoskeletal tumors. The low dislocation rate, combined with satisfactory functional outcomes, supports its use as a preferred method for hip reconstruction in this challenging patient population. Future studies with larger cohorts and longer follow-up periods are warranted to further validate these findings and refine surgical techniques for optimizing outcomes in orthopedic oncology.
Limitations
While this study provides valuable insights into the outcomes of bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure, several limitations should be acknowledged. First, the retrospective design introduces potential biases in data collection and analysis, as it relies on historical records and may lack standardized follow-up protocols. Second, the relatively small sample size (n=32) limits the generalizability of the findings and reduces the statistical power to detect significant associations, particularly for rare complications, such as dislocations or infections. Third, the single-center nature of the study may limit the external validity of the results, as surgical techniques and patient populations can vary across institutions. Fourth, the mean follow-up period of 77.46 months, while substantial, may not capture long-term complications, such as late implant failure or acetabular erosion, which could emerge beyond this timeframe. Finally, the study did not include a control group undergoing alternative reconstruction methods, such as total hip arthroplasty, which limits the ability to directly compare outcomes between different surgical approaches. Addressing these limitations in future prospective, multicenter studies with larger cohorts and longer follow-up periods would strengthen the evidence supporting this technique.
Future directions
Building on the findings of this study, several avenues for future research can further enhance the understanding and application of bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure. First, prospective, multicenter studies with larger patient cohorts are needed to validate the low dislocation rates and favorable functional outcomes observed in this study. Such studies would provide stronger evidence and improve the generalizability of the results across diverse patient populations and surgical settings. Second, comparative studies between bipolar hemiarthroplasty and total hip arthroplasty in the context of proximal femoral tumor resection would provide valuable insights into the relative advantages and disadvantages of each approach. This would help surgeons make more informed decisions based on patient-specific factors, such as tumor biology, life expectancy, and functional demands. Third, biomechanical studies could explore the role of implant design and surgical techniques in enhancing hip stability and reducing complications. For example, investigating the impact of modular prostheses, custom implants, or alternative fixation methods could lead to innovations that further improve outcomes. Finally, the integration of advanced imaging and navigation technologies into surgical planning and execution could enhance the precision of tumor resection and implant placement, potentially reducing complications and improving functional outcomes. The use of 3D-printed patient-specific implants and biomaterials or augmented reality-guided surgery represents promising areas for future exploration.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1403.859). Informed consent was obtained from all participants included in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Sam Hajialiloo Sami; Investigation: Sam Hajialiloo Sami, Khalil Kargar, and Amin Hamidzadeh Khiavi; Data curation: Amin Hamidzadeh Khiavi, and Bushra Zareie; Formal analysis: Bushra Zareie; Writing the original draft: Amin Hamidzadeh Khiavi, and Roshanak Shams; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors gratefully acknowledge the contributions of all the patients who participated in this study, as well as the surgeons, nurses, and medical staff involved in the care and treatment provided. Special thanks to the multidisciplinary teams whose collaboration made the comprehensive management of these complex cases possible.
References
Primary and metastatic bone tumors often affect the proximal femur, making it the third most common site for metastatic disease after the lungs and liver [1, 2]. The proximal femur is also the most frequently affected long bone with metastatic tumors [3, 4]. Treatment primarily aims to alleviate pain and enhance the patient’s quality of life [3]. Osteosarcomas and Ewing’s sarcomas are the most common primary bone tumors arising in the lower limbs [5, 6]. Previously, amputation was the primary treatment method, significantly affecting patient function and well-being [6]. Limb salvage surgery (LSS) is now the preferred approach for treating lower limb bone sarcomas, offering various reconstructive techniques, such as biological and endoprosthetic methods [2, 6]. Over the past few decades, various reconstructive options for LSS following oncological treatment have been developed. These options can be broadly categorized into biological, endoprosthetic, and composite reconstructions. Biological reconstructions involve techniques, such as allografts, vascularized autografts (including bone grafts, flaps, or free flaps), non-vascularized bone autografts, extracorporeal radiation, and segmental bone transport. Endoprosthetic, or non-biological reconstructions, utilize metal prostheses, 3D-printed implants, and expandable endoprostheses [6, 7]. Reconstruction of the bone defect is necessary after tumor resection with LSS. Advances in metallurgy and implant design have made megaprosthetic reconstruction more effective and widely accepted, particularly for patients with bone metastases or at risk of pathological fractures [1, 8]. Moreover, the improved survival rates among patients with bone metastases, combined with the common failure of fixation devices in this area, have resulted in the widespread adoption of megaprosthetic reconstruction for treating impending or existing pathological fractures [1, 9].
However, although modern modular mega prostheses are undoubtedly an advancement over older custom-made versions, they are more expensive than traditional internal fixation methods and are still associated with complications [1]. Reconstructing the hip while preserving it for patients with extremely short proximal femur segments after extensive tumor resection in the femoral diaphysis is a highly challenging procedure [10]. On the other hand, advances in cancer treatments have led to longer survival rates, resulting in a growing number of patients with skeletal metastases who experience fractures or impending fractures, particularly in the proximal femur. These skeletal complications significantly impair the patient’s quality of life. Fracture healing is often compromised in diseased or irradiated bone, and surgeons must consider the possibility that these fractures may not heal properly [3]. Consequently, there has been a rise in the use of excision and proximal femoral replacement (PFR) to treat these lesions, with most procedures being carried out at specialized regional sarcoma centers [1]. Patients who undergo extensive tumor resection and total femur replacement (TFR) are at a high risk of complications, such as hip dislocation and infection, which frequently necessitate multiple implant revisions or even hip disarticulation. These issues can severely affect their independence and overall prognosis. Furthermore, their reduced life expectancy is influenced by difficulties in achieving complete local tumor removal and controlling metastatic spread [11]. The five primary complications associated with hemiarthroplasty or standard hip arthroplasty following PFR include infections, dislocations, acetabular wear, deep vein thrombosis, and aseptic loosening [2, 3, 12-14].
Dislocation is the most frequent and challenging complication after both proximal and total femur endoprosthetic reconstruction [7, 15, 16]. Preserving the abductor muscles and achieving a wide tumor resection margin can help prevent postoperative dislocation and local recurrence [11]. Several factors, such as the surgical technique, the condition of the abductor muscles, prior hip surgeries, and the positioning of the implant components, are recognized as key contributors influencing the dislocation rate [2]. Hemiarthroplasty megaprosthetic reconstruction of the proximal femur following tumor resection is a widely used procedure in orthopedic oncology [8]. Dislocation rates are reportedly lower in patients undergoing proximal femoral hemiarthroplasty compared to those receiving hip arthroplasty for neoplastic conditions [17]. PFR is a salvage procedure initially developed for reconstruction after sarcoma or metastatic cancer resection. These techniques can also be adapted for non-oncologic cases involving significant proximal bone loss [18, 19]. This study aimed to assess the treatment outcomes of patients who underwent proximal femoral or total femoral resection due to bone and soft tissue tumors, followed by endoprosthetic reconstruction using a bipolar hemiarthroplasty type of hip articulation [20]. To contribute to the existing literature, this study seeks to report the survival and functional outcomes of a cohort of patients who underwent proximal femoral resection and reconstruction with a modular resection prosthesis, while also evaluating implant-related survival and complications.
Methods
Study design and eligibility criteria
This retrospective, single-center cohort study analyzed data from 34 patients who underwent bipolar femur replacement with cemented shelf procedures following proximal femoral tumor resection. Inclusion criteria comprised patients diagnosed with proximal femoral tumors who underwent hip replacement after tumor resection. Exclusion criteria included revision surgeries and patients unavailable for follow-up. Two patients were lost to follow-up before six months, leaving 32 patients for analysis. Data were collected from tumor databases, operating records, prosthesis registries, and pathology reports.
Data collection and outcome measures
Demographic information, lesion characteristics, and follow-up duration were documented. The primary outcome was the dislocation rate, while secondary outcomes included fractures, infections, and implant survival. Functional outcomes were assessed using the Musculoskeletal Tumor Society (MSTS) scoring system, which evaluates pain, activity, emotional acceptance, brace use, walking ability, and gait. Each category was rated on a 5-point scale, with a maximum total score of 30 (100%), where higher scores indicate better functional outcomes [21].
Surgical procedure
All patients underwent a core needle biopsy prior to definitive tumor resection. Surgeries were performed in clean-air operating rooms with antibiotic prophylaxis by an experienced orthopedic oncology team. Resection methods for metastatic lesions mirrored those for primary tumors, aiming for wide soft tissue margins while preserving key neurovascular structures to optimize functional outcomes. The femur was reconstructed using cemented bipolar femur replacements, allowing for the reattachment of the gluteus medius and minimus to preserve abductor function. In cases where the greater trochanter was unsalvageable, soft tissue reconstruction was performed. Postoperatively, patients were closely monitored before initiating weight-bearing rehabilitation.
Statistical analysis
Continuous variables, including MSTS scores and implant survival, were presented as Mean±SD. Categorical variables, such as complications and survivorship, were expressed as counts with percentages. Statistical significance was set at P<0.05. SPSS software version 26 (IBM, Armonk, NY, USA) was used for data analysis. Inter-observer agreement for functional and radiographic measurements was assessed using the concordance correlation coefficient, with mean results used for final analysis to minimize variability [21].
Study questions
1. What are the revision-free and overall implant survival rates of conventional bipolar femur replacements with cemented shelf procedures in patients treated for sarcoma?
2. How frequently do dislocations occur following these procedures?
Results
The study included a total of 32 patients, with a gender distribution of 21 males (65.63%) and 11 females (34.38%). The mean follow-up period for these patients was approximately 77.46±57.52 months (range: 7 to 216 months). Of these patients, 68.75% had primary tumors, while the remaining 31.25% presented with metastatic disease. Tumor recurrence rates were approximately 45% for primary cases and 70% for metastatic cases. Orthopedic complications were observed in 25 patients (78.1%) who did not experience any complications, three patients (9.4%) with fractures, two patients (6.3%) with dislocations, and two patients (6.3%) with infections. Chondrosarcoma and osteosarcoma each accounted for about 19% of the pathological diagnoses. Table 1 provides additional details, including biopsy results, metastasis, type of shelf, cause of death, and oncology-related complications.
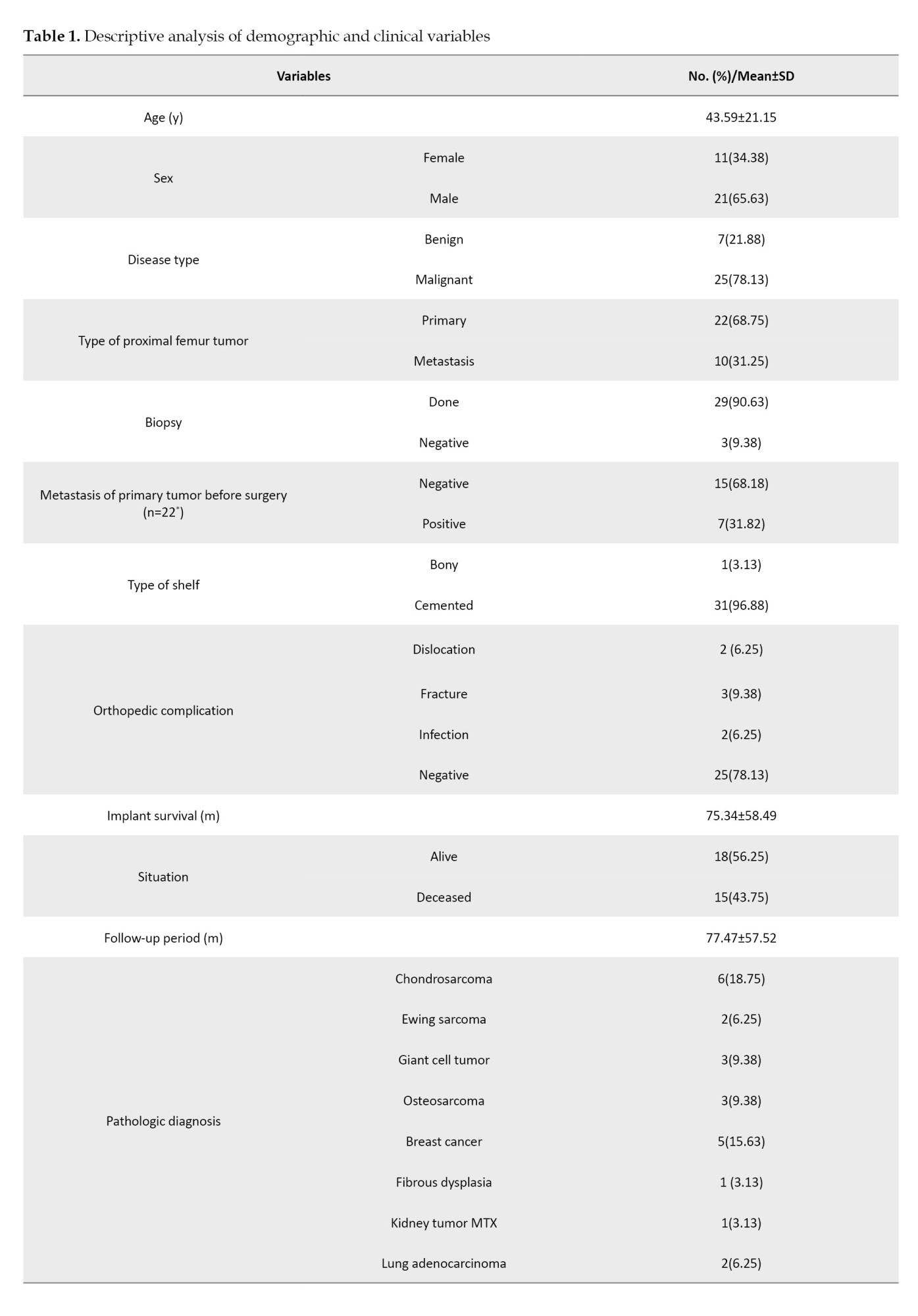
The mean implant survival was 75.34±58.49 months. Among the 14 patients who died, lung metastasis was the leading cause of death, accounting for 71.43% of cases, highlighting its significant impact on mortality in this group.
The study also analyzed the distribution of gender, mean age, recurrence of primary and metastatic tumors, and the type of proximal femur tumor based on the presence or absence of dislocation using two-way tables. No statistically significant differences were found between these variables and the occurrence of dislocation. The mean age of patients who experienced dislocation was 41.5±34.65 years, while those without dislocation had a mean age of 43.7±20.89 years. Dislocation occurred in 8% of patients without primary tumor recurrence, but no dislocations were observed in patients with primary tumor recurrence. Additionally, dislocation was reported in over 14% of patients with metastatic tumor recurrence, while none of the patients without metastatic tumor recurrence experienced dislocation. Overall, there was no significant correlation between primary or metastatic tumor recurrence and the presence of dislocation (P=1.00) (Table 2).
Discussion
This study evaluated the clinical outcomes of acetabulum reconstruction using the shelf procedure in patients undergoing bipolar hemiarthroplasty following proximal femoral tumor resection. The findings demonstrate that this approach provides favorable functional outcomes, with a notably low dislocation rate of 6.3%, which is significantly lower than rates reported in previous studies. For instance, Ashford et al. reported a dislocation rate of 35% in patients undergoing PFR. The reduced dislocation rate in our cohort can be attributed to the meticulous surgical technique, including preservation of the acetabulum, capsulorrhaphy, and reconstruction of the abductor mechanism, which collectively enhance hip stability, as reported by Bickels et al. in 2000 [1, 15]. The functional outcomes, as assessed by the MSTS scoring system, further underscore the efficacy of this approach. The ability to reattach the gluteus medius and minimus during the reconstruction of the bone plays a critical role in maintaining abductor function, which is essential for gait and overall hip stability [17]. This is particularly important in patients with extensive proximal femoral resections, where abductor function is often compromised. The use of cemented bipolar femur replacements provides immediate stability, which is advantageous in patients with metastatic disease or those at risk of pathological fractures [9]. Orthopedic complications, including fractures and infections, were observed in a small percentage of cases, consistent with the known risks associated with endoprosthetic reconstruction [11, 12]. However, the absence of a significant correlation between tumor recurrence and dislocation suggests that the surgical technique and implant positioning are more critical determinants of stability than the oncological status of the patient. This finding highlights the importance of surgical precision and the role of the shelf procedure in achieving stable hip articulation, even in cases with aggressive tumor biology. The high rate of lung metastasis as the leading cause of death (71.43%) in this study underscores the aggressive nature of metastatic bone disease and the importance of systemic oncological management in these patients [4]. Despite this, the low dislocation rate and satisfactory functional outcomes indicate that bipolar hemiarthroplasty with acetabulum reconstruction remains a viable option for improving the quality of life in patients with limited life expectancy. This is particularly relevant given the growing emphasis on palliative care and the need to balance oncological control with functional restoration in patients with advanced disease [5, 6]. In comparison to total hip replacement, bipolar hemiarthroplasty with the shelf procedure offers enhanced stability and a lower risk of dislocation, making it particularly suitable for patients with extensive proximal femoral resections [20]. The findings of this study align with recent literature supporting the use of bipolar hemiarthroplasty in oncological reconstructions, reinforcing its role as a reliable method for hip articulation in complex cases [21]. The modular design of modern endoprostheses allows for customization based on the extent of resection, further enhancing their utility in LSS [8].
Conclusion
In conclusion, this study provides robust evidence that bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure is a safe and effective option for patients undergoing proximal femoral resection due to musculoskeletal tumors. The low dislocation rate, combined with satisfactory functional outcomes, supports its use as a preferred method for hip reconstruction in this challenging patient population. Future studies with larger cohorts and longer follow-up periods are warranted to further validate these findings and refine surgical techniques for optimizing outcomes in orthopedic oncology.
Limitations
While this study provides valuable insights into the outcomes of bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure, several limitations should be acknowledged. First, the retrospective design introduces potential biases in data collection and analysis, as it relies on historical records and may lack standardized follow-up protocols. Second, the relatively small sample size (n=32) limits the generalizability of the findings and reduces the statistical power to detect significant associations, particularly for rare complications, such as dislocations or infections. Third, the single-center nature of the study may limit the external validity of the results, as surgical techniques and patient populations can vary across institutions. Fourth, the mean follow-up period of 77.46 months, while substantial, may not capture long-term complications, such as late implant failure or acetabular erosion, which could emerge beyond this timeframe. Finally, the study did not include a control group undergoing alternative reconstruction methods, such as total hip arthroplasty, which limits the ability to directly compare outcomes between different surgical approaches. Addressing these limitations in future prospective, multicenter studies with larger cohorts and longer follow-up periods would strengthen the evidence supporting this technique.
Future directions
Building on the findings of this study, several avenues for future research can further enhance the understanding and application of bipolar hemiarthroplasty combined with acetabulum reconstruction using the shelf procedure. First, prospective, multicenter studies with larger patient cohorts are needed to validate the low dislocation rates and favorable functional outcomes observed in this study. Such studies would provide stronger evidence and improve the generalizability of the results across diverse patient populations and surgical settings. Second, comparative studies between bipolar hemiarthroplasty and total hip arthroplasty in the context of proximal femoral tumor resection would provide valuable insights into the relative advantages and disadvantages of each approach. This would help surgeons make more informed decisions based on patient-specific factors, such as tumor biology, life expectancy, and functional demands. Third, biomechanical studies could explore the role of implant design and surgical techniques in enhancing hip stability and reducing complications. For example, investigating the impact of modular prostheses, custom implants, or alternative fixation methods could lead to innovations that further improve outcomes. Finally, the integration of advanced imaging and navigation technologies into surgical planning and execution could enhance the precision of tumor resection and implant placement, potentially reducing complications and improving functional outcomes. The use of 3D-printed patient-specific implants and biomaterials or augmented reality-guided surgery represents promising areas for future exploration.
Ethical Considerations
Compliance with ethical guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Research Ethics Committee of Iran University of Medical Sciences, Tehran, Iran (Code: IR.IUMS.REC.1403.859). Informed consent was obtained from all participants included in the study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization: Sam Hajialiloo Sami; Investigation: Sam Hajialiloo Sami, Khalil Kargar, and Amin Hamidzadeh Khiavi; Data curation: Amin Hamidzadeh Khiavi, and Bushra Zareie; Formal analysis: Bushra Zareie; Writing the original draft: Amin Hamidzadeh Khiavi, and Roshanak Shams; Review and editing: All authors.
Conflict of interest
The authors declared no conflict of interests.
Acknowledgments
The authors gratefully acknowledge the contributions of all the patients who participated in this study, as well as the surgeons, nurses, and medical staff involved in the care and treatment provided. Special thanks to the multidisciplinary teams whose collaboration made the comprehensive management of these complex cases possible.
References
- Ashford RU, Hanna SA, Park DH, Pollock RC, Skinner JA, Briggs TW, et al. Proximal femoral replacements for metastatic bone disease: Financial implications for sarcoma units. Int Orthop. 2010; 34(5):709-13. [DOI:10.1007/s00264-009-0838-6] [PMID]
- Zhao Z, Wang J, Guo Y, Niu J, Guo W, Yang R, et al. The outcomes of proximal femur replacement with hemiarthroplasty after tumor resection in individuals with Parkinson's disease. Front Surg. 2023; 10:1279813. [DOI:10.3389/fsurg.2023.1279813] [PMID]
- Li B, Yu Y, Bao Y, Song J. Proximal femoral tumor resection followed by joint prosthesis replacement: A systematic review and meta-analysis. BMC Musculoskelet Disord. 2023; 24(1):779. [DOI:10.1186/s12891-023-06913-w] [PMID]
- Abou Senna WG, Ebeid WA, Abdel Moneim M, Saladin M, Hasan BZ, Badr IT, Abdel Karim M. Long-term outcome of patients with primary or secondary tumors of the proximal femur treated by bipolar modular tumor prosthesis. Arch Orthop Trauma Surg. 2022; 142:33-9. [Link]
- Xu M, Wang Z, Yu XC, Lin JH, Hu YC. Guideline for limb-salvage treatment of osteosarcoma. Orthop Surg. 2020; 12(4):1021-9. [DOI:10.1111/os.14365] [PMID]
- Hovav O, Kolonko S, Zahir SF, Velli G, Chouhan P, Wagels M. Limb salvage surgery reconstructive techniques following long-bone lower limb oncological resection: A systematic review and meta-analysis. ANZ J Surg. 2023; 93(11):2609-20. [DOI:10.1111/ans.18335] [PMID]
- Banskota N, Fang X, Yuan D, Lei S, Zhang W, Duan H. Comparative study of proximal femur bone tumor patients undergoing hemiarthroplasty versus total hip arthroplasty: A meta-analysis. J Clin Med. 2023; 12(3):1209. [DOI:10.3390/jcm12031209] [PMID]
- Theil C, Möllenbeck B, Gosheger G, Schmidt-Bräkling T, Andreou D, Henrichs MP, et al. Acetabular erosion after bipolar hemiarthroplasty in proximal femoral replacement for malignant bone tumors. J Arthroplasty. 2019; 34(11):2692-7. [DOI:10.1016/j.arth.2019.06.014] [PMID]
- Calabró T, Van Rooyen R, Piraino I, Pala E, Trovarelli G, Panagopoulos GN, et al. Reconstruction of the proximal femur with a modular resection prosthesis. Eur J Orthop Surg Traumatol. 2016; 26(4):415-21. [DOI:10.1007/s00590-016-1764-0] [PMID]
- Hu X, Lu M, He X, Li L, Lin J, Zhou Y, et al. Hip reconstruction using a customized intercalary prosthesis with the rhino horn-designed uncemented stem for ultrashort proximal femur segments following tumor resection: A combined biomechanical and clinical study. BMC Musculoskelet Disord. 2022; 23(1):852. [DOI:10.1186/s12891-022-05805-9] [PMID]
- Mori T, Kobayashi E, Sato Y, Takenaka S, Endo M, Nakamura T, et al. What are the complication rates and factors associated with total femur replacement after tumor resection? Findings from the Japanese musculoskeletal oncology group. Clin Orthop Relat Res. 2024; 482(4):702-12. [DOI:10.1097/CORR.0000000000002874] [PMID]
- Sevelda F, Schuh R, Hofstaetter JG, Schinhan M, Windhager R, Funovics PT. Total femur replacement after tumor resection: Limb salvage usually achieved but complications and failures are common. Clin Orthop Relat Res. 2015; 473(6):2079-87. [DOI:10.1007/s11999-015-4282-1] [PMID]
- Jawad MU, Brien EW. Proximal femoral reconstruction with a constrained acetabulum in oncologic patients. Orthopedics. 2014; 37(2):e187-93. [DOI:10.3928/01477447-20140124-24] [PMID]
- Belthur MV, Grimer RJ, Suneja R, Carter SR, Tillman RM. Extensible endoprostheses for bone tumors of the proximal femur in children. J Pediatr Orthop. 2003; 23(2):230-5. [DOI:10.1097/00004694-200303000-00018] [PMID]
- Bickels J, Meller I, Henshaw RM, Malawer MM. Reconstruction of hip stability after proximal and total femur resections. Clin Orthop Relat Res. 2000; (375):218-30. [DOI:10.1097/00003086-200006000-00027] [PMID]
- Henderson ER, Keeney BJ, Pala E, Funovics PT, Eward WC, Groundland JS, et al. The stability of the hip after the use of a proximal femoral endoprosthesis for oncological indications: Analysis of variables relating to the patient and the surgical technique. Bone Joint J. 2017; 99-B(4):531-7. [DOI:10.1302/0301-620X.99B4.BJJ-2016-0960.R1] [PMID]
- Stevenson JD, Kumar VS, Cribb GL, Cool P. Hemiarthroplasty proximal femoral endoprostheses following tumour reconstruction: Is acetabular replacement necessary? Bone Joint J. 2018; 100-B(1):101-8. [DOI:10.1302/0301-620X.100B1.BJJ-2017-0005.R1] [PMID]
- Thaler M, Manson TT, Holzapfel BM, Moskal J. Proximal femoral replacement using the direct anterior approach to the hip. Oper Orthop Traumatol. 2022; 34(3):218-30. [DOI:10.1007/s00064-022-00768-5] [PMID]
- Zavras AG, Fice MP, Dandu N, Rossi DM, Gitelis S, Blank AT, et al. Indication for proximal femoral replacement is associated with risk of failure. J Arthroplasty. 2022; 37(5):917-24. [DOI:10.1016/j.arth.2022.01.013] [PMID]
- Saglam F, Baysal O, Sirin E, Sofulu O, Kesimer MD, Erol B. Is bipolar hemiarthroplasty an appropriate type of hip articulation following proximal femoral or total femoral resections for musculoskeletal malignancies? Arch Orthop Trauma Surg. 2022; 142(2):331-41. [DOI:10.1007/s00402-021-03980-3] [PMID]
- Liu L, Deng XQ, Zhao YJ, Ma RX, Yang L, Song KX, et al. Modular intercalary prosthetic reconstruction for malignant and metastatic tumours of the proximal femur. Sci Rep. 2024; 14(1):5867. [DOI:10.1038/s41598-024-56645-7] [PMID]
Type of Study: Research Article |
Subject:
Tumor surgery
Received: 2023/02/18 | Accepted: 2023/03/24 | Published: 2024/02/1
Received: 2023/02/18 | Accepted: 2023/03/24 | Published: 2024/02/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









